Abstract
In developed countries, low disparity in lifespan contributed by the reduction in the burden of noncommunicable diseases (NCDs) is the key to advances in epidemiological transition. Contrarily, India passing through a phase of the dual burden of CDs and NCDs shows a heavy burden of NCDs responsible for the high disparity in lifespan. The Gini coefficient was decomposed for examining the contribution of 22 causes of death and their repercussions for inequality in age at death for 30 years between 1990–1994 and 2015–2019, using Global Burden of Disease data. The outcomes of the study reveal that India’s epidemiological transition has been just modest on account of high inequality in mortality by NCDs emplaced in the middle through old age despite a consistent mortality decline at infant through old age for communicable diseases (CDs). The structural changes in causes of death structure is shaped by CDs rather than NCDs, but overall bolstered by the adult mortality decline, especially in women. However, the process is restrained by the small contribution of the middle age group and a benign contribution of old mortality decline owing to the low threshold age. India needs to target health interventions in seeking significant mortality decline in the middle age group of 50–69 years that is warranted for epidemiological transition apace as evident in the developed nations.
Similar content being viewed by others
Introduction
Many developed countries in the past long-term have conformed with the course of epidemiological transition as described by Omran’s theory1,2. Omran’s epidemiological transition2 ardently advocates the substitution of communicable diseases (CDs) by the heavy burden of noncommunicable diseases (NCDs) while passing from the phase of ‘Age of Receding Pandemics’, and until the ‘Age of Degenerative and Man-made Diseases.’ However, aberrations are also highlighted3,4,5,6,7, especially with the increase in the pathogenesis and aetiology of chronic diseases and also, imbricated causations across infectious and chronic diseases8,9,10 that are entwined with man-made diseases11. The epidemiological transition shows strong linkages with the advances in mortality transition intrigued by the causes of death structure12,13. Structural changes in causes of death and progression in epidemiological transition is majorly driven by the larger reduction in premature deaths at ages14,15 below the threshold age that separates premature deaths from old ages16. The same diseases show affirmative (positive) role at premature ages whereas show opposing (negative) roles in old ages17,18 owing to the threshold age19. This disparateness of affirmative and dissenting roles about the threshold age of same causes of death is conspicuous in the analysis of lifespan disparity (e†) or inequality in age at death20,21 measured by Gini coefficient at birth (G0)22,23 as compared to life expectancy at birth (e0). Developed countries passing through low mortality regime have shown significant developments in the causes of death structure, low inequality in age at death24, and mortality and/or morbidity compression25,26; however, these phenomena stand modest in developing countries27. Among these fundamental phenomena, exploration of inequality in age at death by age-sex and causes of death deciphers scrupulous assessments of the structural changes in causes of death and hence the progress of epidemiological transition.
Developed countries such as the European Unions, New Zealand, Japan, and England & Wales experience apace in epidemiological transition because of greater reduction in premature mortality, high threshold age, and swift structural changes in cause of death28. The USA’s health policies asserted for the reduction in burden of chronic NCDs29; however, the results over time exhibited higher e† and lower e0 compared to other developed countries30,31. Shkolnikov et al.23 demonstrate higher G0 values in the USA than in the UK attributable to lesser reduction in premature mortality though both countries show similar threshold age, i.e. 80 years and above32. However, developing countries such as India and South Africa show the threshold age of 71.3 years and 58.7 years, respectively32. A low threshold age provides a narrow age-interval for reduction in premature mortality. So, a lag of ten and more years in the threshold age restraints the affirmative contribution of premature ages and moreover, augments negative repercussions of middle and old ages on mortality reductions in developing countries. As a consequence, a reduction in the premature mortality is subdued and the structural changes in causes of death is constrained. Over and above that, developing country India has the challenge of economic cost for the causes of death surveillance33, along with the cognisance of health transition34 and morbidity expansion35.
Smits and Monden36 demonstrates that the diffusion hypothesis is more conclusive while it is contingent upon the reduction in premature mortality. The oversimplification of the Omran’s model is not justified in the cognisance of the welfare Kuznets curve37. A developing country India do achieve on the higher survival of infants, children, and mothers38 to reducing premature mortality through long-term health programmes and policies39. However, NCDs intruded in the mid-1990s, and since thereupon premature mortality becomes a big concern in adult through old ages leading to dual burden of diseases in India40. Inevitably, the country attests a languid progression in mortality compression27 enduring large premature mortality and slow mortality deceleration41,42. Therefore, it is crucial to examine the role of the heavy burden of chronic NCDs43,44 and also injuries45 over a wide age range in adult through old ages for the progression in epidemiological transition in India.
The study assesses the role of inequality in age at death by causes of death for advances in epidemiological transition in India during a period of 30 years between 1990–1994 and 2015–2019. We tested the hypotheses that (a) whether chronic NCDs versus communicable diseases (CDs) contributes to higher inequality in age at death, (b) whether mortality decline in adult and higher age groups is crucial for structural changes in causes of death in high versus low mortality regimes; and, together they construe the prolonged dual burden of disease in India. The specific objectives of the study are (1) to assess the age- and cause-specific contribution to the changes in life expectancy at birth (Δe0) and inequality in age at death (ΔG0) and (2) to examine the transformation in age at death by age, sex, and causes of death. The study aims to explore the phenomenal phase of dual burden of disease by inequalities in mortality by causes of death and hence comprehends the progress of epidemiological transition in India.
Data and methods
Data
The age-cause-specific death rates (ACSDR) for 21 causes of death (level 2) by quinquennial age groups up to 95 + years and sex were retrieved from Global Burden of Disease (GBD)46 for the entire period of 1990–2019 (Supplementary Figs. S1 and S2). The causes of death are mapped with International Classification of Diseases (ICD) 10 classification47 in GBD data. There has been concern and issues for the availability of data and quality of data on causes of death for many countries as obstacles for computing mortality estimates48,49,50,51. The GBD data provides mortality estimates adjusted for systematic biases or inaccurate reporting for many countries and is also comparable across regions and time.
Methods
Construction of abridged life tables
Abridged life tables were constructed using the Chiang method52,53, based on five-year moving average of ACSDR of 21 causes of death and overall mortality rate, by sex, in the studied period. Chiang method is based on the derivation of relation for the total number of person-years lived between exact ages x and x + n (\({{}_{n}\mathrm{L}}_{\mathrm{x}})\) in terms of the average number of years lived by an individual of age x who dies in the interval (x, x + n) \(({{}_{n}\mathrm{a}}_{\mathrm{x}}\)). The columns of the life table are obtained using the following formulas:
\({{}_{n}\mathrm{q}}_{\mathrm{x}}:\) probability of dying between age x and x + n
\({\mathrm{l}}_{\mathrm{x}}:\) number of people alive at the exact age x among a hypothetical birth cohort of 100,000, usually called the radix of the life table.
\({{}_{n}\mathrm{d}}_{\mathrm{x}}:\) number of deaths in the age interval x to x + n
\({{}_{n}\mathrm{L}}_{\mathrm{x}}:\) total number of person-years lived between exact ages x and x + n
\({{}_{n}\mathrm{a}}_{\mathrm{x}}:\) average number of years lived in the age interval x to x + n
\({\mathrm{T}}_{\mathrm{x}}:\) total number of person-years lived beyond Age x
\({\mathrm{e}}_{\mathrm{x}}\): average number of years of life remaining for a person alive at the beginning of age interval x.
Inequality in age at death
The Gini coefficient at birth (G0) and the disparity in lifespan (e†) are often applied in the field of demography. G0 measures the variability in age at death. Whereas, e† measures life years lost due to deaths. Wilmoth and Horiuchi54 and Vaupel, et al.32 have shown that many inequality measures, including the Gini, are highly correlated. We applied G022 as a measure of inequality in age at death because it satisfies the four fundamental properties, i.e. the Pigou-Dalton transfer principle, scale invariance, population variance, and symmetry for an inequality measure23, and so, is a preferred measure of inequality. The G0 for an abridged life table is expressed as:
where,
\({\widehat{a}}_{x}\) is the adjusted \({a}_{x}\) for deviation in the pace of \({{}_{n}q}_{x}\) by age, and \({a}_{x}\left[=\frac{\left({{}_{n}L}_{x}/n\right)-{l}_{x+n}}{({l}_{x}-{l}_{x+n})}\right]\) is the person-years lived by the individuals who have died within the given interval.
Decomposition of e0 and G0 using the replacement method
Yadav, et al.55 shows that discrete56 and replacement57 methods of decomposition analyses23,58 produce similar results for e0 and G0. The difference of quantities between two populations is shown as
and,
where, \({M}^{({x}_{i})}\) is a vector of age-specific death rates (ASDR) with elements \(m^{\prime}_{x}\) for x < = xi and \({m}_{x}\) for x > = xi.
Decomposition of e0 and G0 by causes of death and age groups
Specifically, the contribution of \({j}{th}\) cause of death to the contribution \({\in }_{i}\) in \({i}{th}\) age-interval [\(x, x+n)\) is calculated as
where, \({{}^{a}m}_{{x}_{i}|{x}_{i+n}}^{j}\) and \({{}^{b}m}_{{x}_{i}|{x}_{i+n}}^{j}\) are ACSDR of \({j}{th}\) cause of death in \({i}{th}\) age-interval [\(x, x+n)\) in the population \(a\) and \(b\), respectively, and \({{}^{a}m}_{{x}_{i}|{x}_{i+n}}\) and \({{}^{b}m}_{{x}_{i}|{x}_{i+n}}\) are ASDR in \({i}^{th}\) age-interval [\(x, x+n)\) in the population \(a\) and \(b\), respectively. The decomposition analysis provides age-cause-specific contributions to Δe0 and ΔG0 for both sexes, which are comparable across population subgroups and over time. The age group of 85+ years is the last age group presented for any level of presentation. Also, we have considered neonatal disorders and maternal disorders as separate diseases, so 22 causes of death in total.
Ethical approval
We confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Results
Age-specific contributions to Δe0 and ΔG0, India, 1990–2019
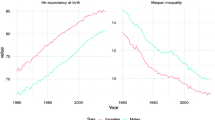
The e0 for men and women increased from 59.8 and 60.8 years in 1990–1994 to 68.8 and 71.3 years, respectively, during 1990–2019. Contemporaneously, the G0 values for men and women declined respectively from 0.219 and 0.225 in 1990–1994, 0.188 and 0.181 in 2003–2007, and to 0.154 and 0.146 in 2015–2019 (Fig. 1). Men compared to women show higher G0 values since the mid-2000s. A higher G0 value confirms high uncertainty in age at death in men than in women. The decomposition analysis of these G0 values by quinquennial age groups reveals a huge equalising contribution of 78.1 and 69.6% to ΔG0 (Fig. 3, Table 1) by male and female in 0–4 years, respectively, which is approximately one-and-a-half times than that to Δe0 (Fig. 2, Table 1). It testifies that decline in G0 values is majorly driven by mortality reductions among infants and children.
However, men and women in their adult age group of 15–49 years have shown most dramatic temporal changes from almost zero or negative contribution in the late 2000s and then manoeuvre it to considerable values of 19.4 and 25.4% to ΔG0 (Fig. 3) and 15 and 18.8%, respectively, to Δe0 in the late 2010s (Fig. 2). This skimpy, meagre contribution of adult ages in men has played a major role for the sex differentials in e0 and G0 negatively skewed towards men.
The discordance between age-specific contributions to Δe0 and ΔG0 are apparent in the middle (50–69 years) and old (70 + years) age groups. The contribution of 19.5 and 14%, respectively, to Δe0 by men and women in middle age group is approximately three-folds than that to ΔG0. It shows a quantum leap for Δe0 but not for ΔG0. On the other hand, a disequalising (negative) contribution of − 14.5 and − 12.9% to ΔG0 by men and women in old ages, respectively, signify a disparate role not manifested in the decomposition analysis of Δe0 (Table 1). These large disequalising contributions impede the progression in G0, hence the phenomenon of high e0 and low G0 is restrained.
The scrutinization of outputs reveals greater, significant role of infant and child age groups for changes in G0 and e0 for the entire period of 1990–2019; however, to take note, their age-specific contributions to ΔG0 and Δe0 has more or less remained unchanged over time. Rather, temporal changes in age-specific contributions at adult (15–49 years) especially in men are conspicuous. Further, the middle and old age groups contributed variably to Δe0 and ΔG0, but, their temporal contribution has moderately changed. In sum, India’s pattern of age-specific contributions to Δe0 or ΔG0 has remained more or less similar during studied period; nonetheless, the pattern has shown encouraging mortality changes at adult ages since the mid-2000s.
Dominance of chronic NCDs versus CDs, India, 1990–2019
The decomposition analysis by causes of death demonstrate that communicable diseases (CDs), NCDs, and injuries contributed respectively 85.6, 4.6, and 9.8% in men and 86.8, 4.8, and 8.3% in women to ΔG0 between 1990–1994 and 2015–2019 (Table 2). The contributions to ΔG0 by NCDs were larger when compared to that of Δe0. The results show that CDs committedly reshapes the distribution of age at death, whereas NCDs hardly matters for equalising age at death. Exploring by 22 causes of death (Figs. 4 and 5) reveals that the huge contribution by CDs in men and women comprises of the largest contribution of 24.4 and 20.9%, respectively, to ΔG0 by respiratory infections and tuberculosis. Respiratory infections and tuberculosis together with other infectious diseases, enteric infections, and neonatal and maternal disorders have contributed approximately 72.7 and 74.1% to ΔG0 in men and women, respectively. Temporal analysis reveals that the share of these four diseases have remained nearly stagnant to ΔG0 (Fig. 5) and Δe0 (Fig. 4) in the studied period. This nearly stagnant contributions confirm a consistent mortality decline for these four diseases. In addition to that, the share of neonatal disorders in female children has been approximately doubled from 6.9 in 1990–1994 to 11.4% to ΔG0 in 2015–2019, confirming a mortality decline among female children. However, the share of neglected tropical diseases and malaria and nutritional deficiencies reduced by half to ΔG0 during 1990–2019 because of mortality increase. Of great importance, these CDs manoeuvre a low dispersion in the distribution of age at death and guides the causes of death structure.
HIV/AIDS and sexually transmitted infections is the only disease among CDs, which had shown negative contribution to Δe0 as well as disequalising contribution to ΔG0 for more than 20 years between the mid-1990s and the mid-2010s. Nonetheless, this negative contribution of HIV/AIDS and sexually transmitted infections reduced to ~ − 0.5% in 2015–2019, with the rapid decline in its prevalence and mortality rate.
Among injuries, unintentional injuries in men and women have shown small contributions of 6.2 and 4.2% to ΔG0, respectively. Other two causes of death, namely self-harm and interpersonal violence and transport injuries, showed very small contributions (Table 2).
Compared to CDs and injuries, NCDs have shown small contribution to Δe0 and negligible contribution to ΔG0. Chronic respiratory diseases, mainly comprise of chronic obstructive pulmonary disease (COPD), asthma, and pneumoconiosis, and cardiovascular diseases, mainly comprise of hypertensive heart disease and strokes, have shown contributions in the range of 6–8% to Δe0; however, they showed negligible contributions to ΔG0. Specifically, chronic respiratory diseases and cardiovascular diseases in men has shown disequalising contributions to ΔG0 between the mid-2000s to the mid-2010s which indicates expansion of deaths over age and time.
In sum, NCDs shows insignificant effect on the dispersion in age at death besides small contribution to Δe0 that corroborates a shift in age at death. Negligible contributions by many causes of death among NCDs to ΔG0 intrinsically negate their small contributions to Δe0. Thus, NCDs has shown an insufficient contribution and attests its aftermath by impeding the progression in G0. Further, the dominance of NCDs at adult and higher ages is also upheld by the modest adult-, middle-, and old-age mortality decline.
Transformation in distribution of age at death by causes of death, India, 1990–2019
India during the period of 1990–2019 shows an impressive pattern of age-specific contributions mainly dominated by CDs in infant through old ages (Figs. 6, 7, 8, and 9). Infants show reduction in their toll of deaths caused by neonatal disorders which have been most crucial for a shorter toe of the tilted j-shaped age pattern of mortality (see Supplementary Figs. S1 and S2) and thus, to a more left-skewed unimodal distribution of age at death. This transformation was also sustained by the reduction in the burden caused by respiratory infections and tuberculosis, enteric infections, other infectious diseases, and nutritional deficiencies in infant as well as child and adolescent age groups (Figs. 7 and 9).
Temporal changes in age-cause-specific contributions to Δe0, men and women, India, 1990–2019. CRD, chronic respiratory diseases, CVDs cardiovascular diseases, Dia&k diabetes and kidney diseases, DigeD digestive diseases, Enter enteric (diarrhea and typhoid) infections, HIV/A HIV/AIDS and STI, Mat maternal disorders, Menta mental disorders, Muscu musculoskeletal disorders, Neo neonatal disorders, Neopl neoplasms, Neuro neurological disorders, NTD&M neg. tropical diseases and malaria, NutrD nutritional deficiencies, ONCDs other noncommunicable diseases, Otinf other infectious diseases, RI&T respiratory infections and tuberculosis, SelHV self-harm and interpersonal violence, SkiSu skin and subcutaneous diseases, SubUs substance use disorders, Trans transport injuries, Unint unintentional injuries.
Temporal changes in age-cause-specific contributions to ΔG0, men and women, India, 1990–2019. CRD, chronic respiratory diseases, CVDs cardiovascular diseases, Dia&k diabetes and kidney diseases, DigeD digestive diseases, Enter enteric (diarrhea and typhoid) infections, HIV/A HIV/AIDS and STI, Mat maternal disorders, Menta mental disorders, Muscu musculoskeletal disorders, Neo neonatal disorders, Neopl neoplasms, Neuro neurological disorders, NTD&M neg. tropical diseases and malaria, NutrD nutritional deficiencies, ONCDs other noncommunicable diseases, Otinf other infectious diseases, RI&T respiratory infections and tuberculosis, SelHV self-harm and interpersonal violence, SkiSu skin and subcutaneous diseases, SubUs substance use disorders, Trans transport injuries, Unint unintentional injuries.
In the later stages of life, i.e. from adult to old ages, respiratory infections and tuberculosis and enteric infections show their distinguishable contributions to Δe0 and ΔG0 (Figs. 6 and 8). Adult men and adult women show respectively 4.5 and 9.2% whereas middle-aged men and middle-aged women show 2.3 and 3.7% reduction in toll of deaths caused by respiratory infections and tuberculosis and enteric infections for a better G0 (Figs. 8 and 9). Adult women did experience an aversion of 6.5% maternal deaths in addition to whatsoever reckoned in adult men (Figs. 7 and 9). Contrary to these equalising effects by many CDs, HIV/AIDS and sexually transmitted diseases exhibited disequalising effect on ΔG0 by adult men and adult women which lessens the equalising contribution in adult age group for a span of time (Fig. 9).
Men and women in their middle-age group have shown small contributions of 2.3 and 3.7% to ΔG0, respectively, by respiratory infections and tuberculosis together with enteric infections. Compared to these two predominant diseases, cardiovascular diseases plus chronic respiratory diseases for men and women respectively have shown smaller contribution of 0.8 and 1.7% in adult age group and 1.1 and 1.8% in the middle age group to ΔG0 (Figs. 7 and 9). In sum, these four causes of death contributed on an average 3.3 and 5.5% to ΔG0 (Fig. 9) whereas 17.8 and 14.6%, respectively, to Δe0 (Fig. 7) by men and women in their middle ages. These large contribution to Δe0 by enteric infections and respiratory infections and tuberculosis at middle ages attested deceleration in mortality rates (Supplementary Fig. S1), but a small contribution to ΔG0 at the same ages reveals negligible changes in the distribution of age at death. The middle-aged persons survived and delayed their deaths; thus, they have been instrumental for a shift in the distribution of age at death by adding a few points to e0 but insignificantly contribute to its dispersion. Thus, its insufficient contribution for a change in dispersion curbs the progression in G0.
The progression in G0 is further opposed by the three-fold disequalising effect for both men and women in their old age group of 70 + years in comparison to that of middle age group by the same causes of death, i.e. respiratory infections and tuberculosis, enteric infections, cardiovascular diseases and chronic respiratory diseases. By causes of death, the disequalising effect in 70 + years is mainly contributed by enteric infections; on an average, a contribution of − 4.2 and − 6.4% to ΔG0 in men and women, respectively, during 1990–2019 (Fig. 9). The disequalising effect in old men and old women were approximately − 1.5 and − 2% to ΔG0, respectively, for each of cardiovascular diseases, chronic respiratory diseases, and respiratory infections and tuberculosis and enteric infections (Fig. 9). The disequalising contributions by these dominant causes of death at old ages are a consequence of a higher mortality rates with minor changes at old ages (Figs. 8 and 9). Also, disequalising contribution at old ages in India remains large because of senility and low threshold age.
To note, the chronic NCDs, enteric infections and respiratory infections and tuberculosis showed larger disequalising contributions in old age group than small equalising contributions in the middle age group. So, the net contribution by chronic NCDs and enteric infections and respiratory and infectious diseases in higher age groups is negative. Also, other causes of death showed negligible contributions in middle and old age groups. It implies that a wide age-interval comprising middle and old ages in India is not at all contributing to the progression in G0.
The outcomes reveal that the transformations in age at death are majorly contributed by enteric infections followed by respiratory diseases and infectious diseases. CDs have been contributory for a shift in e0 as well as reshaping the distribution of age at death despite its lower mortality rate than that of NCDs during the studied period. Contrary to the remarkable role of CDs, many NCDs did not contribute enough to equalising age at death in adult through old ages; however, they corroborate for a trivial shift in e0. Nonetheless, a greater change in CDs and a subtle change in NCDs testify the progression in the later phases of epidemiological transition.
Overall, the results reveal a worsening phase in epidemiological transition caused by chronic NCDs in adult, middle, and old age groups, with nearly unchanged toll of deaths caused by injuries in adult ages, with great contribution of mortality decline of CDs in infant through oldest of old ages. While the analyses of e0 conceals the reason for modest changes in cause of death structure, particularly for NCDs, the analyses of G0 apparently highlights negligible contribution in wide age-interval in middle through old ages. The outcomes unravel that progression in epidemiological transition is curbed by the high inequality in age at death caused by chronic NCDs in India. Higher inequalities in age at death contributed by the mortality pattern of chronic NCDs raises concern about the structural changes in causes of death not befitting the progression in epidemiological transition.
Discussion
India transcended from the high mortality regime in the early 1990s to a low mortality regime in the late 2010s. Despite showing a significant decline in the burden of CDs mainly among infants and children during 1990–2019, the adults and olds are enduring the heavy burden of NCDs together with that of CDs. There are evidences of chronic NCDs contributing for a rise in e0 (Figs. 2 and 4); nonetheless, its role for causes of death structure explicitly examined by disparity in lifespan is more crucial. In particular, for India, mortality analysis by causes of death has largely remained unexplored. Acknowledging the gap, this study examines the inequality in mortality (Fig. 1) by 22 causes of death by performing the decomposition analyses59 to assess age-cause-specific contributions to the changes in life expectancy at birth (Δe0) and inequality in age at death (ΔG0), using GBD data for the entire period of 1990–2019. The study aims to examine the progress of epidemiological transition during a period of 30 years between 1990 and 2019.
The study outcomes reveal that many CDs rather than NCDs significantly contributed to Δe0 and ΔG0 (Table 2). A reduction in the burden of CDs in infant through old ages signify their greater role for a structural change in causes of death (Figs. 4 and 5). Amongst demographic age groups, infants have been the largest contributor to Δe0 and ΔG0 followed by children, adolescents, and women in their reproductive age groups (Figs. 2 and 3). The same is also corroborated by the rapid decline in infant mortality rate and under-five mortality (U5MR), and Maternal Mortality Ratio (MMR)60 over time. Further, the dramatic changes in the age-specific contributions by men in adult age group is bolstered by the reduction in the burden of HIV/AIDS and sexually transmitted diseases61 together with that of respiratory infections and tuberculosis and enteric infections. Enteric infections and respiratory infections and tuberculosis also show considerable contributions to Δe0 and ΔG0 at middle and old ages (Figs. 7 and 9).
However, many NCDs at middle through old ages contribute considerably to Δe0 but negligibly to ΔG0. The disparateness in the age-specific contributions to Δe0 (Figs. 6 and 7) and ΔG0 (Figs. 8 and 9) by CDs and NCDs at middle and old ages highlights the contrasts for a shift in e0 versus transformation in age at death as measured by G0. The mortality decline for CDs at infant through old ages showed a shift in e0 as well as reshaped the distribution of age at death; however, the mortality decline for NCDs at middle and old ages trivially corroborated the shift in e0 but importantly didn’t contribute to the transformation in age at death or its dispersion (G0) (Figs. 6, 7, 8, and 9). A negligible contribution to ΔG0 by NCDs at middle through old ages was on the account of its disequalising contributions.
By the virtue of equalising (positive) and disequalising (negative) effects on G0, the NCDs and CDs showing affirmative contributions before the threshold age, however, do not contribute for a better G0 after that threshold age17,62 (Figs. 8 and 9). The low threshold age in 65–69 years62 is critical for India (Fig. 9) because a possibility of reduction in premature deaths is restrained by a narrow age-interval. On the other hand, a wide age-interval at middle through old ages burdened with NCDs as well as CDs allows for high disparity in lifespan. Thus, a low threshold age puts major constraints for possible affirmative age-specific contributions from NCDs emplaced at middle and old ages. The same is also applicable for CDs, however, given their preponderance at infant through old ages they do have large reduction in the burden at younger ages that compensates for disequalising contributions in old ages. Such changes in mortality rates by age and variations in causes of death has a repercussion on the age pattern of mortality. While there are significant changes in the mortality rates and variations in cause of death over time in the infant, child, and adult age groups; however, the same is modest in middle through old ages which is also evident in terms of modest mortality deceleration at old ages over time42,63. As a consequence, the pattern of age-specific contributions has remained more or less unchanged and a modest structural change in causes of death is witnessed in India.
On the other hand, developed countries such as Japan, Sweden, Switzerland, Singapore, Australia, Germany, Russia, the USA, and other developed countries show significant changes in the pattern of age-specific contributions as well as causes of death structure, and importantly high causes-of-death variation23,64,65,66. Bergeron-Boucher et al.13 for low-mortality countries demonstrate significant rise in cause-of-death variation, measured by entropy, since the early 1990s. Yoshinaga and Une67 for Japan demonstrate dramatic changes in the cause of death structure from the dominance of tuberculosis and pneumonia until the 1960s to cerebrovascular diseases between 1970 and 1990s, and heart diseases other than ischemic heart disease since 2000s, along with shift in the major contributing age group, i.e. from 0–4 years to 75–84 years. Japan manifests changes in causes of death structure many times and swift changes in the pattern of age-specific contributions to gain one of the highest e0 in the world. Denmark show a significant change in the contribution of middle age group which was negligible during 1960–75, and increased to large, significant contribution of ~ 50% during 1995–201417. Such mortality changes at middle through old ages64,67,68 concomitant of causes of death structure impels a stronger transformation in the distribution of age at death in order to keep epidemiological transition apace in these developed countries1,69.
On the contrary, India lacks such demographic developments. Linear increase in e0 depicts a smooth progression in mortality transition, however, scrutinization of G0 reveals high inequality in age at death caused by NCDs, similar pattern of age-specific contributions over time, and modest changes in the cause of death structure mainly attributed to CDs in the studied period. Yadav and Arokiasamy70 demonstrate a change in the causes of death structure wherein the burden of NCDs surpassed CDs in mid-1980s; however, thereafter, since the early 1990s the age pattern of mortality of many NCDs marginally changed accounting for toll of deaths (Figs. 5 and S1). The results in this study showed high inequality in mortality distribution causes by many NCDs which was camouflaged in the analysis of e0. The outcome of the study demonstrates that high inequality mortality caused by many NCDs have been responsible for slowing down the advances in the epidemiological transition during a period of 30 years between 1990 and 2019. Furthermore, the untimely and behindhand programs for chronic NCDs71 has already instigated morbidity expansion that rather strengthens dual burden of diseases in India.
In particular, India lacks a mortality decline at the middle ages. The mortality decline at middle ages dominated by high mortality rates of chronic NCDs presents three major benefits: (a) large equalising effect for decline in G0, (b) shift in the threshold age, and (c) benign disequalising contributions in old ages. This demographic development can be achieved by reduction in toll of deaths caused by enteric infections, respiratory infections and tuberculosis, cardiovascular diseases, and chronic respiratory diseases in the middle age group of 50–69 years. It appalling to note that despite a linear increase in e0, India shows a modest reduction in premature mortality that in turn undermines the fundamental demographic processes such as mortality compression, the phenomenon of high e0 and low G0, and morbidity compression. The middle age group provides a compatible possibility for progress of these fundamental demographic processes and epidemiological as well as mortality transition comparable to that in developed countries in a short time. The developed nations demonstrate advances in the third and later phases6,7 of epidemiological transition by a greater role of middle age group for structural changes among NCDs, i.e. in the age pattern of mortality, causes of death structure, and importantly causes-of-death variation.
The Ministry of Health and Family Welfare (MoHFW) in its recent health report National Multisectoral Action Plan (NMAP) for Prevention and Control of Common Noncommunicable Diseases (2017–2022)72, National Programme for Health Care of Elderly (NPHCE)73 and National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular diseases and Strokes (NPCDCS)74 strategizes for the assessment of economic and mortality burden of NCDs by strengthening patient data and harmonization of disease data. Under NPCDCS, the MoHFW has proposed to developed standard protocols for data collection, analysis, and reporting of data for different NCDs services at all levels. For this purpose, the Health Management Information System (HMIS) is also leveraged to identify linkage modalities with NCDs services. The interpretation of the results could be better explained with a harmonized data between other sources of data such as Sample Registration System (SRS), Medical Certification of Causes of death (MCCD), and MoHFW, and other health survey data. However, for India, details of causes of death mapped with ICD classification are not available by age, sex and residence for a long period. Also, the use of detailed GBD data needs cautious interpretations50,51,75,76. While the life table estimates between GBD data and SRS are very close; nonetheless, synchronous details of causes of death since the early 1990s are available in GBD data.
The national NCD monitoring framework in way forward has prioritise the reduction of premature mortality from 10 to 25% in another five years in the age group of 30–70 years caused by cardiovascular diseases and chronic respiratory diseases72. The outcomes of this study point out that surveillance of population in the middle age group of 50–69 years for NCDs, especially COPD, asthma, and pneumoconiosis, can reduce premature mortality in a short time. Also, screening and diagnosis in a narrow age interval lessens the burden on public health system and ascertain effective utilization of limited sources. The contribution of middle ages to mortality decline has been undermined just because of low threshold age in India. This remained neglected since a long time in the policy frameworks as well as research studies. The MoHFW need to prioritise for the surveillance and investment in the middle age group of 50–69 years which promises high possibility to reduction in the premature mortality.
Conclusion
The study reveals (1) large, significant contributions of CDs for reshaping the distribution of age at death and (2) an exacerbated predicament offset by the intrusion of NCDs for a high inequality in age at death. During a period of 30 years between 1990–1994 and 2015–2019, the structural changes in causes of death has been attributed to CDs and marginally to NCDs. A subtle contribution of NCDs to the transformation in distribution of age at death is evident.
The progression in epidemiological transition is modulated mainly by two factors: (a) moderate contribution of adult age group and (b) greater mortality decline attributable to CDs. The role of NCDs is emplaced at middle and higher ages and the pace of epidemiological transition has been modest because of low threshold age in India; importantly, the possible contribution of middle age group is constrained attributable to high inequality in NCDs. The study reveals the high inequality in age at death in India caused by NCDs at middle (50–69 years) ages is the priority to deal effectively in policies and programs. These are underlying reasons for the prolonged phenomenon of dual burden of diseases in India. In a long period of 30 years, India has shown modest changes in causes of death structure. It rather manifests a divergence from that of oversimplified the Omran’s epidemiological transition.
Our study outcomes highlight the urgent tuning of policies targeting middle-aged persons as their survival can make a shift in the threshold age, contribute to structural changes in cause of death, and low inequality in age at death. This will lessen the dual burden of diseases in India for a demographic leap, morbidity compression, prevent health losses and increase lifespan spent in good health.
Data availability
The datasets generated and/or analysed during the current study are available in the Global Burden of Disease Study 2019 (GBD 2019), Institute for Health Metrics and Evaluation (IHME), United States, http://ghdx.healthdata.org/gbd-results-tool46.
Abbreviations
- GBD:
-
Global burden of diseases
- IHME:
-
Institute for health metrics and evaluation
- NCDs:
-
Noncommunicable diseases
- CDs:
-
Communicable diseases
- ASDR:
-
Age-specific death rates
- ACSDR:
-
Age-cause-specific death rates
- ICD:
-
International classification of diseases
- COPD:
-
Chronic obstructive pulmonary disease
- IMR:
-
Infant mortality rate
- U5MR:
-
Under-five mortality rate
- MMR:
-
Maternal mortality ratio
- MoHFW:
-
Ministry of health and family welfare
- NPCDCS:
-
National programme for prevention and control of cancer, diabetes, cardiovascular diseases and strokes
- MCCD:
-
Medical certification of causes of death
- SRS:
-
Sample registration system
- HMIS:
-
Health management information system
- NPHCE:
-
National programme for health care of elderly
- NMAP:
-
National multisectoral action plan
- CRD:
-
Chronic respiratory diseases
- CVDs:
-
Cardiovascular diseases
- Dia&k:
-
Diabetes and kidney diseases
- DigeD:
-
Digestive diseases
- Enter:
-
Enteric (diarrhea and typhoid) infections
- HIV/A:
-
HIV/AIDS and STI
- Mat:
-
Maternal disorders
- Menta:
-
Mental disorders
- Muscu:
-
Musculoskeletal disorders
- Neo:
-
Neonatal disorders
- Neopl:
-
Neoplasms
- Neuro:
-
Neurological disorders
- NTD&M:
-
Neg. tropical diseases and malaria
- NutrD:
-
Nutritional deficiencies
- ONCDs:
-
Other noncommunicable diseases
- Otinf:
-
Other infectious diseases
- RI&T:
-
Respiratory infections and tuberculosis
- SelHV:
-
Self-harm and interpersonal violence
- SkiSu:
-
Skin and subcutaneous diseases
- SubUs:
-
Substance use disorders
- Trans:
-
Transport injuries
- Unint:
-
Unintentional injuries
References
Salomon, J. A. & Murray, C. J. L. The epidemiologic transition revisited: compositional models for causes of death by age and sex. Popul. Dev. Rev. 28, 205–228. https://doi.org/10.1111/j.1728-4457.2002.00205.x (2002).
Omran, A. R. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Mem. Fund. Q 49, 509–538 (1971).
Moser, K., Shkolnikov, V. & Leon, D. A. World mortality 1950–2000: Divergence replaces convergence from the late 1980s. Bull. World Health Organ. 83 (2005).
Santosa, A., Wall, S., Fottrell, E., Hogberg, U. & Byass, P. The development and experience of epidemiological transition theory over four decades: A systematic review. Glob. Health Action 7, 23574. https://doi.org/10.3402/gha.v7.23574 (2014).
Caselli, G., Meslé, F. & Vallin, J. Epidemiologic transition theory exceptions. Genus 58, 9–51 (2002).
Olshansky, S. J. & Ault, A. B. The fourth stage of the epidemiologic transition: The age of delayed degenerative diseases. Milbank Q 64, 355–391 (1986).
Hazra, N. C. & Gulliford, M. Evolution of the “fourth stage” of epidemiologic transition in people aged 80 years and over: Population-based cohort study using electronic health records. Popul. Health Metr. 15, 18. https://doi.org/10.1186/s12963-017-0136-2 (2017).
Mercer, A. J. Updating the epidemiological transition model. Epidemiol. Infect. 146, 680–687. https://doi.org/10.1017/S0950268818000572 (2018).
Mercer, A. Infections, Chronic Disease, and the Epidemiological Transition. A New Perspective. (University of Rochester Press, 2014).
Omran, A. R. The epidemiologic transition theory revisited thirty years later. World Health Stat. Q. 53, 99–119 (1998).
Robine, J. M. Redefining the Stages of the epidemiological transition by a study of the dispersion of life. Popul. English Select. 13, 173–194 (2001).
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet 396, 1204–1222. https://doi.org/10.1016/s0140-6736(20)30925-9 (2020).
Bergeron-Boucher, M. P., Aburto, J. M. & Raalte, A. A. V. Diversification in causes of death in low-mortality countries: emerging patterns and implications. BMJ Glob. Health 5. https://doi.org/10.1136/bmjgh-2020-002414 (2020).
Norheim, O. F. et al. Avoiding 40% of the premature deaths in each country, 2010–30: Review of national mortality trends to help quantify the UN Sustainable Development Goal for health. Lancet 385, 239–252. https://doi.org/10.1016/S0140-6736(14)61591-9 (2015).
Leon, D. A., Jdanov, D. A. & Shkolnikov, V. M. Trends in life expectancy and age-specific mortality in England and Wales, 1970–2016, in comparison with a set of 22 high-income countries: An analysis of vital statistics data. The Lancet Public Health 4, e575–e582. https://doi.org/10.1016/s2468-2667(19)30177-x (2019).
Aburto, J. M., Villavicencio, F., Basellini, U., Kjaergaard, S. & Vaupel, J. W. Dynamics of life expectancy and life span equality. Proc. Natl. Acad. Sci. U S A 117, 5250–5259. https://doi.org/10.1073/pnas.1915884117 (2020).
Aburto, J. M., Wensink, M., Raalte, A. A. V. & Lindahl-Jacobsen, R. Potential gains in life expectancy by reducing inequality of lifespans in Denmark: An international comparison and cause-of-death analysis. BMC Public Health 18, 831. https://doi.org/10.1186/s12889-018-5730-0 (2018).
Vaupel, J. W. & Romo, V. C. Decomposing change in life expectancy: A bouquet of formulas in honor of Nathan Keyfitz’s 90th birthday. Demography 40, 201–216. https://doi.org/10.1353/dem.2003.0018 (2003).
Aburto, J. M., Alvarez-Martínez, J.-A., Villavicencio, F. & Vaupel, J. W. The threshold age of the lifetable entropy. Demogr. Res. 41, 83–102. https://doi.org/10.4054/DemRes.2019.41.4 (2019).
Shkolnikov, V. M., Andreev, E. M., Zhang, Z., Oeppen, J. & Vaupel, J. W. Losses of expected lifetime in the United States and other developed countries: Methods and empirical analyses. Demography 48, 211–239. https://doi.org/10.1007/s13524-011-0015-6 (2011).
van Raalte, A. A. & Caswell, H. Perturbation analysis of indices of lifespan variability. Demography 50, 1615–1640. https://doi.org/10.1007/s13524-013-0223-3 (2013).
Hanada, K. A formula of Gini’s concentration ratio and its application to life tables. J. Japan Stat. Soc. 13, 95–98 (1983).
Shkolnikov, V. M., Andreev, E. E. & Begun, A. Z. Gini coefficient as a life table function: computation from discrete data, decomposition of differences and empirical examples. Demogr. Res. 8, 305–358. https://doi.org/10.4054/DemRes.2003.8.11 (2003).
Németh, L. Life expectancy versus lifespan inequality: A smudge or a clear relationship?. PLoS ONE 12, e0185702. https://doi.org/10.1371/journal.pone.0185702 (2017).
Fries, J. F., Bruce, B. & Chakravarty, E. Compression of morbidity 1980–2011: A focused review of paradigms and progress. J. Aging Res. 1–10, 2011. https://doi.org/10.4061/2011/261702 (2011).
Kannisto, V. Measuring the Compression of Mortality. Demogr. Res. 13. https://doi.org/10.4054/DemRes.2000.3.6 (2000).
Yadav, S. & Perianayagam, A. Mortality compression and variability in age at death in India. Compar. Popul. Stud. 45. https://doi.org/10.12765/CPoS-2020-20 (2020).
Shiels, M. S. et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: An analysis of death certificate data. Lancet 389, 1043–1054. https://doi.org/10.1016/S0140-6736(17)30187-3 (2017).
Case, A. & Deaton, A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. USA 112, 15078–15083. https://doi.org/10.1073/pnas.1518393112 (2015).
Avendano, M. & Kawachi, I. Why do Americans have shorter life expectancy and worse health than do people in other high-income countries?. Annu. Rev. Public Health 35, 307–325. https://doi.org/10.1146/annurev-publhealth-032013-182411 (2014).
Acciai, F. & Firebaugh, G. Twin consequences of rising U.S. death rates among young adults: Lower life expectancy and greater lifespan variability. Prev. Med. 127, 105793. https://doi.org/10.1016/j.ypmed.2019.105793 (2019).
Vaupel, J. W., Zhang, Z. & Raalte, A. A. V. Life expectancy and disparity: an international comparison of life table data. BMJ Open 1, 1–6 (2011).
Jha, P. Reliable direct measurement of causes of death in low- and middle-income countries. BMC Med. 12, 19. https://doi.org/10.1186/1741-7015-12-19 (2014).
Kumar, B. G. Low mortality and high morbidity in Kerala reconsidered. Popul. Dev. Rev. 19, 103–121 (1993).
Sole-Auro, A. & Alcaniz, M. Are we living longer but less healthy? Trends in mortality and morbidity in Catalonia (Spain), 1994–2011. Eur. J. Ageing 12, 61–70. https://doi.org/10.1007/s10433-014-0317-9 (2015).
Smits, J. & Monden, C. Length of life inequality around the globe. Soc. Sci. Med. 68, 1114–1123. https://doi.org/10.1016/j.socscimed.2008.12.034 (2009).
Clark, R. World health inequality: Convergence, divergence, and development. Soc. Sci. Med. 72, 617–624 (2011).
Claeson, C., Bos, E. R., Mawji, T. & Pathmanathan, I. Reducing child mortality in India in the new millennium. Bull. World Health Organ. 78, 1192–1199 (2000).
MoHFW (Ministry of Health and Family Welfare). Reproductive & Child Health Programme Phase II, 8th Joint Review Mission. (Ministry of Health and Family Welfare, New Delhi, 2011).
Arokiasamy, P. & Yadav, S. Changing age patterns of morbidity vis-à-vis mortality in India. J. Biosoc. Sci. 46, 462–479. https://doi.org/10.1017/S002193201300062X (2014).
Lee, R. D. Rethinking the evolutionary theory of aging: Transfers, not births, shape senescence in social species. Proc. Natl. Acad. Sci. 100, 9637–9642. https://doi.org/10.1073/pnas.1530303100 (2003).
Yadav, A., Yadav, S. & Kesarwani, R. Decelerating mortality rates in older ages and its prospects through Lee-Carter approach. PLoS ONE 7, 1. https://doi.org/10.1371/journal.pone.0050941 (2012).
India State-level Disease Burden Initiative Collaborators. Nations within a nation: Variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. The Lancet 390, 2437–2460. https://doi.org/10.1016/S0140-6736(17)32804-0 (2017).
Yadav, S., Kothavale, A., Yadav, P. K. & Yadav, N. in Collaborative Governance for Sustainable Development of Health and Well-Being: Issues and Perspective Vol. I Non-Communicable diseases (eds Harshad P. Thakur et al.) Ch. 7, 117–134 (2021).
Jagnoor, J. et al. Childhood and adult mortality from unintentional falls in India. Bull. World Health Organ. 89, 733–740. https://doi.org/10.2471/BLT.11.086306 (2011).
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. (Institute for Health Metrics and Evaluation (IHME), Seattle, United States of America, 2020).
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Cause List Mapped to ICD Codes., (Institute for Health Metrics and Evaluation (IHME), Seattle, United States of America, 2020).
Maher, C. & Ferreira, G. Time to reconsider what Global Burden of Disease studies really tell us about low back pain. Ann. Rheum. Dis. 81, 306–308. https://doi.org/10.1136/annrheumdis-2021-221173 (2022).
Voigt, K. & King, N. B. Out of alignment? Limitations of the global burden of disease in assessing the allocation of global health aid. Public Health Ethics 10, 244–256. https://doi.org/10.1093/phe/phx012 (2017).
Bhalla, K. & Harrison, J. E. GBD-2010 overestimates deaths from road injuries in OECD countries: New methods perform poorly. Int. J. Epidemiol. 44, 1648–1656. https://doi.org/10.1093/ije/dyv019 (2015).
Garcia-Basteiro, A. L., Brew, J., Williams, B., Borgdorff, M. & Cobelens, F. What is the true tuberculosis mortality burden? Differences in estimates by the World Health Organization and the Global Burden of Disease study. Int. J. Epidemiol. 47, 1549–1560. https://doi.org/10.1093/ije/dyy144 (2018).
Chiang, C. L. On constructing current life tables. J. Am. Stat. Assoc. 67, 538–541. https://doi.org/10.1080/01621459.1972.10481245 (1972).
Schoen, R. Calculating life tables by estimating Chiang’s a from observed rates. Demography 15, 625–635. https://doi.org/10.2307/2061212 (1978).
Wilmoth, J. R. & Horiuchi, S. Rectangularization revisited: Variability of age at death within human populations. Demography 36, 475–495. https://doi.org/10.2307/2648085 (1999).
Yadav, S., Yadav, P. K. & Yadav, N. Impact of COVID-19 on life expectancy at birth in India: A decomposition analysis. BMC Public Health 21, 1906. https://doi.org/10.1186/s12889-021-11690-z (2021).
Arriaga, E. E. Measuring and explaining the change in life expectancies. Demography 21, 83–96. https://doi.org/10.2307/2061029 (1984).
Kitagawa, E. M. Standardized comparisons in population research. Demography 1, 296–315 (1964).
Bergeron-Boucher, M., Ebeling, M. & Canudas-Romo, V. Decomposing changes in life expectancy: Compression versus shifting mortality. Demogr. Res. 33, 391–424. https://doi.org/10.4054/DemRes.2015.33.14 (2015).
Wagner, P. Sensitivity of life disparity with respect to changes in mortality rates. Demogr. Res. 23, 63–72. https://doi.org/10.4054/DemRes.2010.23.3 (2010).
ORGI (Office of the Registrar General & Census Commissioner, India). Sample registration system (SRS)-statistical report 2020. (MoHFW, GOI, New Delhi, 2020).
Jha, P. et al. HIV mortality and infection in India: estimates from nationally representative mortality survey of 1.1 million homes. BMJ 340, c621. https://doi.org/10.1136/bmj.c621 (2010).
Yadav, S. Progress of inequality in age at death in India: Role of adult mortality. Eur. J. Popul. 37, 523–550. https://doi.org/10.1007/s10680-021-09577-1 (2021).
Horiuchi, S. & Wilmoth, J. R. Deceleration in the age pattern of mortality at older ages. Demography 35, 391–412 (1998).
Klenk, J., Keil, U., Jaensch, A., Christiansen, M. C. & Nagel, G. Changes in life expectancy 1950–2010: contributions from age- and disease-specific mortality in selected countries. Popul Health Metr. 14, 20. https://doi.org/10.1186/s12963-016-0089-x (2016).
Beltran-Sanchez, H., Preston, S. H. & Canudas-Romo, V. An integrated approach to cause-of-death analysis: Cause-deleted life tables and decompositions of life expectancy. Demogr. Res. 19, 1323. https://doi.org/10.4054/DemRes.2008.19.35 (2008).
Sudharsanan, N., Aburto, J. M., Riffe, T. & van Raalte, A. Commentary: Large variation in the epidemiological transition across countries: Is it still valuable as a mortality theory?. Int. J. Epidemiol. https://doi.org/10.1093/ije/dyac107 (2022).
Yoshinaga, K. & Une, H. Contributions of mortality changes by age group and selected causes of death to the increase in Japanese life expectancy at birth from 1950 to 2000. Eur. J. Epidemiol. 20, 49–57. https://doi.org/10.1007/s10654-004-9557-x (2005).
Zarulli, V., Kashnitsky, I. & Vaupel, J. W. Death rates at specific life stages mold the sex gap in life expectancy. Proc. Natl. Acad. Sci. USA 118, 1. https://doi.org/10.1073/pnas.2010588118 (2021).
Kochanek, K. D., Arias, E. & Bastian, B. A. The effect of changes in selected age-specific causes of death on non-Hispanic white life expectancy between 2000 and 2014. NCHS Data Brief 1, 1–8 (2016).
Yadav, S. & Arokiasamy, P. Understanding epidemiological transition in India. Glob. Health Action 7, 23248. https://doi.org/10.3402/gha.v7.23248 (2014).
Rajaratnam, J. K. et al. Worldwide mortality in men and women aged 15–59 years from 1970 to 2010: A systematic analysis. Lancet 375, 1704–1720 (2010).
MoHFW (Ministry of Health and Family Welfare). National Multisectoral Action Plan for Prevention and Control of Common Noncommunicable Diseases (2017–2022). (MoHFW, GOI, New Delhi, 2017).
MoHFW (Ministry of Health and Family Welfare). Update on National Programme for Health Care of Elderly. (MoHFW, New Delhi, 2022).
MoHFW (Ministry of Health and Family Welfare). National programme for prevention and control of cancer, diabetes, cardiovascular diseases & stroke (NPCDCS). (MoHFW, New Delhi, 2013).
King, C. H. & Bertino, A. M. Asymmetries of poverty: Why global burden of disease valuations underestimate the burden of neglected tropical diseases. PLoS Negl. Trop. Dis. 2, e209. https://doi.org/10.1371/journal.pntd.0000209 (2008).
Seligman, B. J., Cullen, M. R. & Horwitz, R. I. Aging, transition, and estimating the global burden of disease. PLoS ONE 6, e20264. https://doi.org/10.1371/journal.pone.0020264 (2011).
Acknowledgements
The authors would like to thank the anonymous reviewers for their comments and suggestion.
Author information
Authors and Affiliations
Contributions
S.Y., A.P. conceptualised the study, S.Y. conducted the analyses, S.Y. prepared tables and figures, and S.Y. wrote the first draft manuscript. S.Y., A.P., S.A.P., and S.A.C. revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yadav, S., Perianayagam, A., Patel, S.A. et al. The role of age inequalities in cause of death in the slow pace of epidemiological transition in India. Sci Rep 12, 20291 (2022). https://doi.org/10.1038/s41598-022-23599-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-23599-7
This article is cited by
-
Subnational estimates of life expectancy at birth in India: evidence from NFHS and SRS data
BMC Public Health (2024)
-
Impact of COVID-19 on subnational variations in life expectancy and life disparity at birth in India: evidence from NFHS and SRS data
Archives of Public Health (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.