Abstract
Objective:
On the day of birth, the bleeding time of very low birth-weight (VLBW, <1500 g) neonates is generally prolonged, compared with term neonates. However, their bleeding time generally improves (shortens) over the next 7 to 10 days. Ampicillin can prolong the bleeding times of term and late preterm neonates, but its effect on VLBW neonates, who already have a somewhat prolonged bleeding time initially, is not known.
Syudy Design:
This was a prospective, single-centered, paired, before vs after test of the effect of ampicillin on template bleeding time and PFA-100 time (platelet function analyzer). Ampicillin was dosed at every 12 h intravenously, but decisions about discontinuation were made by the responsible clinician, independent of this study.
Result:
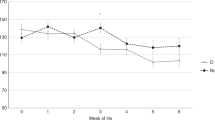
A total of 20 VLBW neonates were studied. They ranged from 23- to 30-weeks gestation at birth and weighed 500 to1410 g. Initial bleeding times averaged 166 s (95% CI, 138 to 194) and initial PFA-100 times averaged 119 s (95% CI, 90 to 148). In all, 10 had ampicillin dosing stopped after a shorter course (4 to 7 doses) and 10 had it continued for a longer course (10 to 15 doses). Blood cultures were sterile in all 20, and no differences in laboratory or clinical features were found between those treated with a shorter vs longer course. After stopping the ampicillin following a short course the bleeding times and PFA-100 times were similar to the initial values. However, after a longer course the bleeding times were prolonged by an average of 2 min, to 284 s (95% CI, 242 to 326; P=0.001 vs initial). The PFA-100 times also trended longer by an average of 44 s (P=0.07). The number of doses of ampicillin received in the first week correlated with the degree of prolongation in bleeding time (r=0.68).
Conclusion:
Over the first week of life, a period when the bleeding time of VLBW neonates normally shortens, the opposite occurred (the bleeding time lengthened) if ⩾10 doses of ampicillin were administered.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Andrew M, Castle V, Mitchell L, Paes B . Modified bleeding time in the infant. Am J Hematol 1989; 30: 190–191.
Borzini P, Laxxaro A, Mazzucco L, Papili F . The in-vitro bleeding time for the screening of platelet function in the newborn: assessment of a normal reference range. Eur J Pediatr 2001; 160: 199–200.
Del Vecchio A, Latini G, Henry E, Christensen RD . Template bleeding times of 240 neonates born at 24 to 41weeks gestation. J Perinatol 2008; 28: 427–431.
Del Vecchio A . Use of the bleeding time in the neonatal intensive care unit. Acta Paediatr Suppl 2002; 91: 82–86.
Sheffield MJ, Lambert DK, Henry E, Christensen RD . Effect of ampicillin on the bleeding time of neonatal intensive care unit patients. J Perinatol 2010; 30: 527–530.
Burroughs SF, Johnson GJ . Beta-lactam antibiotic-induced platelet dysfunction: evidence for irreversible inhibition of platelet activation in vitro and in vivo after prolonged exposure to penicillin. Blood 1990; 75: 1473–1480.
Brown III CH, Bradshaw MJ, Natelson EA, Alfrey Jr CP, Williams Jr TW . Defective platelet function following the administration of penicillin compounds. Blood 1976; 47: 949–956.
Burroughs SF, Johnson GJ . Beta-lactam antibiotics inhibit agonist-stimulated platelet calcium influx. Thromb Haemost 1993; 69: 503–508.
Sheffield MS, Schmutz N, Lambert DK, Henry E, Christensen RD . Ibuprofen lysine administration to neonates with a patent ductus arteriosus: effect on platelet plug formation assessed by in vivo and in vitro measurements. J Perinatol 2009; 29: 39–43.
Israels SJ, Cheang T, McMillan-Ward EM, Cheang M . Evaluation of primary hemostasis in neonates with a new in vitro platelet function analyzer. J Pediatr 2001; 138: 116–119.
Boudewijns M, Raes M, Peeters V, Mewis A, Cartuvvels R, Magerman K et al. Evaluation of platelet function on cord blood in 80 healthy term neonates using the Platelet Function Analyser (PFA-100); shorter in vitro bleeding times in neonates than adults. Eur J Pediatr 2003; 162: 212–213.
Shah U, Ma AD . Tests of platelet function. Curr Opin Hematol 2007; 14: 432–437.
Roschitz B, Sudi K, Köstenberger M, Muntean W . Shorter PFA-100 closure times in neonates than in adults: role of red cells, white cells, platelets and von Willebrand factor. Acta Paediatr 2001; 90: 664–670.
Kim IS, Jeong YH, Kang MK, Koh JS, Park Y, Hwang SJ et al. Correlation of high post-treatment platelet reactivity assessed by light transmittance aggregometry and the VerifyNow P2Y(12) assay. J Thromb Thrombolysis 2010; 30 (4): 486–495.
Morel-Kopp MC, Aboud M, Tan CW, Kulathilake C, Ward C . Whole blood impedance aggregometry detects heparin-induced thrombocytopenia antibodies. Thromb Res 2010; 125: e234–e239.
Hanke AA, Dellweg C, Kienbaum P, Weber CF, Görlinger K, Rahe-Meyer N . Effects of desmopressin on platelet function under conditions of hypothermia and acidosis: an in vitro study using multiple electrode aggregometry*. Anaesthesia 2010; 65 (7): 688–691.
Sharma P, Saxena R . A novel thromboelastographic score to identify overt disseminated intravascular coagulation resulting in a hypocoagulable state. Am J Clin Pathol 2010; 134: 97–102.
Bidet A, Jais C, Puymirat E, Coste P, Nurden A, Jakubowski J et al. VerifyNow and VASP phosphorylation assays give similar results for patients receiving clopidogrel, but they do not always correlate with platelet aggregation. Platelets 2010; 21: 94–100.
Gasparyan AY . Aspirin and clopidogrel resistance: methodological challenges and opportunities. Vasc Health Risk Manag 2010; 6: 109–112.
Chirico G, Barbieri F, Chirico C . Antibiotics for the newborn. J Matern Fetal Neonatal Med 2009; 22 (Suppl 3): 46–49.
Penning-van Beest FJ, Koerselman J, Herings RM . Risk of major bleeding during concomitant use of antibiotic drugs and coumarin anticoagulants. J Thromb Haemost 2008; 6: 284–290.
Ferreiro JL, Sibbing D, Angiolillo DJ . Platelet function testing and risk of bleeding complications. Thromb Haemost 2010; 103: 1128–1135.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest
Rights and permissions
About this article
Cite this article
Sheffield, M., Lambert, D., Baer, V. et al. Effect of ampicillin on bleeding time in very low birth-weight neonates during the first week after birth. J Perinatol 31, 477–480 (2011). https://doi.org/10.1038/jp.2010.154
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.154
Keywords
This article is cited by
-
Ampicillin dosing in premature infants for early-onset sepsis: exposure-driven efficacy, safety, and stewardship
Journal of Perinatology (2022)
-
Results of a two-center, before and after study of piperacillin–tazobactam versus ampicillin and gentamicin as empiric therapy for suspected sepsis at birth in neonates ⩽1500 g
Journal of Perinatology (2013)