Abstract
Objective
Evaluate the association between small for gestational age (SGA) severity and morbidity and mortality in a contemporary, population of very preterm infants.
Study design
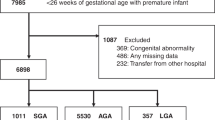
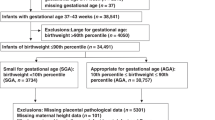
This secondary analysis of a California statewide database evaluated singleton infants born during 2008–2018 at 24–32 weeks’ gestation, with a birthweight <15th percentile. We analyzed neonatal outcomes in relation to weight for gestational age (WGA) and symmetry of growth restriction.
Results
An increase in WGA by one z-score was associated with decreased major morbidity or mortality risk (aRR 0.73, 95% CI 0.68–0.77) and other adverse outcomes. The association was maintained across gestational ages and did not differ by fetal growth restriction diagnosis. Symmetric growth restriction was not associated with neonatal outcomes after standardizing for gestational age at birth.
Conclusions
Increasing SGA severity had a significant impact on neonatal outcomes among very preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Pilliod RA, Cheng YW, Snowden JM, Doss AE, Caughey AB. The risk of intrauterine fetal death in the small-for-gestational-age fetus. Am J Obstet Gynecol. 2012;207:318.e1–318.e6.
Mendez-Figueroa H, Truong VTT, Pedroza C, Chauhan SP. Morbidity and Mortality in Small-for-Gestational-Age Infants: A Secondary Analysis of Nine MFMU Network Studies. Am J Perinatol. 2017;34:323–32.
Gardosi J, Francis A. Adverse pregnancy outcome and association with small for gestational age birthweight by customized and population-based percentiles. Am J Obstet Gynecol. 2009;201:28.e1–28.e8.
Monier I, Ancel PY, Ego A, Jarreau PH, Lebeaux C, Kaminski M, et al. Fetal and neonatal outcomes of preterm infants born before 32 weeks of gestation according to antenatal vs postnatal assessments of restricted growth. Am J Obstet Gynecol. 2017;216:516.e1–516.e10.
Chauhan S, Beydoun H, Chang E, Sandlin A, Dahlke J, Igwe E, et al. Prenatal Detection of Fetal Growth Restriction in Newborns Classified as Small for Gestational Age: Correlates and Risk of Neonatal Morbidity. Am J Perinatol. 2013;31:187–94.
Moraitis AA, Wood AM, Fleming M, Smith GCS. Birth Weight Percentile and the Risk of Term Perinatal Death: Obstet Gynecol. 2014;124:274–83.
Qiu X, Lodha A, Shah P, Sankaran K, Seshia M, Yee W, et al. Neonatal Outcomes of Small for Gestational Age Preterm Infants in Canada. Am J Perinatol. 2012;29:87–94.
De Jesus LC, Pappas A, Shankaran S, Li L, Das A, Bell EF, et al. Outcomes of Small for Gestational Age Infants Born at <27 Weeks’ Gestation. J Pediatr. 2013;163:55–60.e3.
Boghossian NS, Geraci M, Edwards EM, Horbar JD. Morbidity and Mortality in Small for Gestational Age Infants at 22 to 29 Weeks’ Gestation. Pediatrics 2018;141:e20172533.
McIntire DD, Bloom SL, Casey BM, Leveno KJ. Birth Weight in Relation to Morbidity and Mortality among Newborn Infants. N. Engl J Med. 1999;340:1234–8.
Nobile S, Marchionni P, Carnielli VP. Neonatal outcome of small for gestational age preterm infants. Eur J Pediatr. 2017;176:1083–8.
Blue NR, Beddow ME, Savabi M, Katukuri VR, Mozurkewich EL, Chao CR. A Comparison of Methods for the Diagnosis of Fetal Growth Restriction Between the Royal College of Obstetricians and Gynaecologists and the American College of Obstetricians and Gynecologists: Obstet Gynecol. 2018;131:835–41.
Ludvigsson JF, Lu D, Hammarström L, Cnattingius S, Fang F. Small for gestational age and risk of childhood mortality: A Swedish population study. Smith GC, editor. PLOS Med. 2018;15:e1002717.
Fratelli N, Valcamonico A, Prefumo F, Pagani G, Guarneri T, Frusca T. Effects of antenatal recognition and follow-up on perinatal outcomes in small-for-gestational age infants delivered after 36 weeks. Acta Obstet Gynecol Scand. 2013;92:223–9.
Roeckner JT, Pressman K, Odibo L, Duncan JR, Odibo AO. Outcome-based comparison of SMFM and ISUOG definitions of fetal growth restriction. Ultrasound Obstet Gynecol. 2021;57:925–30.
Lindqvist PG, Molin J. Does antenatal identification of small-for-gestational age fetuses significantly improve their outcome? Ultrasound Obstet Gynecol. 2005;25:258–64.
Verlijsdonk JW, Winkens B, Boers K, Scherjon S, Roumen F. Suspected versus non-suspected small-for-gestational age fetuses at term: perinatal outcomes. J Matern Fetal Neonatal Med. 2012;25:938–43.
Monier I, Blondel B, Ego A, Kaminiski M, Goffinet F, Zeitlin J. Poor effectiveness of antenatal detection of fetal growth restriction and consequences for obstetric management and neonatal outcomes: a French national study. BJOG Int J Obstet Gynaecol. 2015;122:518–27.
Mattioli KP, Sanderson M, Chauhan SP. Inadequate identification of small-for-gestational-age fetuses at an urban teaching hospital. Int J Gynecol Obstet. 2010;109:140–3.
Hei M, Lee S, Shah P, Jain A. for the Canadian Neonatal Network. Outcomes for Symmetrical and Asymmetrical Small for Gestational Age Preterm Infants in Canadian Tertiary NICUs. Am J Perinatol. 2014;32:725–32.
Sharma D, Farahbakhsh N, Shastri S, Sharma P. Intrauterine growth restriction – part 2. J Matern Fetal Neonatal Med. 2016;29:4037–48.
Bocca-Tjeertes I, Bos A, Kerstjens J, de Winter A, Reijneveld S. Symmetrical and Asymmetrical Growth Restriction in Preterm-Born Children. PEDIATRICS. 2014;133:e650–6.
Gould JB. The Role of Regional Collaboratives: The California Perinatal Quality Care Collaborative Model. Clin Perinatol. 2010;37:71–86.
CPQCC. Is That Baby Eligible Final? Birth Year 2022, What eligibility means for NICU, HRIF, CPeTS and VON [Internet]. [cited 2022 Jun 22]. Available from: https://www.cpqcc.org/sites/default/files/Is%20That%20Baby%20Eligible%20Final_1.pdf
Talge NM, Mudd LM, Sikorskii A, Basso O. United States Birth Weight Reference Corrected For Implausible Gestational Age Estimates. Pediatrics. 2014;133:844–53.
Seeds JW, Peng T. Impaired growth and risk of fetal death: Is the tenth percentile the appropriate standard? Am J Obstet Gynecol. 1998;178:658–69.
Xu H, Simonet F, Luo ZC. Optimal birth weight percentile cut-offs in defining small- or large-for-gestational-age. Acta Paediatr. 2010;99:550–5.
Martins JG, Biggio JR, Abuhamad A. Society for Maternal-Fetal Medicine Consult Series #52: Diagnosis and management of fetal growth restriction. Am J Obstet Gynecol. 2020;223:B2–17.
Melamed N, Pittini A, Barrett J, Shah J, Yoon EW, Lemyre B, et al. Antenatal Corticosteroids and Outcomes of Small-for-Gestational-Age Neonates. Obstet Gynecol. 2016;128:1001–8.
von Dadelszen P, Magee LA, Taylor EL, Muir JC, Stewart SD, Sherman P, et al. Maternal hypertension and neonatal outcome among small for gestational age infants. Obstet Gynecol. 2005;106:335–9.
Lee HC, Liu J, Profit J, Hintz SR, Gould JB. Survival Without Major Morbidity Among Very Low Birth Weight Infants in California. Pediatrics 2020;146:e20193865.
Manuck TA, Rice MM, Bailit JL, Grobman WA, Reddy UM, Wapner RJ, et al. Preterm neonatal morbidity and mortality by gestational age: a contemporary cohort. Am J Obstet Gynecol. 2016;215:103.e1–103.e14.
Baschat AA, Cosmi E, Bilardo CM, Wolf H, Berg C, Rigano S, et al. Predictors of Neonatal Outcome in Early- Onset Placental Dysfunction: Obstet Gynecol. 2007;109:253–61.
Ananth CV, Vintzileos AM. Distinguishing pathological from constitutional small for gestational age births in population-based studies. Early Hum Dev. 2009;85:653–8.
Ting JY, Kingdom JC, Shah PS. Antenatal glucocorticoids, magnesium sulfate, and mode of birth in preterm fetal small for gestational age. Am J Obstet Gynecol. 2018;218:S818–28.
Li H, Gudmundsson S, Olofsson P. Acute centralization of blood flow in compromised human fetuses evoked by uterine contractions. Early Hum Dev. 2006;82(Nov):747–52.
Baalbaki S, Kuper S, Wang M, Steele R, Biggio J, Harper L. Impact of Intended Mode of Delivery on Outcomes in Preterm Growth-Restricted Fetuses. Am J Perinatol. 2018;35:605–10.
Mlynarczyk M, Chauhan SP, Baydoun HA, Wilkes CM, Earhart KR, Zhao Y, et al. The clinical significance of an estimated fetal weight below the 10th percentile: a comparison of outcomes of <5th vs 5th-9th percentile. Am J Obstet Gynecol. 2017;217:198.e1–198.e11.
Zhang-Rutledge K, Mack LM, Mastrobattista JM, Gandhi M. Significance and Outcomes of Fetal Growth Restriction Below the 5th Percentile Compared to the 5th to 10th Percentiles on Midgestation Growth Ultrasonography. J Ultrasound Med J Am Inst Ultrasound Med. 2018;37:2243–9.
Sharma D, Shastri S, Farahbakhsh N, Sharma P. Intrauterine growth restriction – part 1. J Matern Fetal Neonatal Med. 2016;29:3977–87.
Hiersch L, Melamed N. Fetal growth velocity and body proportion in the assessment of growth. Am J Obstet Gynecol. 2018;218:S700–S711.e1.
Lees CC, Romero R, Stampalija T, Dall’Asta A, DeVore GR, Prefumo F, et al. The diagnosis and management of suspected fetal growth restriction: an evidence-based approach. Am J Obstet Gynecol. 2022;226:366–78.
Lees C, Stampalija T, Hecher K. Diagnosis and management of fetal growth restriction: the ISUOG guideline and comparison with the SMFM guideline. Ultrasound Obstet Gynecol. 2021;57:884–7.
Walker AR, Waites BT, Caughey AB. Twins versus singleton pregnancies: outcomes in small for gestational age late preterm deliveries. J Matern Fetal Neonatal Med. 2020;33:895–900.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Preterm Birth 1 Epidemiology and causes of preterm birth. Lancet 2008;371(Jan):75–84.
Fumagalli M, Schiavolin P, Bassi L, Groppo M, Uccella S, De Carli A, et al. The Impact of Twin Birth on Early Neonatal Outcomes. Am J Perinatol. 2015;33:063–70.
Multifetal Gestations: Twin, Triplet, and Higher-Order Multifetal Pregnancies: ACOG Practice Bulletin, Number 231. Obstet Gynecol. 2021;137:e145–62.
Acknowledgements
We appreciate the approval from the CPQCC to conduct this investigation.
Author information
Authors and Affiliations
Contributions
KM contributed to the concept of the work, drafting and revising the manuscript. SL substantially contributed to the design of the study, analysis and co-wrote the manuscript. LS contributed to design, data analysis and revising of the manuscript. KB, MD and HL substantially contributed to the conception of the work, drafting and revising the manuscript and gave approval of this version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the California Committee for the Protection of Human Subjects (IRB #12-06-0393) and the Stanford University Institutional Review Board (IRB #14746). The Study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Minor, K.C., Bianco, K., Sie, L. et al. Severity of small-for-gestational-age and morbidity and mortality among very preterm neonates. J Perinatol 43, 437–444 (2023). https://doi.org/10.1038/s41372-022-01544-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01544-w