Key Points
-
Kidney disorders associated with haematological malignancies can result from the disease process itself, complications of therapy or direct toxicity of chemotherapeutic agents
-
New therapies for haematological malignancies are associated with renal toxicity, which is not commonly seen with older treatment regimens
-
Acute kidney injury is common among patients with multiple myeloma, leukaemia or lymphoma, and negatively influences the prognosis of these patients
-
Glomerular diseases are rare manifestations of haematological malignancies, can precede or follow diagnosis of the malignancy, and can have a wide range of histopathological features
-
Volume expansion and lowering of serum uric acid can prevent the consequences of tumour lysis syndrome; once the condition is established, close attention must be paid to life-threatening acid–base and electrolyte disorders
-
Chronic kidney disease has emerged as an important consequence of haematopoietic stem cell and bone marrow transplantation
Abstract
Advances in chemotherapy for haematological malignancies, resulting from a greater understanding of the complex pathophysiology of these diseases, have improved the survival of patients with these disorders. Clinicians must now, therefore, be more aware of the issues related to fluid, electrolyte, and acid–base disorders, as well as acute and chronic kidney injuries that can develop in such patients as a result of the underlying malignancy and its treatment. Patients with acute kidney injury associated with haematological malignancy have a worse prognosis than do other patients with acute kidney injury. Glomerular diseases associated with haematological malignancies are thought to be paraneoplastic syndromes with variable histological presentations. Some of the newest therapeutic agents used to treat haematological malignancies have adverse renal effects that can preclude continuation of treatment, often leading to difficult clinical decisions when patients have advanced disease and alternative treatment options are limited. Haematopoietic stem cell transplantation has an expanding role as a therapy for haematological malignancies but is also associated with important renal complications. Here, we review the literature that examines the incidences, aetiologies, mechanisms and treatment options for renal disorders associated with haematological malignancies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Rodriguez-Abreu, D., Bordoni, A. & Zucca, E. Epidemiology of hematological malignancies. Ann. Oncol. 18 (Suppl. 1), i3–i8 (2007).
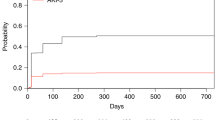
Canet, E. et al. Acute kidney injury in patients with newly diagnosed high-grade hematological malignancies: impact on remission and survival. PLoS ONE 8, e55870 (2013).
Hutchison, C. A. et al. The pathogenesis and diagnosis of acute kidney injury in multiple myeloma. Nat. Rev. Nephrol. 8, 43–51 (2011).
Hutchison, C. A. et al. Novel approaches for reducing free light chains in patients with myeloma kidney. Nat. Rev. Nephrol. 8, 234–243 (2012).
Bagshaw, S. M. et al. Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: a population-based study. Crit. Care 9, R700–R709 (2005).
Salahudeen, A. K. et al. Incidence rate, clinical correlates, and outcomes of AKI in patients admitted to a comprehensive cancer center. Clin. J. Am. Soc. Nephrol. 8, 347–354 (2013).
de Mendonça, A. et al. Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med. 26, 915–921 (2000).
Christiansen, C. F., Johansen, M. B., Langeberg, W. J., Fryzek, J. P. & Sørensen, H. T. Incidence of acute kidney injury in cancer patients: a Danish population-based cohort study. Eur. J. Intern. Med. 22, 399–406 (2011).
Lahoti, A. et al. Predictors and outcome of acute kidney injury in patients with acute myelogenous leukemia or high-risk myelodysplastic syndrome. Cancer 116, 4063–4068 (2010).
Munker, R., Hill, U., Jehn, U., Kolb, H. J. & Schalhorn, A. Renal complications in acute leukemias. Haematologica 83, 416–421 (1998).
Khalil, M. A. et al. Acute kidney injury in lymphoma: a single centre experience. Int. J. Nephrol. 2014, 272961 (2014).
Li, S. J. et al. Renal involvement in non-Hodgkin lymphoma: proven by renal biopsy. PLoS ONE 9, e95190 (2014).
Luciano, R. L. & Brewster, U. C. Kidney involvement in leukemia and lymphoma. Adv. Chronic Kidney Dis. 21, 27–35 (2014).
Aström, M., Bodin, L., Hörnsten, P., Wahlin, A. & Tidefelt, U. Evidence for a bimodal relation between serum lysozyme and prognosis in 232 patients with acute myeloid leukaemia. Eur. J. Haematol. 70, 26–33 (2003).
Levinson, S. S., Elin, R. J. & Yam, L. Light chain proteinuria and lysozymuria in a patient with acute monocytic leukemia. Clin. Chem. 48, 1131–1132 (2002).
Patel, T. V., Rennke, H. G., Sloan, J. M., DeAngelo, D. J. & Charytan, D. M. A forgotten cause of kidney injury in chronic myelomonocytic leukemia. Am. J. Kidney Dis. 54, 159–164 (2009).
Soares, M., Feres, G. A. & Salluh, J. I. Systemic inflammatory response syndrome and multiple organ dysfunction in patients with acute tumor lysis syndrome. Clinics (Sao Paulo) 64, 479–481 (2009).
Kochenderfer, J. N. et al. B-cell depletion and remissions of malignancy along with cytokine-associated toxicity in a clinical trial of anti-CD19 chimeric-antigen-receptor-transduced T cells. Blood 119, 2709–2720 (2012).
Montesinos, P. et al. Differentiation syndrome in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and anthracycline chemotherapy: characteristics, outcome, and prognostic factors. Blood 113, 775–783 (2009).
Patatanian, E. & Thompson, D. F. Retinoic acid syndrome: a review. J. Clin. Pharm. Ther. 33, 331–338 (2008).
Tallman, M. S. & Altman, J. K. How I treat acute promyelocytic leukemia. Blood 114, 5126–5135 (2009).
Ramos-Casals, M., Brito-Zerón, P., López-Guillermo, A., Khamashta, M. A. & Bosch, X. Adult haemophagocytic syndrome. Lancet 383, 1503–1516 (2014).
Holt, S. et al. Cytokine nephropathy and multi-organ dysfunction in lymphoma. Nephrol. Dial. Transplant. 13, 1853–1857 (1998).
Henter, J. I. et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr. Blood Cancer 48, 124–131 (2007).
Levin, M. D., Betjes, M. G., van der Kwast, T. H., Wenberg, B. L. & Leebeek, F. W. Acute renal cortex necrosis caused by arterial thrombosis during treatment for acute promyelocytic leukemia. Haematologica 88, ECR21 (2003).
Porcu, P. et al. Hyperleukocytic leukemias and leukostasis: a review of pathophysiology, clinical presentation and management. Leuk. Lymphoma 39, 1–18 (2000).
Murray, J. C., Dorfman, S. R., Brandt, M. L. & Dreyer, Z. E. Renal venous thrombosis complicating acute myeloid leukemia with hyperleukocytosis. J. Pediatr. Hematol. Oncol. 18, 327–330 (1996).
Zuckerman, T., Ganzel, C., Tallman, M. S. & Rowe, J. M. How I treat hematologic emergencies in adults with acute leukemia. Blood 120, 1993–2002 (2012).
Chong, B. H., Trew, P., Meng, L. & Pitney, W. R. Anuric renal failure due to encasement of the ureters by lymphoma—ureteric obstruction without dilatation. Aust. N. Z. J. Med. 11, 542–544 (1981).
Richmond, J., Sherman, R. S., Diamond, H. D. & Craver, L. F. Renal lesions associated with malignant lymphomas. Am. J. Med. 32, 184–207 (1962).
Cvetkovic, Z. P., Cvetkovic, B. R., Celeketic, D., Milenkovic, D. & Perunicic-Pekovic, G. Bilateral ureteral obstruction due to primary myelofibrosis caused hyperuricaemia. Acta Chir. Iugosl. 57, 79–83 (2010).
Davidson, M. B. et al. Pathophysiology, clinical consequences, and treatment of tumor lysis syndrome. Am. J. Med. 116, 546–554 (2004).
Cohen, L. F., Balow, J. E., Magrath, I. T., Poplack, D. G. & Ziegler, J. L. Acute tumor lysis syndrome. A review of 37 patients with Burkitt's lymphoma. Am. J. Med. 68, 486–491 (1980).
Wilson, F. P. & Berns, J. S. Tumor lysis syndrome: new challenges and recent advances. Adv. Chronic Kidney Dis. 21, 18–26 (2014).
Montesinos, P. et al. Tumor lysis syndrome in patients with acute myeloid leukemia: identification of risk factors and development of a predictive model. Haematologica 93, 67–74 (2008).
Coiffier, B., Altman, A., Pui, C. H., Younes, A. & Cairo, M. S. Guidelines for the management of pediatric and adult tumor lysis syndrome: an evidence-based review. J. Clin. Oncol. 26, 2767–2778 (2008).
Cairo, M. S. & Bishop, M. Tumour lysis syndrome: new therapeutic strategies and classification. Br. J. Haematol. 127, 3–11 (2004).
Cairo, M. S., Coiffier, B., Reiter, A., Younes, A. & TLS Expert Panel. Recommendations for the evaluation of risk and prophylaxis of tumour lysis syndrome (TLS) in adults and children with malignant diseases: an expert TLS panel consensus. Br. J. Haematol. 149, 578–586 (2010).
Riccio, B., Mato, A., Olson, E. M., Berns, J. S. & Luger, S. Spontaneous tumor lysis syndrome in acute myeloid leukemia: two cases and a review of the literature. Cancer Biol. Ther. 5, 1614–1617 (2006).
Kjellstrand, C. M., Cambell, D. C. 2nd, von Hartitzsch, B. & Buselmeier, T. J. Hyperuricemic acute renal failure. Arch. Intern. Med. 133, 349–359 (1974).
Conger, J. D. & Falk, S. A. Intrarenal dynamics in the pathogenesis and prevention of acute urate nephropathy. J. Clin. Invest. 59, 786–793 (1977).
Vadhan-Raj, S. et al. A randomized trial of a single-dose rasburicase versus five-daily doses in patients at risk for tumor lysis syndrome. Ann. Oncol. 23, 1640–1645 (2012).
Feng, X. et al. Efficacy and cost of single-dose rasburicase in prevention and treatment of adult tumour lysis syndrome: a meta-analysis. J. Clin. Pharm. Ther. 38, 301–308 (2013).
Lopez-Olivo, M. A., Pratt, G., Palla, S. L. & Salahudeen, A. Rasburicase in tumor lysis syndrome of the adult: a systematic review and meta-analysis. Am. J. Kidney Dis. 62, 481–492 (2013).
Sakarcan, A. & Quigley, R. Hyperphosphatemia in tumor lysis syndrome: the role of hemodialysis and continuous veno-venous hemofiltration. Pediatr. Nephrol. 8, 351–353 (1994).
Agha-Razii, M. et al. Continuous veno-venous hemodiafiltration for the treatment of spontaneous tumor lysis syndrome complicated by acute renal failure and severe hyperuricemia. Clin. Nephrol. 54, 59–63 (2000).
Obrador, G. T., Price, B., O'Meara, Y. & Salant, D. J. Acute renal failure due to lymphomatous infiltration of the kidneys. J. Am. Soc. Nephrol. 8, 1348–1354 (1997).
Da'as, N. et al. Kidney involvement and renal manifestations in non-Hodgkin's lymphoma and lymphocytic leukemia: a retrospective study in 700 patients. Eur. J. Haematol. 67, 158–164 (2001).
Porcaro, A. B. et al. Primary lymphoma of the kidney. Report of a case and update of the literature. Arch. Ital. Urol. Androl. 74, 44–47 (2002).
Shirali, A. C. & Perazella, M. A. Tubulointerstitial injury associated with chemotherapeutic agents. Adv. Chronic Kidney Dis. 21, 56–63 (2014).
Perazella, M. A. & Moeckel, G. W. Nephrotoxicity from chemotherapeutic agents: clinical manifestations, pathobiology, and prevention/therapy. Semin. Nephrol. 30, 570–581 (2010).
Faruque, L. I. et al. Systematic review of the risk of adverse outcomes associated with vascular endothelial growth factor inhibitors for the treatment of cancer. PLoS ONE 9, e101145 (2014).
Gafter-Gvili, A., Ram, R., Gafter, U., Shpilberg, O. & Raanani, P. Renal failure associated with tyrosine kinase inhibitors—case report and review of the literature. Leuk. Res. 34, 123–127 (2010).
Jhaveri, K. D., Flombaum, C. D., Kroog, G. & Glezerman, I. G. Nephrotoxicities associated with the use of tyrosine kinase inhibitors: a single-center experience and review of the literature. Nephron Clin. Pract. 117, c312–c319 (2011).
Kumar, N. & Shirali, A. C. What is the best therapy for toxicity in the setting of methotrexate-associated acute kidney injury: high-flux hemodialysis or carboxypeptidase G2? Semin. Dial. 27, 226–228 (2014).
Widemann, B. C. et al. Efficacy of glucarpidase (carboxypeptidase g2) in patients with acute kidney injury after high-dose methotrexate therapy. Pharmacotherapy 34, 427–439 (2014).
Filippatos, T. D., Milionis, H. J. & Elisaf, M. S. Alterations in electrolyte equilibrium in patients with acute leukemia. Eur. J. Haematol. 75, 449–460 (2005).
Lantz, B., Carlmark, B. & Reizenstein, P. Electrolytes and whole body potassium in acute leukemia. Acta Med. Scand. 206, 45–50 (1979).
Milionis, H. J., Bourantas, C. L., Siamopoulos, K. C. & Elisaf, M. S. Acid-base and electrolyte abnormalities in patients with acute leukemia. Am. J. Hematol. 62, 201–207 (1999).
Olgar, S., Yetgin, S., Cetin, M., Aras, T. & Akhan, O. Electrolyte abnormalities at diagnosis of acute lymphocytic leukemia may be a clue for renal damage in long-term period. J. Pediatr. Hematol. Oncol. 27, 202–206 (2005).
Uribarri, J., Oh, M. S. & Carroll, H. J. Salt-losing nephropathy. Clinical presentation and mechanisms. Am. J. Nephrol. 3, 193–198 (1983).
Dhaliwal, H. S. et al. Combination chemotherapy for intermediate and high grade non-Hodgkin's lymphoma. Br. J. Cancer 68, 767–774 (1993).
Nakamura, F., Kishimoto, Y., Handa, T., Arai, Y. & Mitani, K. Myelodysplastic syndrome with central diabetes insipidus manifesting hypodipsic hypernatremia and dehydration. Am. J. Hematol. 75, 213–216 (2004).
de la Chapelle, A. & Lahtinen, R. Monosomy 7 predisposes to diabetes insipidus in leukaemia and myelodysplastic syndrome. Eur. J. Haematol. 39, 404–411 (1987).
Dickenmann, M. J. & Brunner, F. P. Hypernatraemia and polyuria in a patient with acute myeloid leukaemia and allogeneic bone marrow transplant. Nephrol. Dial. Transplant. 13, 2687–2689 (1998).
O'Regan, S., Carson, S., Chesney, R. W. & Drummond, K. N. Electrolyte and acid-base disturbances in the management of leukemia. Blood 49, 345–353 (1977).
Elisaf, M. S., Burads, K. & Siamopoulos, K. C. Pronounced electrolyte abnormalities in a patient with acute leukemia. Haematologica 82, 384 (1997).
Young, I. S., Bailie, K. & Trimble, E. R. Severe hypophosphataemia in a patient with acute leukaemia. Ann. Clin. Biochem. 30, 326–328 (1993).
Vachvanichsanong, P., Maipang, M., Dissaneewate, P., Wongchanchailert, M. & Laosombat, V. Severe hyperphosphatemia following acute tumor lysis syndrome. Med. Pediatr. Oncol. 24, 63–66 (1995).
Peter, S. A. & Cervantes, J. F. Hypercalcemia associated with adult T-cell leukemia/lymphoma (ATL). J. Natl Med. Assoc. 87, 746–748 (1995).
Vlasveld, L. T. et al. Parathyroid hormone-related protein (PTH-rP)-associated hypercalcemia in a patient with an atypical chronic lymphocytic leukemia. Neth. J. Med. 54, 21–26 (1999).
Kumar, S., Mow, B. M. & Kaufmann, S. H. Hypercalcemia complicating leukemic transformation of agnogenic myeloid metaplasia-myelofibrosis. Mayo Clin. Proc. 74, 1233–1237 (1999).
McKee, L. C. Jr. Hypocalcemia in leukemia. South. Med. J. 68, 828–832 (1975).
Le Prise, P. Y., Oudry, B. & Richier, J. L. Letter: Phosphate metabolism disorder in a case of acute lymphoblastic leukemia. Initial hypophosphoremia. [French] Nouv. Presse Med. 3, 896 (1974).
Zamkoff, K. W. & Kirshner, J. J. Marked hypophosphatemia associated with acute myelomonocytic leukemia. Indirect evidence of phosphorus uptake by leukemic cells. Arch. Intern. Med. 140, 1523–1524 (1980).
Seymour, J. F. & Gagel, R. F. Calcitriol: the major humoral mediator of hypercalcemia in Hodgkin's disease and non-Hodgkin's lymphomas. Blood 82, 1383–1394 (1993).
Kintzel, P. E. & Scott, W. L. Pseudohyperkalemia in a patient with chronic lymphoblastic leukemia and tumor lysis syndrome. J. Oncol. Pharm. Pract. 18, 432–435 (2012).
Mir, M. A. & Delamore, I. W. Metabolic disorders in acute myeloid leukaemia. Br. J. Haematol. 40, 79–92 (1978).
Ruiz, J. P., Singh, A. K. & Hart, P. Type B lactic acidosis secondary to malignancy: case report, review of published cases, insights into pathogenesis, and prospects for therapy. ScientificWorldJournal 11, 1316–1324 (2011).
Jhaveri, K. D., Shah, H. H., Calderon, K., Campenot, E. S. & Radhakrishnan, J. Glomerular diseases seen with cancer and chemotherapy: a narrative review. Kidney Int. 84, 34–44 (2013).
Audard, V. et al. Minimal change nephrotic syndrome and classical Hodgkin's lymphoma: report of 21 cases and review of the literature. Kidney Int. 69, 2251–2260 (2006).
Mallouk, A., Pham, P. T. & Pham, P. C. Concurrent FSGS and Hodgkin's lymphoma: case report and literature review on the link between nephrotic glomerulopathies and hematological malignancies. Clin. Exp. Nephrol. 10, 284–289 (2006).
Lai, K. W. et al. Overexpression of interleukin-13 induces minimal-change-like nephropathy in rats. J. Am. Soc. Nephrol. 18, 1476–1485 (2007).
Audard, V. et al. Occurrence of minimal change nephrotic syndrome in classical Hodgkin lymphoma is closely related to the induction of c-mip in Hodgkin-Reed Sternberg cells and podocytes. Blood 115, 3756–3762 (2010).
Iwama, H., Horikoshi, S., Shirato, I. & Tomino, Y. Epstein–Barr virus detection in kidney biopsy specimens correlates with glomerular mesangial injury. Am. J. Kidney Dis. 32, 785–793 (1998).
Kratochvil, D., Amann, K., Bruck, H. & Büttner, M. Membranoproliferative glomerulonephritis complicating Waldenström's macroglobulinemia. BMC Nephrol. 13, 172 (2012).
Morel-Maroger, L., Basch, A., Danon, F., Verroust, P. & Richet, G. Pathology of the kidney in Waldenström's macroglobulinemia. Study of sixteen cases. N. Engl. J. Med. 283, 123–129 (1970).
Telio, D. et al. Two distinct syndromes of lymphoma-associated AL amyloidosis: a case series and review of the literature. Am. J. Hematol. 85, 805–808 (2010).
Bhatia, M., Kher, K. & Minniti, C. P. Acute lymphoblastic leukemia in a child with nephrotic syndrome. Pediatr. Nephrol. 19, 1290–1293 (2004).
Levi, I., Dinour, D., Ben-Bassat, I. & Raanani, P. Acute myeloid leukemia associated with nephrotic syndrome: case report and literature review. Leuk. Lymphoma 43, 1133–1136 (2002).
Cambier, J. F. & Ronco, P. Onco-nephrology: glomerular diseases with cancer. Clin. J. Am. Soc. Nephrol. 7, 1701–1712 (2012).
Moulin, B. et al. Glomerulonephritis in chronic lymphocytic leukemia and related B-cell lymphomas. Kidney Int. 42, 127–135 (1992).
Brouet, J. C., Clauvel, J. P., Danon, F., Klein, M. & Seligmann, M. Biologic and clinical significance of cryoglobulins. A report of 86 cases. Am. J. Med. 57, 775–788 (1974).
Budak-Alpdogan, T., Lawrence, R. A., Bayik, M. & Akoglu, E. Nephrotic syndrome associated with alpha interferon therapy in chronic myeloid leukemia. Clin. Nephrol. 48, 59–60 (1997).
Tsutsumi, C. et al. Membranous nephropathy after allogeneic stem cell transplantation: report of 2 cases. Int. J. Hematol. 79, 193–197 (2004).
Agarwal, R. G., Gupta, K. D. & Bharadwaj, T. P. Nephrotic syndrome in the possible terminal blast-cell crisis in myeloid leukaemia (a case report). J. Assoc. Physicians India 20, 799–801 (1972).
Talwar, R., Dash, S. C. & Kucheria, K. A case of chronic myeloid leukemia complicated with minimal change nephrotic syndrome. Acta Haematol. 109, 101–103 (2003).
Said, S. M. et al. Myeloproliferative neoplasms cause glomerulopathy. Kidney Int. 80, 753–759 (2011).
Ruiz-Ortega, M., Largo, R., Bustos, C., Gómez-Garre, D. & Egido, J. Platelet-activating factor stimulates gene expression and synthesis of matrix proteins in cultured rat and human mesangial cells: role of TGF-β. J. Am. Soc. Nephrol. 8, 1266–1275 (1997).
Bogdanovic, R. et al. Glomerular involvement in myelodysplastic syndromes. Pediatr. Nephrol. 16, 1053–1057 (2001).
Sawinski, D. The kidney effects of hematopoietic stem cell transplantation. Adv. Chronic Kidney Dis. 21, 96–105 (2014).
Remberger, M. et al. Improved survival after allogeneic hematopoietic stem cell transplantation in recent years. A single-center study. Biol. Blood Marrow Transplant. 17, 1688–1697 (2011).
Zager, R. A. et al. Acute renal failure following bone marrow transplantation: a retrospective study of 272 patients. Am. J. Kidney Dis. 13, 210–216 (1989).
Parikh, C. R. et al. Renal dysfunction in allogeneic hematopoietic cell transplantation. Kidney Int. 62, 566–573 (2002).
Kogon, A. & Hingorani, S. Acute kidney injury in hematopoietic cell transplantation. Semin. Nephrol. 30, 615–626 (2010).
Schrier, R. W. & Parikh, C. R. Comparison of renal injury in myeloablative autologous, myeloablative allogeneic and non-myeloablative allogeneic haematopoietic cell transplantation. Nephrol. Dial. Transplant. 20, 678–683 (2005).
Lopes, J. A. et al. Contemporary analysis of the influence of acute kidney injury after reduced intensity conditioning haematopoietic cell transplantation on long-term survival. Bone Marrow Transplant. 42, 619–626 (2008).
Hahn, T. et al. Acute renal failure requiring dialysis after allogeneic blood and marrow transplantation identifies very poor prognosis patients. Bone Marrow Transplant. 32, 405–410 (2003).
Zager, R. A. Acute renal failure in the setting of bone marrow transplantation. Kidney Int. 46, 1443–1458 (1994).
Carreras, E. et al. Incidence and outcome of hepatic veno-occlusive disease after blood or marrow transplantation: a prospective cohort study of the European Group for Blood and Marrow Transplantation. Blood 92, 3599–3604 (1998).
Dignan, F. L. et al. BCSH/BSBMT guideline: diagnosis and management of veno-occlusive disease (sinusoidal obstruction syndrome) following haematopoietic stem cell transplantation. Br. J. Haematol. 163, 444–457 (2013).
Hingorani, S. Chronic kidney disease in long-term survivors of hematopoietic cell transplantation: epidemiology, pathogenesis, and treatment. J. Am. Soc. Nephrol. 17, 1995–2005 (2006).
Kersting, S., Hené, R. J., Koomans, H. A. & Verdonck, L. F. Chronic kidney disease after myeloablative allogeneic hematopoietic stem cell transplantation. Biol. Blood Marrow Transplant. 13, 1169–1175 (2007).
Hingorani, S., Guthrie, K. A., Schoch, G., Weiss, N. S. & McDonald, G. B. Chronic kidney disease in long-term survivors of hematopoietic cell transplant. Bone Marrow Transplant. 39, 223–229 (2007).
Chan, G. S. et al. Clinicopathologic analysis of renal biopsies after haematopoietic stem cell transplantation. Nephrology (Carlton) 13, 322–330 (2008).
Reddy, P. Pathophysiology of acute graft-versus-host disease. Hematol. Oncol. 21, 149–161 (2003).
Brukamp, K. et al. Nephrotic syndrome after hematopoietic cell transplantation: do glomerular lesions represent renal graft-versus-host disease? Clin. J. Am. Soc. Nephrol. 1, 685–694 (2006).
Colombo, A. A. et al. Nephrotic syndrome after allogeneic hematopoietic stem cell transplantation as a late complication of chronic graft-versus-host disease. Transplantation 81, 1087–1092 (2006).
Elliott, M. A. et al. Posttransplantation thrombotic thrombocytopenic purpura: a single-center experience and a contemporary review. Mayo Clin. Proc. 78, 421–430 (2003).
Laskin, B. L., Goebel, J., Davies, S. M. & Jodele, S. Small vessels, big trouble in the kidneys and beyond: hematopoietic stem cell transplantation-associated thrombotic microangiopathy. Blood 118, 1452–1462 (2011).
Cohen, E. P. & Robbins, M. E. Radiation nephropathy. Semin. Nephrol. 23, 486–499 (2003).
Moulder, J. E., Cohen, E. P., Fish., B. L. & Hill, P. Prophylaxis of bone marrow transplant nephropathy with captopril, an inhibitor of angiotensin-converting enzyme. Radiat. Res. 136, 404–407 (1993).
Cohen, E. P. et al. Captopril to mitigate chronic renal failure after hematopoietic stem cell transplantation: a randomized controlled trial. Int. J. Radiat. Oncol. Biol. Phys. 70, 1546–1551 (2008).
Author information
Authors and Affiliations
Contributions
A.G. researched data for the article and wrote the article. D.S. and J.S.B. made substantial contributions to discussion of the content and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Ganguli, A., Sawinski, D. & Berns, J. Kidney diseases associated with haematological cancers. Nat Rev Nephrol 11, 478–490 (2015). https://doi.org/10.1038/nrneph.2015.81
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2015.81
This article is cited by
-
Mechanistic characterization of a Drosophila model of paraneoplastic nephrotic syndrome
Nature Communications (2024)
-
A rare cause of oligoanuric kidney failure – a diagnosis not to miss: Answers
Pediatric Nephrology (2022)
-
Methotrexate-induced acute kidney injury in patients with hematological malignancies: three case reports with literature review
Renal Replacement Therapy (2018)
-
Acute kidney injury in critically ill cancer patients: an update
Critical Care (2016)
-
Obstructive Uropathy as an Initial Presentation of Primary Myelofibrosis: Case Report and Review of Literature
Indian Journal of Hematology and Blood Transfusion (2016)