Abstract
Objective
To compare rates of small- and large-for-gestational age (SGA and LGA) neonates using four different weight centiles, and to relate these classifications to neonatal morbidity.
Study design
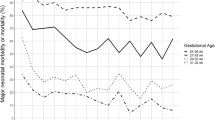
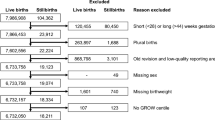
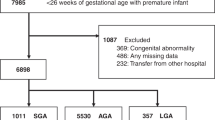
Neonates born at 33–40 weeks’ gestation in a multiethnic population were classified as SGA or LGA by population reference (Fenton), population standard (INTERGROWTH), fetal growth curves (WHO), and customized (GROW) centiles. Likelihood of composite morbidity was determined compared with a common appropriate-for-gestational age referent group.
Result
Among 45,505 neonates, SGA and LGA rates varied up to threefold by different centiles. Those most likely to develop neonatal morbidity were SGA or LGA on both the population reference and an alternative centile. Customized centiles identified over twice as many at-risk SGA neonates.
Conclusions
Customized centiles were most useful in identifying neonates at increased risk of morbidity, and those that were small on both customized and population reference centiles were at the highest risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Horbar JD, Carpenter JH, Badger GJ, Kenny MJ, Soll RF, Morrow KA, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129:1019–26.
Manuck TA, Rice MM, Bailit JL, Grobman WA, Reddy UM, Wapner RJ, et al. Preterm neonatal morbidity and mortality by gestational age: a contemporary cohort. Am J Obstet Gynecol. 2016;215:103.e101–103.e114.
Pasupathy D, McCowan LM, Poston L, Kenny LC, Dekker GA, North RA, et al. Perinatal outcomes in large infants using customised birthweight centiles and conventional measures of high birthweight. Paediatr Perinat Epidemiol. 2012;26:543–52.
Roland D, Madar J, Connolly G. The Newborn Early Warning (NEW) system: development of an at-risk infant intervention system. Infant. 2010;6:116–20.
Yu J, Flatley C, Greer RM, Kumar S. Birth-weight centiles and the risk of serious adverse neonatal outcomes at term. J Perinat Med. 2018;46:1048–56.
Chiavaroli V, Marcovecchio ML, de Giorgis T, Diesse L, Chiarelli F, Mohn A. Progression of cardio-metabolic risk factors in subjects born small and large for gestational age. PLoS ONE. 2014;9:e104278.
Crispi F, Miranda J, Gratacós E. Long-term cardiovascular consequences of fetal growth restriction: biology, clinical implications, and opportunities for prevention of adult disease. Am J Obstet Gynecol. 2018;218:S869–79.
Theodore RF, Broadbent J, Nagin D, Ambler A, Hogan S, Ramrakha S, et al. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension. 2015;66:1108–15.
McCowan LM, Figueras F, Anderson NH. Evidence-based national guidelines for the management of suspected fetal growth restriction: comparison, consensus, and controversy. Am J Obstet Gynecol. 2018;218:S855–68.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Papageorghiou AT, Ohuma EO, Altman DG, Todros T, Ismail LC, Lambert A, et al. International standards for fetal growth based on serial ultrasound measurements: the Fetal Growth Longitudinal Study of the INTERGROWTH-21st Project. Lancet. 2014;384:869–79.
Kiserud T, Piaggio G, Carroli G, Widmer M, Carvalho J, Jensen LN, et al. The World Health Organization Fetal Growth Charts: a multinational longitudinal study of ultrasound biometric measurements and estimated fetal weight. PLoS Med. 2017;14:e1002220.
Gardosi J. New definition of small for gestational age based on fetal growth potential. Horm Res Paediatr. 2006;65:S15–8.
Gardosi J. Customized fetal growth standards: rationale and clinical application. Semin Perinatol. 2004;28:33–40.
Villar J, Altman D, Purwar M, Noble J, Knight H, Ruyan P, et al. The objectives, design and implementation of the INTERGROWTH‐21st Project. BJOG. 2013;120:S9–S26.
Anderson NH, Sadler LC, McKinlay CJD, McCowan LM. INTERGROWTH-21st vs customized birthweight standards for identification of perinatal mortality and morbidity. Am J Obstet Gynecol. 2016;214:509.e501–507.
Hutcheon JA, Zhang X, Platt RW, Cnattingius S, Kramer MS. The case against customised birthweight standards. Paediatr Perinat Epidemiol. 2011;25:11–16.
McIntire DD, Bloom SL, Casey BM, Leveno KJ. Birth weight in relation to morbidity and mortality among newborn infants. N Engl J Med. 1999;340:1234–8.
Brown H, Speechley K, Macnab J, Natale R, Campbell M. Biological determinants of spontaneous late preterm and early term birth: a retrospective cohort study. BJOG. 2015;122:491–9.
Gunay F, Alpay H, Gokce I, Bilgen H. Is late-preterm birth a risk factor for hypertension in childhood? Eur J Pediatr. 2014;173:751–6.
Heinonen K, Eriksson JG, Lahti J, Kajantie E, Pesonen A-K, Tuovinen S, et al. Late preterm birth and neurocognitive performance in late adulthood: a birth cohort study. Pediatrics. 2015;135:e818–e825.
Villar J, Cheikh Ismail L, Victora CG, Ohuma EO, Bertino E, Altman DG, et al. International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet. 2014;384:857–68.
Australasian Society for Ultrasound in Medicine. Guidelines for the mid trimester obstetric scan (D2); 2007. http://www.asum.com.au/site/policies.php.
Australasian Society for Ultrasound in Medicine. Statement on normal ultrasonic fetal measurements (D7); 2007. http://www.asum.com.au/site/policies.php.
Farquhar C. Seventh annual report of the Perinatal and Maternal Mortality Review Committee: Reporting mortality, 2011. Wellington: Health Quality and Safety Commission; 2013.
Ministry of Health. Ethnicity data protocols for the health and disability sector; 2004. http://www.nzhis.govt.nz/documentation/ethnicity/index.html.
Villar J, Ismail LC, Victora CG, Ohuma EO, Bertino E, Altman DG, et al. International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet. 2014;384:857–68.
Gardosi J, Mongelli M, Wilcox M, Chang A. An adjustable fetal weight standard. Ultrasound Obstet Gynecol. 1995;6:168–74.
Anderson N, Sadler L, Stewart A, McCowan L. Maternal and pathological pregnancy characteristics in customised birthweight centiles and identification of at‐risk small‐for‐gestational‐age infants: a retrospective cohort study. BJOG. 2012;119:848–56.
Engle WA. Age terminology during the perinatal period. Pediatrics. 2004;114:1362–4.
Gluckman PD, Pinal CS. Maternal-placental-fetal interactions in the endocrine regulation of fetal growth. Endocrine. 2002;19:81–89.
Bassett N, Oliver M, Breier B, Gluckman P. The effect of maternal starvation on plasma insulin-like growth factor I concentrations in the late gestation ovine fetus. Pediatr Res. 1990;27:401–4.
Brosens I, Dixon H, Robertson W. Fetal growth retardation and the arteries of the placental bed. BJOG. 1977;84:656–63.
Salafia CM, Minior VK, Pezzullo JC, Popek EJ, Rosenkrantz TS, Vintzileos AM. Intrauterine growth restriction in infants of less than thirty-two weeks’ gestation: associated placental pathologic features. Am J Obstet Gynecol. 1995;173:1049–57.
Salafia C, Pezzullo J, Ghidini A, Lopez-Zeno J, Whittington S. Clinical correlations of patterns of placental pathology in preterm pre-eclampsia. Placenta. 1998;19:67–72.
Dekker G, De Vries J, Doelitzsch P, Huijgens P, Von Blomberg B, Jakobs C, et al. Underlying disorders associated with severe early-onset preeclampsia. Am J Obstet Gynecol. 1995;173:1042–8.
Lorentzen B, Henriksen T. Plasma lipids and vascular dysfunction in preeclampsia. Semin Reprod Med. 1998;16:33–39.
Kaaja R. Insulin resistance syndrome in preeclampsia. Semin Reprod Endocrinol. 1998;16:41–46.
Lackman F, Capewell V, Richardson B, Gagnon R. The risks of spontaneous preterm delivery and perinatal mortality in relation to size at birth according to fetal versus neonatal growth standards. Am J Obstet Gynecol. 2001;184:946–53.
Walton A, Hammond J. The maternal effects on growth and conformation in shire horse-shetland pony crosses. Proc R Soc Lond B Biol Sci. 1938;125:311–35.
Fowden AL, Ward JW, Wooding F, Forhead AJ, Constancia M. Programming placental nutrient transport capacity. J Physiol. 2006;572:5–15.
Allen W, Wilsher S, Turnbull C, Stewart F, Ousey J, Rossdale P, et al. Influence of maternal size on placental, fetal and postnatal growth in the horse. I. Development in utero. Reproduction. 2002;123:445–53.
Gluckman PD, Hanson MA. Maternal constraint of fetal growth and its consequences. Semin Fetal Neonatal Med. 2004;9:419–25.
Kramer MS. Determinants of low birth weight: methodological assessment and meta-analysis. Bull World Health Organ. 1987;65:663–737.
Gardosi J, Clausson B, Francis A. The value of customised centiles in assessing perinatal mortality risk associated with parity and maternal size. BJOG. 2009;116:1356–63.
Lawlor D, Fraser A, Lindsay R, Ness A, Dabelea D, Catalano P, et al. Association of existing diabetes, gestational diabetes and glycosuria in pregnancy with macrosomia and offspring body mass index, waist and fat mass in later childhood: findings from a prospective pregnancy cohort. Diabetologia. 2010;53:89–97.
Logan KM, Gale C, Hyde MJ, Santhakumaran S, Modi N. Diabetes in pregnancy and infant adiposity: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2017;102:F65–F72.
Donnelley E, Raynes-Greenow C, Turner R, Carberry A, Jeffery H. Antenatal predictors and body composition of large-for-gestational-age newborns: perinatal health outcomes. J Perinatol. 2014;34:698.
Ananth CV, Vintzileos AM. Maternal-fetal conditions necessitating a medical intervention resulting in preterm birth. Am J Obstet Gynecol. 2006;195:1557–63.
Villar J, Ohuma E, Stirnemann J, Papageorghiou A, Kennedy S. Clarification of INTERGROWTH-21st newborn birthweight standards—Authors’ reply. Lancet. 2018;391:1996.
Robinson A, Winckworth LC, Eleftheriou G, Hewitson R, Holme H. Prospective evaluation of the Whitt Neonatal Trigger Score in an ‘at-risk’ neonatal population. J Paediatr Child Health. 2017;53:950–6.
Author information
Authors and Affiliations
Contributions
RDC and CJDM had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: RDC and CJDM. Acquisition, analysis, or interpretation of data: all authors. Drafting of the paper: RDC and CJDM. Critical revision of the paper for important intellectual content: all authors. Statistical analysis: RDC and CJDM. Administrative, technical, or material support: JEH and CJDM. Supervision: JEH and CJDM.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cartwright, R.D., Anderson, N.H., Sadler, L.C. et al. Neonatal morbidity and small and large size for gestation: a comparison of birthweight centiles. J Perinatol 40, 732–742 (2020). https://doi.org/10.1038/s41372-020-0631-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0631-3
This article is cited by
-
Combined maternal central adiposity measures in relation to infant birth size
Scientific Reports (2024)
-
Performances of birthweight charts to predict adverse perinatal outcomes related to SGA in a cohort of nulliparas
BMC Pregnancy and Childbirth (2022)
-
Neurodevelopmental outcomes of singleton large for gestational age infants <29 weeks’ gestation: a retrospective cohort study
Journal of Perinatology (2021)