Abstract
Development of an effective therapy to overcome colistin resistance in Klebsiella pneumoniae, a common pathogen causing catheter-related biofilm infections in vascular catheters, has become a serious therapeutic challenge that must be addressed urgently. Although colistin and EDTA have successful roles for eradicating biofilms, no in vitro and in vivo studies have investigated their efficacy in catheter-related biofilm infections of colistin-resistant K. pneumoniae. In this study, colistin resistance was significantly reversed in both planktonic and mature biofilms of colistin-resistant K. pneumoniae by a combination of colistin (0.25–1 µg/ml) with EDTA (12 mg/ml). This novel colistin-EDTA combination was also demonstrated to have potent efficacy in eradicating colistin-resistant K. pneumoniae catheter-related biofilm infections, and eliminating the risk of recurrence in vivo. Furthermore, this study revealed significant therapeutic efficacy of colistin-EDTA combination in reducing bacterial load in internal organs, lowering serum creatinine, and protecting treated mice from mortality. Altered in vivo expression of different virulence genes indicate bacterial adaptive responses to survive in hostile environments under different treatments. According to these data discovered in this study, a novel colistin-EDTA combination provides favorable efficacy and safety for successful eradication of colistin-resistant K. pneumonia catheter-related biofilm infections.
Similar content being viewed by others
Introduction
K. pneumoniae is one of the most prevalent Gram-negative pathogens involved in bacterial colonization and catheter-related biofilm infections which are typical consequences that frequently arise in vascular catheters1,2 Bacterial colonization of vascular catheters occurs frequently within 24 h of use and the severity of catheter-related biofilm infections are significantly correlated to the duration of catheterization2. Nowadays, occurrence of catheter-related biofilm infections by multidrug-resistant K. pneumoniae is increasing3, posing a significant challenge in selecting appropriate treatment. Because of rising antibiotic resistance and biofilm tolerance to both antimicrobial and host immunological responses1, clinicians are confronted with higher mortality rates1, especially in critically ill patients.
Adding to the urgency of the problem, colistin-resistant K. pneumoniae infections are increasing in intensive care units, especially in patients who ultimately depend on vascular catheters for short-term (< 10 days) or long-term (≥ 30 days) use, depending on their requirements4,5. These catheters are frequently colonised by biofilms which act as a potential source of bloodstream infections during the critical phases when treatment options are limited1. In most cases, surgical removal is required, however obtaining alternate venous access for catheter replacement is problematic6. Moreover, replacing infected catheters carries the risk of traumatic injuries, limited catheter access, and increased treatment costs6. Currently, the antibiotic lock technique can be attempted to control these complications7. This procedure targets intraluminal biofilms lining the lumen of the infected catheters through the instillation of a solution containing a high concentration of single or combined antimicrobial agents7. Increasing concerns about multi-resistant infections have prompted the evaluation of novel lock solutions that combine different antibiotics or nonantibiotic compounds7,8. Ethylenediaminetetraacetic acid (EDTA) is an FDA-approved metal ions chelator with a favorable pharmacokinetic safety profile for intravenous treatment of lead poisoning9. EDTA increases outer membrane permeabilization with the release of LPS and augments antibiotic activity by facilitating antibiotic penetration to reach their targets9.
EDTA also exhibits antibiofilm activity by disrupting the biofilm matrix via strong metal ions chelation activities9. According to previous studies, EDTA increased the effectiveness of existing antibiotics for eradicating Gram-negative bacteria mature biofilms10,11,12,13. It has preferable bactericidal activities against inner biofilm cells with lower metabolic activities14. As colistin monotherapy was unable to eradicate mature biofilms in bacterial infections15, we hypothesized that it would be interesting to combine colistin with EDTA, to augment colistin activity, and make it re-effective against resistant pathogens, at lower dosages.
To the best of our knowledge, no study has been conducted to evaluate the activities of novel colistin-EDTA combination on colistin-resistant K. pneumoniae. The primary objective of this study was to investigate the effectiveness of novel colistin-EDTA combination in catheter-related biofilm infections of colistin-resistant K. pneumoniae both in vitro and in vivo.
Results
Colistin-EDTA combination displays synergistic activity against colistin-resistant K. pneumoniae clinical isolates
All colistin-resistant K. pneumoniae clinical isolates had no visible signs of growth in the presence of 3–24 mg/ml EDTA (Table 1). Combination of colistin (0.25 µg/ml) with EDTA (12 mg/ml) exhibited potent synergistic activity (FICI ≤ 0.5) against all planktonic colistin-resistant K. pneumoniae isolates (Table 1). Compared to colistin and EDTA alone, colistin-EDTA combination showed ≥ 3 log reduction in CFUs within 2 h (Fig. 1).
MBEC values for colistin-resistant K. pneumoniae biofilms were 8–1000-fold higher for colistin and two–fourfold higher for EDTA alone. Interestingly, colistin (0.5–1 µg/ml) in combination with EDTA (12 mg/ml) was able to completely eradicate the mature biofilms of colistin-resistant K. pneumoniae clinical isolates (p < 0.05) (Table 1).
Combination of colistin-EDTA shows potent efficacy in eradicating biofilms within a 24-h treatment exposure
The single exposure to colistin (1 µg/ml) plus EDTA (12 mg/ml) in combination displayed progressive reductions in biofilm biovolume in a time-dependent manner with the most pronounced eradication effects within 24 h (p < 0.01) (Fig. 2a). Within a short exposure time (6 h), bacterial cell viability within the biofilm was significantly reduced (p < 0.001) with colistin-EDTA combination treatment when compared to EDTA or colistin alone (Fig. 2b). When compared to the PBS control (untreated) group, colistin alone resulted in a lower cell viability but a higher rise in biofilm biovolume. Interestingly, EDTA alone displayed significant reduction in bacteria cell viability within the biofilm after 6-h exposure, but sharp increase of viable cells on 12 and 24 h (Fig. 2b).
Effects of colistin, EDTA and colistin-EDTA combination on (a) biofilm biovolume (OD 560). (b) biofilm cell viability (%) of colistin-resistant K. pneumoniae at different time interval in vitro. All experiments in (a, b) were performed as three biologically independent experiments, and the mean ± s.d. is shown. P values were determined using an unpaired, two-tailed Student’s t-test.
Colistin-EDTA combination significantly eradicate catheter-related biofilm infections of colistin-resistant K. pneumoniae in vitro and in vivo
There was significant reduction in biofilm biomass (p < 0.001) with a significantly lower live/dead ratio (p < 0.01) of bacteria within biofilms treated with colistin-EDTA combination (1 µg/ml + 12 mg/ml) when compared to colistin (1 µg/ml) or EDTA (12 mg/ml) alone, both in vitro (Fig. 3a–c) and in vivo (Fig. 3d–f). Furthermore, as compared to colistin and EDTA alone, the colistin-EDTA combination displayed significantly increased inhibitory effects on biofilm biovolume (p < 0.001) of colistin-resistant K. pneumoniae, both in vitro and in vivo (Fig. 3). Confocal imaging analysis further confirmed the significant reduction in biofilm biovolume and viable cells of colistin-resistant K. pneumoniae within biofilms exposed to colistin-EDTA combination, compared to EDTA or colistin alone (Fig. 4).
Effects of colistin (1 µg/ml), EDTA (12 mg/ml) and colistin- EDTA combination (1 µg/ml + 12 mg/ml)on colistin-resistant K. pneumoniae biofilms (a) in vitro biomass (b) in vitro Live/Dead cell ratio (c) in vitro bio-volume inhibition, and catheter-related biofilm infection of colistin-resistant K. pneumoniae (d) in vivo biomass, (e) in vivo bio-volume inhibition (f) in vivo Live/Dead cell ratio. All experiments in (a–f) were performed as three biologically independent experiments, and the mean ± s.d. is shown. P values were determined using an unpaired, two-tailed Student’s t-test.
Confocal imaging analysis (3D and cross sectional). (A–C) PBS-treated, (D–F) Colistin-treated, (G–I) EDTA-treated, (J–L) Colistin-EDTA combination-treated catheter-related biofilm infection of colistin-resistant K. pneumoniae in vivo. All experiments in (A–L) were performed as three biologically independent experiments, and the mean ± s.d. is shown. P values were determined using an unpaired, two-tailed Student’s t-test.
Colistin-EDTA combination significantly decreases bacterial load in internal organs and serum creatinine
Throughout all tested days, mice treated with colistin-EDTA combination (1 µg/ml + 12 mg/ml) exhibited a significant reduction in K. pneumoniae bacterial load in internal organs—blood, heart, kidneys, lungs, spleen, and tissues surrounding catheter, when compared to mice treated with colistin or EDTA alone (p < 0.05) (Fig. 5b). Significantly, EDTA-treated mice had lower bacterial loads in various internal organs on all tested days when compared to colistin-treated mice (p < 0.05) (Fig. 5b). Furthermore, infected mice treated with colistin-EDTA combination showed significantly lower serum creatinine levels than mice treated with colistin or EDTA alone (p < 0.05). In comparison to colistin-treated mice, administration of EDTA alone significantly reduced serum creatinine levels in treated mice (p < 0.05) (Fig. 5c).
Colistin-EDTA combination significantly improves the survival of mice
Mice treated with the colistin-EDTA combination displayed significantly higher survival rates of 100% until day 7 when compared to mice given colistin alone (p < 0.0001) or EDTA alone (p < 0.001) (Fig. 5d). Interestingly, EDTA-treated mice had significantly higher survival rates than the colistin-treated mice (p < 0.0001).
Exposure to colistin-EDTA combination result in altered expressions of virulent genes in vivo
Expression of kfu was significantly increased (p < 0.05) after giving colistin-EDTA combination as compared to colistin or EDTA-treated groups. Genes—ybtS and luxS expression were similar in both colistin and colistin-EDTA-treated groups, however their expression become significantly increased (p < 0.05) after EDTA treatment. The expression of mrkD was not significantly (p > 0.05) affected by all treatments. The gene-ompK 35 expression was increased significantly (p < 0.05) with EDTA as compared to colistin treatment, but the expression level decreased significantly (p < 0.05) with colistin-EDTA combination treatment. The expression of ompK36 was found to be comparable in colistin and colistin-EDTA combination treatments, despite EDTA decreasing expression (p < 0.05) of this gene. For uge and wabG, their expression levels were significantly increased (p < 0.05) after exposure to EDTA as compared to colistin and colistin-EDTA combination treatments (Fig. 6).
Discussion
The rising trend of colistin resistance and catheter-related biofilm infections in K. pneumoniae has led to recurrent and often untreatable infections, especially in critically ill patients3,16. Therefore, an effective therapy to overcome colistin resistant K. pneumoniae catheter-related biofilm infections has become an urgent necessity. In this study, mature colistin-resistant K. pneumoniae biofilms showed significant antimicrobial tolerance with an MBEC 1000 times higher than their corresponding MIC values. These findings are in line with a previous study that indicated higher antimicrobial tolerance of mature biofilms due to the barrier effects of biofilm matrix which limit antibiotic penetration17. Interestingly, colistin resistance was significantly reversed in both planktonic and mature biofilms of colistin-resistant K. pneumoniae when colistin (0.25–1 µg/ml) was given in combination with EDTA (12 mg/ml). These findings agree with a prior study showing synergistic antibacterial effects of antimicrobial peptide AA23 and EDTA on planktonic Gram-negative bacteria18.
The enhanced antimicrobial spectrum of colistin-EDTA combination against planktonic colistin-resistant K. pneumoniae could be owing to their synergistic interactions in increasing bacterial membrane permeability, which augments intracellular content release, and bacterial death9,19. Also, the chelation activities of EDTA may potentiate colistin's entry into bacteria to exert their bactericidal effects by blocking essential respiratory enzymes which are important intracellular targets of colistin20.
Increased biofilm biovolume of K. pneumoniae following exposure to subinhibitory concentrations of colistin (1 µg/ml) observed in this study could be explained as a bacterial adaptive survival response to antibiotic stress21. These findings are also consistent with previous research which indicated an increase in development of MDR Acinetobacter baumanii biofilms by sub-inhibitory doses of colistin and polymyxin (1/2 and 1/4 MIC) through regulating efflux pump and biofilm-related gene expression22. Because antibiotics at sub-inhibitory doses can facilitate biofilm formation in clinically important pathogens through different strategies21, it is valuable to further investigate the mechanisms involved in increasing colistin-resistant K. pneumoniae biofilms in the presence of antibiotic stress.
Although colistin displayed antibiofilm effects on metabolically inactive cells in the inner layers of Escherichia coli and MRSA biofilms with intrinsic colistin resistance, regrowth of colistin-resistant phenotypes was also observed following treatment with 16 mg/L of colistin monotherapy14,15. Even though EDTA produced potent antimicrobial activities in reducing biofilm biovolume and biofilm-embedded viable cells, incomplete biofilm eradication and a sharp increase in biofilm cells after 24-h EDTA (12 mg/ml) treatment suggests that antibiotics should be administered in conjunction with EDTA for curative treatment and preventative measures for recurrence of catheter-related biofilm infections. Interestingly, the colistin-EDTA combination displayed improved antibiofilm activities in completely eradicating mature biofilm and inhibiting biofilm bacterial viabilities within 24 h of treatment. This may have occurred due to the biofilm matrix disruption by EDTA's metal ion chelation, which may not only facilitate colistin penetration into biofilm inner layers, but also increase bacterial release, where they act synergistically to produce lethal effects on released biofilm bacteria9,10,14,23. Previous studies also demonstrated that EDTA increased bactericidal effects of gentamicin on Enterobacteriaceae biofilms by matrix disruption and synergistic bactericidal effects11.
To further confirm the efficacy of the colistin-EDTA combination, a catheter-related biofilm infection was developed in immunocompromised mice to obtain a clinically relevant animal model that relates to patients’ conditions commonly seen in clinical settings. Interestingly, administration of colistin-EDTA combination within 24-h exposure not only successfully eradicated catheter-related biofilm infections, but also decreased bacterial viabilities, demonstrating their potent efficacy for eliminating the risk of recurrence both in vitro and in vivo. These findings support the previous study demonstrating the in vitro and in vivo effectiveness of gentamicin-EDTA combination for the eradication of catheter-associated Gram-negative pathogens in Totally Implantable Venous-Access Ports (TIVAP) catheters11,12.
Furthermore, the colistin-EDTA combination was observed to reduce bacterial load in internal organs, decrease serum creatinine, and provide significant protection against mortality in treated mice, indicating their significant synergistic therapeutic efficacy and safety in vivo. These results are consistent with previous study in which EDTA enhanced imipenem susceptibilities to treat New Delhi metallo-ß-lactamase-1(NDM 1) producing E. coli and reduced systemic bacterial burden in a murine sepsis model24. In pneumonic mice induced by Pseudomonas aeruginosa, reduced pulmonary bacterial burden and striking improvement with 100% survival were observed after subcutaneous and intranasal administration of imipenem-EDTA combination25. Colistin exposure has been linked to increased serum creatinine in treated patients due to their induced oxidative stress in proximal renal tubules26. However, the lower dose of colistin in the colistin-EDTA combination, as well as the combined vasodilatation and antioxidant effects of EDTA27, may help to mitigate these potential side-effects of colistin in treated mice. Whereas a subinhibitory dose of colistin in colistin-EDTA combination has been shown to prevent bacterial regrowth and achieve significant in vitro and in vivo efficacies, using colistin-EDTA combination could prevent not only the resurgence of the resistant population, but also development of renal complications which are major limiting factors for colistin usage in clinical settings28. Although pseudo-thrombocytopenia can occur by flushing or diffusion into the systemic circulation when EDTA is used inside catheters as lock solution29, the dose of EDTA used in this study was 12 mg/ml, which is lower than the FDA-approved dose of EDTA for use in lead poisoning (total daily dose of 1000 mg/m2)30, the dose used in hemodialysis catheters (30 mg/ml)31 and slightly higher than the dose for reducing cardiovascular events in diabetic patients with peripheral vascular disease (6 mg/ml)32.
This study also revealed altered in vivo expression of various virulence genes of K. pneumoniae which include those related to lipopolysaccharide (wabG and uge) that protect bacteria from host immune defenses for enhancing pathogenicity, porin genes (ompK 35 and 36) for nutrient transport to improve bacterial survival inside the host, iron acquisition system genes (kfu and ybtS) which modulate host immune responses for systemic survival and dissemination, type 3 fimbria adhesin – mrkD for bacterial binding to develop biofilm on abiotic surfaces such as catheters, and type 2 quorum-sensing regulatory system gene – luxS to promote biofilm development by facilitating cell to cell communication33.
. Exposure to antimicrobial agents create a stressful environment for bacteria and it could result in altered expression of bacterial genes which reflects how the bacteria deal with the stress inside the host34. Altered in vivo expression of virulence genes found in this study point to the bacterial adaptive response to survive in hostile environment that occurred as the impacts of different treatments tested in mice35,36. Given the scarcity of knowledge on the involvement of these genes in the response to various stresses induced by colistin and EDTA treatment in K. pneumoniae, further studies are needed to investigate the consequence of virulence gene upregulation following this treatment.
Although the subcutaneous catheter-related biofilm infection model used in this study is relevant to conditions seen in clinical settings and linked to device-associated infections or catheter-associated bloodstream infection, randomized control trials will be required to validate the clinical safety and efficacy of colistin-EDTA combination therapy in the treatment of catheter-related biofilm infection.
In conclusion, this is the first in vitro and in vivo study which highlights a novel colistin-EDTA combination therapy successfully reversing colistin resistance and eradicating K. pneumoniae catheter-related biofilm infections, while also demonstrating a favorable safety profile with low resistance and toxicity risks.
Material and methods
Strains and growth conditions
The colistin-resistant K. pneumoniae clinical isolates (n = 47) with different resistance profiles were obtained without preference from a strain repository at the Department of Microbiology, King Chulalongkorn Memorial Hospital. Clinical strains had been isolated during 2016–2019 from 47 infected patients as part of the standard care of the patients and was not related to the present study. Strains were stored in a repository collection after standard characterization and identification (including 16S rRNA sequencing using primers as documented previously) (Supplementary Table S4). The clinical isolates were cultured on Müller–Hinton agar (Sigma-Aldrich) plates at 37 °C. The strains were stored at − 80 °C in tryptic soy broth (Sigma-Aldrich) with 15% glycerol until they were used in subsequent experiments.
Antimicrobial agents
Colistin and EDTA were purchased from Sigma-Aldrich and stock solutions were prepared less than 24 h before use. Colistin and EDTA were dissolved in cation-adjusted Müller-Hinton II broth (MHIIB) (Becton Dickinson) medium and the supplemented medium sterilized by filtration through a membrane filter nominally with 0.22 μm pores. Serial dilutions of the colistin and EDTA stocks were prepared in MHIIB medium immediately before use.
K. pneumoniae susceptibilities to colistin and EDTA
K. pneumoniae planktonic susceptibility (Minimal Inhibitory Concentrations, MICs) to colistin were established using standard techniques (broth microdilution) according to EUCAST (criteria for Enterobacteriaceae for colistin only)37and CLSI guidelines38. E. coli ATCC 25922, and P. aeruginosa ATCC 27853 were used as quality control strains. To establish K. pneumoniae planktonic MIC for colistin and EDTA, drugs were serially diluted two-fold in 96-well microtiter plates and bacteria added. The MIC to EDTA was also determined by serial dilution as above. The plates were incubated at 37 °C for 18 h.
Synergistic activities of colistin-EDTA combination against planktonic colistin-resistant K. pneumoniae clinical isolates
The synergistic activities of colistin and EDTA combination against planktonic colistin-resistant K. pneumoniae clinical isolates were screened by checkerboard assay. The synergistic activities were interpreted as follows: Synergy: FIC index ≤ 0.5; Additive: 0.5 > FIC index ≤ 1; Indifference: 1 > FIC index ≤ 4, and Antagonism: FIC index > 4, respectively39.
Time-kill assay
Planktonic colistin-resistant K. pneumoniae isolates that showed the synergistic activities with colistin-EDTA combination were confirmed by using time-kill assay. The bacteria were grown with no drug, each drug, and drug combinations. The viable bacterial cells were collected at 0, 2, 4, 6, 8, 12, and 24 h. After incubation, the CFU/ml of viable bacterial cells were quantified by colony counting on solid media. The synergistic activities were interpreted when there was ≥ 2 log10 (CFU/ml)-fold decrease in combination compared with the single antibiotic; Bactericidal activity was defined as a ≥ 3 log10(CFU/ml)-fold decrease when compared to the number of viable cells at initial time point39.
Quantification of biofilm by crystal violet assay
Quantification of biofilm formation was done by crystal violet assay as described previously40. Briefly overnight culture of bacteria were standardized with OD of 0.02 at 600 nm (5 × 107 CFU mL−1) and 100 μL aliquots are added in triplicate to flat-bottomed 96-well polystyrene microtiter plates (SPL Life Sciences). The plates were incubated at 37 °C for 24 h. Adherent biofilms were fixed with crystal violet (0.1%) and stained biofilms were solubilized with 30% acetic acid. The absorbance (OD) at 560 nm were determined using a microtiter-plate-reading fluorimeter (Varioskan Flash Multimode Reader; Thermo Fisher Scientific). All experiments were performed in triplicate and repeated three times.
Effects of colistin, EDTA and colistin-EDTA combination for eradication of in vitro biofilms
The eradication effects of colistin, EDTA, and colistin-EDTA combination on 24 h-old in vitro biofilms of colistin-resistant K. pneumoniae were studied to determine the minimum biofilm eradication concentration (MBECs) as described previously41. Tests covered single, or combination of colistin- EDTA at 37 °C for the following treatment times; 6, 12, 24, and 48 h. The eradication effects on in vitro biofilms biovolume and biofilm cell viability were analyzed by crystal violet and PrestoBlue assays as described previously42.
Animal study
Female 8-week-old C57BL/6 background mice were purchased from Nomura Siam International (Pathumwan, Bangkok, Thailand) and were used in all experiments. Animals were at rest for 1 week in the animal facility before use. Animals received food and water ad libitum and were housed at a maximum of 2 mice per cage, weighed and closely monitored for any signs of distress throughout experimental periods.
Catheter-related biofilm infection mouse model
The previously described in vivo catheter-related infection model was performed with modifications43 (Fig. 5a). Mice were immunosuppressed by subcutaneous administration of dexamethasone at 0.25 mg/kg/dose once a day for 3 days before catheter implantation, which was maintained throughout the study. To avoid any bacterial contamination of the host, the drinking water was supplemented with ampicillin sodium powder (0.5 g/L) before catheter implantation and stopped one day before implantation. 25-mm catheters (NIPRO) with an inner diameter of 1.45 mm were pre-coated overnight with 1.8 ml of 100% fetal bovine serum (Gibco™; Waltham, MA) at 37° C. Catheters were then inoculated with cell suspensions of colistin-resistant K. pneumoniae in MHIIB at final concentrations of 5 × 107 CFU ml−1 for 90 min at 37 °C to allow for microbial adhesion to catheters. For each experimental set, in vitro-infected catheters were processed for assessment of microbial recovery to confirm standardized microbial adherence to catheters prior to implantation. Following in vitro microbial adhesion, catheter pieces were rinsed with PBS and kept on ice until implanted. Subcutaneous implantation of catheter pieces (approximately 0.5–1 cm) was done on the left and right side of the flank of animal under isoflurane anesthesia. The incisions were closed with sutures. The wound was disinfected with 0.5% chlorhexidine in 70% alcohol, or with 1% iodine isopropanol. Animals were monitored until they recovered from anesthesia, and then daily for any developing clinical signs of distress. Animals were euthanized by isoflurane inhalation and collected samples (catheters, blood, heart, tissues surrounding catheter, lungs, spleen, and kidneys) were aseptically harvested individually.
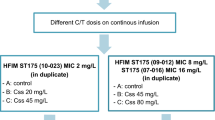
Effects of colistin, EDTA and colistin-EDTA combination on catheter-related biofilm infection mouse model
Animals were divided into control (no therapy) group and experimental (therapy) group with 3 subgroups. The catheter-related biofilm infections of colistin-resistant K. pneumoniae in implanted catheters were exposed to PBS (control), colistin (1 µg/ml), EDTA (12 mg/ml) and colistin- EDTA (1 µg/ml + 12 mg/ml) for a total of 4 groups with 10 animals in each group. After 24 h of different treatments, catheters were removed under aseptic conditions and the efficacies of each treatment in different groups were analyzed by confocal laser scanning microscope (biomass, Live/Dead ratio and biovolume inhibition) and bacterial counting44. In addition, animals were monitored regularly for 7 days or until death, whichever occurred first, to determine their survival. Also, mice were sacrificed on different days post-infection by cervical dislocation to determine viable cell count (CFU/ml) in treated catheter and internal organs (blood, heart, kidneys, lungs, spleen, and tissues surrounding catheter) after each treatment as described previously24. Measurements of serum creatinine levels were done after exposure to each treatment in all treated groups as described previously45.
Confocal laser scanning microscopic analysis (CLSM)
For CLSM analysis, supernatants are carefully removed and biofilms are subsequently stained with the LIVE/DEAD Bacterial Viability Kit (Invitrogen) according to the manufacturer’s protocol. MATLAB-based tool PHLIP (without connected volume filtration) were used to calculate descriptive parameters of biofilms (including biovolume, substratum coverage, area-to-volume ratio, spatial spreading and 3D colocalization) from the integrated total of each individual slice of a thresholded z-stack as described previously42,46,47. The calculation of the different proportions of green (live bacteria) as well as red and yellow/colocalized (dead bacteria) biovolumes from the analyzed stacks were using the 'colocalization in 3D' value and the parameters 'red', 'green', and 'total biovolume' (in μm3) generated by the PHLIP software as described previously47,48. A biofilm was considered affected by an antibiotic or EDTA or combination within the given concentration range when there is a constant increase in the red + yellow (RY) biovolume fraction within the given antibiotic concentration range and this fraction is at least 80% of the total biovolume.
Effect of single and combination of colistin-EDTA on in vivo virulence gene expression
The expression level of virulence factors (kfu luxS, mrkD, ompK35, ompK36, uge, wabG and ybtS) were determined with Quantitative RT-PCR (qRT-PCR) using the specific primers as described previously48,49. All primers are listed in Supplementary Table S4.
Total mRNA were extracted from control and experimental groups of in vivo catheter-related biofilm infection that were challenged with various treatments for 24 h. All samples are analyzed in triplicate. Using the housekeeping gene—16srRNA for normalization, the relative quantification of gene expression for each treatment group was computed using the ΔΔCT (CT is threshold cycle) method to evaluate and compare fold change differences.
Data analysis
All statistical analysis was conducted using R statistic package50. The data were compared by either unpaired two-tailed Student’s t-test or unpaired two-tailed Mann–Whitney’s U test. All data were presented as the mean ± s.d. Statistical significance was accepted at p < 0.05, p < 0.01, p < 0.001, and p < 0.0001.
Ethical approval
The study protocol was approved by the Institutional Review Board (IRB) of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand (COA No. 045/2020, IRB No. 774/63) was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments and comparable ethical standards. Animal care and use protocol are based upon the National Institutes of Health (NIH), USA. The protocol was approved by the Institutional Animal Care and Use Committee of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand (Certificate No- 033/2563, Research Project No. – 020/2563). The study was carried out in compliance with the ARRIVE guidelines (Animal Research: Reporting of In Vivo Experiments).
Informed consent
For this retrospective study of anonymous clinical isolates, the requirement for informed consent from patients was waived by Institutional Review Board (IRB) of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand (COA No. 045/2020, IRB No. 774/63).
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its additional information.
References
Gominet, M., Compain, F., Beloin, C. & Lebeaux, D. Central venous catheters and biofilms: Where do we stand in 2017?. APMIS 125, 365–375 (2017).
Donlan, R. M. Biofilms and device-associated infections. Emerg. Infect. Dis. 7, 277 (2001).
Lendak, D. et al. Changing epidemiology of catheter-related bloodstream infections in neutropenic oncohematological patients. PLoS ONE 16, e0251010 (2021).
Raad, I. I., Sabbagh, M. F., Rand, K. H. & Sherertz, R. J. Quantitative tip culture methods and the diagnosis of central venous catheter-related infections. Diagn. Microbiol. Infect. Dis. 15, 13–20 (1992).
Antoniadou, A. et al. Colistin-resistant isolates of Klebsiella pneumoniae emerging in intensive care unit patients: First report of a multiclonal cluster. J. Antimicrob. Chemother. 59, 786–790 (2007).
Mermel, L. A. et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 49, 1–45 (2009).
Justo, J. A. & Bookstaver, P. B. Antibiotic lock therapy: Review of technique and logistical challenges. Infect. Drug Resist. 7, 343–363 (2014).
Liu, Y., Li, R., Xiao, X. & Wang, Z. Antibiotic adjuvants: an alternative approach to overcome multi-drug resistant Gram-negative bacteria. Crit. Rev. Microbiol. 45, 301–314 (2019).
Finnegan, S. & Percival, S. L. EDTA: An antimicrobial and antibiofilm agent for use in wound care. Adv. Wound Care (New Rochelle) 4, 415–421 (2015).
Percival, S. L. et al. Tetrasodium EDTA as a novel central venous catheter lock solution against biofilm. Infect. Control Hosp. Epidemiol. 26, 515–519 (2005).
Lebeaux, D., Leflon-Guibout, V., Ghigo, J. M. & Beloin, C. In vitro activity of gentamicin, vancomycin or amikacin combined with EDTA or l-arginine as lock therapy against a wide spectrum of biofilm-forming clinical strains isolated from catheter-related infections. J. Antimicrob. Chemother. 70, 1704–1712 (2015).
Chauhan, A., Lebeaux, D., Ghigo, J. M. & Beloin, C. Full and broad-spectrum in vivo eradication of catheter-associated biofilms using gentamicin-EDTA antibiotic lock therapy. Antimicrob. Agents Chemother. 56, 6310–6318 (2012).
Biswas, S., Brunel, J. M., Dubus, J. C., Reynaud-Gaubert, M. & Rolain, J. M. Colistin: An update on the antibiotic of the 21st century. Expert. Rev. Anti Infect. Ther. 10, 917–934 (2012).
Lora-Tamayo, J., Murillo, O. & Ariza, J. Clinical use of colistin in biofilm-associated infections. Adv. Exp. Med. Biol. 1145, 181–195 (2019).
Klinger-Strobel, M., Stein, C., Forstner, C., Makarewicz, O. & Pletz, M. W. Effects of colistin on biofilm matrices of Escherichia coli and Staphylococcus aureus. Int. J. Antimicrob. Agents 49, 472–479 (2017).
Capone, A. et al. High rate of colistin resistance among patients with carbapenem-resistant Klebsiella pneumoniae infection accounts for an excess of mortality. Clin. Microbiol. Infect. 19, E23-e30 (2013).
Anderl, J. N., Franklin, M. J. & Stewart, P. S. Role of antibiotic penetration limitation in Klebsiella pneumoniae biofilm resistance to ampicillin and ciprofloxacin. Antimicrob. Agents Chemother. 44, 1818–1824 (2000).
Umerska, A. et al. Synergistic effect of combinations containing EDTA and the antimicrobial peptide AA230, an arenicin-3 derivative, on Gram-negative bacteria. Biomolecules 8, 122 (2018).
Petrosillo, N., Taglietti, F. & Granata, G. Treatment options for Colistin resistant Klebsiella pneumoniae: Present and future. J. Clin. Med. 8, 934 (2019).
Deris, Z. Z. et al. A secondary mode of action of polymyxins against Gram-negative bacteria involves the inhibition of NADH-quinone oxidoreductase activity. J. Antibiot. (Tokyo) 67, 147–151 (2014).
Song, T., Duperthuy, M. & Wai, S. N. Sub-optimal treatment of bacterial biofilms. Antibiotics (Basel) https://doi.org/10.3390/antibiotics5020023 (2016).
Sato, Y., Unno, Y., Ubagai, T. & Ono, Y. Sub-minimum inhibitory concentrations of colistin and polymyxin B promote Acinetobacter baumannii biofilm formation. PLoS ONE 13, e0194556. https://doi.org/10.1371/journal.pone.0194556 (2018).
Haagensen, J. A. et al. Differentiation and distribution of colistin- and sodium dodecyl sulfate-tolerant cells in Pseudomonas aeruginosa biofilms. J. Bacteriol. 189, 28–37 (2007).
Yoshizumi, A. et al. Efficacies of calcium-EDTA in combination with imipenem in a murine model of sepsis caused by Escherichia coli with NDM-1 β-lactamase. J. Infect. Chemother. 19, 992–995 (2013).
Aoki, N. et al. Efficacy of calcium-EDTA as an inhibitor for metallo-β-lactamase in a mouse model of Pseudomonas aeruginosa pneumonia. Antimicrob. Agents Chemother. 54, 4582–4588 (2010).
Gai, Z., Samodelov, S. L., Kullak-Ublick, G. A. & Visentin, M. Molecular mechanisms of Colistin-induced nephrotoxicity. Molecules 24, 653 (2019).
Foglieni, C. et al. Protective effect of EDTA preadministration on renal ischemia. BMC Nephrol. 7, 5 (2006).
Ordooei Javan, A., Shokouhi, S. & Sahraei, Z. A review on colistin nephrotoxicity. Eur. J. Clin. Pharmacol. 71, 801–810 (2015).
Lippi, G. & Plebani, M. EDTA-dependent pseudothrombocytopenia: Further insights and recommendations for prevention of a clinically threatening artifact. Clin. Chem. Lab Med. 50, 1281–1285 (2012).
Porru, S. & Alessio, L. The use of chelating agents in occupational lead poisoning. Occup. Med. (Lond.) 46, 41–48 (1996).
Campos, R. P., do Nascimento, M. M., Chula, D. C. & Riella, M. C. Minocycline-EDTA lock solution prevents catheter-related bacteremia in hemodialysis. J. Am. Soc. Nephrol. 22, 1939–1945 (2011).
Ujueta, F. et al. The effect of EDTA-based chelation on patients with diabetes and peripheral artery disease in the Trial to Assess Chelation Therapy (TACT). J. Diabetes Complicat. 33, 490–494 (2019).
Paczosa, M. K. & Mecsas, J. Klebsiella pneumoniae: Going on the Offense with a Strong Defense. Microbiol. Mol. Biol. Rev. 80, 629–661 (2016).
Dorman, C. J. Flexible response: DNA supercoiling, transcription and bacterial adaptation to environmental stress. Trends Microbiol. 4, 214–216 (1996).
Poole, K. Bacterial stress responses as determinants of antimicrobial resistance. J. Antimicrob. Chemother. 67, 2069–2089 (2012).
Guest, R. L. & Raivio, T. L. Role of the Gram-negative envelope stress response in the presence of antimicrobial agents. Trends Microbiol. 24, 377–390 (2016).
EUCAST. Clinical Breakpoints. European Committee for Antimicrobial Susceptibility Testing; version 6 (2016).
CLSI. Performance Standards for Antimicrobial Susceptibility Testing - Twenty-Fifth Informational Supplement. (Clinical and Laboratory Standards Institute, M100, 2020).
Vidaillac, C., Benichou, L. & Duval, R. E. In vitro synergy of colistin combinations against colistin-resistant Acinetobacter baumannii, Pseudomonas aeruginosa, and Klebsiella pneumoniae isolates. Antimicrob. Agents Chemother. 56, 4856–4861 (2012).
O’Toole, G. A. Microtiter dish biofilm formation assay. J. Vis. Exp https://doi.org/10.3791/2437 (2011).
Jorge, P., Grzywacz, D., Kamysz, W., Lourenço, A. & Pereira, M. O. Searching for new strategies against biofilm infections: Colistin-AMP combinations against Pseudomonas aeruginosa and Staphylococcus aureus single- and double-species biofilms. PLoS ONE 12, e0174654 (2017).
Wannigama, D. L. et al. Simple fluorometric-based assay of antibiotic effectiveness for Acinetobacter baumannii biofilms. Sci. Rep. 9, 6300 (2019).
Kucharíková, S., Vande Velde, G., Himmelreich, U. & Van Dijck, P. Candida albicans biofilm development on medically-relevant foreign bodies in a mouse subcutaneous model followed by bioluminescence imaging. J. Vis. Exp. https://doi.org/10.3791/52239 (2015).
Cerca, N., Gomes, F., Pereira, S., Teixeira, P. & Oliveira, R. Confocal laser scanning microscopy analysis of S. epidermidis biofilms exposed to farnesol, vancomycin and rifampicin. BMC Res. Notes 5, 244 (2012).
Yuen, P. S. et al. A simplified method for HPLC determination of creatinine in mouse serum. Am. J. Physiol. Renal. Physiol. 286, F1116-1119 (2004).
Wannigama, D. L. et al. A rapid and simple method for routine determination of antibiotic sensitivity to biofilm populations of Pseudomonas aeruginosa. Ann. Clin. Microbiol. Antimicrob. 19, 8. https://doi.org/10.1186/s12941-020-00350-6 (2020).
Müsken, M., Di Fiore, S., Römling, U. & Häussler, S. A 96-well-plate–based optical method for the quantitative and qualitative evaluation of Pseudomonas aeruginosa biofilm formation and its application to susceptibility testing. Nat. Protoc. 5, 1460–1469. https://doi.org/10.1038/nprot.2010.110 (2010).
Vuotto, C. et al. Biofilm formation and antibiotic resistance in Klebsiella pneumoniae urinary strains. J. Appl. Microbiol. 123, 1003–1018 (2017).
Compain, F. et al. Multiplex PCR for detection of seven virulence factors and K1/K2 capsular serotypes of Klebsiella pneumoniae. J. Clin. Microbiol. 52, 4377–4380 (2014).
RcoreTeam. R, a Language and Environment for Statistical Computing. (R Foundation for Statistical Computing, Vienna, Austria, 2016).
Acknowledgements
We thank the staff of the bacteriology division, Department of Microbiology at King Chulalongkorn Memorial Hospital, for providing the K. pneumoniae clinical isolates.
Funding
This work was supported by a grant from the 90th Year Anniversary Ratchadapiseksompotch Endowment Fund from the Faculty of Medicine and Graduate School, Chulalongkorn University, Bangkok, Thailand and Ratchadapiseksompotch Fund, Chulalongkorn University Bangkok, Thailand (grant No. CU_GR_63_119_30_26). Aye Mya Sithu Shein was supported under the Chulalongkorn University Graduate Scholarship Program for ASEAN Countries. Dhammika Leshan Wannigama was supported by Chulalongkorn University (Second Century Fund- C2F Fellowship), and the University of Western Australia (Overseas Research Experience Fellowship). The sponsor(s) had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
A.M.S.S.: investigation, data curation, formal analysis, writing the original draft of the manuscript. D.L.W.: conception, funding acquisition, investigation, supervision, data curation, formal analysis, writing the original draft of the manuscript. P.G.H.: conception, supervision, critical review and editing of the manuscript. C.H.: conception, formal analysis, supervision, critical review and editing of the manuscript. S.A.: conception, formal analysis, supervision, critical review and editing of the manuscript. P.H.: conception, formal analysis, supervision, critical review and editing of the manuscript. N.C.: confocal microscopy data, analysis, supervision, critical review and editing of the manuscript. T.S.: formal analysis, supervision, critical review and editing of the manuscript. S.L.-in.: supervision, critical review and editing of the manuscript. L.T.: conception for mouse model. S.N.: bacteria identification and clinical collection. U.R.: bacteria identification and clinical collection. N.K.: bacteria identification and clinical collection. M.L.: bacteria identification and clinical collection. S.S.: bacteria identification and clinical collection. N.M.: bacteria identification and clinical collection. T.T.: formal analysis of real-time PCR data, critical review and editing of the manuscript. L.G.: conception for mouse model, critical review and editing of the manuscript. C.X.: conception for mouse model, critical review and editing of the manuscript. R.K.: conception for mouse model, formal analysis, supervision, critical review and editing of the manuscript. P.P.: supervision, critical review and editing of the manuscript. R.R.: supervision, critical review and editing of the manuscript. A.L.: supervision, critical review and editing of the manuscript. T.C.: conception, funding acquisition, supervision, critical review and editing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shein, A.M.S., Wannigama, D.L., Higgins, P.G. et al. Novel colistin-EDTA combination for successful eradication of colistin-resistant Klebsiella pneumoniae catheter-related biofilm infections. Sci Rep 11, 21676 (2021). https://doi.org/10.1038/s41598-021-01052-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-01052-5
This article is cited by
-
The use of combination therapy for the improvement of colistin activity against bacterial biofilm
Brazilian Journal of Microbiology (2024)
-
Biofilm inhibition/eradication: exploring strategies and confronting challenges in combatting biofilm
Archives of Microbiology (2024)
-
High prevalence of mgrB-mediated colistin resistance among carbapenem-resistant Klebsiella pneumoniae is associated with biofilm formation, and can be overcome by colistin-EDTA combination therapy
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.