Abstract
Background
The correlation between procoagulant levels—factor VIII (FVIII), von Willebrand factor (vWF), and fibrinogen—and risk of thrombosis has been well documented in adult populations. We hypothesize that interaction of passively transferred isoagglutinins in premature neonates with a compromised immune system may trigger an immune response that can target the immature gastrointestinal tract. The objective of this study is to evaluate if there are procoagulant level differences in preterm newborns stratified by ABO blood group.
Methods
VWF, FVIII, and fibrinogen levels were analyzed in neonates ≤32 weeks and/or birthweight ≤1500 g over the first 6 weeks of life. Demographic, blood type, and transfusion data were collected.
Results
Elevations in vWF and FVIII were found to be statistically significant in the third week of life in non-O neonates vs. type O neonates. FVIII was also found to be significantly elevated in week 1. Transfused neonates also showed elevations between weeks 0 and 3.
Conclusion
There appears to be a time-dependent variation in procoagulant factor levels in preterm newborns. Although the clinical significance remains unclear, prothrombotic factors vWF and FVIII are significantly higher in non-O blood-type preterm neonates in the third week of life.
Similar content being viewed by others
Introduction
ABO blood groups were first recognized by Landsteiner in 1900, but the biologic significance and function(s) of these carbohydrates and red blood cell (RBC) structures remain unclear. Non-O (A, B, and AB) blood groups differ from O blood group secondary to the expression of glycosyltransferase activity that converts the precursor H to either A or B carbohydrate phenotype. These carbohydrate structures are expressed not only on RBCs but also throughout the body, such as on epithelium, sensory neurons, platelets, and vascular endothelium.1
Differential expression of ABH antigens has been associated with clinical disease in adults. For example, A antigen expression with Pseudomonas infections, B with Salmonella typhi, and O with Helicobacter pylori. Group A antigen expression has also been associated with increased risk of several types of cancer—rectal, cervical, gastric, breast, and ovarian,2 group B blood type with diabetes, and all non-O blood types with pancreatic cancer.3 Furthermore, non-O blood-type adults have been shown to have a significantly increased risk for peripheral vascular, venous thromboembolic, and ischemic heart disease.2,4,5,6 Increased levels of plasma coagulation proteins, von Willebrand factor (vWF), and factor VIII (FVIII) may contribute to increased risk for these conditions over a lifetime.
Individually, vWF and FVIII levels vary between blood groups in adults. Both plasma FVIII and vWF levels tend to be lower in individuals with type O blood groups compared to type A or B.7,8,9 Souto et al.7 found no difference between the non-O groups for FVIII, but a trend towards higher levels in those with AB blood group and lowest levels in those with type O. In a study of 1100 normal adults, Gill et al.10 showed statistically significant differences in vWF Ag levels among those with non-O groups (AB highest, then B, then A). Shima et al.11 and Souto et al.7 both showed lowest vWF levels in those carrying an O allele (AO, BO) compared to those without an O allele (AA, BB, AB). The glycotransferases inherited by non-group O individuals post-translationally derivatize vWF molecules, making them less susceptible to cleavage by ADAMTS13 metalloproteinase, affecting vWF removal from circulation. The lower plasma levels of vWF, characteristic of O blood group individuals, are due to a shorter vWF survival, mainly attributable to faster clearance and its shorter half-life.12 It is not known if these differences are also true in the preterm population.
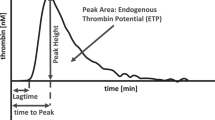
Procoagulant factors vWF and FVIII circulate in a noncovalent complex; vWF mediates the interaction between platelets and damaged blood vessel walls and acts as a carrier molecule for FVIII. The wide range in vWF–FVIII complex levels in the normal “reference laboratory” population (50–150 IU/dL) has a skewed distribution toward higher levels.13 Plasma FVIII–vWF complex levels are 25% higher in non-O blood group adults than O blood group adults.10 Environmental factors can also influence vWF–FVIII levels: increasing age, gender (female > male), acute-phase response to malignancy, infection, or inflammation can all significantly increase levels.13 RBC transfusion is one of the most common procedures performed in the neonatal intensive care unit (NICU) and up to 80% of all infants <1.5 kg at birth will be transfused at least once during their NICU stay;14 ABO histo-blood groups and transfused cells could have a potentially significant interaction.
Very few studies have reported on normal values or differences in procoagulant factor levels in newborns, especially in the preterm population. Andrew et al.15 reported reference values for many coagulation factors (including vWF, FVIII, and fibrinogen) in a consecutive cohort of 118 healthy full-term and 137 “healthy” premature infants in the first 6 months of life. True reference ranges for neonates under 30 weeks of age were not available as these infants were not considered “normal” secondary to postnatal complications and there was no stratification based on blood type. In that same study, it is notable that values from fetuses at 19–27 weeks gestation were approximately less than half the mean value of all three factors compared to “healthy” neonates born at 28–31 weeks. The correlation between FVIII and vWF factor and the risk for thrombotic events, as well as their inverse correlation with bleeding diathesis, has been well documented in adult populations.16,17 As there are many different factors that may contribute to a prothrombotic state, the aim of this study was to determine if levels of vWF, fibrinogen, and FVIII in the first 6 weeks of life differ between ABO blood groups in preterm newborns.
Methods
Subjects
Loyola University Medical Center is a perinatal referral center with a 50-bed level III NICU that admits both inborn and outborn neonates. After Institutional Review Board’s approval, neonates born at ≤32 weeks and/or ≤1500 g at birth were prospectively enrolled from November 2014 through November 2017 within the first 72 h of life. Exclusion criteria included the presence of severe congenital anomalies, transfusion of cryoprecipitate or fresh frozen plasma (FFP) before obtaining the initial study sample, exchange transfusion, and outborn infants with transfer to Loyola beyond 72 h of life.
Measurements and protocol
A 0.5 mL blood sample was obtained within 72 h of life and then once weekly for the next 6 weeks. The time interval of once weekly lab draws was chosen to coincide with the patient’s regular lab schedule in an attempt to avoid excess blood draws and central line access for research labs alone. If the neonate developed necrotizing enterocolitis (NEC), a sample was drawn at the time of diagnosis and then repeated 24 h later, after which point no more blood samples were drawn. Whole blood samples were placed in tubes containing 3.2% buffered sodium citrate (0.109 M) at a ratio of nine parts blood to one part citrate. Citrated whole blood samples were centrifuged at 1100 × g for 10 min. The supernatant platelet-poor plasma was harvested and stored in aliquots at −70 °C until analysis.
Samples were thawed and batch analyzed for levels of vWF, fibrinogen, and FVIII. VWF and fibrinogen levels were measured using the ZYMUTEST vWF assay and ZYMUTEST fibrinogen assay (Aniara, West Chester, OH, USA). Levels of coagulation of FVIII were measured using the VisuLize FVIII Antigen Kit (Affinity Biologicals, Ancaster, ON, Canada). All assays were run according to manufacturer’s instructions and plasma samples were diluted according to the manufacturer’s recommendations so that expected levels in human plasma would fall in the middle of the calibration curves. Optical densities were measured using an ELx405 plate reader (BioTek, Winooski, VT, USA). Enzyme-linked immunosorbent assays (ELISAs) were chosen to measure the various coagulation markers primarily to minimize the amount of plasma required to run these assays. These assays are designated as research use only by the manufacturers and are not meant for clinical diagnoses. We are not aware of age-specific normal ranges for these particular assays.
Data analysis
Individual charts were reviewed to determine maternal blood group, the neonate’s blood group, gestational age, birthweight, date of birth, transfusion history (type and date), date of death or discharge from the unit, and diagnosis of NEC or spontaneous intestinal perforation (SIP). The mean values of each procoagulant factor were compared statistically using the Mann–Whitney U test. The χ2 or Fisher’s exact test highlighted categorical differences. A p value of <0.05 was considered statistically significant.
The Mann–Whitney U test was chosen since comparing the mean values each week between group O and non-O neonates requires a non-parametric statistical test to neutralize the assumption that the data are parametrically distributed. Each weekly mean value is independent of every other weekly mean value, and a lower number of samples were available in later weeks as patients were discharged or fewer labs were drawn. Therefore, tests of correlation or regression across weeks would not only be inappropriate but also risk overfitting the data. Time-based analyses (e.g., Kaplan–Meier, Cox model) did not apply, as the outcome of a dependent variable based on our weekly mean values was not our focus in this study.
Results
There were 149 neonates enrolled in the study with available data during the 3-year study period, out of a possible 352 that met the inclusion criteria. There were no statistically significant differences between group O and non-O (group A, B, and AB) neonates in terms of gender, race/ethnicity, gestational age, and birthweight (Table 1). Blood group distribution among our study cohort was similar to the general population, but with a slightly higher percentage of group B and lower percentage of group A (41% group O, 32% group A, 21% group B, 5% group AB) compared with the national averages of 45% group O, 40% group A, 11% group B, and 4% group AB.18 The incidence of NEC in our study population was 5% (8 total: 3 blood type B, 1 type A, 4 type O) and SIP was 2% (3 total: all type O).
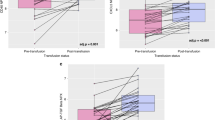
The relationship between ABO blood group phenotype and plasma vWF, FVIII, and fibrinogen levels are depicted in Figs. 1, 2, and 3, respectively. There were statistically significant elevations in week 3 for both vWF and FVIII in the non-O group compared to O: vWF (140 ± 49% vs. 116 ± 35% group O; p = 0.008) and FVIII (128.7 ± 45 IU/dL vs. 110.3 ± 44 IU/dL; p = 0.012). Overall, average vWF levels tended to be lower in type O, but not significantly until week 3. This elevation trend continued through week 6 of life, although no other time in the study period showed statistically significant elevations (Fig. 1). Neonates with non-O blood groups appeared to have slightly higher average values of FVIII over the first 4 weeks of life. There were also significant elevations in FVIII for group non-O compared group O blood types at week 1 (143.2 ± 58 IU/dL vs. 128.6 ± 48 IU/dL; p = 0.043. Figure 2). There were no significant differences between groups for fibrinogen levels during the study period (Fig. 3).
Of the 149 patients with transfusion information available, 4 were excluded because they received FFP. Comparing neonates who received any transfusion with those who were not transfused in the first 6 weeks of life, there was no significant difference in gender or race/ethnicity, although 62% in the study cohort were male. When sorted by blood group, the percentage of neonates who received any transfusion was similar between groups (38% type O, 42% non-O), and the average number of transfusions over the study period was the same (Table 1).
As expected, those who received transfusions were more likely to be lower in birthweight and of lower gestational age. During the study period, 45% or 67/149 required at least one RBC transfusion, and 50 of those 67 (74%) required multiple transfusions. Excluding neonates who received plasma, 59 of 145 (41%) received RBC transfusions, of whom 44 (30%) were transfused at <3 weeks. There were no statistically significant differences in the number of neonates transfused between group O and non-group O cohorts (Table 1; p = 0.348). vWF levels in weeks 0, 1, and 3 were significantly elevated (p = 0.03, p = 0.0004, and p = 0.008, respectively; Fig. 4) and FVIII levels in weeks 0 and 2 (p = 0.03 and p = 0.01; Fig. 5) when comparing those who received transfusion and those who did not. At all weeks of the study, there were no statistically significant differences in fibrinogen levels between the transfused and non-transfused neonates.
Discussion
There have been several studies comparing newborn procoagulant levels to children and adults over time. Andrew et al.19 reported relatively stable mean values of vWF (0.82 U/mL), fibrinogen (2.76 g/L), and FVIII (0.90 U/mL) for children aged 1–5 years who did not differ significantly over time in comparison to adults. Fukui et al.20 measured FVIII activity and vWF in 100 newborn cord plasmas and found the mean level of FVIII procoagulant activity to be “normal,” but vWF activity was slightly lower than normal.20
Very few studies, however, have reported on normal values or differences in procoagulant factor levels in neonates, especially in the preterm population. True reference ranges for premature neonates under 30 weeks gestation is lacking, especially given that it is unclear what effect extreme prematurity and its resultant complications may have on these factors. Andrew et al.15 did report normal values in a cohort of “healthy” 30–36 week gestation preterm neonates. Our study’s mean values are consistent with those reported in the literature and well within the reported ranges in the Andrew et al. study. Our samples were stratified by week of life drawn, so a direct comparison to 1, 5, 30, and 90 day of life was difficult but could be estimated (~week 0, week 1, week 4, week 6). Mean fibrinogen levels appear to peak slightly later in our study (~week 4 vs. at day 5 in the Andrew et al. study), but both appear to downtrend when measured at 6 weeks and 90 days, respectively. Overall mean levels of VIII were higher in our study in week 1 to 2, but remained within the reported ranges in the Andrew study and trended down over 6 weeks and 90 days, respectively. The study values for vWF followed the Andrew data very closely.15
When comparing to adult values, Andrew et al.15 noted that mean values for vitamin K-dependent and contact factors were <70% of adult values, but factors such as fibrinogen, FVI, VIII, and vWF were >70% of adult values. Clinically, however, these infants do not show excessive bleeding with procedures or spontaneous bleeding, perhaps indicating that minor alterations may rapidly place the infant at risk for hemorrhagic or thromboembolic complications. Additionally, the role of estrogen in the early neonatal period on these factors remains unknown. Statistical differences in mean values between premature and full-term infants are smaller when compared to infant to adult; however, both preterm and full-term infants mature toward the adult system during the perinatal period and are similar to adults by 6 months.15
While we did not use a standardized scoring system for degree of illness in our population, we acknowledge that preterm neonates are at higher risk for comorbid illnesses that may affect their procoagulant levels. This may be helpful to distinguish differences in levels between “healthy” and “less healthy” neonates in future research. Maak et al.21 measured FVIII activity and FVIII-related antigen in 20 full-term and preterm newborns in the first days of life and found that FVIII activity did not differ from adult controls, but the concentration of FVIII-related antigen was markedly higher at birth and then decreased toward adult levels in the first days of life. In sick term and preterm newborns with severe pulmonary or intracranial hemorrhage, FVIII antigen level was found to be highest in non-survivors (129.1% ± 8.1) and lowest in term infants between 48 and 72 h of life, making it a potential biomarker for endothelial cell damage in the perinatal period.22 Of note, the mean levels of all three procoagulant factors in our study were similar to and well within the ranges as reported by Andrew et al.15 for “healthy” 30–36 week infants. We chose to examine fibrinogen levels for several reasons: “reference” levels of fibrinogen in premature neonates are either unknown or not well established, so expected variations as a function of BW, GA, or ABO blood group are unspecified. Additionally, fibrinogen is the key final step in the classical coagulation cascade, so demonstrating adequate levels in premature infants provides important support for understanding its role, if any, in neonatal disease. Lastly, fibrinogen is a “positive” acute-phase reactant in response to systemic inflammation and tissue injury. Whether or not such responsiveness occurs in injurious conditions affecting premature neonates is unknown. Unfortunately, no difference was seen in fibrinogen levels in our study, so there may be not be a role for tracking fibrinogen levels in neonatal disease.
In our study, the average vWF level in type O and non-O neonates was similar in the first 2 weeks of life, with a statistically significant elevation in non-O neonates at week 3 (140.4 ± 48.8 IU/dL). While the difference in vWF level in type O and type non-O neonates was not statistically significant in weeks 4–6, the trend towards lower levels in O blood groups matches what is reported in the adult literature. In a review of ABO blood group phenotype and plasma vWF and FVIII levels, O’Donnell et al.13 described multiple studies that confirmed statistically significant elevations in group non-O vs. group O FVIII and vWF levels in adults, with the highest values being group AB and the lowest group O. In six studies evaluating a total of more than 2000 patients, vWF levels for group O individuals ranged from 65.4 to 99.7 IU/dL, with increasing levels in those with A, B, and AB blood groups, and with the highest levels in the AB blood group (113.8–139.0 IU/dL).13
Comparing FVIII levels in our study to the adult published values as stratified by blood group, we found a similar trend of values in the higher range of the reported “normal reference” range of 50–150 IU/dL, with a general downward trend from birth to the sixth week of life. Non-O FVIII values in the adult literature ranged from 110 to 163, 91 to 150, and 107 to 219 IU/dL for blood groups A, B, and AB, respectively.13 While the average FVIII levels in our study were not above the upper “normal” range of 150 IU/dL, there was an overall trend of higher values in non-O neonates compared to group O neonates, especially in the first 3 weeks of life. There is a wide variation in values in weeks 4–6 in our study, likely partially due to a lower number of available samples as patients were discharged or fewer samples were drawn. Overall, it appears that these premature infants have higher levels of vWF and FVIII at birth, which trend down toward adult levels after the first 6 weeks of life.
The timing of statistically significant increases in both FVIII and vWF at ≤3 weeks in transfused neonates are notable because they are seen in neonates who received only a small number of transfusions. Since quantification of FVIII and vWF levels in transfused supernatant RBCs was not performed, it is unknown what portion of these increases might be due to the residual plasma in the transfused RBCs. Increases due to “passive transfusion” are actually less likely as all transfusions in our NICU were from the group O “donor pool”—those with the lowest average levels of FVIII and vWF. Other possible etiologic factors include the clinical state of the individual neonates who required transfusion (acute-phase reactions in a conceivably pro-inflammatory milieu) or to unknown immunomodulatory effects (not yet described in premature neonates) of the transfusion itself.23 It is possible that the downward trend toward adult levels in the later half of the 6 weeks seen in these procoagulant factor values may represent a physiologic nadir given its time association with anemia of prematurity. None of our patients received Epogen, as it is not the standard in our unit. However, exogenous Epogen could potentially affect procoagulant factor levels for several weeks.
In an effort to minimize antibody exposure in our vulnerable population, dedicated aliquots of group O, Rh-negative blood are transfused regardless of the neonates’ blood type. Group O RBCs contain anti-A, anti-B, and anti-A,B isoagglutinins, which may induce hemolysis in a small proportion of native RBC’s. Subsequent release of a small amount of hemoglobinemia and hemoglobinuria leads to nitric oxide scavenging, but its contribution to clinically significant vasoconstriction, ischemia, thrombosis, and renal tubular injury remains to be seen.24 A comparison of outcomes between group O to non-O premature neonates receiving at least one group O RBC transfusion did not find significant differences between groups with regard to survival, length of stay, and common neonatal morbidities (NEC, sepsis, pneumonia, intraventricular hemorrhage, retinopathy of prematurity).25
Several newborn studies have detected a temporal relationship between RBC transfusion and the onset of NEC, as well as a relationship between NEC severity and ABO histo-blood groups.26,27 The elevated levels of vWF and FVIII in the first few weeks of our study could be due, in part, to higher acuity of illness in the first few weeks, higher likelihood of requiring a transfusion, and baseline elevation in premature neonates compared to term. The low incidence of NEC and SIP in our study prevented more in-depth discussion on the effect of these procoagulant levels. While NEC and SIP are often discussed together, they are distinct clinical entities and have different pathophysiology. SIP tends to have an earlier presentation (within the first week of life) and a more focal inflammatory effect in comparison to NEC. All three cases of SIP in our study were O blood types. As type O makes up 40–45% of the general population, only three cases seems too low a number to draw conclusions. However if this trend were to persist in future studies, it may be an interesting distinction given the increased morbidity our previous study found in AB blood-type NEC cases.28 NEC has been associated with a hypercoagulable state. Histopathologically, NEC is associated with a coagulative necrosis with peak onset between 2 and 5 weeks of life. In a previous study examining 24 years of data from our institution’s NICU, neonates were at significantly decreased survival when they develop NEC if the neonate was blood group AB and especially if the mother was group A or AB.28 While NEC is a multifactorial disease, the passive transfer of isoagglutinins from mother to neonate or from transfusions may play a role in triggering an antigen–antibody connection that targets the immature gut. Unlike adults who express blood group determinants only in the proximal colon, fetal intestines express blood group determinants in all parts of the small and large intestine.29 Our previous study found that blood group antigens (A more than B or AB) may increase the risk for humoral immune-mediated inflammatory response as a mechanism of injury in NEC in the presence of passively or actively transferred isoagglutinins.28 Supporting this link, we additionally demonstrated the immunohistochemical expression of A and B antigens on the submucosal endothelium in surgical specimens from neonates with fulminant NEC.30 Of note, type-specific transfusion may be difficult due to maternal isohemagglutinins.25,31 However, given the finding that maternal and neonatal blood groups may correlate to increased mortality from NEC along with the elevated levels of procoagulant factors in non-O neonates, transfusing-type specific blood components to these patients is worthy of further study.
It remains to be seen if these elevations in FVIII and vWF levels in preterm neonates are of clinical significance. While the similar timing of conditions such as NEC and significant elevations of non-O procoagulant levels compared to group O neonates is interesting, these early data merit further investigation. Additionally, the role of maternal passively transferred isoagglutinins and effect of transfusion on these procoagulant levels is unknown, especially in the preterm population. Further studies are warranted to determine if procoagulant factor levels can be used as biomarkers for clinical disease, and what effect transfusion of O-type blood may have on non-O-type neonates over time.
References
Eastlund, T. The histo-blood group ABO system and tissue transplantation. Transfusion 38, 975–88 (1998).
Greenwell, P. Blood group antigens: molecules seeking a function? Glycoconj. J. 14, 159–73 (1997).
Egawa, N. et al. ABO blood type, long-standing diabetes, and the risk of pancreatic cancer. World J. Gastroenterol. 19, 2537–42 (2013).
Medalie, J. H. et al. Blood groups, myocardial infarction and angina pectoris among 10,000 adult males. N. Engl. J. Med. 285, 1348–53 (1971).
Conlan, M. G. et al. Associations of factor VIII and von Willebrand factor with age, race, sex, and risk factors for atherosclerosis. The Atherosclerosis Risk in Communities (ARIC) Study. Thromb. Haemost. 70, 380–5 (1993).
Meade, T. W. et al. Factor VIII, ABO blood group and the incidence of ischaemic heart disease. Br. J. Haematol. 88, 601–7 (1994).
Souto, J. C. et al. Functional effects of the ABO locus polymorphism on plasma levels of von Willebrand factor, factor VIII, and activated partial thromboplastin time. Arterioscler. Thromb. Vasc. Biol. 20, 2024–8 (2000).
McCallum, C. J., Peake, I. R., Newcombe, R. G. & Bloom, A. L. Factor VIII levels and blood group antigens. Thromb. Haemost. 50, 757 (1983).
Mohanty, D. et al. Major blood group antigens—a determinant of factor VIII levels in blood? Thromb. Haemost. 51, 414 (1984).
Gill, J. C., Endres-Brooks, J., Bauer, P. J., Marks, W. J. Jr & Montgomery, R. R. The effect of ABO blood group on the diagnosis of von Willebrand disease. Blood 69, 1691–5 (1987).
Shima, M. et al. ABO blood group genotype and plasma von Willebrand factor in normal individuals. Vox Sang. 68, 236–40 (1995).
Gallinaro, L. et al. A shorter von Willebrand factor survival in O blood group subjects explains how ABO determinants influence plasma von Willebrand factor. Blood 111, 3540–5 (2008).
O'Donnell, J., Mille-Baker, B. & Laffan, M. Human umbilical vein endothelial cells differ from other endothelial cells in failing to express ABO blood group antigens. J. Vasc. Res. 37, 540–7 (2000).
Strauss, R. G. Anaemia of prematurity: pathophysiology and treatment. Blood Rev. 24, 221–5 (2010).
Andrew, M., Paes, B. & Johnston, M. Development of the hemostatic system in the neonate and young infant. Am. J. Pediatr. Hematol. Oncol. 12, 95–104 (1990).
Tsai, H. M. & Lian, E. C. Antibodies to von Willebrand factor-cleaving protease in acute thrombotic thrombocytopenic purpura. N. Engl. J. Med. 339, 1585–94 (1998).
Furlan, M. & Lammle, B. Aetiology and pathogenesis of thrombotic thrombocytopenic purpura and haemolytic uraemic syndrome: the role of von Willebrand factor-cleaving protease. Best. Pract. Res. Clin. Haematol. 14, 437–54 (2001).
Anonymous. Blood types and population 2018. https://www.redcrossblood.org/donate-blood/how-to-donate/types-of-blood-donations/blood-types.html.
Andrew, M. et al. Maturation of the hemostatic system during childhood. Blood 80, 1998–2005 (1992).
Fukui, H. et al. Factor VIII procoagulant activity, factor VIII related antigen and von Willebrand factor in newborn cord blood. Br. J. Haematol. 42, 637–46 (1979).
Maak, B., Scheidt, B. & Frenzel, J. Factor VIII activity and factor VIII related antigen in newborns. Eur. J. Pediatr. 128, 283–9 (1978).
Balla, G. & Karmazsin, L. Factor VIII related antigen in term and preterm newborns with severe neonatal haemorrhage. Acta Paediatr. Hung. 26, 11–5 (1985).
Youssef, L. A. & Spitalnik, S. L. Transfusion-related immunomodulation: a reappraisal. Curr. Opin. Hematol. 24, 551–7 (2017).
Donadee, C. et al. Nitric oxide scavenging by red blood cell microparticles and cell-free hemoglobin as a mechanism for the red cell storage lesion. Circulation 124, 465–76 (2011).
Boral, L. I. et al. Comparison of outcomes of group O vs non-group O premature neonates receiving group O RBC transfusions. Am. J. Clin. Pathol. 140, 780–6 (2013).
Cunningham, K. E., Okolo, F. C., Baker, R., Mollen, K. P. & Good, M. Red blood cell transfusion in premature infants leads to worse necrotizing enterocolitis outcomes. J. Surg. Res. 213, 158–65 (2017).
Dani, C. et al. Red blood cell transfusions can induce proinflammatorycytokines in preterm infants. Transfusion 57, 1304–10 (2017).
Thomson, T. et al. Decreased survival in necrotizing enterocolitis is significantly associated with neonatal and maternal blood group: the AB isoagglutinin hypothesis. J. Perinatol. 12, 630q (2012).
Robbe-Masselot, C., Maes, E., Rousset, M., Michalski, J. C. & Capon, C. Glycosylation of human fetal mucins: a similar repertoire of O-glycans along the intestinal tract. Glycoconj. J. 26, 397–413 (2009).
Manuat C. L. et al. Immunohistochemical demonstration of blood group antigen expression in intestinal endothelium links blood type and necrotizing enterocolitis. J. Neonatal Biol. 5, 1–5 (2016).
Shaikh, S. & Sloan, S. R. Clearance of maternal isohemagglutinins from infant circulation (CME). Transfusion 51, 938–42 (2011).
Acknowledgements
We would like to acknowledge the generous support of the Sykora family—the main contributor to the Neonatal Research fund in our NICU. Additionally, the authors would like to acknowledge Paula Maia at Loyola University Chicago for her diligent work in performing the ELISAs.
Author information
Authors and Affiliations
Contributions
A.L.: Manuscript author, revisions, patient recruitment, data collection, and analysis. W.J.: Director of the lab where samples were processed. O.H.: Statistical analysis and manuscript editing. S.M. and S.L.: data gathering and recruitment. P.J.D.C. and L.A.G.: data analysis and manuscript revision. J.K.M.: principal investigator.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lai, A., Jeske, W., Habeeb, O. et al. ABO blood group and procoagulant factors: the hypercoagulation hypothesis ABO and Procoagulant Factors. Pediatr Res 86, 316–322 (2019). https://doi.org/10.1038/s41390-019-0445-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0445-1