Abstract
Healthy neonates exhibit a well-functioning haemostatic system despite peculiarities regarding composition of clotting factors and inhibitors as well as impaired platelet aggregation. Thrombocytopenia and severe bleeding events are feared in sick infants. Recombinant factor VIIa (rFVIIa) is a haemostatic agent used as a last resort in neonates with refractory bleedings. Aim of this study was to investigate in-vitro (i) changes in thrombin generation with different platelet counts, (ii) effects of rFVIIa under conditions of thrombocytopenia and (iii) potentially differing dose-response of rFVIIa in cord blood as a surrogate for neonatal blood compared to adult blood. Thrombin generation parameters were observed in cord blood plasma and adult plasma with various platelet counts, with or without addition of rFVIIa, respectively. Low platelet counts did not influence thrombin generation in cord blood in contrast to adult blood. RFVIIa primarily affected lag time throughout all platelet concentrations. Interestingly, peak height was reduced exclusively in cord blood plasma after addition of rFVIIa. No significant differences regarding dose-response were observed between cord blood and adult blood. In contrast to adult blood, thrombocytopenia in cord blood does not significantly influence thrombin generation. Even at very low platelet counts there is enough negatively charged surface to support rFVIIa action in plasma from cord blood and adult blood in-vitro.
Similar content being viewed by others
Introduction
Healthy infants exhibit a well-functioning haemostatic system in-vivo and are not prone to easy bruising. The plasmatic coagulation system shows some particularities as many coagulation factors are known to be low at time of birth and adapt to adult levels within the first months of life. As shown by Cvirn et al., low procoagulatory factors are also accompanied by low levels of inhibitory factors, which result in a well-balanced haemostasis1.
Platelets of newborns exhibit impaired platelet function in in-vitro aggregation measurements2. This hypoaggregability is not due to a refractory state caused by preactivation during birth3. Multifactorial impairments in signal transduction have been shown to cause this hypoaggregability, including impaired calcium mobilization, lower numbers of α2-adrenergic receptors and lower GTPase activity in Gq-coupled receptors4,5,6. Despite these impairments, the phospholipid composition of neonatal platelet membranes and the overall phospholipid surface expression upon activation are similar to that of adult platelets.
Thrombin generation is a pivotal step in the formation of a stable fibrin clot and highly dependent on negatively charged phospholipids. Neonatal platelets support thrombin generation equally to adult platelets due to the aforementioned comparable phospholipid composition7.
While healthy infants do not tend to bleed, preterm infants and sick infants exhibit a high bleeding risk, particularly when associated with thrombocytopenia which exacerbates the fragility of their haemostatic system. Thrombocytopenia with a threshold in platelet counts below 150,000/µl is observed in up to 35% of children that have to be treated – for any reason – at a neonatal intensive care unit (NICU) and is even more frequent and severe in preterm babies8. In cases of bleeding and/or platelet counts below 20,000/µl, platelet concentrates are given to increase platelet counts. In cases of refractory bleeding, recombinant factor VIIa (rFVIIa) is a therapeutic option9. However, fragility of the neonatal haemostatic system also leads to an increased risk of thrombosis10.
RFVIIa is licensed for haemophiliac patients with inhibitors, Glanzmann thrombasthenia and FVII deficiency, but it is also used in several off-label indications to cease bleeding that cannot be stopped otherwise. Successful administration in neonates and preterm babies11,12,13 as well as in older children14 is described for cases of refractory bleeding events with/without thrombocytopenia. On the other hand, the prophylactic administration of rFVIIa to preterm infants does not prevent intracranial bleeding15. A study about off-label uses of rFVIIa in childhood reports 3655 off-label administrations of rFVIIa; 39.8% in the first year of life, among these 48% within the first month of life. According to this study, venous and/or arterial thrombosis – the main adverse events – occurred in 10.9% of all pediatric off-label administrations (vs. 2.7% of all label administrations). In neonates the incidence rate was 13.6%9.
Mechanism of action of rFVIIa on platelets is a tissue factor-independent activation of FX in presence of phospholipids. Small amounts of thrombin are generated, leading to a thrombin burst16. The hypothesised mechanism of rFVIIa action in a thrombocytopenic state is a boost of the initial thrombin generation through high-dose rFVIIa, resulting in faster platelet activation, thus compensating for the lower number of platelets17.
Calibrated automated thrombography is an in-vitro method enabling time-dependent tracing of thrombin generation in various conditions. It has been shown that this method is applicable to detect states of hypo- as well as hypercoagulability. It is sensitive to clotting factor deficiencies and reflects the effect of anticoagulant drug18,19,20. When performed in the presence of platelet rich plasma the necessary phospholipids are provided by activated platelets. Therefore, this assay is superior to conventional global tests of haemostasis without platelets which are less sensitive and only detect onset of fibrin clot formation.
Considering aforementioned peculiarities of the neonatal haemostatic system we posed the question whether rFVIIa will perform in a similar manner in samples from adults and from cord blood with neonatal platelets featuring exactly those peculiarities. Particularly we wanted to elucidate the following issues: How does thrombin generation differ in samples from cord blood (CB) compared to adult samples when platelet counts are reduced and no rFVIIa is added? Is there a different in-vitro dose-response to rFVIIa in thrombin generation of platelet rich plasma (PRP) from CB compared to adult PRP, and does a lower dose eventually have a sufficient effect on thrombin generation? Does reduction of platelets influence the rFVIIa support of thrombin generation?
Results
First, we evaluated potential differences between thrombin generation of platelet-rich plasma from cord blood and from adult blood. Figure 1 shows schematics of a thrombin generation trace with the corresponding parameters. In our study samples from cord blood exhibit a shorter lag time and time-to-peak and a higher peak. The endogenous thrombin potential (ETP, Table 1), however, is lower, which is similar to previous reports with platelet-poor plasma1. Taken together thrombin generation in platelet-rich plasma from cord blood differs from that of adult blood.
Schematic depiction of a thrombin generation trace. Endogenous thrombin potential (ETP) – area under the curve, represents the total amount of generated thrombin; lag time – time from tissue factor addition to onset of thrombin generation; peak – maximum level of generated thrombin; time-to-peak (ttpeak) – time from tissue factor addition to peak generation.
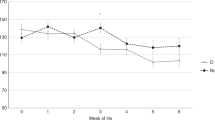
Next, we tested the impact of varying platelet counts on thrombin generation in samples from cord blood and adult blood. Table 1 shows effects of platelets on thrombin generation and parameters without rFVIIa at 100,000 and 10,000 platelets/µl (mean ± SD). While CAT parameters in cord blood derived plasma are comparable at platelet counts of 100.000/µl and 10.000/µl, the values for ETP and peak in adult plasma are significantly reduced at 10,000 platelets/µl compared to 100,000 platelets/µl. Parameters at 100,000, 75,000, 50,000, 10,000 platelets/µl and platelet poor plasma (PPP) in a subset of adult and cord blood (CB) samples are shown in Fig. 2. Values remain constant in CB samples whereas ETP and peak levels are reduced at 10,000 platelets/µl and PPP in adult samples. Taken together, thrombin generation in samples from adult blood exhibits a substantially higher platelet dependency than samples from cord blood.
Impact of decreasing platelet counts on thrombin generation parameters without rFVIIa. Course of parameters of thrombin generation – lag time (a), endogenous thrombin potential (ETP) (b), peak height (c), time-to-peak (ttpeak) (d) – in cord blood derived and adult plasma with platelets at different platelet counts (100,000/µl, 75,000/µl, 50,000/µl, 10,000/µl and PPP; n = 5).
Then, we tested the impact of rFVIIa on thrombin generation at varying platelet counts in samples from cord blood and from adult blood. The impact of rFVIIa on thrombin generation is primarily reflected in the shortening of lag time. Results of thrombin generation experiments – run with 1.5 µg/ml rFVIIa at different platelet concentrations – are outlined in Table 2 and are given as ratios ± SD to vehicle. The use of 3.0 µg/ml rFVIIa did not further increase the effects observed with 1.5 µg/ml rFVIIa (data not shown). The ratios provide comparability between CB and adult blood as absolute values differ broadly. For lag time shortening, the ratios reflect a more pronounced impact of rFVIIa in CB than in adult blood (Table 2) whereas the absolute reductions in lag time are within a similar range in CB and in adult blood (1.22–1.38 min and 0.91–1.13 min, respectively). Concerning peak heights the addition of rFVIIa leads to a reduction in CB but not in adult blood. Lower maximum amount of generated thrombin with rFVIIa might be due to lower prothrombin levels in CB leading to substrate consumption caused by accelerated initial thrombin generation rates. ETP shows no significant change, neither in the adult group nor in the CB group. These effects are comparable for all platelet concentrations. Taken together, we found a similar impact of rFVIIa in samples from cord blood and from adult blood, and no platelet-dependency in rFVIIa-action.
Finally, we evaluated potential differences in rFVIIa dose response of thrombin generation in samples from cord blood and from adult blood. Dose response of lag time shortening was analysed by performing thrombin generation experiments with different rFVIIa concentrations in PRP samples from CB and adult blood. Figure 3 shows results of experiments with PRP at 100,000 and 10,000 platelets/µl with varying rFVIIa concentrations compared to vehicle. In these tests, standard deviations are relatively high, reflecting the varying dose response of our samples. Significant differences in lag time reduction between CB and adult blood were not found. It is remarkable that even with the lowest concentration of rFVIIa (0.023 µg/ml), a measurable reaction could be observed in both groups. While ETP remains unchanged in these experiments, peak levels in CB samples abate gradually with higher rFVIIa levels (Fig. 3b). Taken together, overall dose response is comparable in samples from cord blood and adult blood, and both cohorts exhibit high sensitivity to rFVIIa even at very low concentrations.
To explain the varying dependency of thrombin generation on platelet counts in samples from cord blood and adult blood, we performed additional experiments and evaluated the impact of differing TFPI-levels in standard plasma. TFPI depleted standard plasma reconstituted to neonatal (18 ng/ml) or adult (48 ng/ml) TFPI levels show similar platelet-dependencies as plasma from CB and adult blood respectively (Fig. 4). Samples with 48 ng/ml TFPI exhibit a substantial reduction in ETP and peak while samples with 18 ng/ml TFPI show only minor changes with decreasing platelet counts. Taken together, thrombin generation in samples with lower TFPI levels is less dependent on the presence of platelets.
Impact of varying TFPI concentrations on platelet count dependency of thrombin generation. CAT measurements were done with TFPI depleted standard plasma reconstituted with recombinant TFPI (18 and 48 ng/ml). ETP (a) and peak (b) are depicted with varying counts of washed platelets added to the plasma samples (100,000/µl, 10,000/µl, PPP).
Discussion
Aim of our study was to evaluate the support of thrombin generation by neonatal platelets and the effect of factor rFVIIa simulating thrombocytopenia in-vitro. Neonatal platelets show impaired aggregation in-vitro but no apparent lack in function in-vivo since primary haemostasis seems to be functional in healthy newborns21,22,23. Specific peculiarities of neonatal platelets explain this hypoaggregability24,25,26. We wanted to study the role of platelet counts in thrombin generation in cord blood (CB) and the effects of procoagulant agent rFVIIa under these circumstances.
In our thrombin generation experiments with adult samples and no rFVIIa, low platelet counts of 10,000/µl lead to diminished endogenous thrombin potential- (ETP-) and peak-levels compared to 100,000/µl, while lag time and time-to-peak were not influenced by platelet counts (Fig. 2). In CB samples no remarkable change was observed at declining platelet numbers in any of the thrombin generation parameters.
Apparently, normal thrombin generation can be established in CB, even with low platelet counts. In our experimental setup the source of phospholipids, which are required to support thrombin generation, are endogenously derived from platelets.
There is no activation of platelets during birth and the phospholipid content in CB does not differ from adults3,7. Possibly, lower amounts of negatively charged phospholipids are required to optimally support thrombin generation in newborns due to lower plasma levels of tissue factor pathway inhibitor (TFPI) and antithrombin (AT) in the neonatal haemostatic system. Additionally, elevated microparticles in CB may contribute to the overall phospholipid content to provide sufficient support of thrombin generation27. We tested this hypothesis by mimicking neonatal and adult TFPI levels using TFPI depleted standard plasma and recombinant TFPI. Our results showed that ETP and peak are less dependent on platelet counts at lower TFPI levels hinting to a substantial role of TFPI in platelet dependency of thrombin generation. Interestingly, ETP and peak were higher with 48 ng/ml than with 18 ng/ml TFPI when ample amounts of platelet surface were available (100.000/µl). This may seem contradictory to TFPI’s inhibiting function but fits well with thrombin generation observed in plasma from CB and adult blood. Possibly, TFPI plays an additional role in the positive feedback loop of thrombin generation by thrombin itself.
Our findings differ from Gerotziafas et al., who described an elongation of lag time and time-to-peak in adult samples with low platelet counts. Presumably, these contrasts are due to unknown tissue factor concentrations and the addition of exogenous phospholipids in their study28.
Using rFVIIa, we observed a similar dose response in CB derived plasma and in adult samples. The total amount of generated thrombin (ETP) shows no significant change after adding rFVIIa, but the kinetics of reaction change. The effect of rFVIIa lies in the acceleration of the initial thrombin burst, resulting in shortened lag time and time-to-peak. The shortening of lag time after addition of rFVIIa in newborn (and preterm) platelet poor plasma has already been shown by Streif et al. with a subsampling method29. These findings are now also observed in thrombocytopenic CB derived plasma and adult plasma, respectively. We did not find significant differences of rFVIIa-effects at varying platelet counts. In our experiments, the mean percentage of shortening was 62% to 66% of negative control in CB plasma and 75% to 80% in adult plasma, not depending on platelet counts. We conclude that a reduction of platelets does not influence the rFVIIa support of thrombin generation.
Interestingly, the absolute values for lag time shortening were similar for adult and cord blood samples. This is noteworthy because – without rFVIIa – lag time in samples from CB was already shorter than in adult samples. We postulate that plasmatic coagulation factors, especially the lower levels of tissue factor pathway inhibitor (TFPI), contribute to a comparable shift despite lower absolute baseline lag time in CB samples, which resulted in a higher relative reduction than in adult samples1. Reduction of peak levels with rFVIIa was only observed in samples from cord blood. Possibly, lower TFPI levels and low amounts of prothrombin in neonates result in a higher fraction of prothrombin being converted by rFVIIa. Thus, less prothrombin might be remaining for peak thrombin generation via FVIII/FIX.
The presented results from in-vitro experiments were done with 1.5 μg/ml rFVIIa, which roughly corresponds to 90 μg/kg, the recommended dose in a clinical setting. Additionally, we tried several lower concentrations as we were interested in dose dependent effects on thrombin generation in cord plasma, taking into consideration that physiological levels of FVII are lower in newborns. Therefore, we would have expected a lower dose of rFVIIa to reach the same effect when compared to adults. Administered rFVIIa doses in neonates vary greatly within the literature. In a case series of 36 newborns, the dose of rFVIIa was mostly received with good response but varied broadly between 15 µg/kg and 200 µg/kg30. Greisen et al. describe the effect of rFVIIa-doses of 5 µg/kg and 80 µg/kg in preterm babies with prolonged prothrombin time (PT). PT was already significantly shortened at the lowest dose (5 µg/kg)31. Usually, a supraphysiological dose of rFVIIa is needed for pharmacological purposes. As shown by Shibeko et al., this need can not only be explained by a phospholipid-related pathway but also by a competition between rFVIIa and factor VII zymogen (FVII) for tissue factor binding32.
Our results do not support this assumption as we did not find a maximum lag time shortening at levels below 1.5 μg/ml, neither at 100,000 nor at 10,000 platelets/µl. Therefore, in our experiments we found no evidence for a heightened dose response in neonates and comparable saturating rFVIIa concentrations.
Limitations of such trials lie in the use of cord blood, which may not reflect a neonatal in-vivo situation ideally. It is, however, the only ethically justifiable way to achieve sufficient quantities of neonatal platelets. We presumed a platelet count of 100,000/µl to be functionally normal as usually no bleeding occurs and higher levels were not feasible in the long term. Presentation of data as ratios was done to establish comparability of study cohorts, but may marginally distort the results as small changes at lower baseline levels affect ratios more than at higher baseline levels.
In summary, we found that even at low platelet counts exhaustive rFVIIa action is observable in plasma from cord blood as well as from adult blood. The in-vitro hypoaggregability of neonatal platelets does not result in an impaired support of thrombin generation with or without rFVIIa. Nevertheless, the neonatal haemostatic system is known to be fragile. Peculiarities of neonatal haemostasis should be taken into consideration in addition to the critical health state, when rFVIIa has to be administered to babies due to the relatively high thrombosis rate in this age cohort.
Methods
This study was approved by the local ethics committee (Ethikkommission der Medizinischen Universität Graz), and all participants gave written informed consent in accordance with the Declaration of Helsinki.
Each experiment was repeated five-times with a total of ten different participants. Blood of adult volunteers (5 males, 5 females) was drawn with a 21 gauge needle from the antecubital vein, without applying venostasis, into precitrated S-Monovette premarked tubes (3 ml) from Sarstedt (Nümbrecht, Germany), containing 0.30 ml 0.106 mol/l trisodium citrate solution. Cord blood was obtained from term newborns (gestational age 38–42 weeks), immediately following delivery into the abovementioned citrate tube and processed shortly. For thrombin generation experiments, platelet-rich plasma (PRP) was obtained by centrifugation (200 × g, 10 min, 20 °C) and platelet count was measured using a Sysmex KX 21 cell counter. Platelet-poor plasma (PPP) was obtained by centrifugation (1600 × g, 10 min, 20 °C).
RFVIIa (Eptacog alpha; Novoseven©, Novo Nordisk A/S, Danmark) was reconstituted according to manufacturer’s instruction and stored in aliquots of 35 µl at −80 °C for later use. These were diluted with NaCl 0.9% to obtain the desired concentration.
Thrombin generation experiments
PRP was diluted with autologous platelet poor plasma (PPP) to produce platelet counts of 100,000, 75,000, 50,000 and 10,000/µl. Thrombin generation was performed using Calibrated Automated Thrombography according to Hemker et al. as reported previously20,27. This method allows the continuous tracing of thrombin generated in-vitro in a specific plasma sample over time. Thrombin generation assays were performed using a Fluoroskan Ascent plate reader (Thermo Labsystems, Helsinki, Finland) and Thrombinoscope© software (Thrombinoscope BV, Maastricht, the Netherlands). 20 µl of PRP-reagent (1 pM tissue factor final concentration) or calibrator (both Thrombinoscope BV, Maastricht, The Netherlands) and rFVIIa in a final concentration of 1.5 µg/ml and 3.0 µg/ml were placed into respective wells of a 96-well-plate (Immulon 2 HB, Thermo Scientific). 80 µl PRP with the respective platelet counts were added. The measurement was started by automatic dispensing of 20 µl fluobuffer-CaCl2 (20 mM Hepes, 140 mM NaCl, 5 mg/ml bovine serum albumin, and 16.7 mM CaCl2 final concentration, pH 7.35), containing a fluorogenic substrate (Z-Gly-Gly-Arg-amino-methyl-coumarin, Bachem, Bubendorf, 417 µM final concentration). Thrombin generation profiles were recorded in triplicates. Further thrombin generation experiments were performed with platelet counts of 100,000 and 10,000/µl (+platelet poor plasma, PPP) and varying concentrations of rFVIIa (1.5, 0.75, 0.38, 0.19, 0.09, 0.047, 0.023 µg/ml). The thrombin generation parameters lag time, endogenous thrombin potential (ETP), peak, time-to-peak (ttpeak) and velocity index (velix) were calculated from respective profiles. Figure 1 shows schematics of a thrombin generation trace with the corresponding parameters. The velix was calculated with the formula [peak thrombin/(peak time − lag time)].
In a follow-up experiment, TFPI-depleted plasma (Sekisui Diagnostics, Lexington, MA) was reconstituted with recombinant TFPI (18 ng/ml or 48 ng/ml, Abcam, Cambridge, UK) to mimic neonatal or adult TFPI levels. Washed platelets from an adult donor were added to a subset of these plasma samples with platelet counts of 100,000 and 10,000/µl, respectively, before CAT measurements.
Statistical analysis
Data are presented as mean ± SD or relative changes ± SD. Differences within cord blood or adult samples were analysed using ANOVA. Corrections for multiple comparisons were made using the Holm-Šídák method (α = 0.05), and multiplicity adjusted P-values were calculated for each comparison. Graphpad Prism 6.0 (Graphpad software, San Diego, CA) was used for performing calculations and creating figures. The datasets generated and/or analysed during the current study are available from the corresponding author on request.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
Cvirn, G., Gallistl, S., Leschnik, B. & Muntean, W. Low tissue factor pathway inhibitor (TFPI) together with low antithrombin allows sufficient thrombin generation in neonates. J Thromb Haemost 1, 263–268 (2003).
Israels, S. J., Rand, M. L. & Michelson, A. D. Neonatal platelet function. Semin Thromb Hemost 29, 363–372 (2003).
Grosshaupt, B., Muntean, W. & Sedlmayr, P. Hyporeactivity of neonatal platelets is not caused by preactivation during birth. Eur J Pediatr 156, 944–948 (1997).
Corby, D. G. & O’Barr, T. P. Decreased alpha-adrenergic receptors in newborn platelets: cause of abnormal response to epinephrine. Dev Pharmacol Ther 2, 215–225 (1981).
Gelman, B., Setty, B. N., Chen, D., Amin-Hanjani, S. & Stuart, M. J. Impaired mobilization of intracellular calcium in neonatal platelets. Pediatr Res 39, 692–696 (1996).
Israels, S. J., Cheang, T., Roberston, C., McMillan-Ward, E. M. & McNicol, A. Impaired signal transduction in neonatal platelets. Pediatr Res 45, 687–691 (1999).
Bernhard, H. et al. Phospholipid content, expression and support of thrombin generation of neonatal platelets. Acta Paediatr 98, 251–255 (2009).
Castle, V. et al. Frequency and mechanism of neonatal thrombocytopenia. J Pediatr 108, 749–755 (1986).
Witmer, C. M., Huang, Y. S., Lynch, K., Raffini, L. J. & Shah, S. S. Off-label recombinant factor VIIa use and thrombosis in children: a multi-center cohort study. J Pediatr 158, 820–825.e821 (2011).
Haley, K. M. Neonatal Venous Thromboembolism. Front Pediatr 5, 136 (2017).
Brady, K. M., Easley, R. B. & Tobias, J. D. Recombinant activated factor VII (rFVIIa) treatment in infants with hemorrhage. Paediatr Anaesth 16, 1042–1046 (2006).
Mitsiakos, G. et al. Is the use of rFVIIa safe and effective in bleeding neonates? A retrospective series of 8 cases. J Pediatr Hematol Oncol 29, 145–150 (2007).
Dang, C. N. et al. Recombinant activated factor VIIa treatment for refractory hemorrhage in infants. J Perinatol 31, 188–192 (2011).
Alten, J. A. et al. Pediatric off-label use of recombinant factor VIIa. Pediatrics 123, 1066–1072 (2009).
Veldman, A., Josef, J., Fischer, D. & Volk, W. R. A prospective pilot study of prophylactic treatment of preterm neonates with recombinant activated factor VII during the first 72 hours of life. Pediatr Crit Care Med 7, 34–39 (2006).
Lisman, T. & de Groot, P. G. The interaction of recombinant factor VIIa with platelet glycoprotein Ib. Thromb Res 125(Suppl 1), S13–15 (2010).
Poon, M. C. The evidence for the use of recombinant human activated factor VII in the treatment of bleeding patients with quantitative and qualitative platelet disorders. Transfus Med Rev 21, 223–236 (2007).
Fritsch, P. et al. Thrombin generation in factor VIII-depleted neonatal plasma: nearly normal because of physiologically low antithrombin and tissue factor pathway inhibitor. J Thromb Haemost 4, 1071–1077 (2006).
Cimenti, C., Koestenberger, M., Leschnik, B., Haidl, H. & Muntean, W. The respective and combined anticoagulant effects of recombinant human activated protein C, melagatran and heparins using CAT. Thromb Res 119, 361–367 (2007).
Hemker, H. C. et al. Calibrated automated thrombin generation measurement in clotting plasma. Pathophysiol Haemost Thromb 33, 4–15 (2003).
Andrew, M., Schmidt, B., Mitchell, L., Paes, B. & Ofosu, F. Thrombin generation in newborn plasma is critically dependent on the concentration of prothrombin. Thromb Haemost 63, 27–30 (1990).
Boudewijns, M. et al. Evaluation of platelet function on cord blood in 80 healthy term neonates using the Platelet Function Analyser (PFA-100); shorter in vitro bleeding times in neonates than adults. Eur J Pediatr 162, 212–213 (2003).
Israels, S. J., Cheang, T., McMillan-Ward, E. M. & Cheang, M. Evaluation of primary hemostasis in neonates with a new in vitro platelet function analyzer. J Pediatr 138, 116–119 (2001).
Schlagenhauf, A. et al. Prostaglandin E2 levels and platelet function are different in cord blood compared to adults. Thromb Haemost 113, 97–106 (2015).
Schlagenhauf, A., Schweintzger, S., Birner-Gruenberger, R., Leschnik, B. & Muntean, W. Newborn platelets: lower levels of protease-activated receptors cause hypoaggregability to thrombin. Platelets 21, 641–647 (2010).
Urban, D. et al. Decreased numbers of dense granules in fetal and neonatal platelets. Haematologica 102, e36–e38 (2017).
Schweintzger, S. et al. Microparticles in newborn cord blood: slight elevation after normal delivery. Thromb Res 128, 62–67 (2011).
Gerotziafas, G. T. et al. The role of platelets and recombinant factor VIIa on thrombin generation, platelet activation and clot formation. Thromb Haemost 91, 977–985 (2004).
Streif, W. et al. Influence of exogenous factor VIIa on thrombin generation in cord plasma of full-term and pre-term newborns. Blood Coagul Fibrinolysis 11, 349–357 (2000).
Robertson, J. D. Prevention of intraventricular haemorrhage: a role for recombinant activated factor VII? J Paediatr Child Health 42, 325–331 (2006).
Greisen, G. & Andreasen, R. B. Recombinant factor VIIa in preterm neonates with prolonged prothrombin time. Blood Coagul Fibrinolysis 14, 117–120 (2003).
Shibeko, A. M., Woodle, S. A., Lee, T. K. & Ovanesov, M. V. Unifying the mechanism of recombinant FVIIa action: dose dependence is regulated differently by tissue factor and phospholipids. Blood 120, 891–899 (2012).
Author information
Authors and Affiliations
Contributions
H.H., S.G., W.M. and conceived the study, H.H., B.L. and A.S. did experimental work, H.H. wrote the main manuscript text, S.P. revised the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Haidl, H., Pohl, S., Leschnik, B. et al. Neonatal thrombocytopenia: Thrombin generation in presence of reduced platelet counts and effects of rFVIIa in cord blood. Sci Rep 9, 8014 (2019). https://doi.org/10.1038/s41598-019-44199-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-44199-y
This article is cited by
-
The role of the calibrated automated thrombogram in neonates: describing mechanisms of neonatal haemostasis and evaluating haemostatic drugs
European Journal of Pediatrics (2022)
-
New insights into neonatal coagulation: normal clot formation despite lower intra-clot thrombin levels
Pediatric Research (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.