Abstract
Study design
Retrospective comparative clinical study.
Objective
To establish eligible diagnostic criteria for traumatic cervical spinal cord injury (TCSCI) without major fracture or dislocation and create a definitive clinical protocol by comparing the pathophysiology of CSCI in both traumatic and degenerative disorders.
Setting
Fukuoka, Japan.
Methods
A total of 21 TCSCI patients and 16 rapid progressive clinical deterioration of cervical spondylotic myelopathy (rp-CSM: additional cervical spinal cord injury with an existing cervical myelopathy) patients with impairment graded as C or D on the American Spinal Injury Association (ASIA) Impairment Scale were included in the study. Magnetic resonance (MR) images and ASIA motor scores were evaluated for all of the patients at the time of admission and 12 months postoperatively.
Results
The T2-weighted MR images for all patients showed an abnormally high intramedullary signal in the area of the injured segment at the first examination. At 12 months post-surgery, 47.62% of patients with TCSCI and none with rp-CSM had an abnormally low intramedullary signal change on T1-weighted MR images. The neurological improvement with rp-CSM was significantly greater than that with TCSCI at 12 months postoperatively.
Conclusions
Our results suggest that the pathophysiology of CSCI between traumatic injury and degenerative disorder are similar, but not identical. The most important factor in the early pathophysiological differential diagnosis between these two pathologies is the presence of an existing cervical myelopathy. We believe that early prognosis with eligible diagnosis for CSCI may lead to early preparations for social rehabilitation in each case.
Similar content being viewed by others
Introduction
Most patients with traumatic cervical spinal cord injury (TCSCI) without major fracture or dislocation have pre-existing cervical spondylotic changes or cervical ossification of the posterior longitudinal ligament (OPLL), which results in narrowing of the cervical spinal canal [1]. Hyperextension of the cervical spine has been postulated to be an important mechanism of TCSCI in the absence of major bony injuries [1,2,3,4,5,6].
Numerous controversies exist with regard to the clinical management of TCSCI. Some authors recommended the surgical treatment of TCSCI without major fracture or dislocation with cervical spinal cord compression at the injured segment [7,8,9,10]. In particular, La Rosa et al. [9] reported that early decompression surgery within 24 h of trauma had a significantly better outcome when clinically compared with late surgical management. In contrast, there have been some negative reports [11,12,13] regarding the effects of the surgical treatment. Kawano et al. [12] reported that surgical treatment of TCSCI without major fracture or dislocation with spinal cord compression, even in the acute stage, was not found to be superior to conservative treatment. Therefore, the same pathophysiological diagnosis can have decisively different clinical protocols and clinical outcomes. We considered that there might be differences among surgeons in the pathological diagnostic criteria being used.
We previously reported the pathophysiology of rapid, progressive, clinical deterioration of cervical spondylotic myelopathy (rp-CSM) [14]. We defined this pathophysiology as additional cervical spinal cord injury by natural course or from a minor trauma with an existing cervical myelopathy due to cervical spondylosis (including cervical OPLL). Diagnostic imaging of rp-CSM revealed cervical cord compression at the injured segment with an abnormal intramedullary signal change observed only on T2 weighted magnetic resonance image (MRI). The apparent pathology of rp-CSM is extremely similar to that of TCSCI, though this is based on limited medical information. The diagnostic criteria for TCSCI without major fracture or dislocation are still obscure, and the pathophysiology of rp-CSM might be included in a broad sense with TCSCI in general. The pathophysiology of CSCI between traumatic and degenerative states must be different, and as a matter of course, clinical protocols and clinical outcomes must be different between these two pathophysiologies.
The purpose of this retrospective clinical study was to establish eligible diagnostic criteria for TCSCI without major fracture or dislocation and create a definitive clinical protocol by comparing the pathophysiology of CSCI in both traumatic and degenerative disorders. We believe that an eligible diagnosis and a certain treatment of TCSCI may facilitate early preparations for social rehabilitation in each CSCI case.
Materials and methods
Study population
A total of 21 patients with TCSCI without major fracture or dislocation (admitted within 48 h after trauma, 15 men and six women; average age 63.0 years) and 16 patients with rp-CSM (11 men and five women; average age 75.1 years) were included in the study. All patients had motor impairment grades of C or D per the American Spinal Injury Association (ASIA) Impairment Scale. Patients with a history of any past spinal surgery or neuropathic disease were excluded from the study. All patients were treated surgically by means of French-door cervical laminoplasty by experienced spine surgeons.
Institutional Review Board approval was granted and informed consent was obtained from all patients.
Radiographic analysis (MRI)
MRIs included T1- and T2-weighted sagittal images were evaluated at the time of admission and 12 months postoperatively. We assessed the injured cervical cord segment by examining the intramedullary signal changes as determined on T2-weighted MRIs. The injured segment involved in the TCSCI and rp-CSM are shown in Table 1. Both groups had a high frequency of injuries at the C3-4 segment.
Neurological evaluation
Clinical assessments of upper and lower limb function were performed preoperatively and 12 months postoperatively using the ASIA motor scores (upper limb: range, 0–50; lower limb: range, 0–50; total: range, 0–100). The neurological improvement ratio during the 12 months post-surgery was defined as {(12 months postoperative ASIA motor score) – (preoperative ASIA motor score)/(50 or 100) − (preoperative ASIA motor score)} × 100.
Statistical analysis
The Mann–Whitney U test was used for all statistical analyses. A P value of less than 0.05 was considered statistically significant.
Results
The average age of the patients with rp-CSM was significantly higher than those with TCSCI (p < 0.001). Sex did not appear to affect the condition between two subjects.
Radiographic analysis (MRI)
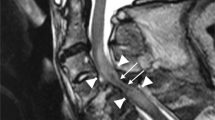
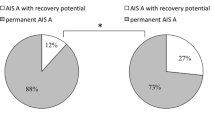
All patients had cervical cord a blurred, high intramedullary signal area at the injured segment only on T2-weighted MRIs at the first examination (Fig. 1). However, at 12 months postoperatively, the blurred high signal area converged to a localized point. Moreover, 10 out of 21 (47.62%) patients with TCSCI and none (0%) of the patients with rp-CSM showed a localized abnormal intramedullary low signal change at the injured segment on T1-weighted MRIs (Fig. 2).
Neurological evaluation
The ASIA motor scores for all patients preoperatively and 12 months postoperatively are shown in Table 2. All of the ASIA motor scores (upper limb, lower limb, and total) significantly improved over the 12 months after surgery (p < 0.001 for all scores).
Significant differences were observed between the two groups for all ASIA motor scores both preoperatively and 12 months postoperatively (p < 0.001 for all). With respect to the neurological improvement ratio, significant differences were observed for both the lower limb and total ratios (p < 0.01 and p < 0.05, respectively), however, there was no significant difference in the score for the upper limb.
Discussion
MRI is a noninvasive method used to monitor the pathologic features of spinal cord lesions. MR images can provide various types of diagnostic information and has become essential as the gold standard for diagnosing spinal cord injury (SCI). The existence of intramedullary signal intensity and signal location, as well as the effacement of the spinal cord compression, on the images helps us to diagnose patients with SCI. In our series, the C3-4 segment was the most commonly injured segment in patients with TCSCI without major fracture or dislocation or rp-CSM diagnosed by T2-weighted sagittal MR images in the early stage.
It has been reported in several histopathologic studies of CSCI that a blurred intramedullary high-signal area on the T2-weighted MR image is thought to represent edema or petechial hemorrhage. In contrast, a low-signal area on the T1-weighted MR image is thought to indicate necrosis, myelomalacia, or an intramedullary cyst [15, 16]. Ohshio et al. [15] reported that severe spinal cord injuries were characterized by abnormal intramedullary signal intensities that were low on T1-weighted MRIs and high on the T2-weighted MRIs. In the gray matter, an abnormally high intensity on a T2-weighted MRI is regarded as the first sign of nerve alteration, and an abnormally low intensity on a T1-weighted MRI is regarded as a secondary sign that indicates severe nerve alteration. In our series, all of the patients with TCSCI without major fracture or dislocation and rp-CSM had abnormally high signals in the area of the injured segment on T2-weighted images. However, on the T1-weighted MRIs, 47.62% of the patients with TCSCI had abnormally low signal change at the sub-acute or chronic stages, and none of the patients with degenerative CSCI had abnormal signal changes. Our results suggest that the T1-weighted MRIs are the most reliable quantitated tool to discriminate between traumatic and degenerative states of CSCI. However, abnormal signal changes on the T1-weighted MRIs appear in the sub-acute or chronic stages after injury, and unfortunately, we cannot reference the differences of causative mechanism of these abnormal signal changes between traumatic and degenerative state of CSCI in this retrospective study. Therefore, these images cannot be a valuable diagnostic tool for an early differential diagnosis between the traumatic and degenerative states of CSCI.
In the series, preoperative neurological status in the patients with TSCSI was significantly more severe than for those with degenerative CSCI; however, significant improvement in the neurological findings in both the upper and lower limbs following decompression surgery was observed for both traumatic and degenerative CSCI. Regarding to the neurological improvement ratio12 month postoperatively, the patients with degenerative CSCI had a significantly higher improvement ratio in the lower limbs and in total function than those with TCSCI. Our previous study demonstrated that the natural neurological course of the TCSCI gradually improved within three months post-injury with or without surgical treatment, and surgical intervention for decompression does not affect the clinical outcome at 12 months postoperatively [12]. Of course, if there was a severe cervical cord compression at the injured segment, the indication of decompression surgery should be considered. However, there is no evidence of efficacy of early decompression surgery for genuine TCSCI [12]. Therefore, general or neurological status of TCSCI should be considered cautiously for elective surgical management. In contrast, in the degenerative CSCI, natural neurological course gradually deteriorated after injury, and early surgical decompression greatly affect the clinical outcome [14]. Our results suggest that these two pathophysiologies are similar, but not identical.
Based on our results, the most important factor in the early pathophysiological differential diagnosis between traumatic and degenerative CSCI is the presence of an existing cervical myelopathy. A detailed clinical history to determine of presence of existing cervical myelopathy is important. We believe that early prognosis with eligible diagnosis for CSCI may lead to early preparations for social rehabilitation in each case.
Certain issues remain unaddressed in the current study. The preoperative age and neurological status were significantly different between the patients with traumatic and degenerative CSCI. Therefore, using the current investigation as a pilot study, further research using a larger patient population and long-term follow-up may help in resolving several remaining unclear issues. Moreover, the pathophysiological difference between traumatic and degenerative CSCI needs to be clarified in greater detail.
Conclusions
Our results suggested that the pathophysiologies of TCSCI and degenerative CSCI are similar, but not identical. T1-weighted MR images are the most reliable quantitated method to discriminate between traumatic and degenerative CSCI at the sub-acute or chronic stages. For an early pathophysiological diagnosis between traumatic and degenerative CSCI, determining the presence of an existing cervical myelopathy before the trauma is the most important factor. A detailed clinical history of existing cervical myelopathy is necessary.
Data availability
All data supporting the findings of this study are available within the article and its Supplementary Materials.
References
Gupta SK, Rajeev K, Khosla VK, Sharma BS, Paramjit, Mathsriya SN, et al. Spinal cord injury without radiographic abnormality in adults. Spinal Cord. 1999;37:726–9.
Harrop JS, Sharan A, Ratliff J. Central cord injury: pathophysiology, management, and outcomes. Spine J. 2006;6:198S–206S.
Koyanagi I, Iwasaki Y, Hida K, Akino M, Imamura H, Abe H, et al. Acute cervical cord injury without fracture or dislocation of the spinal column. J Neurosurg. 2000;93:15–20.
Shimada K, Tokioka T. Sequential MR studies of cervical cord injury: correlation with neurological damage and clinical outcome. Spinal Cord. 1999;37:410–5.
Shimada K, Tokioka T. Sequential MRI studies in patients with cervical cord injury but without bony injury. Paraplegia. 1995;33:573–8.
Tewari MK, Gifti DS, Singh P, Khosla VK, Mathuriya SN, Gupta SK, et al. Diagnosis and prognostication of adult spinal cord injury without radiographic abnormality using magnetic resonance imaging: analysis of 40 patients. Surg Neurol. 2005;63:204–9.
Bose B, Northrup BE, Osterholm JL, Cotler JM, DiTunno JF. Reanalysis of central cervical cord injury management. Neurosurgery. 1984;15:367–72.
Chen TY, Dickman CA, Eleraky M, Sonntag VKH. The role of decompression for acute incomplete cervical spinal cord injury in cervical spondylosis. Spine. 1998;23:2398–403.
La Rosa G, Conti A, Cardali S, Cacciola F, Tomasello F. Does early decompression improve neurological outcome of spinal cord injured patients? Appraisal of literature using a metaanalytical approach. Spinal Cord. 2004;42:503–12.
Yamazaki T, Yanaka K, Fujita K, Kamezaki T, Uemura K, Nose T. Traumatic central cord syndrome: analysis of factors affecting the outcome. Surg Neurol. 2005;63:95–9.
Itoh Y, Mazaki T, Koshimune K, Morita T, Mizuno S. Randomized controlled study of treatment for acute cervical cord injury with spinal canal stenosis but without radiographic evidence of trauma (SCIWORET): operative or conservative treatment. J Spine Res. 2011;2:965–7.
Kawano O, Ueta T, Shiba K, Iwamoto Y. Outcome of decompression surgery for cervical spinal cord injury without bone and disc injury in patients with spinal cord compression: a multicenter prospective study. Spinal Cord. 2010;48:548–53.
Takao T, Morishita Y, Okada S, Maeda T, Katoh F, Ueta T, et al. Clinical relationship between cervical spinal canal stenosis and traumatic cervical spinal cord injury without major fracture or dislocation. Eur Spine J. 2013;22:2228–31.
Morishita Y, Matsushita A, Maeda T, Ueta T, Naito M, Shiba K. Rapid progressive clinical deterioration of cervical spondylotic myelopathy. Spinal Cord. 2015;9:408–12.
Ohshio I, Hatayama A, Kaneda K, Takahata M, Nagashima K. Correlation between histopathologic features and magnetic resonance images of spinal cord lesions. Spine. 1993;18:1140–9.
Weirich SD, Cotler HB, Narayama PA, Hazle JD, Jackson EF, Coupe KJ, et al. Histopathologic correlation of magnetic resonance imaging signal patterns in a spinal cord injury model. Spine. 1990;15:630–8.
Funding
This work was supported by Grant-in-aid for Scientific Research (C) from The Japanese Ministry of Education, Culture, Sports, Science and Technology (Grant Number 19K09662) and ZENKYOREN (National Mutual Insurance Federation of Agricultural Cooperatives).
Author information
Authors and Affiliations
Contributions
OK was responsible for conceived and/or designed the work that led to the submission, acquired data, and/or played an important role in interpreting the results. TM was responsible for drafted or revised the manuscript for important intellectual content, and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morishita, Y., Kawano, O. & Maeda, T. The pathophysiology of cervical spinal cord injury: what are the differences between traumatic injury and degenerative disorder. Spinal Cord Ser Cases 8, 50 (2022). https://doi.org/10.1038/s41394-022-00517-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00517-7