Abstract
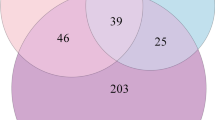
Large-scale cohort and epidemiological studies suggest that post-traumatic stress disorder (PTSD) confers risk for late-onset Alzheimer’s disease and related dementias (ADRD); however, the basis for this association remains unclear. Several prior studies of military veterans have reported that carriers of the apolipoprotein E (APOE) ε4 gene variant are at heightened risk for the development of PTSD following combat exposure, suggesting that PTSD and ADRD may share some genetic risk. Here we designed a cohort study to further examine the hypothesis that ADRD genetic risk also confers risk for PTSD. To do so, we examined APOE ε4 and ε2 genotypes, an Alzheimer’s disease polygenic risk score, and other veteran-relevant risk factors for PTSD in age-stratified groups of individuals of European (n = 123,372) and African (n = 15,220) ancestry in the US Department of Veterans Affairs’ Million Veteran Program. Analyses revealed no significant main effect associations between the APOE ε4 (or ε2) genotype or the Alzheimer’s disease polygenic risk score on PTSD severity or diagnosis. There were also no significant interactions between measures of Alzheimer’s disease genetic risk and either combat exposure severity or history of head injury in association with PTSD in any age group. We conclude that the association between PTSD and the primary ADRD genetic risk factor, APOE ε4, that was reported previously was not replicable in this large and relevant dataset. Thus, the epidemiological association between PTSD and ADRD is not likely to be driven by the major genetic factors underlying ADRD risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The phenotypes and genetic data analyzed here are available to all researchers with MVP access. Approval to access the individual-level MVP data is only available to VA researchers for an approved and funded MVP project, either through a VA Merit Award or a Career Development Award. See https://www.research.va.gov/funding/Guidance-MVP-Data-Access-Merit-Award.pdf for details. All GWAS results for MVP are made available on dbGAP.
Code availability
Analytic code is available for those with approved MVP access by writing to the corresponding author. Our group generated this code.
References
Yaffe, K. et al. Military-related risk factors in female veterans and risk of dementia. Neurology 92, e205–e211 (2019).
Yaffe, K. et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch. Gen. Psychiatry 67, 608–613 (2010).
Qureshi, S. U. et al. Greater prevalence and incidence of dementia in older veterans with posttraumatic stress disorder. J. Am. Geriatr. Soc. 58, 1627–1633 (2010).
Bergman, B. P., Mackay, D. F. & Pell, J. P. Dementia in Scottish military veterans: early evidence from a retrospective cohort study. Psychol. Med. 53, 1015–1020 (2023).
Gunak, M. M. et al. Post-traumatic stress disorder as a risk factor for dementia: systematic review and meta-analysis. Br. J. Psychiatry 217, 600–608 (2020).
Clouston, S. A. P. et al. Incidence of mild cognitive impairment in World Trade Center responders: long-term consequences of re-experiencing the events on 9/11/2001. Alzheimers Dement. 11, 628–636 (2019).
Bhattarai, J. J., Oehlert, M. E., Multon, K. D. & Sumerall, S. W. Dementia and cognitive impairment among U.S. veterans with a history of MDD or PTSD: a retrospective cohort study based on sex and race. J. Aging Health 31, 1398–1422 (2019).
Mawanda, F., Wallace, R. B., McCoy, K. & Abrams, T. E. PTSD, psychotropic medication use, and the risk of dementia among US veterans: a retrospective cohort study. J. Am. Geriatr. Soc. 65, 1043–1050 (2017).
Wang, T. Y. et al. Risk for developing dementia among patients with posttraumatic stress disorder: a nationwide longitudinal study. J. Affect. Disord. 205, 306–310 (2016).
Logue, M. W. et al. Alzheimer’s disease and related dementias among aging veterans: examining gene-by-environment interactions with post-traumatic stress disorder and traumatic brain injury. Alzheimers Dement. 19, 2549–2559 (2023).
Greenberg, M. S., Tanev, K., Marin, M. F. & Pitman, R. K. Stress, PTSD, and dementia. Alzheimers Dement. 10, S155–S165 (2014).
Farrer, L. A. et al. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. JAMA 278, 1349–1356 (1997).
Genin, E. et al. APOE and Alzheimer disease: a major gene with semi-dominant inheritance. Mol. Psychiatry 16, 903–907 (2011).
Kunkle, B. W. et al. Novel Alzheimer disease risk loci and pathways in African American individuals using the African Genome Resources panel: a meta-analysis. JAMA Neurol. 78, 102–113 (2021).
Logue, M. W., Dasgupta, S. & Farrer, L. A. Genetics of Alzheimer’s disease in the African American population. J. Clin. Med. 12, 5189 (2023).
Sherva, R. et al. African ancestry GWAS of dementia in a large military cohort identifies significant risk loci. Mol. Psychiatry 28, 1293–1302 (2023).
Bellenguez, C. et al. New insights into the genetic etiology of Alzheimer’s disease and related dementias. Nat. Genet. 54, 412–436 (2022).
Blacker, D. et al. ApoE-4 and age at onset of Alzheimer’s disease: the NIMH genetics initiative. Neurology 48, 139–147 (1997).
Sando, S. B. et al. APOE epsilon 4 lowers age at onset and is a high risk factor for Alzheimer’s disease; a case control study from central Norway. BMC Neurol. 8, 9 (2008).
Reiman, E. M. et al. Exceptionally low likelihood of Alzheimer’s dementia in APOE2 homozygotes from a 5,000-person neuropathological study. Nat. Commun. 11, 667 (2020).
Phillips, M. C. Apolipoprotein E isoforms and lipoprotein metabolism. IUBMB Life 66, 616–623 (2014).
Lumsden, A. L., Mulugeta, A., Zhou, A. & Hypponen, E. Apolipoprotein E (APOE) genotype-associated disease risks: a phenome-wide, registry-based, case-control study utilising the UK Biobank. EBioMedicine 59, 102954 (2020).
Liu, C. C., Liu, C. C., Kanekiyo, T., Xu, H. & Bu, G. Apolipoprotein E and Alzheimer disease: risk, mechanisms and therapy. Nat. Rev. Neurol. 9, 106–118 (2013).
Alagarsamy, J., Jaeschke, A. & Hui, D. Y. Apolipoprotein E in cardiometabolic and neurological health and diseases. Int. J. Mol. Sci. 23, 9892 (2022).
Averill, L. A. et al. Apolipoprotein E gene polymorphism, posttraumatic stress disorder, and cognitive function in older U.S. veterans: results from the National Health and Resilience in Veterans Study. Depress. Anxiety 36, 834–845 (2019).
Lutz, M. W., Luo, S., Williamson, D. E. & Chiba-Falek, O. Shared genetic etiology underlying late-onset Alzheimer’s disease and posttraumatic stress syndrome. Alzheimers Dement. 16, 1280–1292 (2020).
Porter, B. et al. Measuring aggregated and specific combat exposures: associations between combat exposure measures and posttraumatic stress disorder, depression, and alcohol-related problems. J. Trauma Stress 31, 296–306 (2018).
Lyons, M. J. et al. Gene-environment interaction of ApoE genotype and combat exposure on PTSD. Am. J. Med. Genet. B Neuropsychiatr. Genet. 162B, 762–769 (2013).
Kimbrel, N. A. et al. Effect of the APOE ε4 allele and combat exposure on PTSD among Iraq/Afghanistan-era veterans. Depress. Anxiety 32, 307–315 (2015).
Peterson, C. K., James, L. M., Anders, S. L., Engdahl, B. E. & Georgopoulos, A. P. The number of cysteine residues per mole in apolipoprotein E is associated with the severity of PTSD re-experiencing symptoms. J. Neuropsychiatry Clin. Neurosci. 27, 157–161 (2015).
Freeman, T., Roca, V., Guggenheim, F., Kimbrell, T. & Griffin, W. S. Neuropsychiatric associations of apolipoprotein E alleles in subjects with combat-related posttraumatic stress disorder. J. Neuropsychiatry Clin. Neurosci. 17, 541–543 (2005).
Logue, M. W. et al. A genome-wide association study of post-traumatic stress disorder identifies the retinoid-related orphan receptor alpha (RORA) gene as a significant risk locus. Mol. Psychiatry 18, 937–942 (2013).
Duncan, L. E. et al. Largest GWAS of PTSD (N=20 070) yields genetic overlap with schizophrenia and sex differences in heritability. Mol. Psychiatry https://doi.org/10.1038/mp.2017.77 (2017).
Nievergelt, C. M. et al. International meta-analysis of PTSD genome-wide association studies identifies sex- and ancestry-specific genetic risk loci. Nat. Commun. 10, 4558 (2019).
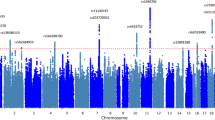
Stein, M. B. et al. Genome-wide association analyses of post-traumatic stress disorder and its symptom subdomains in the Million Veteran Program. Nat. Genet. 53, 174–184 (2021).
Kim, T. Y. et al. Apolipoprotein E gene polymorphism, alcohol use, and their interactions in combat-related posttraumatic stress disorder. Depress. Anxiety 30, 1194–1201 (2013).
Johnson, L. A. et al. ApoE2 exaggerates PTSD-related behavioral, cognitive, and neuroendocrine alterations. Neuropsychopharmacology 40, 2443–2453 (2015).
Roby, Y. Apolipoprotein E variants and genetic susceptibility to combat-related post-traumatic stress disorder: a meta-analysis. Psychiatr. Genet. 27, 121–130 (2017).
Olsen, R. H., Agam, M., Davis, M. J. & Raber, J. ApoE isoform-dependent deficits in extinction of contextual fear conditioning. Genes Brain Behav. 11, 806–812 (2012).
Vasterling, J. J. et al. Longitudinal associations among posttraumatic stress disorder symptoms, traumatic brain injury, and neurocognitive functioning in army soldiers deployed to the Iraq war. J. Int. Neuropsychol. Soc. 24, 311–323 (2018).
Bryant, R. A. et al. The psychiatric sequelae of traumatic injury. Am. J. Psychiatry 167, 312–320 (2010).
Yurgil, K. A. et al. Association between traumatic brain injury and risk of posttraumatic stress disorder in active-duty Marines. JAMA Psychiatry 71, 149–157 (2014).
Merritt, V. C. et al. Apolipoprotein E epsilon4 genotype is associated with elevated psychiatric distress in veterans with a history of mild to moderate traumatic brain injury. J. Neurotrauma 35, 2272–2282 (2018).
Kunkle, B. W. et al. Author correction: Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat. Genet. 51, 1423–1424 (2019).
Kunkle, B. W. et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat. Genet. 51, 414–430 (2019).
Cimino, N., Kang, M. S., Honig, L. S. & Rutherford, B. R. Blood-based biomarkers for Alzheimer’s disease in older adults with posttraumatic stress disorder. J. Alzheimers Dis. Rep. 6, 49–56 (2022).
Weiner, M. W. et al. Traumatic brain injury and post-traumatic stress disorder are not associated with Alzheimer’s disease pathology measured with biomarkers. Alzheimers Dement. https://doi.org/10.1002/alz.12712 (2022).
Pattinson, C. L. et al. Elevated tau in military personnel relates to chronic symptoms following traumatic brain injury. J. Head Trauma Rehabil. 35, 66–73 (2020).
Elias, A. et al. Amyloid-β, tau, and 18F-fluorodeoxyglucose positron emission tomography in posttraumatic stress disorder. J. Alzheimers Dis. 73, 163–173 (2020).
Kritikos, M. et al. Plasma amyloid beta 40/42, phosphorylated tau 181, and neurofilament light are associated with cognitive impairment and neuropathological changes among World Trade Center responders: a prospective cohort study of exposures and cognitive aging at midlife. Alzheimers Dement. 15, e12409 (2023).
Elman, J. A. et al. Genetic risk for coronary heart disease alters the influence of Alzheimer’s genetic risk on mild cognitive impairment. Neurobiol. Aging 84, 237 e235–237 e212 (2019).
Miller, M. W. & Sadeh, N. Traumatic stress, oxidative stress and post-traumatic stress disorder: neurodegeneration and the accelerated-aging hypothesis. Mol. Psychiatry 19, 1156–1162 (2014).
Perry, G., Cash, A. D. & Smith, M. A. Alzheimer disease and oxidative stress. J. Biomed. Biotechnol. 2, 120–123 (2002).
Jones, K. A. & Thomsen, C. The role of the innate immune system in psychiatric disorders. Mol. Cell Neurosci. 53, 52–62 (2013).
Lee, Y. J., Han, S. B., Nam, S. Y., Oh, K. W. & Hong, J. T. Inflammation and Alzheimer’s disease. Arch. Pharm. Res. 33, 1539–1556 (2010).
Wieckowska-Gacek, A., Mietelska-Porowska, A., Wydrych, M. & Wojda, U. Western diet as a trigger of Alzheimer’s disease: from metabolic syndrome and systemic inflammation to neuroinflammation and neurodegeneration. Ageing Res. Rev. 70, 101397 (2021).
He, J. T., Zhao, X., Xu, L. & Mao, C. Y. Vascular risk factors and Alzheimer’s disease: blood-brain barrier disruption, metabolic syndromes, and molecular links. J. Alzheimers Dis. 73, 39–58 (2020).
Wolf, E. J. et al. Posttraumatic stress disorder as a catalyst for the association between metabolic syndrome and reduced cortical thickness. Biol. Psychiatry 80, 363–371 (2016).
Litkowski, E. M. et al. A diabetes genetic risk score is associated with all-cause dementia and clinically diagnosed vascular dementia in the Million Veteran Program. Diabetes Care 45, 2544–2552 (2022).
Rosenbaum, S. et al. The prevalence and risk of metabolic syndrome and its components among people with posttraumatic stress disorder: a systematic review and meta-analysis. Metabolism 64, 926–933 (2015).
Faborode, O. S., Dalle, E. & Mabandla, M. V. Inescapable footshocks induce molecular changes in the prefrontal cortex of rats in an amyloid-beta-42 model of Alzheimer’s disease. Behav. Brain Res. 419, 113679 (2022).
Wei, Z. et al. GSK-3beta and ERK1/2 incongruously act in tau hyperphosphorylation in SPS-induced PTSD rats. Aging 11, 7978–7995 (2019).
Bahorik, A., Bobrow, K., Hoang, T. & Yaffe, K. Increased risk of dementia in older female US veterans with alcohol use disorder. Addiction 116, 2049–2055 (2021).
Mohlenhoff, B. S., O’Donovan, A., Weiner, M. W. & Neylan, T. C. Dementia risk in posttraumatic stress disorder: the relevance of sleep-related abnormalities in brain structure, amyloid, and inflammation. Curr. Psychiatry Rep. 19, 89 (2017).
A Product of the CMS Alliance to Modernize Healthcare Federally Funded Research and Development Center Centers for Medicare & Medicaid Services (CMS). Assessment A Demographics (RAND Corporation, 2015).
Terhakopian, A., Sinaii, N., Engel, C. C., Schnurr, P. P. & Hoge, C. W. Estimating population prevalence of posttraumatic stress disorder: an example using the PTSD checklist. J. Trauma Stress 21, 290–300 (2008).
Harrington, K. M. et al. Validation of an electronic medical record-based algorithm for identifying posttraumatic stress disorder in U.S. Veterans. J. Trauma. Stress 32, 226–237 (2019).
Nguyen, X. T. et al. Data Resource Profile: self-reported data in the Million Veteran Program: survey development and insights from the first 850 736 participants. Int. J. Epidemiol. 52, e1–e17 (2023).
Weathers, F., Litz, B., Herman, D., Huska, J. A. & Keane, T. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. In Annual Convention of the International Society for Traumatic Stress Studies (1993).
Vogt, D. S., Proctor, S. P., King, D. W., King, L. A. & Vasterling, J. J. Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment 15, 391–403 (2008).
Hunter-Zinck, H. et al. Genotyping array design and data quality control in the Million Veteran Program. Am. J. Hum. Genet. 106, 535–548 (2020).
Schurz, H. et al. Evaluating the accuracy of imputation methods in a five-way admixed population. Front. Genet. 10, 34 (2019).
Fang, H. et al. Harmonizing genetic ancestry and self-identified race/ethnicity in genome-wide association studies. Am. J. Hum. Genet. 105, 763–772 (2019).
Choi, S. W. & O’Reilly, P. F. PRSice-2: polygenic risk score software for biobank-scale data. Gigascience 8, giz082 (2019).
Zhang, Q. et al. Risk prediction of late-onset Alzheimer’s disease implies an oligogenic architecture. Nat. Commun. 11, 4799 (2020).
Acknowledgements
This research is based on data from the Million Veteran Program, Office of Research and Development, Veterans Health Administration. It was supported by VA BLR&D grant 1 I01 BX004192 (MVP015) to M.W.L. and by the Department of VA Clinical Science Research and Development Career Development Award IK2CX002192-01A2 to J.R.F. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government.
Author information
Authors and Affiliations
Contributions
M.W.L., M.W.M., R.S., K.M.H., J.R.F., E.J.W. and J.M.G. were responsible for conceptualization. R.Z. and R.S. were responsible for data analysis and data curation. M.W.M., M.W.L., E.J.W., R.Z., R.S. and N.P.D. were responsible for data interpretation. M.W.L., J.M.G. and K.M.H. developed the methodology. M.W.L. acquired the funding. E.J.W., M.W.M. and M.W.L. wrote the original draft. All authors edited and approved the paper. J.M.G. was responsible for resources.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Jacob Raber and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Tables 1–3.
Rights and permissions
About this article
Cite this article
Wolf, E.J., Miller, M.W., Zhang, R. et al. No replication of Alzheimer’s disease genetics as a moderator of the association between combat exposure and PTSD risk in 138,592 combat veterans. Nat. Mental Health (2024). https://doi.org/10.1038/s44220-024-00225-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44220-024-00225-1