Abstract
Increased intra-individual variability of a variety of biomarkers is generally associated with poor health and reflects physiological dysregulation. Correlations among these biomarker variabilities should then represent interactions among heterogeneous biomarker regulatory systems. Herein, in an attempt to elucidate the network structure of physiological systems, we probed the inter-variability correlations of 22 biomarkers. Time series data on 19 blood-based and 3 hemodynamic biomarkers were collected over a one-year period for 334 hemodialysis patients, and their variabilities were evaluated by coefficients of variation. The network diagram exhibited six clusters in the physiological systems, corresponding to the regulatory domains for metabolism, inflammation, circulation, liver, salt, and protein. These domains were captured as latent factors in exploratory and confirmatory factor analyses (CFA). The 6-factor CFA model indicates that dysregulation in each of the domains manifests itself as increased variability in a specific set of biomarkers. Comparison of a diabetic and non-diabetic group within the cohort by multi-group CFA revealed that the diabetic cohort showed reduced capacities in the metabolism and salt domains and higher variabilities of the biomarkers belonging to these domains. The variability-based network analysis visualizes the concept of homeostasis and could be a valuable tool for exploring both healthy and pathological conditions.
Similar content being viewed by others
Introduction
In patients undergoing maintenance hemodialysis (HD) therapy, multiple blood tests are performed on a regular basis to ensure proper management of the patient's physical condition. We have been exploring the implications of intra-individual variabilities in time series data obtained from these patients. For many of the blood biomarkers examined, their variability increased with advancing age, and became accelerated synchronously prior to death1,2. Such biomarker variability is often associated with mortality and indicators of ill health3. Furthermore, a cumulative index of biomarker variabilities, as estimated by principal component analysis, has been reported to show consistent association with almost all known poor prognostic factors, and is a reliable predictor of frailty and mortality2,4. These observations can be reasonably explained by assuming that increased variability in each biomarker represents deterioration of the respective regulatory system, or “dysregulation”. With this reasoning, correlations among the variabilities for different biomarkers would represent a proximity of their regulatory mechanisms. Such inter-variability correlations were found positive for all pairwise combinations of biomarkers, indicating that the regulation of each biomarker cooperates with each other to maintain biological homeostasis2,3,4. Accordingly, we considered that by using the correlations among the variabilities for a sufficient number of biomarkers, it should be possible to get a holistic view of the physiological system.
Similar relationships between intra-individual variability and poor health have also been shown for biological parameters other than blood-based biomarkers. For example, variability in blood pressure (BP)5,6, heart rate (HR)7, gait8,9,10, body temperature11, emotion12, and sleep13 have been reported to be associated with adverse outcomes. Therefore, whatever the type of biomarker, intra-individual variability may represent its dysregulation.
In this study, we attempted to elucidate the network structure of the physiological systems from the correlations of their biomarker variabilities and examined the impact of underlying pathologies on such variabilities. In that case, incorporating more biomarkers would capture a wider range of the original physiological systems. Accordingly, in addition to the 19 blood biomarkers which we assessed in our previous investigation to estimate the overall physiological dysregulation4, three hemodynamic biomarkers: systolic BP (SBP), diastolic BP (DBP), and pulse rate (PR) were newly incorporated into this analysis.
Our objectives were (1) to examine whether variabilities of the BP/PR have comparable properties as other biomarker variabilities and can be treated in the same way; (2) to visualize the physiological network based on multiple biomarker variabilities; and (3) to identify diabetes-specific dysregulations using network analysis.
Methods
Patients
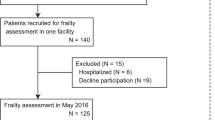
A total of 359 patients underwent maintenance HD throughout the one-year data collection period (January 1, 2020, to December 31, 2020) at one of the two participating HD facilities in Saitama-City, Japan. Among them, 341 patients had received more than 100 dialysis treatments and undergone more than 21 of the 24 scheduled blood tests during the aforementioned period. To reduce the impact of the potentially higher variabilities of biomarkers during the HD initiation phase1, 7 patients who had been on HD treatment for less than 6 months at the beginning of the data collection period were excluded, and the remaining 334 patients were enrolled in the study. Their age, sex, HD vintage, and body mass index were retrieved from their medical records, and subjects who were receiving antidiabetic drug treatment or having their glycated albumin (GA) levels measured regularly were classified as diabetic, regardless of their GA levels.
This retrospective observational study was conducted with the approval of the institutional ethics committee of Hakuyukai Medical Corporation (approval number: 03-002), in accordance with the principles of the Declaration of Helsinki. All of the patients, who were undergoing HD treatment at the participating facilities in 2020, provided informed consent for use of the clinical records.
Hemodynamic biomarkers
During each HD session, the SBP, DBP, and PR were measured intermittently using an automatic oscillometric BP monitor built into the dialysis machine, and their records were stored on a connected server computer through a HD management software. The measurements were taken in the sitting or supine position, depending on the patient. The median number of pre-dialysis measurements per patient during the year was 147 (interquartile range: 118–156). The SBP, DBP and PR for each patient were aggregated either monthly or yearly, and their mean levels were abbreviated as SBP-M, DBP-M, and PR-M, respectively. Their variabilities were evaluated as log 10-transformed coefficients of variation (CV = population standard deviation/mean), which were abbreviated as SBP-LCV, DBP-LCV, and PR-LCV, respectively4.
Blood biomarkers
At the participating HD facilities, 19 blood parameters were routinely measured in all the HD patients according to the same protocol. Measurements of the white blood cell (WBC), hemoglobin (Hb), platelet (Plat), albumin (Alb), blood urea nitrogen (BUN), creatinine (Cr), potassium (K), uncorrected calcium (Ca), and phosphate (P) were performed twice a month, and those of the total protein (TP), uric acid (UA), sodium (Na), and chloride (Cl) were measured once a month. In addition, the serum levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), lactate dehydrogenase (LDH), alkaline phosphatase (ALP), LDL cholesterol (LDL), and HDL cholesterol (HDL) were measured every two months. For diabetic patients, glycated albumin (GA) measurements were undertaken monthly based on the recommendations of the Japanese Society for Dialysis Therapy14. The blood samples were taken before the first HD session of the week and analyzed by a single outside laboratory. As with hemodynamic biomarkers, the mean value (M) and variability (LCV) of blood biomarker X were calculated from 1-year data for individual patients and were abbreviated as X-M and X-LCV, respectively. There were no missing M and LCV values for all biomarkers studied in the enrolled patients.
Statistical analysis
All the statistical analyses were performed in R.3.5.0 (R Core Team, 2018) using the corrplot, gplots, lavaan, psych, qgraph, semPlot, and semTools packages. The results were expressed as the means ± SD, and P value of < 0.05 were considered as being indicative of statistical significance. Bivariate correlations between continuous variables in the study items (demographic variables, biomarker levels, and biomarker variability) were assessed by calculating the Pearson or Spearman correlation coefficients according to the distribution of the variables. For combinations containing binary variables, point-biserial correlation coefficients were calculated. The P-values were determined by the Welch t-test, Mann–Whitney u-test, or Fisher’s exact test, as appropriate. In the determinations of the correlations among the LCVs, the P-values were not adjusted for multiple comparisons since it is evident that almost all the LCVs are correlated with each other and multiple comparison adjustments are only appropriate when there is a risk of overinterpreting a single false positive among many negatives4.
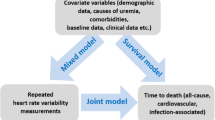
The overall relationship among the biomarker variabilities (LCVs) was assessed from their correlation matrix and visualized as a 2-dimensional diagram based on the Fruchterman–Reingold algorithm15. It was further assessed by exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). Because the LCVs do not fully satisfy multivariate normality, the CFA was performed with a robust maximum likelihood estimator “MLR” in the lavaan package.
The goodness-of-fit of the factor analysis models was evaluated by determination of the Comparative Fit Index (CFI), Tucker–Lewis Index (TLI), Root Mean Square Error of Approximation (RMSEA) and other relevant parameters. CFI > 0.90 (0.95), TLI > 0.90 (0.95), and RMSEA < 0.08 (0.05) were considered as representing an acceptable (or good) fit of the model16,17.
For the two groups comprising the population, a multi-group CFA was applied to determine if the measurement models were comparable and if there were differences in the factor means. In this process, four CFA models with progressively stringent equality constraints (i.e., configural, metric, scalar, and strict invariance models) were compared using the changes in the goodness-of-fit indices18. If ΔCFI < − 0.01, ΔTLI < − 0.01, or ΔRMSEA > 0.015 was observed, the compared models were considered as not being equivalent19,20. In these estimates of model fit, the chi-square difference tests were also included, but were not applied because they were too sensitive to the sample size17,19,21.
Results
Patient characteristics
A total of 334 patients were enrolled in this study, and their characteristics and laboratory data are presented in Table 1. The mean patient age was 62.9 ± 11.9 years (range = 28.6–88.4 years), and most of the patients had a long HD vintage (interquartile range = 3.8–15.7 years). Of the 334 participants, 327 were scheduled to receive 3 HD sessions per week, and the remaining 7 were scheduled to receive 2 sessions per week. One hundred and forty-three of the participants had diabetes, of which only two had type 1 diabetes. Of the 22 LCVs examined, only the Na-LCV was rejected for a normal distribution by the Kolmogorov–Smirnov test.
Pre-dialysis blood pressure, pulse rate, and their variability
To confirm that our hemodynamic data were similar in characteristics to those previously reported, we first examined their seasonal variations. Each patient’s pre-dialysis SBP, DBP, and PR measurements were compiled on a monthly basis, and the seasonal differences were examined. As reported for HD patients22,23,24,25, the yearly mean SBP in this cohort was high (Table 1), and the monthly mean SBP and DBP were higher in winter and lower in summer (Fig. 1a). Comparison of the values for August and February, as representative values for the summer and winter months by the paired t-test showed a highly significant difference. (SBP-M: 153.6 ± 19.6 vs. 145.8 ± 20.3, P < 10–16; DBP-M: 82.1 ± 11.6 vs. 77.3 ± 5.9, P < 10–22). On the other hand, the monthly means of the PR for these months were 76.3 ± 10.8 and 75.9 ± 10.7, and the difference was not significant (P = 0.24).
Monthly mean levels and variability of the pre-dialysis blood pressure and pulse rate. SBP systolic blood pressure, DBP diastolic blood pressure, PR pulse rate. The monthly SBP, DBP, and PR measurements were compiled for each patient. The number of eligible patients per month was 331–334. Error bar represents the 95% confidence interval.
After confirming the seasonal trend of BP levels, we continued to examine the characteristics of BP variability. The monthly SBP/DBP variability did not show any clear seasonal changes (Fig. 1b). There was no significant difference in the values for February and August (SBP-LCV: − 1.11 ± 0.15 vs. − 1.10 ± 0.15, P = 0.21; DBP-LCV: − 1.10 ± 0.16 vs. − 1.10 ± 0.16, P = 0.96). The PR variability tended to be lower during the summer months, and the difference between the values for February and August was significant (− 1.21 ± 0.17 vs. − 1.24 ± 0.18, P = 0.008). The LCV values calculated from all the measurements during the one-year period are presented in Table 1.
Correlations among the biomarker variabilities
A total of 22 biomarkers, including 19 blood-based biomarkers and 3 hemodynamic biomarkers, were assessed in this study. Pair-wise correlations among the demographic variables, mean levels of the biomarkers (Ms), and their variabilities (LCVs) were computed, and the entire correlation matrix (52 × 52) is provided as Supplementary Table S1. It is also presented as a heatmap in Fig. 2a. As shown in both the table and figure, the 231 correlation coefficients for the possible pair-wise combinations of the 22 biomarker LCVs were all positive, with one exception (r = − 0.028 between UA-LCV and DBP-LCV, P = 0.611). Although the correlations were weak for many combinations, they were significant for 209 of them (90.5%).
Correlations among the demographic parameters, biomarker levels, and their variabilities. (a) The correlation matrix in Supplementary Table S1 is shown as a heatmap. The sign and strength of the correlation coefficient are displayed by the color and its density, respectively. HD hemodialysis, DM diabetes mellitus, BMI body mass index. (b) Distribution of the 231 correlation coefficients among the biomarker LCVs is represented as a histogram. Among them, biomarker pairs including at least one hemodynamic biomarker are shown in green.
Comparison of the correlation coefficients between the two groups of combinations (Fig. 2b), one consisting of only blood biomarkers (171 correlations) and the other including at least one hemodynamic biomarker (60 correlations), revealed generally lower coefficients in the latter group. However, even in the latter group, the correlations were still significant for 49 combinations (81.7%).
In addition, examining the relationship between hemodynamic biomarker variabilities and blood biomarker levels (Supplementary Table S1) revealed that a higher SBP/DBP variability was associated with lower serum levels of Alb, BUN, Cr, and Ca, and higher serum levels of ALP. Such correlations with prognosis-related factors were also observed for many blood biomarker variabilities. These results lend support to the notion that hemodynamic biomarker variabilities are similar in characteristics to blood biomarker variabilities, and that both represent dysregulation.
Network structure of physiological regulation
Based on the idea that correlations between variabilities in biomarker pairs signify proximity of the two biomarker regulatory systems, we estimated the structure of the physiological network from the correlation matrix of the 22 LCVs. In the network diagram (Fig. 3a), each node originally represents a biomarker dysregulation, but can also be viewed as the biomarker-specific regulatory system itself because the edge connecting 2 nodes designates the proximity of their regulatory systems. These nodes (22 LCVs) formed 5 to 6 clusters, which can be regarded as sub-systems26, domains27,28, or modules29 within the overall physiological system. Because many centrality measures showed very similar patterns for this network, only their representative plots are presented. As depicted in Fig. 3b, BUN-LCV, followed by Alb-LCV, Cr-LCV and K-LCV show high centrality values, suggesting that these regulatory systems may act as the hubs of the physiological network.
Network structure of physiological regulation. (a) The structure of the regulatory systems involving the 22 biomarkers can be visualized as a two-dimensional diagram. Each node labeled a X-LCV represents a regulatory system of biomarker X or its dysregulation. The thickness and relative length of the lines connecting the nodes express the strength of the correlation. Green color denotes a positive correlation. (b) Centrality plot for the network depicting the betweenness, closeness, and strength of each node.
Exploratory factor analyses
To describe the structure of the physiological network in quantitative terms, EFA was conducted for the 22 LCVs. As for the number of factors in the EFA, several estimation methods suggested numbers between 5 and 8. After a close examination of each EFA model with a different number of factors, we selected a six-factor model using maximum likelihood estimation and Oblimin rotation as the most appropriate one. The factor loadings of the model (Table 2) are consistent with the modular structure observed in Fig. 3a and can be visualized as shown in Supplementary Fig. S1. Both diagrams convinced us that the latent factors represent regulatory domains (or sub-systems) for metabolism, inflammation, circulation, liver, salt, and protein. The fit indices of the EFA model are good: χ2 (df) = 178.8 (114), χ2/df = 1.57; CFI = 0.971; TLI = 0.940; RMSEA = 0.041; Root Mean Square Residual (RMSR) = 0.030.
Confirmatory factor analysis
With reference to the EFA, we developed a simpler CFA model with 6 comparable latent factors and a few cross-loadings (Fig. 4). Except for the χ2 test, which is known to be sensitive to the number of samples, the model showed good fit with the alternative fit indices: χ2 (df) = 147.6 (87), P ≤ 0.001, χ2/df = 1.70; CFI = 0.966; TLI = 0.952; SRMR = 0.041; RMSEA = 0.046. The model indicates that the dysfunction of a postulated regulatory domain (= latent factor) increases the variability of a set of biomarkers belonging to it. On the basis of this CFA model, we also constructed second-order and bifactor CFA models (Supplementary Figs. S2 and S3). These additional CFA models showed comparable fit to that of the original CFA model.
Association of domain-specific dysregulation with clinical parameters
The regulatory capacity of each domain is expected to vary depending on the health status of the patient. Therefore, we estimated factor scores for the six domains and examined their association with various health indicators of the patients (Table 3). Regarding blood biomarkers, lower levels of Alb, BUN, Cr, Na, LDL and higher levels of AST and ALP are associated with dysregulation in most of the domains, while BMI and SBP levels show positive and negative associations that vary by domain. To compare mean factor scores across different groups, it is assumed that the relationship between latent factors and observed variables in each group is approximately equal, i.e., measurement invariance has been established. Therefore, the effects of gender and diabetes were further analyzed using multi-group CFA.
Comparison of diabetic and non-diabetic HD patients
In the multi-group CFA, the diabetic (n = 143) and non-diabetic (n = 191) groups were first analyzed separately using the constructed CFA model (Fig. 4). Then, four models with different equality constraints were compared to see if the measurement structures of the two groups could be considered to be identical (Table 4)19. In the increasingly restricted models, changes of the alternative fit indices (ΔCFI, ΔTLI, and ΔRMSEA) were all less than 0.01, and the strict invariance model had the lowest AIC/BIC values. This result justifies that the mean scores of the 6 factors can be compared for both groups in the strict invariance model, in which factor loadings, intercepts, and residual variances are constrained to be equal in the two groups. As shown in Table 5, the diabetic group showed significantly higher factor means for factor 1 (metabolism) and factor 4 (salt), indicating that both domains are more dysregulated in diabetic subjects as compared to non-diabetic subjects.
Comparison of female and male HD patients
A similar multi-group CFA was conducted between the male and female groups. In this grouping, scalar invariance, rather than strict invariance, was achieved (Table 4), and in the scalar invariance model, the mean factor scores for the six domains did not differ significantly between the gender groups (Table 5). Considering the potential confounding of diabetes and gender, we attempted a multigroup CFA with four groups combining both factors. However, due to the small sample size in each group resulting from the splitting, the analysis could not be completed30.
Discussion
In this study, we analyzed the multivariate structure of the biomarker variabilities in HD patients and obtained a number of novel findings. First, the hemodynamic biomarkers (BP and PR) showed similar patterns to those previously described for blood biomarkers: high variability was a sign of poor health and was correlated with the variabilities of other biomarkers. Second, network analysis showed a clear structure in how the biomarker variabilities correlated with, and presumably influenced, each other. Third, factor analysis identified six key axes of variability in the biomarkers and showed distinct variability profiles in diabetics and non-diabetics. While the overall variability likely remains important, variability in specific domains also appears to contain relevant biological information.
BP variability has been measured in several ways and is categorized into very short-term (beat-to-beat), short-term (along 24 h), mid-term (between days), and long-term (visit-to-visit) variability5,6. The BP variability in this study was calculated from all the pre-HD BP measurements made over a 1-year period, and thus can be considered as representing long-term BP variability.
With regard to long-term BP variability, its associations with all-cause and cardiovascular mortality are well documented in the general population5,6 as well as in the HD population31,32,33,34. Such BP variability has also been reported to be larger in the elderly35,36 especially those with frailty37,38, functional decline39, and cognitive impairment40.
In contrast to studies on the BP variability, research on HR variability initially focused on very short-term variability. Beat-to-beat HR variability is well known to be negatively associated with the cardiovascular morbidity, mortality, and aging41,42. On the other hand, recent studies have shown that long-term HR (or PR) variability is positively associated with all-cause mortality7,43,44 suggesting a distinct physiological significance of both types of variations. In any case, variabilities of these basic hemodynamic biomarkers measured at each visit are commonly associated with a poor health status.
Similar to the hemodynamic biomarkers, variabilities in a number of blood-based biomarkers have been shown to be associated with mortality, frailty, and multiple adverse health indicators2,3,4,45. As shown in Fig. 2, the variability levels of the biomarkers are widely cross-correlated, regardless of which biomarker type they belong to. Therefore, all of the biomarker variabilities determined over this timescale seemed to consistently represent physiological dysregulation.
Homeostasis is an essential physiological function for organisms to adapt to environmental changes and adverse stresses, and is sustained by numerous regulatory mechanisms that exist at multiple levels (from molecules to cells, organs, and the body). These regulatory mechanisms are interlinked within cells, between cells, and between organs, and dysregulation of one mechanism can affect the regulation of others through their interactions29. Frailty is now recognized as a multi-system physiological dysregulation resulting from such process46,47,48.
To understand the complex interactions within the physiological system, several studies have conducted network analysis using relationship among individual regulatory systems49. As a measure of relationship, some studies have employed temporal linkage between different physiological signals50,51, while others have used associations among variables representing dysregulation or pathological states52,53,54. In the latter cases, physiologic dysregulation is often assessed by biomarker levels. However, the relationship between biomarker levels and mortality risk can be U-shaped and, moreover, varies depending on the individual's physical condition. In the general population, hypertension, obesity, and hypercholesterolemia increase the mortality risk, but this relationship is known to be reversed in patients with comorbidities such as end stage renal disease and heart failure and in the very elderly (reverse epidemiology)55,56,57. Therefore, assessment of dysregulation by biomarker levels is not straightforward. In this study, we employed biomarker variabilities (LCVs) as measures of dysregulation, which are largely normally distributed and have been reported to be monotonically related to health indicators such as mortality and frailty2,3,45. The resulting network diagram, built solely on LCVs, is consistent with our prior knowledge about the regulatory systems, which supports the validity of the LCV-based analysis.
Our CFA model demonstrates the modular structure of the physiological network29, in which 6 latent factors are positively correlated with each other (Fig. 4). In the second-order CFA models (Supplementary Fig. S2), these inter-factor correlations are replaced by a higher-order factor, representing the view that systemic dysregulation manifests itself through dysregulation in individual domains. On the other hand, the bifactor CFA model (Supplementary Fig. S3) presents the view that there is a general dysregulation that is independent of dysregulation in individual domains. The comparable fit of these models indicates that the physiological system can be viewed in more than one way and understood as consisting of both general and domain-specific regulation. Such general regulation could be referred to as “allostatic load”58, “health status”52, or “multisystemic (dys)regulation”59.
Subsequent multi-group CFA demonstrated that diabetic patients have greater functional impairment than non-diabetic patients in 2 physiological domains, namely, metabolism and salt. In agreement with the factor structure of the model, the diabetic patients showed higher variabilities of K, Cr, BUN, Na, and Cl (see Supplementary Table S1). Our previous studies, which used datasets from different years (specifically 2002 and 2015–16), also showed similar correlation patterns among blood biomarkers, with higher variability in the same set of biomarkers in the diabetic group3,4. These observations on prevalent HD patients suggest that the increased dysregulation in diabetic patients is neither limited to glucose metabolism nor is global, but is related to specific physiological domains.
It has been reported that the levels of various metabolites (lipids, amino acids, glycogen, thiamine, etc.) in organs and blood are altered in patients with type 2 diabetes (T2D), depending on their stage61,62. While it has been argued that the early changes may be related to insulin resistance, the specific mechanism remains unknown. The domain we have named metabolism is associated with the regulation of BUN, Cr, P, and UA, suggesting that diabetic HD patients, probably in the late stages of diabetes, have abnormalities in the metabolism of nitrogen-containing compounds such as amino acids. In addition, T2D patients are known to be predisposed to sodium retention from the early stages of the disease63. It has been thought that hyperglycemia and the associated diuresis, glucosuria, and hyperinsulinemia cause upregulation of renal glucose transporters and sodium channels, leading to increased renal sodium reabsorption64,65. On the other hand, recent studies using 23Na magnetic resonance imaging have reported that sodium can be stored in the skin in an osmotically inactive form and that this dermal Na-binding capacity is reduced in T2D patients60,66. Our results indicate that in dialysis patients who have already lost renal function, diabetic patients are still more impaired in sodium regulation than non-diabetic patients. In the diabetic HD patients, GA levels do not appear to be associated with dysregulation in any of the domains (Table 3), making it unlikely that hyperglycemia itself is causing sodium dysregulation. In this regard, the decreased dermal sodium-binding capacity seems to be one plausible cause of this dysregulation64.
There are several potential limitations to this study. First, although the biomarkers examined in this study are not few, they are far from exhaustive, and the inferred network may only be a part of the real system. As mentioned in the introduction section, if time-series data on other biomarkers, such as gait, sleep, etc., were also available, a more comprehensive physiological network could be constructed. Second, as this study showed, the average BP levels vary seasonally23, and the blood parameter levels are also known to have seasonal variations67,68. This seasonality may affect the assessment of the variability. It is, however, difficult to extract a seasonal factor from each individual's data. A much larger cohort would be needed for a more refined analysis that takes seasonal factors into account. Third, we performed a multi-group CFA to examine the effects of diabetes and gender on physiological regulatory systems. However, the large sample size required for a multi-group analysis did not allow for a detailed analysis of the interaction of background factors. A larger cohort needs to be prepared for further analysis. Forth, the results obtained in this study are based on data from HD patients in a specific geographic area. To generalize our findings, it would be necessary to confirm them in a separate cohort. The last point that should be mentioned is a problem common to most statistical inferences based on population data. Most statistical studies using aggregate data have been conducted under the assumption that the relationships among observables are approximately the same in each individual of the population (local homogeneity or ergodicity)59,69,70. The present study has also estimated individual physiological structures based on statistical inferences derived from inter-individual correlations. However, this generalization from population to individual is not necessarily valid71. To strengthen our results, it is necessary to develop a method that can analyze physiological systems on an individual basis.
While the dynamics of various biomarkers have mostly been analyzed separately, it is now clear that they are interrelated. We have shown that the widespread correlations among the biomarker variabilities reflects mutual linkages of the regulatory systems in the body. Network analysis of multifarious biomarker variabilities could be a strong tool for exploring normal and pathological processes in physiological systems.
Data availability
All processed data generated in this study are included in this publication and its Supplementary Information, but the raw data cannot be made openly available to protect the confidentiality of personal information and to comply with the terms of patient consent. Requests related to the raw data should be addressed to the corresponding author.
References
Nakazato, Y., Kurane, R., Hirose, S., Watanabe, A. & Shimoyama, H. Aging and death-associated changes in serum albumin variability over the course of chronic hemodialysis treatment. PLoS One 12, e0185216 (2017).
Cohen, A. A. et al. Synchrony of biomarker variability indicates a critical transition: Application to mortality prediction in hemodialysis. iScience 25, 104385 (2022).
Nakazato, Y., Kurane, R., Hirose, S., Watanabe, A. & Shimoyama, H. Variability of laboratory parameters is associated with frailty markers and predicts non-cardiac mortality in hemodialysis patients. Clin. Exp. Nephrol. 19, 1165–1178 (2015).
Nakazato, Y. et al. Estimation of homeostatic dysregulation and frailty using biomarker variability: A principal component analysis of hemodialysis patients. Sci. Rep. 10, 10314 (2020).
Parati, G., Stergiou, G. S., Dolan, E. & Bilo, G. Blood pressure variability: Clinical relevance and application. J. Clin. Hypertens. 20, 1133–1137 (2018).
Stevens, S. L. et al. Blood pressure variability and cardiovascular disease: Systematic review and meta-analysis. BMJ (Online) 354, i4098 (2016).
Yang, X. et al. The link between elevated long-term resting heart rate and SBP variability for all-cause mortality. J. Hypertens. 37, 84–91 (2019).
Miyazaki, T. et al. Relationships between gait regularity and cognitive function, including cognitive domains and mild cognitive impairment, in community-dwelling older people. Healthc. 9, 1571 (2021).
Byun, S. et al. Gait variability can predict the risk of cognitive decline in cognitively normal older people. Dement. Geriatr. Cogn. Disord. 45, 251–261 (2018).
Montero-Odasso, M. et al. Gait variability is associated with frailty in community-dwelling older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 66A, 568–576 (2011).
Amiya, E. et al. Differences in body temperature variability between subjects with and without diabetes and predictive value for cardiovascular events. Circ. J. 77, 1844–1853 (2013).
Ong, A. D. & Steptoe, A. Association of positive affect instability with all-cause mortality in older adults in England. JAMA Netw. Open 3, e207725 (2020).
Bei, B., Wiley, J. F., Trinder, J. & Manber, R. Beyond the mean: A systematic review on the correlates of daily intraindividual variability of sleep/wake patterns. Sleep Med. Rev. 28, 108–124 (2016).
Nakao, T. et al. Best practice for diabetic patients on hemodialysis 2012. Ther. Apher. Dial. 19, 40–66 (2015).
Fruchterman, T. M. J. & Reingold, E. M. Graph drawing by force-directed placement. Softw. Pract. Exp. 21, 1129–1164 (1991).
Browne, M. W. & Cudeck, R. Alternative ways of assessing model fit. Sociol. Methods Res. 21, 230–258 (1992).
Hu, L. T. & Bentler, P. M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 6, 1–55 (1999).
Fischer, R. & Karl, J. A. A primer to (cross-cultural) multi-group invariance testing possibilities in R. Front. Psychol. 10, (2019).
Cheung, G. W. & Rensvold, R. B. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Model. A Multidiscip. J. 9, 233–255 (2002).
Chen, F. F. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Model. A Multidiscip. J. 14, 464–504 (2007).
Putnick, D. L. & Bornstein, M. H. Measurement invariance conventions and reporting: The state of the art and future directions for psychological research. Dev. Rev. 41, 71–90 (2016).
Wu, Z. et al. Seasonal variation: A non-negligible factor associated with blood pressure in patients undergoing hemodialysis. Front. Cardiovasc. Med. 9, (2022).
Argilés, À., Mourad, G. & Mion, C. Seasonal changes in blood pressure in patients with end-stage renal disease treated with hemodialysis. N. Engl. J. Med. 339, 1364–1370 (1998).
Agarwal, R. et al. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am. J. Med. 115, 291–297 (2003).
Cheung, A. K. et al. Seasonal variations in clinical and laboratory variables among chronic hemodialysis patients. J. Am. Soc. Nephrol. 13, 2345–2352 (2002).
Lehnertz, K., Bröhl, T. & Rings, T. The human organism as an integrated interaction network: Recent conceptual and methodological challenges. Front. Physiol. 11, 598694 (2020).
Sharma, A. et al. A network analysis to compare biomarker profiles in patients with and without diabetes mellitus in acute heart failure. Eur. J. Heart Fail. 19, 1310–1320 (2017).
Lu, Y. et al. Physiological dysregulation, frailty, and impacts on adverse health and functional outcomes. Front. Med. 8, 751022 (2021).
Cho, D.-Y., Kim, Y.-A. & Przytycka, T. M. Chapter 5: Network biology approach to complex diseases. PLoS Comput. Biol. 8, e1002820 (2012).
Kyriazos, T. A. Applied psychometrics: Sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology 09, 2207–2230 (2018).
Tozawa, M., Iseki, K., Yoshi, S. & Fukiyama, K. Blood pressure variability as an adverse prognostic risk factor in end-stage renal disease. Nephrol. Dial. Transplant. 14, 1976–1981 (1999).
Wang, Y. et al. Cycles, arrows and turbulence: Time patterns in renal disease, a path from epidemiology to personalized medicine?. Blood Purif. 47, 1–14 (2018).
Shafi, T. et al. Predialysis systolic BP variability and outcomes in hemodialysis patients. J. Am. Soc. Nephrol. 25, 799–809 (2014).
Brunelli, S. M. et al. Association between long-term blood pressure variability and mortality among incident hemodialysis patients. Am. J. Kidney Dis. 52, 716–726 (2008).
Muntner, P. et al. The relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population: Findings from NHANES III, 1988 to 1994. Hypertension 57, 160–166 (2011).
Zhou, J. et al. Gender- and age-specific associations of visit-to-visit blood pressure variability with anxiety. Front. Cardiovasc. Med. 8, (2021).
Woo, J., Yu, R., Tsoi, K. & Meng, H. Variability in repeated blood pressure measurements as a marker of frailty. J. Nutr. Health. Aging 22, 1122–1127 (2018).
Rouch, L. et al. Visit-to-visit blood pressure variability and incident frailty in older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 76, 1369–1375 (2021).
Ogliari, G. et al. Visit-to-visit blood pressure variability and future functional decline in old age. J. Hypertens. 34, 1544–1550 (2016).
de Heus, R. A. A. et al. Association between blood pressure variability with dementia and cognitive impairment: A systematic review and meta-analysis. Hypertension 78, 1478–1489 (2021).
Tsuji, H. et al. Reduced heart rate variability and mortality risk in an elderly cohort: The Framingham heart study. Circulation 90, 878–883 (1994).
Lipsitz, L. A., Mietus, J., Moody, G. B. & Goldberger, A. L. Spectral characteristics of heart rate variability before and during postural tilt. Relations to aging and risk of syncope. Circulation 81, 1803–1810 (1990).
Wang, G., Li, Y. & Zou, X. Several Indicators of critical transitions for complex diseases based on stochastic analysis. Comput. Math. Methods Med. 2017, 7560758 (2017).
Zhao, M. X. et al. Effect of resting heart rate on the risk of all-cause death in Chinese patients with hypertension: Analysis of the Kailuan follow-up study. BMJ Open 10, e032699 (2020).
Segar, M. W. et al. Association of visit-to-visit variability in kidney function and serum electrolyte indexes with risk of adverse clinical outcomes among patients with heart failure with preserved ejection fraction. JAMA Cardiol. 6, 68–77 (2021).
Varadhan, R., Walston, J. D. J. D. & Bandeen-Roche, K. Can a link be found between physical resilience and frailty in older adults by studying dynamical systems?. J. Am. Geriatr. Soc. 66, 1455–1458 (2018).
Li, Q. et al. Homeostatic dysregulation proceeds in parallel in multiple physiological systems. Aging Cell 14, 1103–1112 (2015).
Ghachem, A. et al. Evidence from two cohorts for the frailty syndrome as an emergent state of parallel dysregulation in multiple physiological systems. Biogerontology 22, 63–79 (2021).
Ivanov, P. C. The new field of network physiology: Building the human physiolome. Front. Netw. Physiol. 1, 1 (2021).
Bashan, A., Bartsch, R. P., Kantelhardt, J. W., Havlin, S. & Ivanov, P. C. Network physiology reveals relations between network topology and physiological function. Nat. Commun. 3, 702 (2012).
Bartsch, R. P., Liu, K. K. L. L., Bashan, A. & Ivanov, P. C. Network physiology: How organ systems dynamically interact. PLoS One 10, e0142143 (2015).
Félix Caballero, F. et al. Advanced analytical methodologies for measuring healthy ageing and its determinants, using factor analysis and machine learning techniques: The ATHLOS project. Sci. Rep. 7, 43955 (2017).
Barajas-Martínez, A. et al. Metabolic physiological networks: The impact of age. Front. Physiol. 11, 587994 (2020).
Barajas-Martínez, A. et al. Physiological network from anthropometric and blood test biomarkers. Front. Physiol. 11, (2021).
Kalantar-Zadeh, K., Ikizler, T. A., Block, G., Avram, M. M. & Kopple, J. D. Malnutrition-inflammation complex syndrome in dialysis patients: Causes and consequences. Am. J. Kidney Dis. 42, 864–881 (2003).
Myasoedova, E. et al. Lipid paradox in rheumatoid arthritis: The impact of serum lipid measures and systemic inflammation on the risk of cardiovascular disease. Ann. Rheum. Dis. 70, 482–487 (2011).
Kalantar-Zadeh, K., Block, G., Horwich, T. & Fonarow, G. C. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J. Am. Coll. Cardiol. 43, 1439–1444 (2004).
Wiley, J. F., Gruenewald, T. L., Karlamangla, A. S. & Seeman, T. E. Modeling multisystem physiological dysregulation. Psychosom. Med. 78, 290–301 (2016).
Gross, A. L. et al. Derivation of a measure of physiological multisystem dysregulation: Results from WHAS and health ABC. Mech. Ageing Dev. 188, 111258 (2020).
Hanson, P. et al. Sodium in the dermis colocates to glycosaminoglycan scaffold, with diminishment in type 2 diabetes mellitus. JCI Insight 6, e145470 (2021).
Diamanti, K. et al. Organ-specific metabolic pathways distinguish prediabetes, type 2 diabetes, and normal tissues. Cell Rep. Med. 3, 100763 (2022).
Sanches, J. M., Zhao, L. N., Salehi, A., Wollheim, C. B. & Kaldis, P. Pathophysiology of type 2 diabetes and the impact of altered metabolic interorgan crosstalk. FEBS J. https://doi.org/10.1111/febs.16306 (2021).
Weder, A. B. Sodium metabolism, hypertension, and diabetes. Am. J. Med. Sci. 307, S53–S59 (1994).
Hanson, P. et al. Novel perspectives of sodium handling in type 2 diabetes mellitus. Expert Rev. Endocrinol. Metab. 17, 333–341 (2022).
Zhao, Y. et al. Sodium intake regulates glucose homeostasis through the PPARδ/adiponectin-mediated SGLT2 pathway. Cell Metab. 23, 699–711 (2016).
Kopp, C. et al. Elevated tissue sodium deposition in patients with type 2 diabetes on hemodialysis detected by 23Na magnetic resonance imaging. Kidney Int. 93, 1191–1197 (2018).
Kooman, J. P. et al. ‘Time and time again’: Oscillatory and longitudinal time patterns in dialysis patients. Kidney Blood Press. Res. 35, 534–548 (2012).
Broers, N. J. H. et al. Season affects body composition and estimation of fluid overload in haemodialysis patients: variations in body composition; A survey from the European MONDO database. Nephrol. Dial. Transplant 30, 676–681 (2015).
Molenaar, P. C. M. A manifesto on psychology as idiographic science: bringing the person back into scientific psychology, this time forever. Meas. Interdiscip. Res. Perspect. 2, 201–218 (2004).
Adolf, J., Schuurman, N. K., Borkenau, P., Borsboom, D. & Dolan, C. V. Measurement invariance within and between individuals: A distinct problem in testing the equivalence of intra- and inter-individual model structures. Front. Psychol. 5, 1–14 (2014).
Fisher, A. J., Medaglia, J. D. & Jeronimus, B. F. Lack of group-to-individual generalizability is a threat to human subjects research. Proc. Natl. Acad. Sci. U. S. A. 115, E6106–E6115 (2018).
Acknowledgements
We thank Mr. Hitoshi Sugihara for his technical assistance in extracting data from electronic recording system. AAC is supported by a Fonds de Recherche du Québec—Santé Senior Salary Award and is a member of the FRQ-S funded Centre de recherche du CHUS and Centre de recherche sur le vieillissement.
Author information
Authors and Affiliations
Contributions
Y.N. designed and performed statistical analyses. M.S. and H.S. were involved blood pressure data acquisition. A.W., H.K., and Hf.S. organized the database and contributed to data interpretation. A.A.C. and Y.N. contributed to the interpretation of the results and preparation of the manuscript. All authors critically reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
A.A.C. is founder and CEO at Oken Health, and all the other authors declared no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakazato, Y., Shimoyama, M., Cohen, A.A. et al. Intercorrelated variability in blood and hemodynamic biomarkers reveals physiological network in hemodialysis patients. Sci Rep 13, 1660 (2023). https://doi.org/10.1038/s41598-023-28345-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-28345-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.