Abstract
Objectives:
Pathophysiological mechanisms underlying spinal cord injury (SCI) partially involve edema and formation of a hematoma. Myelotomy seems to be a promising intervention. However, the appropriate timing of myelotomy is still unknown in SCI. Here we aimed to determine the timing of microsurgical myelotomy in an animal model of SCI.
Methods:
The SCI model was contusion-induced with a new york university impactor. Sixty-five adult female rats were randomly divided into the following groups: laminectomy alone (the ‘sham group’, SG), laminectomy plus contusion (the ‘contusion group’, CG) or laminectomy plus contusion followed by myelotomy at 8, 24 or 48 h (8 h-MTG [myelotomy-treated group], 24 h-MTG or 48 h-MTG). Functional recovery was evaluated via the open field test and the inclined plane test every week after SCI. The percentage of spared white matter area (SWMA) and ultrastructure characteristics of the injured dorsolateral spinal cord were determined on the 42nd day after SCI.
Results:
Compared with the CG, myelotomy at 8 h-MTG or 24 h-MTG greatly improved the BASSO-BEATTIE- BRESNAHAN scores (P<0.008), whereas the 48 h-MTG showed less efficacy (P=0.023). All myelotomy groups showed higher mean angle values in an inclined plane test (P<0.005) and had greater percentages of SWMA than the CG. Rats in the 24 h-MTG showed a higher intra-axonal fraction and myelin fraction than those in 48 h-MTG (P<0.005).
Conclusion:
Myelotomy up to 48 h after SCI improves recovery in rats. The potential time window of myelotomy may be between 8 and 24 h after SCI.
Similar content being viewed by others
Introduction
Traumatic spinal cord injury (SCI) is a catastrophic event for individuals, family and society. Its pathophysiology involves primary and secondary mechanisms of injury. Primary injury is usually mechanical impact, and transient or persistent compression. Secondary mechanisms involve a cascade of vascular, cellular and biochemical events, such as hemorrhage, edema, ischemia, cell death and oxidative stress.1 The development of intramedullary hemorrhage exacerbates necrosis, causes swelling in the spinal cord, and higher intramedullary pressure under constraint from the meninges. The hemorrhagic necrosis and fluid accumulation at the lesion site also aggravate secondary injury.
Decompression surgery is considered as an important therapeutic measure for traumatic SCI and includes spinal surgery, durotomy, pial incision and myelotomy.2, 3, 4, 5, 6, 7, 8, 9 Spinal decompression surgery has been widely used in the clinic; however, it cannot remove the constraint from the dura mater and especially the pia mater. Although durotomy or pial incision can release the constraint from the meninges, the hemorrhagic and necrotic tissues cannot be evacuated. Myelotomy has not been widely used for SCI due to its potential risk of further injury of the spinal cord. However, myelotomy not only removes the constraint, hemorrhagic and necrotic tissues to relieve the intramedullary pressure, but also reduces deleterious effects from hematoma and accumulated fluid within the damage tissue.
A century ago, Allen9 firstly reported the efficacy of myelotomy for SCI. Myelotomy has since been examined in many pre-clinical and clinical studies.5, 6, 8, 10, 11 Previous studies have shown that myelotomy significantly improves functional recovery when compared with opening of the meninges after SCI.7, 12 However, questions are raised regarding application of myelotomy for SCI, such as suitable operation timing. From the perspective of the reduction of intramedullary pressure, myelotomy should be performed as soon as possible after SCI; from the perspective of the debridement of aseptic necrosis, myelotomy should be performed with a fully liquefied lesion and a clear anatomical delimitation in order to get an adequate drainage, and to minimize the risk of potential surgical damage. The unknown timing of myelotomy limits its clinical application.
Operation time is one of the most important factors affecting the efficacy of surgery. Recent studies have demonstrated that bony decompression prior to 24 h after SCI made greater improvement than late surgery.2, 3, 4, 13 Only a few studies have been performed to examine the timing of myelotomy. Kalderon et al.6 compared the efficacy of partial myelotomy at 1, 2, 4 and 24 h after SCI in rat by observing the damaged area, and their results suggested the outcome within 1–4 h was a slightly better than that at 24 h after SCI. Moreover, a study by Zhu et al.5 of 30 patients (American Spinal Injury Association Impairment Scale, AIS A) showed that myelotomy performed between 4–14 days after SCI followed by intensive rehabilitation resulted in impressive improvement in many patients. Up to now, the optimal timing of myelotomy in the management of SCI is still unknown. Here, we aimed to determine optimal timing of myelotomy using a rat model of spinal cord contusion by observing behavioral and histological changes at different time points.
Materials and methods
Animals
Sixty-five Sprague–Dawley female rats (11 weeks old prior to surgery) were randomly divided into five groups (N=13 each): SG, CG, 8 h-MTG, 24 h-MTG or 48 h-MTG. Six rats died more than 5 h after the contusion procedure (two in the CG, one in the 8 h-MTG, one in the 24 h-MTG and two in the 48 h-MTG), fifty-nine rats were used for the final data analysis. All rats were housed in the same environment with free access to chow and water, at a constant temperature of 20–28 °C. The bladders were emptied manually every 8 h until recovery of reflex bladder emptying or until the mice were killed. The experimental protocol was approved by the Institutional Animal Care and Use Committee of Capital Medical University (approval number 2011-D-007).
A rat model of spinal cord injury
Adult rats were anesthetized with chloral hydrate (400 mg kg−1) by an intraperitoneal (I.P.) injection, and a laminectomy was performed at the T9–T10 level to expose the spinal cord without disrupting the dura mater. The spinous processes of T8 and T11 were clamped to stabilize the spine, and the exposed cord was subjected to contusion (10 g rod, 25 mm height) using a New York University (NYU) weight-drop device. Surgery was aseptic and performed under a Carl Zeiss operating microscope (73446, Oberkochen, Germany).
Microsurgical myelotomy
Rats were re-anesthetized at 8, 24 or 48 h after SCI. Microsurgical myelotomy was performed under a Zeiss operating microscope. The incision was disinfected and the stitches were removed. The spinal cord tissue with dark purple appearance was exposed. A 1-ml disposable syringe needle (27 G) was used to puncture a small hole in the dorsal dura mater, slightly away from the midline. The dura mater was cut with a microscissor (Micro Scissors Straight 22.5 cm, Daddy D Pro Surgical Company, USA), then the arachnoid was exposed. A 3.5-mm-long incision was made by a blunt microprobe (its tip size is 0.2 mm in diameter, modified from KRAYENBUHL NERVE HOOK, WI-GS-3382, Wrangler Instruments, Pakistan) so as to penetrate the spinal cord longitudinally into the posterolateral region and approximately half way through the spinal cord (1.0–1.5 mm depth). The incision in the spinal cord was then washed gently by warm saline (37 °C, 1 ml at a time) twice, necrotic cord and dark bloody clot were usually washed out, a piece of gelfoam was then placed on the surface of the dura mater, and finally the muscles and skin layers were sutured. We found that survival rates for 8 h-MTG, 24 h-MTG, 48 h-MTG and CG were 92.3% (12/13), 92.3% (12/13), 84.6% (11/13) and 84.6% (11/13), respectively. The survival rates did not differ significantly among groups (P>0.05).
Evaluation of motor function
Locomotor function was evaluated according to the open field test (Basso-Beattie- Bresnahan, BBB) and the inclined plane test. The open field test was carried out once a week until the end of the experiments (score 21: normal; Score 0: no hindlimb movement). The scores were averaged for each group at each time point.
The inclined plane test was used to evaluate the maximum angle on the inclined plane on which each animal maintained a stable position for at least 5 s. Each rat had three trials. Results from each rat were averaged for each group.
All behavioral tests were blinded and observed by two independent observers. Both observers averaged their data.
Tissue preparation and Luxol fast blue staining
Rats were anesthetized with an overdose of chloral hydrate, and transcardially perfused with normal saline, followed by a solution containing 4% paraformaldehyde in 0.1 M sodium phosphate buffer, pH 7.4. The spinal cords (15 mm in length) containing the injury site were collected and postfixed in the same fixative overnight at 4 °C. The spinal cords were subdivided into the injury center, rostral and caudal segments, and then embedded in paraffin. Sections (4 μm) were cut at the injury epicenter, 5 mm rostral to the epicenter and 5 mm caudal to the epicenter.
Luxol fast blue staining was used for the staining of myelin. The sections were treated with 0.1% Luxol fast blue solution (Sigma Chemical, St Louis, MO, USA) with 95% ethanol at 60 °C overnight, then with 0.01% Li2CO3 for color separation. Stained sections were viewed under an Olympus microscope (BH-2, Melville, NY, USA) at × 40 magnification. Images were captured with a Magna Fire SP CCD camera (Optronics, Goleta, CA, USA) using Magna Fire SP 2.1 software (Optronics). For quantitative analysis, a second section per site was chosen from six rats per group; thus, a total of six sections in every site for each group was used for calculation. An ‘irregular’ tool and ‘measure’ tool in Image-Pro Plus (IPP) 6.0 software (Media Cybernetics Inc., Silver spring, MD, USA) were used to calculate the SWMA and total cross-sectional area. The percentage of SWMA was derived from the percentage of SWMA in the total cross-sectional area (from the sham group) measured.14
Electron microscopy
At 42 days post-injury, five rats randomly selected in each group were anesthetized and transcardially perfused with normal saline, and 2.5% glutaraldehyde and 2% paraformaldehyde. The dorsolateral part of 3-mm spinal cord segment rostral to the injury epicenter was cut into a 1 mm × 1 mm × 3 mm piece. The samples were postfixed in the same fixative for 2 h at 4 °C, rinsed three times in 0.1 M sodium cacodylate buffer (pH=7.2), postfixed in 1% osmium tetroxide for 2 h at 4 °C, they were then rinsed in PBS, dehydrated in a graded series of alcohol and propylene oxide and embedded in epon (SPI). Transverse serial sections were sliced at rostral side of the pieces, and a second section per rat was chosen for analysis. Ultrathin (70 nm) sections were prepared on an ultra-microtome, and then stained with uranyl acetate and lead citrate. The sections were viewed using a transmission electron microscope (H-7650, Hitachi, Japan).
Ten microscopy fields of every section were selected randomly and photographed at a magnification of × 10 000. The average histological parameters of 10 microphotographs (18 × 18 μm2) of each rat were used for quantitative analysis using IPP 6.0 software (10 microphotographs per section,1section per rat). As described previously,15 intra-axonal area was calculated by a sum of axonal areas (calculated with inner diameter and assuming circular axonal profiles). Myelin area was estimated by the difference in areas of the inner and outer circular profiles of the axons summed over all axons. Extra-axonal area was defined as the area by deducting intra-axonal area and myelin area from the whole microphotograph area. All areas were expressed as their ratios to the area of the whole microphotograph (that is, intra-axonal fraction+extra-axonal fraction+myelin fraction=1). Finally, the cumulative axonal membrane circumference was estimated by the sum of all the axonal perimeters calculated with din.
Statistical analysis
The statistical analysis was performed using SPSS software 17.0 (SPSS Inc., Chicago, IL, USA). All the data were analyzed using one-way analysis of variance (ANOVA) with Bonferroni for post-hoc comparisons (corrected α=0.008 for the BBB score and percentage of SWMA, α=0.005 for the inclined plane test and ultrastructure). All values were expressed as mean±s.d.
Results
Myelotomy improves locomotor functions of rats with SCI
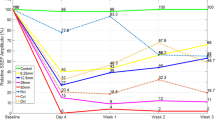
Before SCI, BBB scores in all groups were 21. After SCI, rats in the 8 h-MTG or 24 h-MTG showed significantly better performance compared with those in the CG at 35 and 42 days post-injury (P<0.008) (Figure 1). Moreover, mean BBB score in rats in the 48 h-MTG was increased by 2.3 points compared with that in the CG at 42 days post-injury (P=0.023, P>0.008). No significant difference in BBB scores was detected among the three myelotomy groups (P>0.008). At 42 days after injury, the average BBB score in the rats in the 24 h-MTG was 16, and their toe clearance occurred frequently during forward limb advancement; their predominant paw position was parallel at initial contact. Average BBB score of the rats in the 48 h-MTG group was 14 and the rats had no toe clearance or paw position parallel at initial contact.
Before injury, mean angle scores in all groups showed ∼65 °. Mean angle value in both 8 h-MTG and 24 h-MTG was increased by 5.0 or 8.8 ° when compared with that in the CG at 14 days post-injury, respectively (P<0.005; Figure 2). The improvement in functional recovery continued throughout the survival period. The rats in the myelotomy groups scored 7–10 points more than those in the CG group at 42 days after injury. Moreover, the mean angle value in 48 h-MTG was significantly higher than that in the CG only at 42 days post-injury (P<0.005). At 14, 21 or 28 days post injury, a significant difference in the mean angle value was detected between 24 h-MTG and 48 h-MTG (P<0.005).
More spared white matter was found in the spinal cord of rats with myelotomy
At 42 days after SCI, for the injury epicenter, the percentages of SWMA of each of the three MTG were higher than those of the CG by 0.104, 0.15 or 0.095, respectively (Figure 3; P=0.026 for 8 h-MTG, P=0.001 for 24 h-MTG; P=0.046 for 48 h-MTG). However, at 5 mm caudal or 5 mm rostral to the injury epicenter, no significant difference was found between each of the three MTG and CG.
Myelotomy preserved ultrastructures of myelin and axons
We found that normal ultrastructures of the spinal cord were severely damaged in the CG, axons appear obviously disorganized and demyelinated, and intra-myelinic vacuolization occurred (Figure 4b). By contrast, more well-preserved myelin and axons in the three MTG were found compared with those in the CG (Figures 4c–e). Quantitative analysis (Table 1) revealed that the 24 h-MTG showed a higher intra-axonal fraction and myelin fraction, and a lower extra-axonal fraction when compared with the 48 h-MTG (P<0.005).
Electron microscopic (EM) micrographs showing axons, myelin and extra-axonal space of spinal cord sections (around the dorsolateral part of the spinal cord 3 mm rostral to the injury epicenter) 42 days after injury. (a) A representative EM photo of the sham group showed normal axons and myelin. (b) A representative EM photo of the CG showed severe disruption of axon and myelin (including dissolved axon, obvious intramyelinic vacuolization). EM microphotos from 8 h-MTG (c), 24 h-MTG (d) and 48 h-MTG (e) showed less or slighter loss of myelin compaction, intra-myelinic vacuolization and swollen axon compared with those in the contusion group. White arrow indicates intra-myelinic vacuolization, black arrow indicates a dissolved axon, and white triangle arrow indicates relatively well-preserved myelin sheaths and axons. Scale bar=5 μm in a, b, c, d and e.
Both the BBB scale and inclined plane test showed functional recovery in the 8 h-MTG and 24 h-MTG groups were significantly better than that of the CG. Additionally, the inclined plane test demonstrated 48 h-MTG had a significantly higher angle value than the CG. Results of both histological and ultrastructral analysis showed that 24 h-MTG had significantly better outcomes than the CG. A significant difference in ultrastructural features between 24 h-MTG and 48 h-MTG groups was detected. Thus, the combination of behavioral and histological observation was able to offer more powerful evidence.
Discussion
Our results confirmed that early microsurgical myelotomy could be an effective therapeutic measure for rats with SCI by the observation of their behavior and histology. The BBB scale is a very sensitive and reliable tool in the evaluation of locomotor function in rats after SCI. The upper part of the BBB scale includes rather discrete movement aspects that do not represent major improvements in the motor ability, while the inclined plane test evaluates the improvement of postural control function;16 therefore, the combination of the BBB scale and inclined plane test is a valid method to evaluate the behavioral changes. The motor functions via the BBB scale reached a plateau period from 5 or 6 weeks after spinal cord contusion (25 g cm);14 therefore, we observed the recovery up to 42 days. In the histological study, the quantitative analysis of spared white matter was performed on gross anatomy and at the microscopic level. The spared white matter is the structural basis of function in the rats with injured spinal cord, and previous studies have shown that the residual white matter was significantly and positively correlated with functional deficit by the BBB score or combined behavioral score after SCI.14, 17 Therefore, it is of great significance to improve the preservation of spared white matter for the recovery after SCI. Here, we investigated the ultrastructural changes of the dorsolateral part of the spinal cord. Quantitative analysis of ultrastructure provides more accurate information than immunohistochemical staining with Luxol fast blue.18 The rubrospinal tract, the main part of the dorsolateral funiculus at thoracic spinal cord, involves in the hindlimb locomotion function in rodents.19
Here, we focused on the optimal timing of myelotomy after SCI in rats. The role of timing of surgical decompression after traumatic SCI is one of the most controversial subjects in spine surgery.20, 21 A current evidence-based examination of pre-clinical and clinical studies has shown that epidural decompression should be considered from 8 to 24 h following acute traumatic SCI,4 therefore, we chose 8, 24 and 48 h to evaluate the timing of myelotomy. In this study, our results suggested that myelotomy is still effective in rats up to 48 h after SCI, while previous experimental studies mainly focused on the time points within 24 h.6, 7, 8, 9 In addition, we found that the potential timing of myelotomy may be between 8 and 24 h after SCI. First, myelotomy at 8 or 24 h after SCI significantly increased BBB scores in rats (P<0.008), while myelotomy at 48 h showed less efficacy (P=0.023), which indicated that myelotomy between 8–24 h after SCI had a better outcome than at 48 h. Second, the angle value of the inclined plane test or percentage of SWMA in the 8 h-MTG or 24 h-MTG was higher than that in the 48 h-MTG. Third, improved ultrastructural results showed that the efficacy of myelotomy at 24 h after SCI was better than that at 48 h. In addition, the peak of edema in the white matter was between 48 and 72 h and the timing of maximum hemorrhage was at 12 h after spinal cord contusion in rats.22 Therefore, the injured spinal cord at 48 h-MTG might undergo damage from the hemorrhage and high intramedullary pressure for a relatively longer time than that at 8 h-MTG or 24 h-MTG. On the basis of these findings, the potential ‘time window of myelotomy’ may be between 8 and 24 h after SCI. This result is also similar to the pre-clinical and clinical studies regarding the timing of bony decompression as described previously,3, 4, 13 which meant that the combination of myelotomy and bony decompression would be feasible.
We unexpectedly found that 8 h-MTG did not show a better outcome than the 24 h-MTG, which is different from the results of Kalderon’s study.6 The difference may be related to difference in animal models, surgical procedures or observational indices. Severe contusion (50 gcm) was applied in the Kalderon’s study, while moderate contusion (25 gcm) was applied in the present study. The histopathological changes of the spinal cord after SCI varied with the severity of the impact;17 therefore, the efficacy of myelotomy may vary with the severity of the impact. The damaged area at 1 week was the only index used for the comparison of the effects of myelotomy at different time points in their study, while both the behavioral and histological changes at 6 weeks after SCI were observed in our study. Recovery from anesthesia in chloral-hydrate-anesthetized animals was slow, and a decrease in systolic and diastolic blood pressure was of a high magnitude;23, 24 therefore, it is possible that the shorter anesthesia interval between contusion and myelotomy in 8 h-MTG may lead to decreased systematic blood pressure. Decreased blood pressure leads to decreased blood supply of the spinal cord, and therefore deteriorates ischemia/hypoxia after acute SCI.25 Another possible explanation is that the scattered blood clot in the spinal cord at 8 h after injury has no sufficient time to form the whole clot, and thus, it is harder to remove it thoroughly.
The present study is a preliminary study of optimal timing of myelotomy and it is worthwhile to note several limitations in this study. Although our findings showed significant differences on the BBB scores, this assumption was based on a small number of animals used and no formal power analysis was performed, thus, the current data will be used to inform future studies, which are correctly powered. Moreover, in terms of the mode of surgery, if the impact force is mild and the hematoma is small or absent, the more spared tissue around the lesion epicenter will be preserved and removal of the hemorrhagic tissue by myelotomy may cause further damage to the spared tissue; therefore, the opening of the meninges is more feasible in mild SCI. However, some questions including spinal cord herniation need to be resolved before the opening of the meninges is readily applied in patients. If a durotomy was applied as a control in our study, our conclusion would be more powerful. In the future, we will specially investigate the roles of different surgical methods including durotomy, pial incision or myelotomy in graded spinal cord contusion.
To our best knowledge, this is the first study on the optimal timing of myelotomy after SCI in rats by observation of changes in both behavior and histology. Our findings are expected to have significantly practical implications in patients with SCI, and will provide experimental basis for further understanding myelotomy in different animal models after SCI.
Data archiving
There were no data to deposit.
References
Borgens RB, Liu-Snyder P . Understanding secondary injury. Q Rev Biol 2012; 87: 89–127.
Wyndaele JJ . The impact of early versus late surgical decompression on neurological recovery after traumatic spinal cord injury (SCI). Spinal Cord 2012; 50: 789.
Fehlings MG, Vaccaro A, Wilson JR, Singh A, W Cadotte D, Harrop JS et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS ONE 2012; 7: e32037.
Furlan JC, Noonan V, Cadotte DW, Fehlings MG . Timing of decompressive surgery of spinal cord after traumatic spinal cord injury: an evidence-based examination of pre-clinical and clinical studies. J Neurotrauma 2011; 28: 1371–1399.
Zhu H, Feng YP, Young W, You SW, Shen XF, Liu YS et al. Early neurosurgical intervention of spinal cord contusion: an analysis of 30 cases. Chin Med J (Engl) 2008; 121: 2473–2478.
Kalderon N, Muruganandham M, Koutcher JA, Potuzak M . Therapeutic strategy for acute spinal cord contusion injury: cell elimination combined with microsurgical intervention. PLoS One 2007; 2: e565.
Iwasaki Y, Ito T, Isu T, Tsuru M . [Effects of pial incision and steroid administration on experimental spinal cord injury (author's transl)]. Neurol Med Chir (Tokyo) 1980; 20: 965–970.
Freeman LW, Wright TW . Experimental observations of concussion and contusion of the spinal cord. Ann Surg 1953; 137: 433–443.
Allen A . Surgery of experimental lesion of spinal cord equivalent to crush injury of fracture dislocation of spinal column. JAMA 1911; LVII: 878–880.
Smith JS, Anderson R, Pham T, Bhatia N, Steward O, Gupta R . Role of early surgical decompression of the intradural space after cervical spinal cord injury in an animal model. J Bone Joint Surg Am 2010; 92: 1206–1214.
Koyanagi I, Iwasaki Y, Isu T, Akino M, Abe H, Mitsumori K et al. [Myelotomy for acute cervical cord injury. Report of four cases]. Neurol Med Chir (Tokyo) 1989; 29: 302–306.
Rivlin AS, Tator CH . Effect of vasodilators and myelotomy on recovery after acute spinal cord injury in rats. J Neurosurg 1979; 50: 349–352.
Wilson JR, Singh A, Craven C, Verrier MC, Drew B, Ahn H et al. Early versus late surgery for traumatic spinal cord injury: the results of a prospective Canadian cohort study. Spinal Cord 2012; 50: 840–843.
Basso DM, Beattie MS, Bresnahan JC . Graded histological and locomotor outcomes after spinal cord contusion using the NYU weight-drop device versus transection. Exp Neurol 1996; 139: 244–256.
Concha L, Livy DJ, Beaulieu C, Wheatley BM, Gross DW . In vivo diffusion tensor imaging and histopathology of the fimbria-fornix in temporal lobe epilepsy. J Neurosci 2010; 30: 996–1002.
Sedy J, Urdzikova L, Jendelova P, Sykova E . Methods for behavioral testing of spinal cord injured rats. Neurosci Biobehav Rev 2008; 32: 550–580.
Noble LJ, Wrathall JR . Correlative analyses of lesion development and functional status after graded spinal cord contusive injuries in the rat. Exp Neurol 1989; 103: 34–40.
Kozlowski P, Raj D, Liu J, Lam C, Yung AC, Tetzlaff W . Characterizing white matter damage in rat spinal cord with quantitative MRI and histology. J Neurotrauma 2008; 25: 653–676.
Muir GD, Webb AA, Kanagal S, Taylor L . Dorsolateral cervical spinal injury differentially affects forelimb and hindlimb action in rats. Eur J Neurosci 2007; 25: 1501–1510.
Raslan AM, Nemecek AN . Controversies in the surgical management of spinal cord injuries. Neurol Res Int 2012; 2012: 417834.
Bourassa-Moreau E, Mac-Thiong JM, Ehrmann FD, Thompson C, Parent S . Complications in acute phase hospitalization of traumatic spinal cord injury: does surgical timing matter? J Trauma Acute Care Surg 2013; 74: 849–854.
Weirich SD, Cotler HB, Narayana PA, Hazle JD, Jackson EF, Coupe KJ et al. Histopathologic correlation of magnetic resonance imaging signal patterns in a spinal cord injury model. Spine (Phila Pa 1976) 1990; 15: 630–638.
Rodrigues SF, de Oliveira MA, Martins JO, Sannomiya P, de Cassia TR, Nigro D et al. Differential effects of chloral hydrate- and ketamine/xylazine-induced anesthesia by the s.c. route. Life Sci 2006; 79: 1630–1637.
Nout YS, Beattie MS, Bresnahan JC . Severity of locomotor and cardiovascular derangements after experimental high-thoracic spinal cord injury is anesthesia dependent in rats. J Neurotrauma 2012; 29: 990–999.
Tator CH, Fehlings MG . Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg 1991; 75: 15–26.
Acknowledgements
This work was supported by funds (the Supporting Program of the ‘Twelve Five-year Plan’ for Science & Technology Research of China: 2012BAI34B02, State Natural Science Foundation: No. 81272164 and Special Funds Projects for Basic Scientific Research Business Expenses of Central Public Welfare Research Institutes in Chinese: No. 2011CZ-2).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yang, DG., Li, JJ., Gu, R. et al. Optimal time window of myelotomy in rats with acute traumatic spinal cord injury: a preliminary study. Spinal Cord 51, 673–678 (2013). https://doi.org/10.1038/sc.2013.56
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.56