Abstract
Ceftolozane/tazobactam (C/T) has emerged as a potential agent for the treatment of extensively drug-resistant (XDR) Pseudomonas aeruginosa infections. As it is a time-dependent antimicrobial, prolonged infusion may help achieve pharmacokinetic/pharmacodynamic (PK/PD) targets. To compare alternative steady-state concentrations (Css) of C/T in continuous infusion (CI) against three XDR P. aeruginosa ST175 isolates with C/T minimum inhibitory concentration (MIC) values of 2 to 16 mg/L in a hollow-fiber infection model (HFIM). Duplicate 10-day HFIM assays were performed to evaluate Css of C/T in CI: one compared 20 and 45 mg/L against the C/T-susceptible isolate while the other compared 45 and 80 mg/L against the two C/T-non-susceptible isolates. C/T resistance emerged when C/T-susceptible isolate was treated with C/T in CI at a Css of 20 mg/L; which showed a deletion in the gene encoding AmpC β-lactamase. The higher dosing regimen (80 mg/L) showed a slight advantage in effectiveness. The higher dosing regimen has the greatest bactericidal effect, regardless of C/T MIC. Exposure to the suboptimal Css of 20 mg/L led to the emergence of C/T resistance in the susceptible isolate. Antimicrobial regimens should be optimized through C/T levels monitoring and dose adjustments to improve clinical management.
Similar content being viewed by others
Introduction
The indiscriminate use of antibiotics has contributed to the emergence and selection of multidrug-resistant (MDR) and extensively drug-resistant (XDR) bacteria1,2 and led to a critical decrease in the availability of alternative antibiotic treatments, limiting treatment options and increasing morbidity and mortality3. Pseudomonas aeruginosa has an outstanding capacity to develop resistance through a broad range of mechanisms4,5,6. MDR/XDR P. aeruginosa isolates are particularly concerning, as they are the leading cause of nosocomial infections and a strong contributor to in-hospital mortality7. The ST175 clone is especially significant in several European countries8. The development of tailored antimicrobial treatments could greatly improve the clinical management of infections caused by MDR/XDR P. aeruginosa.
Ceftolozane/tazobactam (C/T; Zerbaxa; Merck & Co, Inc., Kenilworth, NJ) has emerged as a potential agent against MDR/XDR strains that are resistant to all first-line antibiotics9. The combination of ceftolozane, a cephalosporin, and tazobactam, a beta-lactamase inhibitor6, has shown promising results in the treatment of infections caused by P. aeruginosa strains with different resistance patterns10. The current recommended dosage for C/T is a 1-h infusion of 1/0.5 g every 8 h for urinary tract and soft tissue infections and 2/1 g every 8 h for respiratory infections11. The pharmacokinetic (PK) properties of ceftolozane have been studied alone and combined with tazobactam in healthy individuals6,12. As C/T is a time-dependent antibiotic, the percentage of time during the dosing interval in which free drug plasma concentrations remain above the minimum inhibitory concentration (MIC) (%T>MIC) is the best pharmacodynamic (PD) parameter for predicting bacteriological efficacy. The %T>MIC is approximately 40–50% for some cephalosporin6,12, but recent studies have shown that the percentage for ceftolozane is much lower, similar to that reported for carbapenems13,14. The currently recommended C/T dosing regimen thus might be insufficient against P. aeruginosa strains with a C/T MIC above the susceptibility breakpoint of 4 mg/L. Infections caused by these strains would therefore need to be treated with combinations of antibiotics or optimized dosing15.
The aim of this study was to evaluate different steady-state concentrations (Css) of C/T in continuous infusion (CI) to test the effectiveness of C/T and the emergence of resistance in an in vitro hollow-fiber infection model (HFIM). Three XDR P. aeruginosa ST175 isolates with different C/T MICs (2, 8 and 16 mg/L) were tested.
Material and methods
Bacterial isolates
Three XDR P. aeruginosa clinical isolates were analysed: ST175 (10-023), with a C/T MIC of 2 mg/L; ST175 (09-012), with a C/T MIC of 8 mg/L; and ST175 (07-016), with a C/T MIC of 16 mg/L. These isolates had been previously characterized at a molecular level using pulsed-field gel electrophoresis, multi-locus sequence typing, and whole genome sequencing and are representative of the clones and resistance mechanisms in our environment16.
Antibiotics
C/T (Zerbaxa®; lot number SO15404; expiration date, August 2020) was provided by Merck & Co., Inc. (Kenilworth, NJ). CI C/T dosing regimens were simulated to achieve approximate Css of 20, 45 and 80 mg/L (which respectively correspond to 3, 6 and > 9 g/4.5 g every 24 h)17. The exposures to simulate the steady-state human pharmacokinetics of unbound drug were based on elimination half-life of 3 h for ceftolozane18,19. A protein-binding estimate was 20% for ceftolozane. The C/T regimens included a dose range based on previously determined Cmax and AUC19. Exposure to tazobactam was not considered, as this drug has a limited role in ceftolozane’s activity against P. aeruginosa20. C/T concentrations were validated by high-performance liquid chromatography (HPLC)21.
HFIM
The HFIM has been used extensively and described elsewhere18,22. Duplicate 10-day HFIM assays were conducted in two stages to investigate the effectiveness of C/T and the development of antimicrobial resistance. Effectiveness was investigated by treating P. aeruginosa isolates ST175 (09-012) and ST175 (07-016) with C/T in CI at steady-state concentrations of 45 and 80 mg/L, while resistance was investigated by treating ST175 (10-023) to C/T in CI at steady-state concentrations of 20 and 45 mg/L.
Polyethersulfone hemofilters where used as the hollow-fiber cartridges (Aquamax HF03, Nikkiso, Belgium). Each C/T regimen was pumped into the corresponding reservoir by a separate infusion pump to simulate human free drug PK profiles in humans. Fresh drug-free growth medium (cation-adjusted Mueller–Hinton broth [CAMHB]) was continuously infused into the central reservoir to dilute and simulate drug elimination in humans. An equal volume of drug-containing medium was concurrently removed from the central reservoir to maintain an isovolumetric system. The extracapillary space of each HFIM was inoculated with 50 mL of bacterial suspension. High-inoculum infections were simulated. Once inoculated, the bacteria were left in the extracapillary compartment of the HFIM cartridge, where they were exposed to fluctuating drug concentrations. The assays were conducted at 37 °C. Maintenance doses were given continuously at the same rate, according to the clinical dosing frequency. Bacterial densities (log10 CFU/mL) in the cartridges were measured at 0, 8, 24, 48, 72, 96, 144, 168, 192 and 240 h. The samples were washed and suspended in saline solution to minimize drug carryover. Serial decimal dilutions were cultured onto drug-free trypticase soy agar (BBL TSA II, Becton Dickinson) plates to determine the total bacterial population. The lower limit of detection (LLOD) was 1.3 log10 CFU/mL. Study flow is shown in Fig. 1. Bactericidal activity was defined as a reduction of 3 log10 CFU/mL from the initial bacterial load23.
Study flow showing in vitro 10-day HFIM assays conducted with three XDR Pseudomonas aeruginosa ST175 isolates with C/T MICs ranging from 2 to 16 mg/L using different Css of C/T in CI: 20 and 45 mg/L to test the emergence of C/T resistance in the susceptible ST175 (10-023) isolate, and 45 and 80 mg/L to test the effectiveness of C/T against the non-susceptible isolates ST175 (09-012) and ST175 (07-016). C/T, ceftolozane/tazobactam; HFIM, hollow-fiber infection model; MIC, minimum inhibitory concentration; XDR, extensively-drug resistant; Css, steady-state concentration; CI, continuous infusion.
Resistance studies
An aliquot of bacterial suspension from each HFIM was cultured onto drug-containing plates (TSA agar) supplemented with C/T at twofold, fourfold and eightfold the baseline MIC to assess the effect of each regimen on the least susceptible bacterial population. Mutants that grew on these plates were compared with total bacterial population on drug-free TSA plates. When growth was observed after 72 h, up to three colonies were selected to assess C/T MICs and were analysed for changes in MICs from baseline. Antibiotic susceptibility testing was performed according to Clinical & Laboratory Standards Institute (CLSI) guidelines for broth microdilution using CAMHB24. The isolates were serially passaged three times on drug-free plates to assess the stability of the phenotype. To investigate the mechanisms leading to C/T resistance, the presence of structural mutations in the catalytic centre of AmpC was analyzed by PCR and sequencing as whole genome sequencing as previously described25.
Drug concentrations
Antibiotic samples were collected at different time points over the first 48 h (0, 3, 5, 7, 9, 23, 25 27, 29 and 47 h) and once a day for the first dose, until the end of the study. Samples were stored at − 80 °C until analysis. All exposures to simulate steady-state human PK of unbound drug were based on the half-life of ceftolozane (exposure to tazobactam was not considered as previously mentioned). Antibiotic concentrations were analysed by HPLC21.
Results
In vitro susceptibility and resistance mechanisms
The isolates had been previously characterized at a molecular level16. The ST175 (10-023) isolate was susceptible to C/T (MIC 2 mg/L) and resistant to the other β-lactams due to OprD inactivation and AmpC hyperproduction16. The ST175 (09-012) isolate had intermediate resistance to C/T (MIC 8 mg/L) and the mechanisms identified were OprD inactivation, AmpC hyperproduction, and a mutation in PBP3 (R504C) that has been previously associated with increased β-lactam resistance16. The ST175 (07-016) isolate was resistant to C/T (MIC 16 mg/L) and in this case the mechanism identified was the production of a class A carbapenemase GES-5 coupled with OprD inactivation16.
HFIM and data analysis
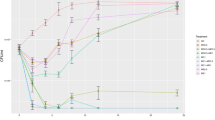
Table 1 shows the total mean reduction (log difference at 24 h) for each antibiotic compared with the control. In Fig. 2 results for the reductions in density over time are shown. For ST175 (10-023) the mean bacterial density of the starting inoculum was 7.54 log10 CFU/mL (Fig. 2A). A five log10 CFU/mL reduction was observed for the Css of 45 mg/L. The Css of 20 mg/L was associated with an initial reduction followed by regrowth on day 6. The final bacterial density was 7 ± 0.45 log10 CFU/mL, which corresponds to an overall reduction of 0.54 log10 CFU/mL (no bactericidal effect).
Mean reduction in bacterial density during the 10-day HFIM assays with ST175 (10-023), ST175 (09-012) and ST175 (07-016) isolates treated with different Css of C/T (20, 45 and 80 mg/L) in CI. Respective C/T MIC values of 2, 8 and 16 mg/L. C/T, ceftolozane/tazobactam; CI, continuous infusion; Css, steady-state concentration; LLOD, lower limit of detection; MIC, minimum inhibitory concentration.
The 10-day HFIM studies to evaluate the effectiveness of higher than the standard Css of C/T (80 mg/L in CI) were performed using the two non-susceptible isolates, ST175 (09-012) and (07-016). The mean starting inoculum was 6.76 log10 CFU/mL. Figure 2B, C shows the changes in bacterial density at the different time points analyzed. Overall, the C/T Css of 80 mg/L in CI showed a slight advantage over the Css of 45 mg/L. Both dosing regimens showed similar effectiveness against ST175 (09-012) up to day 6, but on day 7, the higher regimen achieved eradication of the bacterial population (below the LLOD). The curve for the Css of 45 mg/L plateaued and the final density was 1.65 ± 0.6 log10 CFU/mL. A similar pattern was observed for ST175 (07-016), but in this case, the Css of 80 mg/L did not eradicate the bacterial population. In brief, C/T at both Css (45 and 80 mg/L) exerted bactericidal activity against the two non-susceptible isolates.
Resistance studies
In the 10-day HFIM, a C/T-resistant subpopulation emerged in the susceptible isolate after exposure to the C/T Css of 20 mg/L. Resistance emerged on day 6 at concentrations of 2-, 4-, and eightfold the MIC, and resulted in 1 CFU/mL in 1.6 × 109, 7.8 × 1010, and 3.9 × 1010, respectively. The C/T MIC was ≥ 256 mg/L. Compared to the original population, the resistant subpopulation had a lower meropenem MIC (8 vs 16 mg/L) and a lower imipenem MIC (2 vs 8 mg/L). The analysis of mutations within a set of genes involved in antibiotic resistance compared with those already present in the parental isolate (sequencing of blaAmpC gene) revealed a 19-amino acid deletion (K232-G250) in the Ω-loop of AmpC, which has been associated with C/T resistance25. No resistant subpopulations were detected following exposure to C/T in CI at a Css of 45 mg/L (Fig. 3).
Drug concentrations
The relationship between observed and predicted C/T concentrations is shown in the Supplemental Material. We assessed the agreement between observed results and predicted results with the Bland–Altman plot. For Css 45 and 80 mg/L difference values have less than a 1.96 of standard deviation (SD) from the mean. On the other hand, for Css 20 mg/L one of the 15 values deviates slightly from 1.96 SD.
Discussion
Optimization of antibiotic treatments based on PK/PD properties is essential in MDR/XDR P. aeruginosa infections. C/T has emerged as a promising option in this setting18. The standard C/T dose in intermittent infusion regimens can be optimized in high-inoculum infections, but CI may be a better option for achieving PK/PD targets. Our HFIM study compared different Css of C/T in CI against three XDR P. aeruginosa ST175 isolates with C/T MICs ranging from 2 to 16 mg/L. The criteria for selecting C/T dosages were to compare lower and higher Css from different doses of C/T that are recommended for difficult-to-treat infections. The ST175 clone was selected because it is the most prevalent in our environment and it has been associated with MDR/XDR isolates involved in nosocomial infections8.
Few studies have evaluated C/T infusion dosing in the clinical practice. Pilmis et al.26 compared intermittent infusion and CI in patients with MDR P. aeruginosa infections, and concluded that the current recommended dosing regimen provided unsatisfactory coverage. Another Monte Carlo simulations found that extending the duration of C/T infusion improved the probability of target attainment in the treatment of infections caused by MDR P. aeruginosa strains with different C/T MICs in patients with different renal functions levels15. These results are in consonance with our previous experiments in which different type of infusion (1 h, 4 h and CI) were examined against the same three P. aeruginosa isolates. In summary, these studies showed that the CI regimen achieved the highest bacterial reduction even against non-susceptible isolates (an overall reduction of − 4.95 log10 CFU/ml for the CI infusion versus a reduction of − 1.87 and − 2.78 for the 1 h and 4 h infusion, respectively)27. Sime et al.11 described the population PKs of unbound C/T and evaluated the adequacy of recommended dosing regimens in critically ill patients without renal impairment. They concluded that a loading dose of 1 g/0.5 g followed by 3 g/1.5 g in CI was adequate for empirical coverage of a T > MIC target of 100%. In our study, however, CI of 3 g of ceftolozane resulted in the emergence of C/T resistance, indicating that dosing according to PK/PD parameters is important for improving clinical management.
The administration of C/T at a Css of 45 mg/L achieved a reduction in bacterial density in both susceptible and resistant isolates. It also exerted a bactericidal effect regardless of the C/T MICs of the isolates. This sustained suppression of bacterial growth suggests that C/T in CI may achieve concentrations above the susceptibility breakpoint for a longer period of time. This would be particularly important for P. aeruginosa isolates with higher C/T MIC values.
Optimization of Css in a CI regimen is necessary to achieve an optimal therapeutic effect. A retrospective study analyzing the performance of C/T in patients with XDR P. aeruginosa infections, most of whom were receiving CI, found that 66% achieved supratherapeutic levels28. These results highlight the importance of monitoring C/T plasma concentrations when aiming to optimize treatment28. We performed a 10-day HFIM study to determine whether a low CI C/T dosing regimen would be as effective as the standard regimen against the C/T-susceptible isolate ST175 (10-023) or possibly contribute to the selection of C/T-resistant subpopulations. We found that a Css of 20 mg/L clearly failed to prevent the emergence of resistance, whereas a Css of 45 mg/L had a bactericidal effect. Sequencing of blaAmpC gene in the resistant subpopulation that emerged revealed a 19-amino acid deletion (K232-G250) in the Ω-loop of AmpC, supporting previous reports of a link to C/T resistance25. The C/T-resistant subpopulation was also associated with a decrease in meropenem and imipenem MIC values. This phenomenon of partial reversal of carbapenem resistance concomitant with the acquisition of C/T resistance has been previously reported25. Bacterial antibiotic susceptibility is therefore dynamic and may be influenced by a gain of resistance in other antibiotics29.
Infections caused by P. aeruginosa isolates with C/T MIC values above 2 mg/L have been associated with poor outcomes when treated with a standard C/T dosing regimen30. The use of higher doses (up to 6 g/3 g every 24 h), mainly against non-susceptible strains, has not been found to produce adverse effects11. In this context, we evaluated a CI C/T regimen with a Css of 80 mg/L as an option for optimizing the treatment of infections caused by resistant P. aeruginosa strains. Our results showed that this higher dose displays a slight advantage than the currently recommended regimen, particularly in the case of the isolate with the intermediate C/T MIC, in which the eradication of the bacterial population was achieved.
This study had some limitations. First, we only studied three P. aeruginosa isolates, although they are representative of the different ranges of C/T susceptibility in our environment. Second, despite the use of clinical parameters, we were unable to examine toxicity and infection site effects in vitro, or to determine the contribution of the immune system to bacterial killing, as host immunity could, to a certain extent, modify PD targets. Nonetheless, this absence of immunity means our findings can be extrapolated to immunocompromised patients. Finally, it should be clarified that exposure to tazobactam was not considered although it has a limited role in ceftolozane’s activity against P. aeruginosa.
In summary, our results show that C/T in CI at Css of 45 mg/L leads to a decrease in bacterial burden in P. aeruginosa and is useful against non-susceptible isolates (with a MIC of 8 and 16 mg/L). CI at a Css of 80 mg/L had the strongest bactericidal effect. Administration of the suboptimal Css of 20 mg/L resulted in the emergence of C/T resistance in the susceptible isolate (MIC 2 mg/L). Antimicrobial regimens can be individually optimized by adjusting antibiotic doses to both C/T MIC values and PK/PD targets. Therapeutic drug monitoring would favour better clinical management and help prevent the emergence of antibiotic resistance.
References
Hwang, W. & Yoon, S. S. Virulence characteristics and an action mode of antibiotic resistance in multidrug-resistant Pseudomonas aeruginosa. Sci. Rep. 9, 1–15. https://doi.org/10.1038/s41598-018-37422-9 (2019).
Pendleton, J. N., Gorman, S. P. & Gilmore, B. F. Clinical relevance of the ESKAPE pathogens. Expert Rev. Anti. Infect. Ther. 11, 297–308. https://doi.org/10.1586/eri.13.12 (2013).
Díaz-Cañestro, M. et al. Ceftolozane/tazobactam for the treatment of multidrug resistant Pseudomonas aeruginosa: experience from the Balearic Islands. Eur. J. Clin. Microbiol. Infect. Dis. 37, 2191–2200. https://doi.org/10.1007/s10096-018-3361-0 (2018).
Oliver, A., Mulet, X., López-Causapé, C. & Juan, C. The increasing threat of Pseudomonas aeruginosa high-risk clones. Drug Resist. Updat. 21–22, 41–59. https://doi.org/10.1016/j.drup.2015.08.002 (2015).
Subedi, D., Vijay, A. K. & Willcox, M. Overview of mechanisms of antibiotic resistance in Pseudomonas aeruginosa: an ocular perspective. Clin. Exp. Optom. 1(101), 162–171. https://doi.org/10.1111/cxo.12621 (2018).
Hong, M. C., Hsu, D. I. & Bounthavong, M. Ceftolozane/tazobactam: A novel antipseudomonal cephalosporin and β-lactamase-inhibitor combination. Infect. Drug Resist. 6, 215–223. https://doi.org/10.2147/IDR.S36140 (2013).
Monogue, M. L. & Nicolau, D. P. Antibacterial activity of ceftolozane/tazobactam alone and in combination with other antimicrobial agents against MDR Pseudomonas aeruginosa. J. Antimicrob. Chemother. 73, 942–952. https://doi.org/10.1093/jac/dkx483 (2018).
Bergen, P. J. et al. Synergistic killing of multidrug-resistant Pseudomonas aeruginosa at multiple inocula by colistin combined with doripenem in an in vitro pharmacokinetic/pharmacodynamic model. Antimicrob. Agents Chemother. 55, 5685–5695. https://doi.org/10.1128/AAC.05298-11 (2011).
Papp-Wallace, K. M. & Bonomo, R. A. New β-lactamase inhibitors in the clinic. Infect. Dis. Clin. North Am. 30, 441–464. https://doi.org/10.1016/j.idc.2016.02.007 (2016).
Farrell, D. J., Flamm, R. K., Sader, H. S. & Jones, R. N. Antimicrobial activity of ceftolozane-tazobactam tested against Enterobacteriaceae and Pseudomonas aeruginosa with various resistance patterns isolated in US hospitals (2011–2012). Antimicrob. Agents Chemother. 57, 6305–6310. https://doi.org/10.1128/AAC.01802-13 (2013).
Sime, F. B. et al. Population pharmacokinetics of unbound ceftolozane and tazobactam in critically ill patients without renal dysfunction. Antimicrob. Agents Chemother. 63, 1–12. https://doi.org/10.1128/AAC.01265-19 (2019).
Sorbera, M., Chung, E., Ho, C. W. & Marzella, N. Ceftolozane/tazobactam: A new option in the treatment of complicated gram-negative infections. P T 39, 825–832 (2014).
Macgowan, A. P., Noel, A. R., Tomaselli, S. G., Nicholls, D. & Bowker, K. E. Pharmacodynamics of ceftolozane plus tazobactam studied in an in vitro pharmacokinetic model of infection. Antimicrob Agents Chemother. https://doi.org/10.1128/AAC.00727-15 (2015).
Craig, W. A. & Andes, D. R. In vivo activities of ceftolozane, a new cephalosporin, with and without tazobactam against pseudomonas aeruginosa and enterobacteriaceae, including strains with extended-spectrum-lactamases, in the thighs of neutropenic mice. Antimicrob. Agents Chemother. https://doi.org/10.1128/AAC.01590-12 (2013).
Natesan, S., Pai, M. P. & Lodise, T. P. Determination of alternative ceftolozane/tazobactam dosing regimens for patients with infections due to Pseudomonas aeruginosa with MIC values between 4 and 32 mg/L. J. Antimicrob. Chemother. 1(72), 2813–2816. https://doi.org/10.1093/jac/dkx221 (2017).
del Barrio-Tofiño, E. et al. Genomics and susceptibility profiles of extensively drug-resistant Pseudomonas aeruginosa isolates from Spain. Antimicrob. Agents Chemother. 61, e01589-e1617. https://doi.org/10.1128/AAC.01589-17 (2017).
Sime, F. B. et al. A population pharmacokinetic model-guided evaluation of ceftolozane-tazobactam dosing in critically ill patients undergoing continuous venovenous hemodiafiltration. Antimicrob. Agents Chemother. 64, 1–11. https://doi.org/10.1128/AAC.01655-19 (2020).
Montero, M. et al. Evaluation of ceftolozane-tazobactam in combination with meropenem against pseudomonas aeruginosa sequence type 175 in a hollow-fiber infection model. Antimicrob. Agents Chemother. 62, 1–6. https://doi.org/10.1128/AAC.00026-18 (2018).
VanScoy, B. D. et al. Relationship between ceftolozane-tazobactam exposure and selection for Pseudomonas aeruginosa resistance in a hollow-fiber infection model. Antimicrob. Agents Chemother. 58, 6024–6031. https://doi.org/10.1128/AAC.02310-13 (2014).
Zhanel, G. G. et al. Ceftolozane/tazobactam: a novel cephalosporin/β-lactamase inhibitor combination with activity against multidrug-resistant gram-negative bacilli. Drugs 74, 31–51. https://doi.org/10.1007/s40265-013-0168-2 (2014).
Sutherland, C. A. & Nicolau, D. P. Development of an HPLC method for the determination of ceftolozane/tazobactam in biological and aqueous matrixes. J. Chromatogr. Sci. 54, 1037–1040. https://doi.org/10.1093/chromsci/bmw047 (2016).
Bulitta, J. B. et al. Generating robust and informative nonclinical in vitro and in vivo bacterial infection model efficacy data to support translation to humans. Antimicrob. Agents Chemother. 63, 1–25. https://doi.org/10.1128/AAC.02307-18 (2019).
Montero, M. et al. Efficacy of ceftolozane/tazobactam in combination with colistin against extensively drug-resistant pseudomonas aeruginosa including high risk clones in an in vitro pharmacodynamic model. Antimicrob. Agents Chemother. 10(64), e02542-e2619. https://doi.org/10.1128/AAC.02542-19 (2020).
Patel, J. B. et al. Performance standards for antimicrobial susceptibility testing. Antimicrob. Agents Chemother. https://doi.org/10.1016/S0196-4399(01)88009-0 (2019).
Cabot, G. et al. Pseudomonas aeruginosa Ceftolozane-Tazobactam resistance development requires multiple mutations leading to overexpression and structural modification of AmpC. Antimicrob. Agents Chemother. 1(58), 3091–3099. https://doi.org/10.1128/AAC.02462-13 (2014).
Pilmis, B. et al. Continuous infusion of ceftolozane/tazobactam is associated with a higher probability of target attainment in patients infected with Pseudomonas aeruginosa. Eur. J. Clin. Microbiol. Infect. Dis. 9(38), 1457–1461. https://doi.org/10.1007/s10096-019-03573-4 (2019).
Montero, M., Domene-Ochoa, S., López-Causapé, C., VanScoy, D. B., Luque, S., Sorli, L., et al. Impact of alternative dosing infusions of ceftolozane-tazobactam monotherapy against extremely-resistant (XDR) Pseudomonas aeruginosa Sequence Type 175 isolates with different susceptibility profile ranging from 2 to 16 mg/L in a Hollow-Fiber Infection Mo. ECCMID abstr 2020;abstr 5312.
Navarrete, M.E., Luque, S.M.M. et al., Optimal PK/PD target and high efficacy rates of ceftolozane-tazobactam in patients with infections caused by extensively drug-resistant Pseudomonas aeruginosa, abstr 2946. ECCMID abstr 2020. 2020;
Allen, R. C., Engelstädter, J., Bonhoeffer, S., McDonald, B. A. & Hall, A. R. Reversing resistance: different routes and common themes across pathogens. Proc. R. Soc. B Biol. Sci. 27(284), 20171619. https://doi.org/10.1098/rspb.2017.1619 (2017).
Rodríguez-Núñez, O. et al. Higher MICs (>2 mg/L) predict 30-day mortality in patients with lower respiratory tract infections caused by multidrug- and extensively drug-resistant Pseudomonas aeruginosa treated with ceftolozane/tazobactam. Open Forum Infect. Dis. 6, 1–7. https://doi.org/10.1093/ofid/ofz416 (2019).
Acknowledgements
We thank The Institute for Clinical Pharmacodynamics (ICPD), Schenectady, NY, and the Infectious Pathology and Antimicrobials Research Group (IPAR), Institute Hospital del Mar d’Investigacions Mèdiques (IMIM), for their support.
Funding
This study was partially supported by the Ministerio de Economía y Competitividad of Spain, Instituto de Salud Carlos III. FEDER PI16/00669, PI17/00251, PI18/0076 and the Spanish Network for Research in Infectious Diseases (REIPI RD16/0016).
Author information
Authors and Affiliations
Contributions
Conceptualization: M.M.M.; Methodology: M.M.M., S.D., N.P., L.F. A.; Formal analysis and investigation: M.M.M., S.D.; Writing—original draft preparation: M.M.M., S.D., L.F.A., A.A.-B.; Writing—review and editing: all authors; Funding acquisition: M.M.M., J.P.H.; Supervision: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Montero, M.M., Domene-Ochoa, S., López-Causapé, C. et al. Impact of ceftolozane/tazobactam concentrations in continuous infusion against extensively drug-resistant Pseudomonas aeruginosa isolates in a hollow-fiber infection model. Sci Rep 11, 22178 (2021). https://doi.org/10.1038/s41598-021-01784-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-01784-4
This article is cited by
-
Recent advances in therapeutic targets identification and development of treatment strategies towards Pseudomonas aeruginosa infections
BMC Microbiology (2023)
-
New Ni(II) and Pd(II) complexes bearing derived sulfa drug ligands: synthesis, characterization, DFT calculations, and in silico and in vitro biological activity studies
BioMetals (2023)
-
Use of WATCH antibiotics prior to presentation to the hospital in rural Burkina Faso
Antimicrobial Resistance & Infection Control (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.