Abstract
Background
Small-for-gestational-age (SGA) has a heterogeneous etiology. Our study aimed to examine the childhood health outcomes of etiology-distinct term SGA subgroups.
Methods
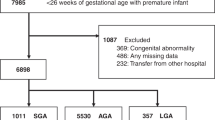
Data from the Collaborative Perinatal Project were used. The etiological factors of SGA were categorized into five groups: maternal, fetal, placental, environmental and physiological factors. Primary child outcomes included low IQ and growth restriction. A total of 8417 term infants were eligible.
Results
Compared with AGA, SGA children due to fetal factors had the highest risk of low IQ (aOR = 1.94, 95% CI: 1.45–2.59). SGA infants due to physiological factors had the highest risk of growth restriction (aOR = 6.04, 95% CI: 3.93–9.27). SGA children had a higher risk of growth restriction with the aOR ranging from 3.05 (95% CI: 2.36–3.96) to 5.77 (95% CI: 4.29–7.75) for the number of risk factors that the SGA infants had from 1 to 5. SGA children with any risk factor were associated with a higher risk of lower IQ with the aOR ranging from 1.59 (95% CI: 1.31–1.94) to 1.96 (95% CI: 1.50–2.55). SGA without the five types of etiologies was not associated with adverse child outcomes except for growth restriction (aOR = 3.82, 95% CI: 2.62–5.55).
Conclusion
Term SGA of different etiologies may lead to different child health outcomes.
Impact
-
Our study found that SGA of different etiologies may lead to different child health outcomes.
-
Compared with AGA, SGA children due to fetal factors had the highest risk of low IQ. SGA infants due to physiological factors had the highest risk of growth restriction.
-
SGA babies should not be treated the same. In the era of precision medicine, our findings may help pediatricians and parents better manage SGA babies according to different etiologies and the number of risk factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data of the National Collaborative Perinatal Project are available at the U.S. National Archives. Website: https://www.archives.gov/research/electronic-records/nih.html?_ga=2.166691642.504404601.1662257591–537933195.1662257591.
References
Verkauskiene, R., Petraitiene, I. & Albertsson Wikland, K. Puberty in children born small for gestational age. Horm. Res. Paediatr. 80, 69–77 (2013).
Kozuki, N. et al. Short maternal stature increases risk of small-for-gestational-age and preterm births in low- and middle-income countries: individual participant data meta-analysis and population attributable fraction. J. Nutr. 145, 2542–2550 (2015).
Khanam, R. et al. Maternal short stature and under-weight status are independent risk factors for preterm birth and small for gestational age in rural Bangladesh. Eur. J. Clin. Nutr. 73, 733–742 (2019).
McCowan, L. & Horgan, R. Risk factors for small for gestational age infants. Best. Pract. Res. Clin. Obstet. Gynaecol. 23, 779–793 (2009).
Okah, F., Cai, J., Dew, P. & Hoff, G. Risk factors for recurrent small-for-gestational-age birth. Am. J. Perinatol. 27, 1–7 (2010).
Betti, M. et al. Neonatal outcome in newborns from mothers with endocrinopathies. Gynecol. Endocrinol. 27, 248–250 (2011).
Berghella, V. Maternal-Fetal Evidence Based Guidelines 2nd edn (CRC Press, 2011).
Xie, C. et al. Stunting at 5 years among SGA newborns. Pediatrics 137, e20152636 (2016).
Hardy, J. B. The Collaborative Perinatal Project: lessons and legacy. Ann. Epidemiol. 13, 303–311 (2003).
Naeye, R. L. Effects of maternal cigarette smoking on the fetus and placenta. Br. J. Obstet. Gynaecol. 85, 732–737 (1978).
Klebanoff, M. A. The Collaborative Perinatal Project: a 50‐year retrospective. Paediatr. Perinat. Epidemiol. 23, 2–8 (2009).
Terry, M. B., Flom, J., Tehranifar, P. & Susser, E. The role of birth cohorts in studies of adult health: the New York Women’s Birth Cohort. Paediatr. Perinat. Epidemiol. 23, 431–445 (2009).
Finken, M. J. J. et al. Children born small for gestational age: differential diagnosis, molecular genetic evaluation, and implications. Endocr. Rev. 39, 851–894 (2018).
Linde, L. E., Rasmussen, S., Kessler, J. & Ebbing, C. Extreme umbilical cord lengths, cord knot and entanglement: risk factors and risk of adverse outcomes, a population-based study. PLoS One 13, e0194814 (2018).
Lei, X. et al. The optimal postnatal growth trajectory for term small for gestational age babies: a prospective cohort study. J. Pediatr. 166, 54–58 (2015).
Kuczmarski, R. J. et al. CDC growth charts: United States. Adv. Data 1–27 (2000).
Krebs, N. F. et al. Assessment of child and adolescent overweight and obesity. Pediatrics 120(Suppl 4), S193–S228 (2007).
Gray, K. A. et al. In utero exposure to background levels of polychlorinated biphenyls and cognitive functioning among school-age children. Am. J. Epidemiol. 162, 17–26 (2005).
Myrianthopoulos, N. C. & French, K. S. An application of the US Bureau of the Census Socioeconomic Index to a large, diversified patient population. Soc. Sci. Med. (1967) 2, 283–299 (1968).
Saenger, P., Czernichow, P., Hughes, I. & Reiter, E. O. Small for gestational age: short stature and beyond. Endocr. Rev. 28, 219–251 (2007).
Willemsen, R., de Kort, S., van der Kaay, D. & Hokken-Koelega, A. Independent effects of prematurity on metabolic and cardiovascular risk factors in short small-for-gestational-age children. J. Clin. Endocrinol. Metab. 93, 452–458 (2008).
Ibáñez, L. et al. Abdominal fat partitioning and high-molecular-weight adiponectin in short children born small for gestational age. J. Clin. Endocrinol. Metab. 94, 1049–1052 (2009).
Kerkhof, G., Breukhoven, P., Leunissen, R., Willemsen, R. & Hokken-Koelega, A. Does preterm birth influence cardiovascular risk in early adulthood? J. Pediatr. 161, 390–396.e391 (2012).
Lohaugen, G. C. et al. Small for gestational age and intrauterine growth restriction decreases cognitive function in young adults. J. Pediatr. 163, 447–453 (2013).
Li, X. et al. Etiological subgroups of small-for-gestational-age: differential neurodevelopmental outcomes. PLoS One 11, e0160677 (2016).
Gharib, H. et al. American Association of Clinical Endocrinologists Medical Guidelines for clinical practice for growth hormone use in adults and children—2003 update. Endocr. Pract. 9, 64–76 (2003).
Funding
All phases of this study were supported by research grants from the National Natural Science Foundation of China (Grant number 81903323) and Shanghai Municipal Health Commission (Grant number 20194Y0157). All authors have indicated they have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Contributions
J.Z. conceptualized and designed the study. F.F. and Y.C. carried out the initial analyses and drafted the initial manuscript. Q.C., J.L., Z.-C.L., F.L., Y.Z. and F.J. critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
Anonymized data were used for this study, and the patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fang, F., Chen, Y., Chen, Q. et al. Etiological subgroups of term small-for-gestational-age and childhood health outcomes. Pediatr Res 94, 378–384 (2023). https://doi.org/10.1038/s41390-022-02412-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02412-1