Abstract
Although blood pressure control is considered the main mechanism for preventing the progression of chronic kidney disease (CKD), angiotensin-converting enzyme inhibitors and angiotensin receptors blockers have an additional organ-protective role. The effects of calcium channel blockers (CCBs) in renal disease are not so clearly defined. CCBs have pleiotropic effects that might contribute to protection of the kidney, such as attenuating the mesangial entrapment of macromolecules, countervailing the mitogenic effect of platelet-derived growth factors and platelet-activating factors and suppressing mesangial cell proliferation. Some evidence has accumulated in recent years demonstrating that the new dihydropyridinic CCBs (such as lercanidipine or efonidipine) may affect both postglomerular and preglomerular vessels, resulting in a decreased filtration fraction and nephroprotective effect. Increasing clinical and experimental evidence supports this view and the use of CCBs in CKD hypertensive patients.
Similar content being viewed by others
Introduction
Hypertension is a major determinant of renal disease progression, irrespective of its cause. The relative risk of 3developing end-stage renal disease in hypertensive patients increases threefold when a patient’s diastolic blood pressure (DBP) increases to 90 mm Hg compared with that of patients with ‘optimal’ BP.1 Although tighter BP control is considered the main mechanism for slowing the progression of chronic renal failure, some antihypertensive agents, such as angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs), have an additional organ-protective role and are routinely used in renal disease.2 In terms of clinical pharmacology and therapeutic use, there are fundamental differences between the dihydropyridine (DHP) group of CCBs (such as nifedipine) and other commonly used non-DHP calcium channel blockers (CCBs; such as verapamil and diltiazem). This latter group has shown little, if any, effect on albuminuria or renal disease progression; therefore, this article will focus on dihydropyridinic CCBs.3 Furthermore, this review seeks to highlight the differences within the DHP CCB group, with a particular emphasis on the renoprotective effects of last-generation CCBs.
Although non-DHP CCB (verapamil and diltiazem) effects on renal disease are beyond the scope of this review, diabetes mellitus animal models provide evidence that they can blunt both the rise in proteinuria as well as mesangial glomerular scarring.4 Diltiazem appears to have an inhibitory effect on mitochondrial sodium–calcium exchange that is unique among CCBs.5 Moreover, non-DHP CCBs have been shown to attenuate the increase in matrix protein synthesis induced by glycated albumin.6 In the experimental remnant kidney model, diltiazem reduced glomerulosclerosis progression compared with verapamil and felodipine, although none of them reduced glomerular hypertrophy.7 From a clinical point of view, several long-term trials with non- DHP drugs have demonstrated reductions in proteinuria intensity and slowed declines in glomerular filtration rates (GFRs),8, 9, 10, 11, 12, 13, 14, 15, 16 although some studies failed to show this effect.17, 18, 19 Specifically, a meta-analysis examining the differential effects of calcium antagonist subclasses on markers of nephropathy progression found similar efficacy between subclasses of calcium antagonists to lower BP but greater reductions in proteinuria non-DHP CCBs compared with classic DHP calcium antagonists.20 Nevertheless, this review will exclusively focus on the effects of dihydropyridinic CCBs on chronic kidney disease (CKD).
‘In vitro’ renoprotective effects of CCBs
Calcium antagonists have pleiotropic effects that might contribute to protecting the kidney against hypertension-induced damage. Calcium antagonists have demonstrated modulation of macromolecular traffic through the mesangium and attenuate mesangial entrapment of macromolecules, which induce inflammatory and proliferative responses.21, 22 It has also been suggested that calcium antagonists may counteract the mitogenic effect of platelet-derived growth factors and platelet-activating factors, which seem to have an important role in renal lesions induced by hypertension.23 Similarly, calcium antagonists suppress mesangial cell proliferation by inhibiting activator protein-1,24 as well as the cell cycle transition from the G1 to S phase,25 and have an inhibitory effect on the stimulated transcriptional action of interleukin-1β and granulocyte/monocyte colony-stimulating factors by platelet-derived growth factors in human mesangial cells.26 In this regard, calcium antagonists have been shown to suppress the phorbol 12-myristate 13-acetate-induced activation of nuclear factor kappa β in cultured human mesangial cells.27
Finally, calcium antagonists might act as free radical scavengers.28, 29 They may reduce the activity of some intracellular free radical sources (that is, they could inhibit the activity of NADPH oxidase, xanthine oxidase and cyclooxygenase, which are the main sources of intracellular reactive oxygen species).30 Second, CCBs may decrease the intracellular-free radical concentration through its direct antioxidant capacity.31 Calcium antagonists may protect the redox potential of the free radical targets through their effect on nuclear factor kappa β and hence on the signaling pathways leading to its activation.32
Last of all, inhibition of the renal effects of endothelin by CCBs has been demonstrated under experimental conditions.33 Endothelin-1 is a potent vasoconstrictor that has been implicated in the pathogenesis of kidney disease and animal models of hypertension.34, 35, 36 It is therefore of considerable interest that endothelin appears to preferentially reduce blood flow in the renal cortex, with either small reductions, or even increases, in the medullary blood flow in anesthetized rats37 and dogs.38 Furthermore, treatments that reduce renal medullary blood flow cause hypertension, if chronically administered, and attenuate BP-lowering mechanisms in the kidney.39, 40 This phenomenon may have important implications in pathological conditions associated with increased circulating or local intrarenal levels of endothelin, such as acute and chronic renal failure,17 advanced atherosclerosis40 and perhaps essential hypertension.41
Effects on renal hemodynamics
The classic molecular target of the CCBs is the voltage-activated L-type Ca2+ channel, also referred to in the past as the DHP receptor because of the presence of a high-affinity DHP-binding site. However, in addition to sharing the antihypertensive effect of CCBs, third-generation DHPs also exhibit therapeutic benefits on renal hemodynamics. In contrast to most CCBs, which predominantly dilate afferent glomerular arterioles and potentially cause glomerular hypertension and other undesirable effects, new DHPs have an additional vasodilatory effect on efferent arterioles. Recent advances in basic science have emphasized that new DHPs can inhibit other types of Ca2+ channels, including the T-type, the neuronal P/Q type and N-type Ca2+ channels.42 In parallel, these Ca2+ channel subtypes have been localized in renal vascular and tubular tissues (T-type, P/Q type) and in sympathetic nerve endings (N-type), which may also impact vascular tone. The lack of functional expression of the L-Type Ca2+ channel and DHP insensitivity to most CCBs in renal efferent arterioles strongly further supports the hypothesis of a critical role of the T-type Ca2+ channel (and possibly of the N- and P/Q types) in the vascular tone in these arterioles. The effect of mibefradil and of new DHPs on non-L-type Ca2+ channels may account for the divergent actions of CCBs on afferent and efferent arterioles and for the beneficial effect on glomerular hemodynamics.43 Recent results have also opened the provocative perspective that neuronal P/Q type (α 1A) Ca2+ channels are also expressed in vascular myocytes (from renal preglomerular resistance vessels and the aorta), as well as in mesangial cells, where they account for Ca2+ influx and the depolarization-mediated contraction of renal afferent arterioles.44
After the discovery of the T-type and the neuronal N, P/Q, and R-type Ca2+ channels, it became clear that DHPs, and often other CCBs as well, could inhibit the various types of Ca2+ channels, which stimulated interest for potential clinical applications. For example, nicardipine had a significant effect on the T-type Ca2+ channel in sensory neurons, but nifedipine and nitrendipine had only a weak effect.45 In vascular myocytes, nicardipine and flunarizine could also inhibit the T-type Ca2+ channel.46 Some DHPs, as well as verapamil and diltiazem, could inhibit P-type Ca2+ currents at concentrations that are not maximally active for the L-type Ca2+ channel inhibition with functional impact on renal afferent arterioles.47
In addition to their remarkable effectiveness in inhibiting the activity of the L-type Ca2+ channel, the last generation of DHPs has additional protective effects on renal function. These effects seem to occur, at least in part, independently of long-term antiremodeling effects that are observed in the ACEI or the ARBs. To explain the differential effect of third-generation DHPs on glomerular function, a blocking action on T-type Ca2+ channels has been proposed, based on the dual effects of these compounds on both L- and T-type Ca2+ channels.48, 49, 50 In contrast with the lack of effect of DHPs such as nifedipine, the other DHPs, such as mibefradil, nilvadipine and efonidipine, inhibit both the T-type and the L-type Ca2+ channels, reversing the angiotensin (Ang) II-induced afferent and efferent arteriolar constriction.51 However, the renoprotective effects of T-type CCBs may be based not only on a reduction in systemic BP but also on decreased Rho-kinase activity, tubulointerstitial fibrosis and epithelial–mesenchymal transitions.52 New DHPs also cause very moderate peripheral edema owing to their equal vasodilatory effects on precapillary and postcapillary vessels, which may reflect the differential expression of T- and L-type Ca2+ channels in arterial and venous tissues.53
For example, the DHPs amlodipine, barnidipine, benidipine, efonidipine, manidipine, nicardipine and nilvadipine, with effects on recombinant Ca2+ channels of both the L-type and the T-type (a1G), were reported to exhibit blocking actions comparable to that of mibefradil on the T-type Ca2+ channel.54, 55 In contrast to the predominant afferent arteriolar action of conventional CCBs (nifedipine, nicardipine, amlodipine and diltiazem), the novel DHP CCBs (for example, manidipine, nilvadipine, benidipine, efonidipine and lercanidipine) potently dilate both afferent and efferent arterioles and have beneficial effects on intrarenal hemodynamics.56 In addition, efonidipine has also been reported to decrease plasma aldosterone concentration in accordance with reported effects on the key role of T-type Ca2+ channels on aldosterone production.57
Effects of classic CCBs on the kidney
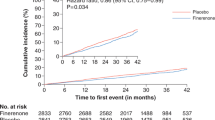
There is a large amount of information regarding the effects of calcium antagonists on human renal disease. Most of the reports have evaluated the changes in proteinuria or urinary albumin excretion (UAE). The studies with follow-up for >12 weeks have been taken into account in this review, which excludes most comparisons against placebo (Figure 1).58, 59 Taken altogether, the results demonstrate a clearly unfavorable effect on CCBs compared with the antiproteinuric effect of renin–angiotensin axis-blocking drugs. Table 1 summarizes the effects of classic CCBs on the GFR and renal failure progression.60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70 The Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm, a multicenter randomized controlled trial (RCT), compared the effects on the cardiovascular end points of two pharmacological regimens: the first was based on amlodipine (using perindopril as the second-step drug) and the other on atenolol (using bendroflumethiazide as the second-step drug). There was a significant reduction in the development of renal impairment associated with the amlodipine-based regimen (15%). Nevertheless, by the end of the trial, as intended by design, most patients (78%) were taking at least two antihypertensive agents, and only 15% were taking amlodipine monotherapy. Therefore, it could be risky to come to any conclusions on the renoprotective effects of amlodipine from this trial.71
Results of the reported trials describing the effects of classic CCBs on albuminuria/proteinuria. Most of the trials cannot show a protective effect on proteinuria and/or albuminuria.59, 60, 77, 78, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 122, 123, 124
Some studies have compared the possible beneficial effect of combining calcium antagonists and renin–angiotensin blocking drugs for treating hypertension but, taken altogether, the published results are conflicting and inconclusive. A ramipril and felodipine combination therapy was tested in the NEPHROS trial. The combination group had a slower renal disease progression rate compared with the felodipine group (P<0.05) but not to the ramipril group (P>0.20). There was a rise in albuminuria after 2 years in the felodipine group (P<0.05), but no significant change was found in the other groups. The beneficial effect of the combination of an ACEI and a calcium antagonist could be due to increased BP reduction.72 Shigihara et al.73 examined the effects of combination therapy using an ACEI plus amlodipine and compared them with the effect of an ACEI alone under intensive BP control (DBP<80 mm Hg) on UAE in hypertensive, type 2 diabetic patients with microalbuminuria. The UAE decrease attained statistical significance only in the combination group (P<0.05).73 Fogari et al.74 compared the long-term effect of amlodipine and fosinopril in monotherapy or in combination on UAE in hypertensive diabetic patients with microalbuminuria. The combination therapy was more effective in reducing BP than either drug alone at any time of the study. All three treatments provided a significant decrease in UAE during the 48-month study period. However, this effect was more pronounced and became evident earlier with fosinopril than with amlodipine monotherapy (after 3 vs. 18 months of therapy). In addition, the combination therapy provided a greater antialbuminuric effect than the use of the drugs singly. This result could be due to the greater antihypertensive effects.74 The REIN 2 study was a multicenter, RCT of patients with non-diabetic proteinuric nephropathies receiving a background treatment with ramipril. The participants were randomly assigned either conventional (DBP<90 mm Hg; n=169) or intensified (SBP/DBP<130/80 mm Hg; n=169) BP control. To achieve the intensified BP level, patients received add-on therapy with felodipine. The main conclusion was that no additional benefit from further BP reduction with felodipine could be shown in patients with non-diabetic proteinuric nephropathies receiving background ACEI therapy.75
The GUARD study (Gauging Albuminuria Reduction With Lotrel in Diabetic Patients With Hypertension) tested the hypothesis that combining an ACEI with either a thiazide diuretic or a CCB will cause similar reductions in BP and albuminuria in hypertensive type 2 diabetics. It was a double-blind RCT on 332 hypertensive, albuminuric type 2 diabetic patients treated with benazepril and either amlodipine or hydrochlorothiazide for 1 year. Both combinations significantly reduced the urinary albumin-to-creatinine ratio and the sitting BP of the entire cohort. The percentage of patients progressing to overt proteinuria was similar between groups. In patients who had only microalbuminuria and hypertension, a larger percentage of the diuretic and ACEI normalized their albuminuria.76
The Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) trial showed that initial antihypertensive therapy with benazepril plus amlodipine was superior to benazepril plus hydrochlorothiazide in reducing cardiovascular morbidity and mortality.77 More recently, a second report has assessed the effects of these drug combinations on the progression of CKD. ACCOMPLISH was a double-blind, randomized trial that recruited 11 506 patients with hypertension who were at high risk for cardiovascular events. They were randomly assigned to receive benazepril (20 mg) plus amlodipine (5 mg; n=5744) or benazepril (20 mg) plus hydrochlorothiazide (12.5 mg; n=5762), orally once daily. Drug doses were force-titrated for patients to attain the recommended BP goals. Progression of CKD, a prespecified end point, was defined as the doubling of the serum creatinine concentration or end-stage renal disease (estimated GFR<15 ml min−1 1·73 m−2 or need for dialysis). The trial was terminated early (mean follow-up 2.9 years) because of the superior efficacy of benazepril plus amlodipine compared with benazepril plus hydrochlorothiazide. Additionally, in patients with CKD, the progression of CKD was slower in the benazepril plus amlodipine group. In 446 of those patients with baseline microalbuminuria, there was a deeper reduction in UAE from baseline in the benazepril plus hydrochlorothiazide group compared with the benazepril plus amlodipine group.78
Nevertheless, the end point in ACCOMPLISH was a composite of the doubling of serum creatinine (this increment approximately reflects a sustained loss of 50% of a patient’s starting GFR) and end-stage renal disease. Although it is assumed that these changes are related to the structural decline in renal function, GFR might be affected by different ways over time: initially a drug might induce a change in GFR via a hemodynamic effect, whereas it might induce long-term GFR changes via renal structural effects. Thus the end point could reflect a reversible hemodynamic GFR change or a structural worsening of kidney function. In ACCOMPLISH, the end point was driven by the doubling of serum creatinine with no difference in end-stage renal disease, which did not occur often. This finding could be interpreted as a hemodynamic change rather than a structural renal function loss. It has been reported that the diuretic plus the ACEI induced a distinct fall in GFR within 12 weeks, whereas the addition of the CCB to the diuretic increased GFR slightly. After this acute hemodynamic change in GFR, the subsequent long-term slope was similar between the two treatment groups.79 Taking these data into consideration, it can be argued that the benefit of CCBs is mainly based on the hemodynamic effect and thus GFR would return to similar levels after stopping the treatments. However, this hypothesis remains untested. There is no reason to reject the concept that hemodynamic changes induced by a diuretic become structural after long-term treatment. The long-term effects of CCBs are produced by non-hemodynamic mechanisms. At worst, the long-term structural effects will cause a slightly higher renal function (if a calcium antagonist is used) or a diuretic-induced decreased renal function, and this situation will be dangerous for the patient.
In a recently published substudy of the ACCOMPLISH trial, 573 subjects underwent 24-h ambulatory BP monitoring. Subjects were recruited from the US cohort and did not differ in baseline clinical characteristics from the overall study population. The study groups did not differ significantly in mean 24-h, daytime or nighttime systolic BP (SBP) levels. The finding that 24-h BP levels did not significantly differ between the two groups supports the original interpretation of the investigators that the difference in the primary composite cardiovascular end point that favored the amlodipine-based regimen could not be explained by between-group differences in BP levels.80
New calcium antagonists
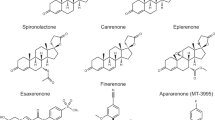
There is an increasing number of reports on the clinical renal effects of new CCBs, which have rendered promising results (Figure 2, Table 2). Bellinghieri et al.81 compared the effects of manidipine and nifedipine on BP and renal function. Significant reductions in SBP and DBP were reached in both treatments. Creatinine blood levels and creatinine clearance were significantly increased in the manidipine group. Proteinuria did not significantly change in the manidipine group, but it increased in the nifedipine group.81 Del Vecchio et al.82 evaluated the efficacy and tolerability of manidipine in comparison with enalapril in patients with chronic renal disease. Proteinuria remained unchanged with manidipine and significantly decreased with enalapril. No significant difference was observed in the rate of renal function decline in the two groups.82 Fogari et al.83 compared the effect of long-term monotherapy with manidipine or lisinopril on UAE and left ventricular mass index in hypertensive patients with type 2 diabetes and microalbuminuria. Manidipine and lisinopril both significantly reduced SBP and DBP levels. Both drugs provided a significant decrease in UAE, but it was significantly more pronounced with lisinopril than with manidipine and became evident earlier in the lisinopril group.83 The aim of the AMANDHA study (Adición de MANidipino al tratamiento de Diabéticos tipo 2 Hipertensos con microAlbuminuria) was to compare the efficacy and safety of adding manidipine vs. amlodipine to the treatment of diabetic patients with uncontrolled hypertension and microalbuminuria despite a full-dose treatment with a renin–angiotensin system blocker for at least 6 months. Manidipine and amlodipine decreased BP values to a similar extent; urinary albumin excretion was reduced by 62.7% vs. 16.6%, respectively, at the end of the extension phase.84
The DIAL (Diabetes Ipertensione Albuminuria Lercanidipina) study evaluated the effectiveness of lercanidipine in comparison with ramipril on the reduction in UAE in patients with type 2 diabetes and persistent microalbuminuria. After 9–12 months of follow-up, a significant reduction in UAE was observed, without differences between the groups.85 More recently, the ZAFRA study has shown a positive effect on proteinuria of the combination of the new CCB lercanidipine (10 mg) and renin–angiotensin axis-blocking drugs. The plasma creatinine concentration did not change, but creatinine clearance measured by a 24 h urine collection increased at the final visit. Proteinuria significantly decreased at the end of the follow-up.86 In a second trial, a higher dose of lercanidipine (20 mg) was associated with renin–angiotensin axis-blocking drugs in a group of patients with proteinuric renal disease. Proteinuria significantly decreased at the end of the follow-up period.87
A plethora of new calcium antagonists have been introduced in the Far East, but they are not authorized in Europe or the United States of America. One of them is efonidipine. A randomized crossover study compared the chronic effects of efonidipine and amlodipine on proteinuria in patients with chronic glomerulonephritis. Urinary protein excretion was significantly less in the efonidipine period than in the amlodipine period. Serum albumin was significantly higher in the efonidipine period than in the amlodipine period.88 In diabetic patients, significant increases in serum creatinine and urinary albumin and a significant decrease in the estimated GFR were observed in the amlodipine group but not in the efonidipine group.89 A study evaluated the effect of efonidipine and ACEIs on BP and proteinuria in hypertensive patients with renal impairment or chronic renal parenchymal disease. Proteinuria tended to decrease in both groups, with a significant reduction observed in proteinuric patients (>1 g per day). Of interest, efonidipine decreased proteinuria in proteinuric patients who failed to manifest decreases in systemic BP.90
In clinical studies, cilnidipine significantly decreased urinary albumin excretion without affecting serum creatinine concentration in hypertensive patients,91 which is comparable to the action of the ACEI, benazepril.92 Other studies have shown that the renoprotective effect of cilnidipine was greater than that of pure L-type Ca2+ channel blockers.93 Furthermore, the combination of cilnidipine and valsartan was shown to decrease the albumin/creatinine ratio more markedly than valsartan alone.94 Recently, the multicenter, open-labeled and randomized trial, Cilnidipine vs. Amlodipine Randomized Trial for Evaluation in Renal disease (CARTER), has shown that cilnidipine is superior to amlodipine in preventing the progression of proteinuria in patients with hypertension and chronic renal disease when coupled with a renin–angiotensin system inhibitor.95 However, the CARTER study found that the antiproteinuric effect of cilnidipine did not significantly differ from that of amlodipine in the diabetic subgroup of patients with macroproteinuria. In the same way, the SAKURA study did not find that cilnidipine was superior to amlodipine for the treatment of albuminuria in hypertensive patients with early-stage diabetic nephropathy.96 Nevertheless, in another trial, cilnidipine was again shown to be superior to amlodipine in preventing the progression of proteinuria in hypertensive patients, even after undergoing treatment with renin–angiotensin system inhibitors.97
Compared with amlodipine, benidipine enhanced the maximum recommended dose of ARBs (80 mg telmisartan daily and 40 mg olmesartan daily) while reducing albuminuria and plasma aldosterone levels over a 6-month study period, independent of its BP-lowering effect.98, 99 An open-labeled randomized trial compared the effects of benidipine with cilnidipine in hypertensive patients with CKD. The patients who were already being treated with ARBs received benidipine or cilnidipine. After 12 months of treatment, a significant and comparable reduction in SBP and DBP in both groups was observed. The urinary protein:creatinine ratio was significantly decreased in both groups after 3 months of treatment and thereafter; however, the difference between groups was not significant after 12 months of treatment. Benidipine exerted an antiproteinuric effect to a greater extent than cilnidipine in patients with diabetes.100 In another trial, benidipine treatment reduced the proteinuria in hypertensive patients with CKD, with the most significant percentage decrease of proteinuria observed in elderly patients.101
Thamcharoen et al.102 performed a meta-analysis on the effect of N- and T-type CCBs on proteinuria, BP and kidney function in hypertensive patients. They searched for single-arm studies and RCTs that examined the effect of L/N- and L/T-type CCBs as an add-on therapy, compared with a standard antihypertensive regimen for proteinuria, on hemodynamic and kidney-related parameters in hypertensive patients with proteinuria. Random-effect model meta-analyses were used to compute changes in outcomes of interest. Seventeen RCTs were found, representing 1905 patients treated with benidipine, azelnidipine or cilnidipine. By meta-analysis, L/N- and L/T-type CCB add-on therapy did not yield significant changes in SBP or DBP compared with standard treatment, but there was a significant decrease in the pulse rate. However, L/N- and L/T-type CCBs resulted in a significant standardized net decrease in albuminuria and proteinuria, along with a standardized net improvement in the estimated GFR and serum creatinine. The conclusion was that despite no additional lowering effect on BP, L/N- and L/T-type CCBs combined with a renin–angiotensin–aldosterone system blocker provided a decrease in proteinuria and improvement in kidney function.
Ending remarks
The enormous amount of information regarding the renoprotective effects of calcium antagonists is complex, and there are conflicting data coming from the reported trials. Nevertheless, the following conclusions can be drawn:
-
1
The use of CCBs in hypertensive patients with renal disease is safe and has no deleterious effects on renal function.
-
2
CCBs may be better than diuretics and beta-blockers at protecting renal function against hypertension.
-
3
Renin–angiotensin axis-blocking drugs are more effective than CCBs at reducing proteinuria.
-
4
The combination of CCBs and renin–angiotensin axis-blocking drugs may be beneficial in improving the renoprotective effects of ACEI and ARBs administered alone.
-
5
Combining renin–angiotensin axis drugs with CCBs is better than a combination with diuretics for preserving renal function and reducing cardiovascular morbidity.
-
6
New-generation CCBs, with vasodilator action on both afferent and efferent glomerular arterioles, may have interesting renoprotective effects, as suggested by some recent reports.
References
Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Ford CE, Ford CE, Shulman NB, Stamler J . Blood pressure and endstage renal disease in men. N Engl J Med 1996; 334: 13–18.
Ruilope LM, Campo C, Rodriguez-Artalejo F, Lahera V, Garcia-Robles R, Rodicio JL . Blood pressure and renal function: therapeutic implications. J Hypertens 1996; 14: 1259–1263.
Robles NR . Calcium antagonists and renal disease. In: Robles NR (ed). Calcium Channel Blockers and Renal Disease. Nova Science Publishers: New York, USA. 2009, pp 105–133.
Tarif N, Bakris GL . Preservation of renal function: the spectrum of effects by calcium-channel blockers. Nephrol Dial Transplant 1997; 12: 2244–2250.
Schwartz A . Molecular and cellular aspects of calcium channel antagonism. Am J Cardiol 1992; 70: 6F–8F.
Gaber L, Walton C, Brown S, Bakris GL . Effects of different antihypertensive treatments on morphologic progression of diabetic nephropathy in uninephrectomized dogs. Kidney Int 1994; 46: 161–169.
Griffin KA, Picken M, Bakris GL, Bidani AK . Comparative effects of selective T- and L-type calcium channel blockers in the remnant kidney model. Hypertension 2001; 37: 1268–1272.
Rubio-Guerra AF . Non-dihydropyridinic calcium antagonists and renal disease. In: Robles NR (ed). Calcium Channel Blockers and Renal Disease. Nova Science Publishers: New York, USA. 2009.
Nathan S, Pepine CJ, Bakris GL . Calcium antagonist. Effects on cardio-renal risk in hypertensive patients. Hypertension 2005; 46: 637–642.
Daina E, Cravedi P, Alpa M, Roccatello D, Gamba S, Perna A, Gaspari F, Remuzzi G, Ruggenenti P . A multidrug, antiproteinuric approach to alport syndrome: a ten-year cohort study. Nephron 2015; 130: 13–20.
Pérez-Maraver M, Carrera MJ, Micaló T, Sahun M, Vinzia C, Soler J, Montanya E . Renoprotective effect of diltiazem in hypertensive type 2 diabetic patients with persistent microalbuminuria despite ACE inhibitor treatment. Diabetes Res Clin Pract 2005; 70: 13–19.
Smith AC, Toto R, Bakris GL . Differential effects of calcium channel blockers on size selectivity of proteinuria in diabetic glomerulopathy. Kidney Int 1998; 54: 889–896.
Bakris GL, Copley JB, Vicknair N, Sadler R, Leurgans S . Calcium channel blockers versus other antihypertensive therapies on progression of NIDDM associated nephropathy. Kidney Int 1996; 50: 1641–1650.
Bakris GL, Copley JB, Vicknair N, Sadler R, Leurgans S . Calcium channel blockers versus other antihypertensive therapies on progression of NIDDM associated nephropathy. Kidney Int 1995; 50: 1641—1650.
Bakris GL, Mangrum A, Copley JB, Vicknair N, Sadler R . Effect of calcium channel or beta-blockade on the progression of diabetic nephropathy in African Americans. Hypertension 1997; 29: 744–750.
Fernandez R, Garcia J, Rodriguez JC, Garrido J, Redon J . Effect of two antihypertensive combinations on metabolic control in type-2 diabetic hypertensive patients with albuminuria. A randomized double blind study. J Hum Hypertens 2001; 15: 849–856.
Preston RA, Materson BJ, Reda DJ, Hamburger RJ, Williams DW, Smith MH . Proteinuria in mild to moderate hypertension: results of the VA cooperative study of six antihypertensive agents and placebo. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Clin Nephrol 1997; 47: 310–315.
Ruggenenti P, Fassi A, Ilieva AP, Bruno S, Ilieve IP, Brusegan V, Rubis N, Gherardi G, Arnoldi F, Ganeva M, Ene-Iordache B, Gaspari F, Perna A, Bossi A, Trevisan R, Dodesini AR, Remuzzi G . Bergamo Nephrologic Diabetes Complications Trial (BENEDICT) Investigators. Preventing microalbuminiria in type 2 diabetes. N Engl J Med 2004; 351: 1941–1951.
Boero R, Rollino C, Massara C, Berto IM, Perosa P, Vagelli G, Lanfranco G, Quarello F . The verapamil versus amlodipine in nondiabetic nephropathies treated with trandolapril (VVANNTT) study. Am J Kidney Dis 2003; 42: 67–75.
Bakris GL, Weir MR, Secic M, Campbell B, Weis-McNulty A . Differential effects of calcium antagonist subclasses on markers of nephropathy progression. Kidney Int 2004; 65: 1991–2002.
Sweeney C, Shultz P, Raij L . Interactions of the endothelium and mesangium in glomerular injury. J Am Soc Nephrol 1990; 1: S13–S20.
Raij L, Keane W . Glomerular mesangium: its function and relationship to angiotensin II. Am J Med 1985; 79 (Suppl 36): 24–30.
Ruilope LM, Campo C, Rodriguez-Artalejo F, Lahera V, Garcia-Robles R, Rodicio JL . Blood pressure and renal function: therapeutic implications. J Hypertens 1996; 14: 1259–1263.
Sugiura T, Imai E, Moriyama T, Horio M, Hori M . Calcium channel blockers inhibit proliferation and matrix production in rat mesangial cells: possible mechanism of suppression of AP-1 and CREB activities. Nephron 2000; 85: 71–80.
Ono T, Liu N, Kusano H, Nogaki F, Makino T, Muso E, Sasayama S . Broad antiproliferative effects of benidipine on cultured human mesangial cells in cell cycle phases. Am J Nephrol 2002; 22: 581–586.
Roth M, Keul R, Emmons LR, Horl WH, Block LH . Manidipine regulates the transcription of cytokine genes. Proc Natl Acad Sci USA 1992; 89: 4071–4075.
Hayashi M, Yamaji Y, Nakazato Y, Saruta T . The effects of calcium channel blockers on nuclear factor kappa B activation in the mesangial cells. Hypertens Res 2000; 23: 521–525.
Fukuo K, Yang J, Yasuda O, Mogi M, Suhara T, Sato N, Suzuki T, Morimoto S, Ogihara T . Nifedipine indirectly upregulates superoxide dismutase expression in endotelial cells via vascular smooth muscle cell-dependent pathways. Circulation 2002; 106: 356–361.
Chen L, Haught WH, Yang B, Saldeen TG, Parathasarathy S, Mehta JL . Preservation of endogenous antioxidant activity and inhibition of lipid peroxidation as common mechanisms of anti-atherosclerotic effects of vitamin E, lovastatin and amlodipine. J Am Coll Cardiol 1997; 30: 569–575.
Lander HR . An essential role for free radicals and derived species in signal transduction. FASEB J 1997; 11: 118–124.
Van Amsterdam FTM, Roveri A, Maiorino M, Ratti E, Ursini F . Lacidipine: a dihydropyridine calcium antagonist with antioxidant activity. Free Rad Biol Med 1992; 12: 183–187.
Cominacini L, Garbin U, Fratta Pasini A, Paulon T, Davoli A, Campagnola M, Marchi E, Pastorino AM, Gaviraghi G, Lo Cascio V . Lacidipine inhibits the activation of the transcription factor Nf-kappaB and the expression of adhesion molecules induced by pro-oxidant signals on endotelial cells. J Hypertens 1997; 15: 1633–1639.
Epstein M . Calcium antagonists and renal protection: Emerging perspectives. J Hypertens 1998; 18 (Suppl 4): S17–S25.
Brooks DP . Endothelin: the ‘prime suspect’ in kidney disease. News Physiol Sci 1997; 12: 83–89.
Fujita K, Matsumura Y, Miyazaki Y, Hashimoto N, Takaoka M, Morimoto S . ETA receptor-mediated role of endothelin in the kidney of DOCA-salt hypertensive rats. Life Sci 1995; 58: PL1–PL7.
Hocher B, Rohmeiss P, Zart R, Diekmann F, Vogt V, Metz D, Fakhury M, Gretz N, Bauer C, Koppenhagen K, Neumayer HH, Distler A . Function and expression of endothelin receptor subtypes in the kidneys of spontaneously hypertensive rats. Cardiovasc Res 1996; 31: 499–510.
Gurbanov K, Rubinstein I, Hoffman A, Abassi Z, Better OS, Winaver J . Differential regulation of renal regional blood flow by endothelin-1. Am J Physiol 1996; 271: F1166–F1172.
Tsuchiya K, Naruse M, Sanaka T, Naruse K, Nitta K, Demura H, Sugino N . Effects of endothelin on renal regional blood flow in dogs. Eur J Pharmacol 1989; 166: 541–543.
Cowley AW Jr . Role of the renal medulla in volume and arterial pressure regulation. Am J Physiol 1997; 273: R1–R15.
Lerman A, Edwards BS, Hallett JW, Heublein DM, Sandberg SM, Burnett JC . Circulating and tissue endothelin immunoreactivity in advanced atherosclerosis. N Engl J Med 1991; 325: 997–1001.
Schiffrin EL, Thibault G . Plasma endothelin in human essential hypertension. Am J Hypertens 1991; 4: 303–308.
Salomonsson M, Sorensen CM, Arendshorst WJ, Steendahl J, Holstein-Rathlou NH . Calcium handling in afferent arterioles. Acta Physiol Scand 2004; 181: 421–429.
Richard S . Effects of calcium antagonists in renal hemodynamics. In: Robles NR (ed). Calcium Channel Blockers and Renal Disease. Nova Science Publishers: New York, USA. 2009.
Hansen PB, Jensen LB, Andreasen D, Friis UG, Skott O . Vascular smooth muscle cells express the α1A subunit of a P-/Q-type voltage-dependent Ca2+ channel, and it is functionally important in renal afferent arterioles. Circ Res 2000; 87: 896–902.
Diochot S, Richard S, Baldy-Moulinier M, Nargeot J, Valmier J . Dihydropyridines, phenylalkylamines and benzothiazepines block N-, P/Q- and R-type calcium currents. Pflugers Arch 1995; 431: 10–19.
Neveu D, Quignard JF, Fernandez A, Richard S, Nargeot J . Differential beta-adrenergic regulation and phenotypic modulation of voltage-gated calcium currents in rat aortic myocytes. J Physiol 1994; 479 (Pt 2): 171–182.
Gustafsson F, Andreasen D, Salomonsson M, Jensen BL, Holstein-Rathlou N . Conducted vasoconstriction in rat mesenteric arterioles: role for dihydropyridine-insensitive Ca2+ channels. Am J Physiol Heart Circ Physiol 2001; 280: H582–H590.
Hayashi K, Ozawa Y, Fujiwara K, Wakino S, Kumagai H, Saruta T . Role of actions of calcium antagonists on efferent arterioles—with special references to glomerular hypertension. Am J Nephrol 2003; 23: 229.
Honda M, Hayashi K, Matsuda H, Kubota E, Tokuyama H, Okubo K, Sugino N . Divergent renal vasodilator action of L- and T-type calcium antagonists in vivo. J Hypertens 2001; 19: 2031.
Furukawa T, Nukada T, Miura R, Ooga K, Honda M, Watanabe S, Koganesawa S, Isshiki T . Differential blocking action of dihydropyridine Ca2+ antagonists on a T-type Ca2+ channel (alpha1G) expressed in Xenopus oocytes. J Cardiovasc Pharmacol 2005; 45: 241.
Ozawa Y, Hayashi K, Nagahama T, Fujiwara K, Saruta T . Effect of T-type selective calcium antagonist on renal microcirculation: studies in the isolated perfused hydronephrotic kidney. Hypertension 2001; 38: 343.
Romanin C, Seydl K, Glossmann H, Schindler H . Activity of cardiac L-type Ca2+ channels is sensitive to cytoplasmic calcium. Pflugers Arch 1992; 420: 410.
Furukawa T, Yamakawa T, Midera T, Sagawa T, Mori Y, Nukada T . Selectivities of dihydropyridine derivatives in blocking Ca(2+) channel subtypes expressed in Xenopus oocytes. J Pharmacol Exp Ther 1999; 291: 464.
Furukawa T, Nukada T, Namiki Y, Miyashita Y, Hatsuno K, Ueno Y, Yamakawa T, Isshiki T . Five different profiles of dihydropyridines in blocking T-type Ca(2+) channel subtypes (Ca(v)3.1 (alpha(1G)), Ca(v)3.2 (alpha(1H)), and Ca(v)3.3 (alpha(1I))) expressed in Xenopus oocytes. Eur J Pharmacol 2009; 613: 100–107.
Hayashi K, Wakino S, Sugano N, Ozawa Y, Homma K, Saruta T . Ca2+ channel subtypes and pharmacology in the kidney. Circ Res 2007; 100: 342.
Hayashi K, Wakino S, Homma K, Sugano N, Saruta T . Pathophysiological significance of T-type Ca2+ channels: role of T-type Ca2+ channels in renal microcirculation. J Pharmacol Sci 2005; 99: 221.
Tsutamoto T, Tanaka T, Nishiyama K, Yamaji M, Kawahara C, Fujii M, Yamamoto T, Horie M . Long-term effect of efonidipine therapy on plasma aldosterone and left ventricular mass index in patients with essential hypertension. Hypertens Res 2009; 32: 670–674.
Baba S, J-MIND Study Group. Nifedipine and enalapril equally reduce the progression of nephropathy in hypertensive type 2 diabetics. Diabetes Res Clin Pract 2001; 54: 191–201.
Fogari R, Derosa G, Zoppi A, Preti P, Lazzari P, Destro M, Fogari E, Rinaldi A, Mugellini A . Effect of telmisartan-amlodipine combination at different doses on urinary albumin excretion in hypertensive diabetic patients with microalbuminuria. Am J Hypertens 2007; 20: 417–422.
Schnack C, Capek M, Banyai M, Kautzky-Willer A, Prager R, Schernthaner G . Long-term treatment with nifedipine reduces urinary albumin excretion and glomerular filtration rate in normotensive type 1 diabetic patients with microalbuminuria. Acta Diabetol 1994; 31: 14–18.
Voyaki SM, Staessen JA, Thijs L, Wang JG, Efstratopoulos AD, Birkenhäger WH, de Leeuw PW, Leonetti G, Nachev C, Rodicio JL, Tuomilehto J, Fagard R, Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Follow-up of renal function in treated and untreated older patients with isolated systolic hypertension. J Hypertens 2001; 19: 511–519.
National Intervention Cooperative Study in Elderly Hypertensives Study Group. Randomized double-blind comparison of a calcium antagonist and a diuretic in elderly hypertensives. Hypertension 1999; 34: 1129–1133.
Brown MJ, Palmer CR, Castaigne A, de Leeuw PW, Mancia G, Rosenthal T, Ruilope LM . Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS Study: intervention as a Goal in Hypertension Treatment (INSIGHT). Lancet 2000; 356: 366–372.
The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: the Antihypertensive and Lipid Lowering treatment to prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288: 2981–2997.
Agodoa LY, Appel L, Bakris GL, Beck G, Bourgoignie J, Brigs JP, Charleston J, Cheek D, Cleveland W, Douglas JG, Douglas M, Dowie D, Faulkner M, Gabriel A, Gassman J, Greene T, Hall Y, Hebert L, Hiremath L, Jamerson K, Johnson CJ, Kopple J, Kusek J, Lash J, Lea J, Lewis JB, Lipkowitz M, Massry S, Middleton J, Miller ER 3rd, Norris K, O'Connor D, Ojo A, Phillips RA, Pogue V, Rahman M, Randall OS, Rostand S, Schulman G, Smith W, Thornley-Brown D, Tisher CC, Toto RD, Wright JT Jr, Xu S, African American Study of Kidney Disease and Hypertension (AASK) Study Group. Effect of ramipril vs amlodipine on renal outcomes in hypertensive nephrosclerosis: a randomized controlled trial. JAMA 2001; 285: 2719–2728.
Marin R, Ruilope LM, Aljama P, Aranda P, Segura J, Diez J, Investigators of the ESPIRAL Study. Efecto del tratamiento antihipertensivo Sobre la Progresión de la Insuficiencia RenAL en pacientes no diabéticos. A random comparison of fosinopril and nifedipine GITS in patients with primary renal disease. J Hypertens 2001; 19: 1871–1876.
Esnault VL, Brown EA, Apetrei E, Bagon J, Calvo C, Dechatel R, Holdaas H, Krcmery S, Kobalava Z, Amlodipine Versus Enalapril in Renal failure (AVER) Study Group. The effects of amlodipine and enalapril on renal function in adults with hypertension and nondiabetic nephropathies: A 3-year, randomized, multicenter, double-blind, placebo-controlled study. Clin Ther 2008; 30: 482–498.
Ziakka S, Kaperonis N, Ferentinou E, Karakasis P, Ntatsis G, Kourvelou C, Papagalanis N . Calcium channels blockers and progression of kidney disease. Ren Fail 2007; 29: 1003–1012.
Nakamura T, Inoue T, Suzuki T, Kawagoe Y, Ueda Y, Koide H, Node K . Comparison of renal and vascular protective effects between telmisartan and amlodipine in hypertensive patients with chronic kidney disease with mild renal insufficiency. Hypertens Res 2008; 31: 841–850.
Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, Ritz E, Atkins RC, Rohde R, Raz I, Collaborative Study Group. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001; 345: 851–860.
Dahlöf B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J, ASCOT Investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicenter randomised controlled trial. Lancet 2005; 366: 895–906.
Herlitz H, Harris K, Risler T, Bonner G, Bernheim J, Channard J, Aurell M . The effect of an ACE inhibitor and a calcium antagonist in the progression of renal disease: the Nephros study. Nephrol Dial Transplant 2001; 16: 2158–2165.
Shigihara T, Sato A, Hayashi K, Saruta T . Effect of combination therapy of angiotensin-converting enzyme inhibitor plus calcium channel blocker on urinary albumin excretion in hypertensive microalbuminuric patients with type II diabetes. Hypertens Res 2000; 23: 219–226.
Fogari R, Preti P, Zoppi A, Rinaldi A, Corradi L, Pasotti C, Poletti L, Marasi G, Derosa G, Mugellini A, Voglini C, Lazzari P . Effects of amlodipine fosinopril combination on microalbuminuria in hypertensive type 2 diabetic patients. Am J Hypertens 2002; 15: 1042–1049.
Ruggenenti P, Perna A, Loriga G, Ganeva M, Ene-Iordache B, Turturro M, Ruggenenti P, Perna A, Loriga G, Ganeva M, Ene-Iordache B, Turturro M . Blood pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial. Lancet 2005; 365: 939–946.
Bakris GL, Toto RD, McCullough PA, Rocha R, Purkayastha D, Davis P, GUARD (Gauging Albuminuria Reduction With Lotrel in Diabetic Patients With Hypertension) Study Investigators. Effects of different ACE inhibitor combinations on albuminuria: results of the GUARD study. Kidney Int 2008; 73: 1303–1309.
Jamerson K, Weber MA, Bakris GL, Dahlöf B, Pitt B, Shi V, Hester A, Gupte J, Gatlin M, Velazquez EJ, ACCOMPLISH Trial Investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk. patients. N Engl J Med 2008; 359: 2417–2428.
Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, Velazquez EJ, Staikos-Byrne L, Kelly RY, Shi V, Chiang YT, Weber MA, ACCOMPLISH Trial investigators for the ACCOMPLISH Trial investigators. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet 2010; 375: 1173–1181.
Sarafidis PA, Bakris G, Weber M, Pitt B, Dahlof B, Velazquez EJ, Shi V, Hester A, Gupte J, Gatlin M . Changes in glomerular filtration rate with benazepril plus amlodipine or benazepril plus hydrochlorothiazide treatment in hypertensive patients at high cardiovascular risk; an analysis of the ACCOMPLISH trial. http://www.abstracts2viewcom/wcn/viewphp?nu=WCN09L_4552009. Accessed 30 November 2010.
Jamerson KA, Bakris GL, Weber MA . 24-h ambulatory blood pressure in the ACCOMPLISH trial. N Engl J Med 2010; 363: 98.
Bellinghieri G, Mazzaglia G, Savica V, Santoro D . Effects of manidipine and nifedipine on blood pressure and renal function in patients with chronic renal failure: a multicenter randomized controlled trial. Ren Fail 2003; 25: 681–689.
Del Vecchio L, Pozzi M, Salvetti A, Maschio G, Fusaroli M, Rovati C, Antonucci F, Cascone C, Scanferla F, Panichi V, Sturani A, Locatelli F, Manidipine Study Group. Efficacy and tolerability of manidipine in the treatment of hypertension in patients with non-diabetic chronic kidney disease without glomerular disease. Prospective, randomized, double-blind study of parallel groups in comparison with enalapril. J Nephrol 2004; 17: 261–269.
Fogari R, Mugellini A, Zoppi A, Lazzari P, Destro M, Rinaldi A, Preti P . Effect of successful hypertension control by manidipine or lisinopril on albuminuria and left ventricular mass in diabetic hypertensive patients with microalbuminuria. Eur J Clin Pharmacol 2005; 61: 483–490.
Martinez-Martin FJ, Saiz-Satjes M . Add-on manidipine versus amlodipine in diabetic patients with hypertension and microalbuminuria: the AMANDHA study. Expert Rev Cardiovasc Ther 2008; 6: 1347–1355.
Dalla Vestra M, Pozza G, Mosca A, Grazioli V, Lapolla A, Fioretto P, Crepaldi G . Effect of lercanidipine compared with ramipril on albumin excretion rate in hypertensive type II diabetic patients with microalbuminuria: DIAL Study (diabete, ipertensione, albuminuria, lercanidipina). Diab Nutr Metab 2004; 17: 259–266.
Robles NR, Ocon J, Gomez Campderá F, Manjon M, Pastor L, Herrera J, Villatoro J, Calls J, Torrijos J, Rodríguez VI, Rodriguez MM, Mendez ML, Morey A, Martinez FI, Marco J, Liebana A, Rincon B, Tornero F . Lercanidipine in chronic renal failure patients: the ZAFRA study. Ren Fail 2005; 27: 73–80.
Robles NR, Romero B, Garcia de Vinuesa E, Sánchez-Casado E, Cubero JJ . Treatment of proteinuria with lercanidipine associated to renin-angiotensin axis blocking drugs. Ren Fail 2010; 32: 192–197.
Ichitmitsu T, Kameda T, Akashiba A, Takahashi T, Ohta S, Yoshii M, Minami J, Ono H, Numabe A, Matsuoka H . Efonidipine reduces proteinuria and plasma aldosterone in patients with chronic glomerulonephritis. Hypertens Res 2007; 30: 621–626.
Sasaki H, Saiki A, Endo K, Ban N, Yamaguchi T, Kawana H, Nagayama D, Ohhira M, Oyama T, Miyashita Y, Shirai K . Protective effects of efonidipine, a T- and L-type calcium channel blocker, on renal function and arterial stiffness in type 2 diabetic patients with hypertension and nephropathy. J Atheroscler Thromb 2009; 16: 568–575.
Hayashi K, Kumagai H, Saruta T . Effect of efonidipine and ACE inhibitors on proteinuria in human hypertension with renal impairment. Am J Hypertens 2003; 16: 116–122.
Tsuchihashi T, Ueno M, Tominaga M, Kajioka T, Onaka U, Eto K, Goto K . Antiproteinuric effect of N type calcium channel blocker, cilnidipine. Clin Exp Hypertens 2005; 27: 583–591.
Rose GW, Ikebukoro H . Cilnidipine as effective as benazepril for control of blood pressure and proteinuria in hypertensive patients with benign nephrosclerosis. Hypertens Res 2001; 24: 377–383.
Kojima S, Shida M, Yokoyama H . Comparison between cilnidipine and amlodipine besilate with respect to proteinuria in hypertensive patients with renal diseases. Hypertens Res 2004; 27: 379–385.
Katayama K, Nomura S, Ishikawa H, Murata T, Koyabu S, Nakano T . Comparison between valsartan and valsartan plus cilnidipine in type II diabetics with normo- and microalbuminuria. Kidney Int 2006; 70: 151–156.
Fujita T, Ando K, Nishimura H, Ideura T, Yasuda G, Isshiki M, Takahashi K, Cilnidipine versus Amlodipine Randomised Trial for Evaluation in Renal Desease(CARTER) Study Investigators. Antiproteinuric effect of calcium channel blocker cilnidipine added to renin angiotensin inhibition in hypertensive patients with chronic renal disease. Kidney Int 2007; 72: 1543–1549.
Ando K, Ueshima K, Tanaka T, Kosugi S, Sato T, Matsuoka H, Nakao K, Fujita T . Comparison of the antialbuminuric effects of L-/N-type and L-type calcium channel blockers in hypertensive patients with diabetes and microalbuminuria: the Study of Assessment for Kidney Function by Urinary Microalbumin in Randomized (SAKURA) Trial. Int J Med Sci 2013; 10: 1209–1216.
Miwa Y, Tsuchihashi T, Ohta Y, Tominaga M, Kawano Y, Sasaguri T, Ueno M, Matsuoka H . Antiproteinuric effect of cilnidipine in hypertensive Japanese treated with renin-angiotensin-system inhibitors-a multicenter, open, randomized trial using 24-hour urine collection. Clin Exp Hypertens 2010; 32: 400–405.
Abe M, Okada K, Maruyama N, Matsumoto S, Maruyama T, Fujita T, Matsumoto K, Soma M . Benidipine reduces albuminuria and plasma aldosterone in mild-to-moderate stage chronic kidney disease with albuminuria. Hypertens Res 2011; 34: 268–273.
Abe M, Okada K, Maruyama T, Maruyama N, Matsumoto K . Comparison of the antiproteinuric effects of the calcium channel blockers benidipine and amlodipine administered in combination with angiotensin receptor blockers to hypertensive patients with stage 3–5 chronic kidney disease. Hypertens Res 2009; 32: 270–275.
Abe M, Okada K, Maruyama N, Matsumoto S, Maruyama T, Fujita T, Matsumoto K, Soma M . Comparison between the antiproteinuric effects of the calcium channel blockers benidipine and cilnidipine in combination with angiotensin receptor blockers in hypertensive patients with chronic kidney disease. Expert Opin Investig Drugs 2010; 19: 1027–1037.
Tomino Y, Shimizu Y, Hamada C, Kurusu A, Ohsawa I, Suzuki Y, Tsuge T, Io H, Kobayashi N, Takeda Y, Asanuma K, Tanaka Y, Suzuki H, Nakata J, Takara K, Horikoshi S . One-year results of an open-label study on antiproteinuric effect of benidipine in elderly patients with chronic kidney disease. J Nephrol 2011; 24: 756–763.
Thamcharoen N, Susantitaphong P, Wongrakpanich S, Chongsathidkiet P, Tantrachoti P, Pitukweerakul S, Avihingsanon Y, Praditpornsilpa K, Jaber BL, Eiam-Ong S . Effect of N- and T-type calcium channel blocker on proteinuria, blood pressure and kidney function in hypertensive patients: a meta-analysis. Hypertens Res 2015; 38: 847–855.
Ranieri G, Andriani A, Lamontanara G, De Cesaris R . Effects of lisinopril and amlodipine on microalbuminuria and renal function in patients with hypertension. Clin Pharmacol Ther 1994; 56: 323–330.
Iino Y, Hayashi M, Kawamura T, Shiigai T, Tomino Y, Yamada K, Kitajima T, Ideura T, Koyama A, Sugisaki T, Suzuki H, Umemura S, Kawaguchii Y, Uchida S, Kuwahara M, Yamazaki T, Japanese Losartan Therapy Intended for the Global Renal Protection in Hypertensive Patients (JLIGHT) Study Investigators. Renoprotective effect of losartan in comparison to amlodipine in patients with chronic kidney disease and hypertension—a report of the Japanese Losartan Therapy Intended for the Global Renal Protection in Hypertensive Patients (JLIGHT) study. Hypertens Res 2004; 27: 21–30.
Kuriyama S, Tomonari H, Tokudome G, Horiguchi M, Hayashi H, Kobayashi H, Ishikawa M, Hosoya T . Antiproteinuric effects of combined antihypertensive therapies in patients with overt type 2 diabetic nephropathy. Hypertens Res 2002; 25: 849–855.
Ecder T, Chapman AB, Brosnahan GM, Edelstein CL, Johnson AM, Schrier RW . Effect of antihypertensive therapy on renal function and urinary albumin excretion in hypertensive patients with autosomal dominant polycystic kidney disease. Am J Kidney Dis 2000; 35: 427–432.
Fernandez Andrade C, Russo D, Iversen B, Zucchelli P, Aranda P, Guerra L, Casado S . Comparison of losartan and amlodipine in renally impaired hypertensive patients. Kidney Int 1998; 54 (Suppl 68): S120–S124.
Viberti G, Wheeldon NG, for the MicroAlbuminuria Reduction With VALsartan (MARVAL) Study Investigators. Microalbuminuria reduction with valsartan in patients with type 2 diabetes mellitus: a blood pressure–independent effect. Circulation 2002; 106: 672–678.
Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S . Arner P; Irbesartan in Patients with Type 2 Diabetes and Microalbuminuria Study Group. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med 2001; 345: 870–878.
Praga M, Fernandez Andrade C, Luño J, Arias M, Poveda R, Mora J, Prat MV, Rivera F, Galceran JM, Ara JM, Aguirre R, Bernis C, Marín R, Campistol JM . l. Antiproteinuric efficacy of losartan in comparison with amlodipine in non-diabetic proteinuric renal diseases: a double-blind, randomised clinical trial. Nephrol Dial Transplant 2003; 18: 1806–1813.
Crepaldi G, Carta Q, Deferrari G, Mangili R, Navalesi R, Santeusanio F, Crepaldi G, Carta Q, Deferrari G, Mangili R, Navalesi R, Santeusanio F . Effects of lisinopril and nifedipine on the progression to overt albuminuria in IDDM patients with incipient nephropathy and normal blood pressure. The Italian Microalbuminuria Study Group in IDDM. Diabetes Care 1998; 21: 104–110.
Crepaldi G, Carraro A, Brocco E, Adezati L, Andreani D, Bompiani G, Brunetti P, Fedele D, Giorgino R, Giustina G . Hypertension and non-insulin-dependent diabetes. A comparison between an angiotensin-converting enzyme inhibitor and a calcium antagonist. Acta Diabetol 1995; 32: 203–208.
Giordano M, Sanders LR, Castellino P, Canessa ML, DeFronzo RA . Effect of alpha-adrenergic blockers, ACE inhibitors, and calcium channel antagonists on renal function in hypertensive non-insulin-dependent diabetic patients. Nephron 1996; 72: 447–453.
O'Donnell MJ, Rowe BR, Lawson N, Horton A, Gyde OH, Barnett AH . Comparison of the effects of an angiotensin converting enzyme inhibitor and a calcium antagonist in hypertensive, macroproteinuric diabetic patients: a randomised double-blind study. J Hum Hypertens 1993; 7: 333–339.
Melbourne Diabetic Nephropathy Study Group. Comparison between perindopril and nifedipine in hypertensive and normotensive diabetic patients with microalbuminuria. BMJ 1991; 302: 210–216.
Leoncini G, Martinoli C, Viazzi F, Ravera M, Parodi D, Ratto E, Vettoretti S, Tomolillo C, Derchi LE, Deferrari G, Pontremoli R . Changes in renal resistive index and urinary albumin excretion in hypertensive patients under long-term treatment with lisinopril or nifedipine GITS. Nephron 2002; 90: 169–173.
Jerums G, Allen TJ, Campbell DJ, Cooper ME, Gilbert RE, Hammond JJ, O'Brien RC, Raffaele J, Tsalamandris C, Melbourne Diabetic Nephropathy Study Group. Long-term renoprotection by perindopril or nifedipine in non-hypertensive patients with Type 2 diabetes and microalbuminuria. Am J Kidney Dis 2001; 37: 890–8990.
Ferder L, Daccordi H, Martello M, Panzalis M, Inserra F . Angiotensin converting enzyme inhibitors versus calcium antagonists in the treatment of diabetic hypertensive patients. Hypertension 1992; 19 (2 Suppl): II237–II242.
Chan JC, Cockram CS, Nicholls MG, Cheung CK, Swaminathan R . Comparison of enalapril and nifedipine in treating non-insulin dependent diabetes associated with hypertension: one year analysis. BMJ 1992; 305: 981–985.
Bilo H, Kluitman E, van Ballegooie E, Potter van Loon BJ, Bakker K, Michels B, Gans R, Donker A . Long term use of captopril or nifedipine in normotensive microalbuminuric patients with insulin-dependent diabetes mellitus. Diabetes Res 1993; 23: 115–122.
Agardh CD, Garcia-Puig J, Charbonnel B, Angelkort B, Barnett AH . Greater reduction of urinary albumin excretion in hypertensive type II diabetic patients with incipient nephropathy by lisinopril than by nifedipine. J Hum Hypertens 1996; 10: 185–192.
The European Study for the Prevention of Renal Disease in Type 1 Diabetes (ESPRIT) Study Group. Effect of 3 years of antihypertensive therapy on renal structure in type 1 diabetic patients with albuminuria. The European Study for the Prevention of Renal Disease in Type 1 Diabetes (ESPRIT). Diabetes 2001; 50: 843–850.
Fogari R, Zoppi A, Corradi L, Mugellini A, Lazzari P, Preti P, Lusardi P . Long-term effects of ramipril and nitrendipine on albuminuria in hypertensive patients with type II diabetes and impaired renal function. J Hum Hypertens 1999; 13: 47–53.
Schrier RW, Estacio RO, Esler A, Mehler P . Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes. Kidney Int 2002; 61: 1086–1097.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Robles, N., Fici, F. & Grassi, G. Dihydropyridine calcium channel blockers and renal disease. Hypertens Res 40, 21–28 (2017). https://doi.org/10.1038/hr.2016.85
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.85
Keywords
This article is cited by
-
L-type calcium channel blocker use and proteinuria among children with chronic kidney diseases
Pediatric Nephrology (2021)
-
PAIT-Survey Follow-Up: Changes in Albuminuria in Hypertensive Diabetic Patients with Mild-Moderate Chronic Kidney Disease
High Blood Pressure & Cardiovascular Prevention (2020)