Abstract
Poor mental health has been found to be more prevalent among those with cancer and is considered a public health crisis since COVID-19. This study assessed the impact of COVID-19 and cancer survivorship on mental health and investigated factors, including online patient-provider communications (OPPC; email/internet/tablet/smartphone), associated with poor mental health prior to and during the early COVID-19. Nationally representative Health Information National Trends Survey data during 2017–2020 (n = 15,871) was used. While the prevalence of poor mental health was high (40–42%), Difference-In-Difference analyses revealed that cancer survivorship and COVID-19 were not associated with poor mental health. However, individuals that used OPPC had 40% higher odds of poor mental health. Low socioeconomic status (low education/income), younger age (18–64 years), and female birth gender were also associated with poor mental health. Findings highlight the persistence of long-standing mental health inequities and identify that OPPC users might be those who need mental health support.
Similar content being viewed by others
Introduction
Poor mental health, including anxiety, depression, and psychological distress, affects individuals’ well-being and quality of life1. Poor mental health has been found to be more common among cancer survivors than those without a history of cancer due to disease-related concerns, including cancer recurrence, modified body image, or challenges in long-term healthcare needs2. It has been reported to negatively impact treatment adherence, self-management, and mortality among cancer survivors3,4,5,6. Approximately 25% to 40% of cancer survivors experienced poor mental health in 20197. Previously, cancer survivors of Black/African American race/ethnicity, who were unmarried, with lower income, with lower education, who live in a rural residence, or who have low health literacy were reported to have poorer mental health3,8,9,10,11,12. As communications with healthcare providers play an important role in psychological distress management, optimal quality of patient-centered communication (PCC) style13,14 and online-based communications with providers15,16,17,18 have been shown to benefit managing poor mental health.
Under the unprecedented COVID-19 pandemic, psychosocial distress or depression increased in the general population19,20,21, as well as among cancer survivors22,23,24 worldwide. However, studies in the U.S. have observed mixed findings. Health Information National Trends Survey (HINTS) cross-sectional data reported that the prevalence of depression/anxiety slightly decreased among cancer survivors in the U.S. during COVID-19 (2019 vs. 2020), but did not compare estimates to adults without a history of cancer25. Alternatively, the COVID-19 Impact Study using 2020 cross-sectional data reported that cancer survivors had more mental health symptoms, including feeling nervous, anxious, hopeless, lonely, and depressed, than their non-cancer counterparts during COVID-1926. Last, a study using longitudinal data from 5 U.S. regions (Thinking and Living With Cancer) found that depression and anxiety worsened to a similar extent between breast cancer survivors ≥60 years of age and those without cancer during the pandemic27. Prior studies, to our knowledge, have not examined both the impact of COVID-19 and cancer survivorship on mental health, encompassing depression/anxiety and psychological distress. Additionally, chronic medical conditions have not been assessed for potential associations with poor mental health previously among cancer survivors during COVID-1925. Moreover, during the pandemic, PCC was significantly associated with cancer survivors’ mental health28, and online patient-provider communication (OPPC) became an essential channel to address psychological distress29,30,31. However, no studies have investigated the associations of PCC and OPPC with mental health accounting for sociodemographic and clinical factors.
Therefore, this study used HINTS data to assess changes in mental health before (2017–2019) and during COVID-19 (2020) in cancer survivors compared to adults without a history of cancer, taking into consideration patient-provider communication (PCC and OPPC). In addition, we examined the associations of the quality of PCC and OPPC with mental health by time period and cancer survivorship after accounting for sociodemographic and clinical factors. The findings of our study will identify those with poor mental health and inform targeted approaches to improve mental health outcomes.
Methods
Data source
Health Information National Trends Survey (HINTS), a nationally representative survey distributed and collected by the National Cancer Institute (NCI) was used for the study. HINTS is a self-administered, publicly available, cross-sectional survey. The present study used HINTS 5 Cycles 1, 2, 3, and 4 (2017–2020). Of note, the COVID-19 sample (2020) was collected from February to June 2020. The respondents of the survey questionnaires were non-institutionalized civilians 18 years and older in the United States. HINTS 5 Cycles 2, 3, and 4 have two geographic stratum: areas with low and high minority concentrations. HINTS 5 Cycle 1 had one more geographic stratum: an area in Central Appalachia. HINTS 5 was a single-mode mailed survey with a two-stage sampling design in Cycles 1, 2, and 4 and a double-mode design with a pilot push-to web survey in addition to the mailed survey in Cycle 3. HINTS 5 Cycle 3 was remediated and updated in March 2021 and we used the most recent version of HINTS data. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines32. The total number of respondents in HINTS 5 Cycles 1–4 was 16,092. The average response rate was 33% (32.4% in Cycle 1 [n = 3285]; 32.4% in Cycle 2 [n = 3504]; 30.3% in Cycle 3 [n = 5438]; 36.7% in Cycle 4 [n = 3865])33. Among the total respondents, those who reported a history of cancer diagnosis were designated as cancer survivors (n = 2579) and the rest were considered as adults without a history of cancer (n = 13,292) after excluding those who missed reporting their history of cancer information (n = 221). We merged the four iterations (HINTS 5 Cycles 1–4) and obtained 200 replicate weights following the analytic suggestions from HINTS after confirming that there were no significant differences between variables of each iteration. The full-sample weights were applied to account for household-level base weight, non-response, and person-level initial weight34.
Outcome
Mental health was measured by depression/anxiety diagnosis and psychological distress symptoms. To determine depression/anxiety diagnosis status, the question “Has a doctor or other healthcare professional ever told you that you had depression or anxiety disorder?” was used with the responses of “yes,” or “no.” To define psychological distress symptoms, the question “Over the past two weeks, how often have you been bothered by any of the following problems? (1) little interest in doing things, (2) feeling down, depressed, hopeless, (3) feeling nervous or anxious, (4) not being able to stop or control worrying” was used. These four questions were the same as those on the Patient Health Questionnaire (PHQ-4), a brief form commonly used to assess mental health35,36. The responses were measured by a Likert scale (1 = always, 2 = usually, 3 = sometimes, 4 = never). The scores from the four questions were summed to compute a total score, ranging from 4 (the worst) to 16 (the best). This total score was recorded as ‘yes’ for the score of 4–13 (mild/moderate/severe) and ‘no’ for the score of 14–16 (normal), following the PHQ-4’s cut-off approach35 to represent psychological distress. As a last step, we created a new mental health variable with depression/anxiety and total psychological distress score. If either depression/anxiety or the new psychological distress was ‘yes,’ then it was coded as poor mental health.
Covariates
Patient-centered communications (PCC) was measured by the following seven questions that represent the main PCC functions that affect health outcomes, defined by the National Cancer Institute (NCI)37. “In your communication with all doctors, nurses, or other health professionals in the past 12 months, how often did they (1) give you the chance to ask health questions, (2) had the attention you needed to your feelings and emotions, (3) involve you in decisions about your health care as much as you wanted, (4) make sure you understood the things you needed to do to take care of your health, (5) explain things in a way you could understand, 6) spend enough time with you, (7) help you deal with uncertain feelings about your health or health care?”37 Responses for each question were measured on a Likert scale (1 = always, 2 = usually, 3 = sometimes, 4 = never). Responses to the seven questions were combined and recoded using the Likert scale numbers to generate a new continuous PCC outcome, ranging from a score of 0 (the least optimal, when all 7 questions were scored “never”) to a score of 100 (the most optimal, when all 7 questions were scored “always”)38. We also created a binary PCC variable with categories for optimal (when all 7 responses were ‘always’) and sub-optimal (any response of usually, sometimes, or never).
Online patient-provider communications (OPPC) were measured by 3 types of communication behaviors, as done previously39, using the following questions; (1) “In the past 12 months, have you used an email or the internet to communicate with a doctor or doctor’s office?”, (2) “Has your tablet or smartphone helped you in discussions with your healthcare provider?”, (3)“In the past 12 months, have you used your online medical record to securely message health care providers and staff?”. The response to each question was either “yes” or “no.” The tablet/smartphone and EHR questions were only asked to those who owned tablet computers/smartphones or used EHR at least once in the past 12 months. In this study, those who did not have a tablet/smartphone or use EHR once in the past 12 months were included in the no digital device use groups.
We chose sociodemographic factors as independent variables of this study based on the social determinants of health conceptual framework from the Healthy People 203040: Age, birth gender, race/ethnicity, household income, educational attainment, marital status, employment status, health insurance type, a usual source of care, and rurality of residence. HINTS used Urban Rural Commuting Area (RUCA) to designate the rurality of residence of the survey respondents, which categorized census tracts using population density, urbanization, and commuting patterns developed by the United States Department of Agriculture41. Clinical factors included general health status, chronic medical conditions (diabetes, high blood pressure, heart disease, lung disease), time since cancer diagnosis, and diagnosed cancer type among survivors.
Statistical analysis
We conducted descriptive analyses to present sociodemographic and clinical characteristics of cancer survivors and adults without a history of cancer prior to and during COVID-19 using means with standard errors (SE) or weighted percentages (%) with SE. The prevalence of poor mental health was estimated using a weighted percentage (%) with SE by sociodemographic and clinical characteristics. The mean PCC score with SE was estimated among cancer survivors and those without a history of cancer in pre-COVID-19 and COVID-19.
We conducted Differences-In-Differences (D-I-D) analysis in a weighted logistic regression model to identify the differences in the odds of poor mental health from pre- to during COVID, among cancer survivors compared to those without a history of cancer. The D-I-D of the odds of poor mental health was reported as an odds ratio (OR) with a 95% confidence interval (95% CI). D-I-D analyses were adjusted for age, gender, race/ethnicity, education, household income, general health status, and the chronic medical condition of lung disease because these variables were associated with mental health in prior studies8,12,21,25 or were confounders in our analyses (i.e., changed covariate estimates by more than 10%). The parallel trends assumption was tested quantitatively and also by visual inspection to assess if the trends of poor mental health were consistent in those with and without a history of cancer before the pandemic42. Additionally, we stratified the D-I-D analysis by PCC quality (optimal vs. sub-optimal) and OPPC (yes vs. no for Email/Internet communication, Tablet/Smartphone for discussion, EHR message) to identify changes in poor mental health by time period and patient-provider communication adjusting for the same covariates.
In addition, we developed a multivariable-adjusted weighted logistic regression model to examine the associations of history of cancer, COVID-19 time period, PCC, and OPPC with mental health after accounting for sociodemographic and clinical factors. Sensitivity analyses were conducted by separating the mental health outcome into psychological distress and chronic depression status to identify if there were differences in factors associated with each mental health outcome. We assessed the interactions of PCC (composite score) and three digital device use measures with both time periods and history of cancer. For these interaction assessments, we included interaction terms in multivariable logistic regression models. As above, variables included in the final models were associated with mental health in prior studies8,12,21,25 or were a potential confounder in our analyses. We performed imputation for any covariates with missingness, ranging from 0.5% to 22.8% (see footnotes of Table 1). Hot deck imputation was applied to account for missingness, which was also used for non-response by HINTS. As Cycle 3 did not contain employment status, it was not included in the model due to its large missingness (35% in employment status). Imputed data were used for all descriptive and regression analyses in SAS 9.4 (SAS studio 3.8, Cary, NC, USA). We did not perform adjustments for multiple testing as our study design was not confirmatory and planned to avoid the potential risk of increasing type II errors43,44. The statistical significance was determined at p < 0.05.
Ethics statement
The current study used the publicly available national survey data, Health Information National Trends Survey (HINTS). HINTS is a deidentified dataset, and this study is a secondary analysis of the deidentified survey. Because the human subject was not involved in this study, written consent is not applicable. Given that identifiable information was not included, this study was deemed exempt from review by the Institutional Review Board at the University of California, Davis.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Results
Sociodemographic and clinical characteristics of the study population
Table 1 shows population characteristics of cancer survivors and adults without a history of cancer, before and during COVID-19. Cancer survivors were older, with 51% of cancer survivors aged 65 or older compared to 17% of adults without a history of cancer. Among cancer survivors, 36% were employed (vs. 58% in those without a history of cancer), 33% had private or employment-based insurance (vs. 54%), 84% had a usual source of care (vs. 63%), 25% reported poor general health status (vs. 14%), and 15–54% had chronic health conditions (vs. 7–35%). All three types of OPPC were similar between groups, yet differed by time, use was lower during COVID-19. PCC score was higher among cancer survivors (mean 70 vs. 62). There were no differences by time period by gender, race/ethnicity, or education.
Prevalence of poor mental health
The prevalence of poor mental health increased from pre-COVID-19 to during COVID-19 in both cancer survivors (by 4.5%) and adults without a history of cancer (by 1.8%) (Fig. 1). During COVID-19, the prevalence of poor mental health during COVID-19 was similar for cancer survivors (41.9%) and adults without a history of cancer (40.2%). We observed the prevalence of poor mental health differed by sociodemographic and health status factors. Younger adults (35–49 years), females, least educated (less than high school), unmarried, those with low income (<$50,000), had Medicaid, had fair/poor health condition, had a chronic disease, or used a tablet/smartphone to communicate with providers had higher than the average prevalence of poor mental health in both groups and time periods (Supplement Table 1).
Impact of early COVID-19 on mental health
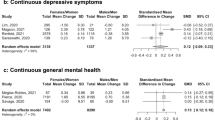
The D-I-D analysis revealed that the changes in poor mental health prior to and during COVID-19 among cancer survivors compared to adults without a history of cancer were not significantly different (Table 2), overall or stratified by PCC or online PPC. When we stratified by PPC (optimal vs. sub-optimal), we observed that the odds of poor mental health significantly increased from pre-COVID-19 to during COVID-19 in adults without a history of cancer among those who had optimal PCC (OR = 1.32, 95% CI 1.00–1.15). Among cancer survivors, there was also an increase among adults with optimal PCC, but it was not statistically significant (OR = 1.31, 95% CI 0.76–2.25).
Factors associated with poor mental health
We did not observe interactions of PCC or digital device use measures with either history of cancer or a time period. Therefore, Table 3 shows factors associated with poor mental health in a multivariable model with cancer survivors and adults without cancer during both time periods. In multivariable models, individuals who used email/internet (OR = 1.39, 1.20–1.60) or tablet/smartphones (OR = 1.39, 1.21–1.59) to communicate with providers were more likely to have poor mental health. The odds of poor mental health were not associated with EHR message use or PCC composite score. In addition, a history of cancer (OR = 1.04, 0.88–1.23 vs. no) and the early COVID-19 pandemic (OR = 1.09, 0.94–1.27 vs. pre-COVID-19 2017–2019) were not associated with poor mental health. However, other health conditions were associated with poor mental health. Those with excellent/good general health status (vs. fair poor) were less likely to have poor mental health. Adults with chronic lung disease (OR = 1.72, 1.47–2.02) were 1.7 times as likely to have poor mental health than those without chronic lung disease.
Demographic factors associated with poor mental health included younger populations (ORs = 1.98–3.25; 18–64 vs. ≥75 years) and females (OR = 1.59, 1.39–1.80). Non-Hispanic Black/African Americans (OR = 0.62, 0.51–0.75), Hispanics (OR = 0.68, 0.56–0.82), and non-Hispanic Asians (OR = 0.54, 0.39–0.75) were less likely to have poor mental health than non-Hispanic White populations. More educated individuals (OR = 0.72, 0.56–0.94 college graduate or more vs. less than high school) were less likely to have poor mental health. Individuals with the lowest income (<$20,000) were approximately 2-3 times as likely to have poor mental health than those with higher income. Sensitivity analyses revealed that the factors associated with psychological distress and chronic depression were similar to poor mental health, except for PCC and EHR OPPC (Table 3). The odds of psychological distress decreased by 2% per 10-unit PCC composite score increase, while the odds of chronic depression status increased by 5% per 10-unit PCC score increase. Using EHR to communicate with providers was associated with chronic depression (OR = 1.22, 1.03–1.46), but no association was shown with poor mental health.
Discussion
We examined the impact of COVID-19 and cancer survivorship on poor mental health and factors associated with poor mental health prior to and during the early COVID-19 pandemic using a nationally representative survey. The prevalence of poor mental health increased to a similar extent in both those with and without a history of cancer from pre-pandemic to early COVID-19, where the prevalence was high at approximately 40%. However, neither the COVID-19 pandemic nor cancer survivorship was associated with poor mental health during the early COVID-19 in the U.S. Notably, we found that OPPC use (email/internet and tablet/smartphone) was significantly associated with poor mental health, suggesting that active digital device users might be those who need mental health supports. In addition, our study identified subgroups of adults, defined by sociodemographic (younger age, females, lower income/education) and clinical (chronic lung disease or poor general health) factors, who were more likely to experience poor mental health. Our findings shed light on populations more likely to experience poor mental health and opportunities for targeted interventions to prevent further mental health inequities in the U.S.
Our findings showed that the prevalence of poor mental health increased during COVID-19 to a similar degree among cancer survivors and those without a history of cancer. Our findings of an increase in poor mental health aligned with the longitudinal study (2014–2020) among breast cancer survivors 60 years and older and adults without a history of cancer from 5 U.S. regions27. Despite the previous concerns that COVID-19-related situations (e.g., delayed cancer care, fear of disease progression) would disproportionately impact the mental health status of cancer survivors during COVID-1945,46, the prevalence did not differ between cancer survivors and those without a history of cancer. This highlights that there were concerns that might have led to poorer mental health in those without a history of cancer as well. Our findings of a high prevalence of poor mental health among U.S. adults during the early pandemic align with the findings of a national survey in April 2020 that observed 52% had mild or severe depression21. Thus, our findings contribute to the evidence of the unusually high prevalence of poor mental health during the early pandemic that will need to be carefully monitored post-pandemic.
In our study, communication through email/internet and tablet/smartphone with health providers was associated with poor mental health after accounting for PCC quality and sociodemographic and clinical factors. The three types of digital devices we considered involve different levels of digital fluency and experience. Specifically, email/internet communications could refer to a lower and general level of digital fluency, whereas discussions with tablet/smartphone require a higher level of digital fluency. On the other hand, messaging via EHR, which was only associated with chronic depression, demands being digitally engaged with the healthcare system. In previous literature, those with poor mental health were more likely to seek online activities for health (e.g., participate in online health discussion forums, and watch health-related videos)47. Given OPPC could be a part of online activity, it is possible that those with existing poor mental health were engaged more in OPPC. However, this interpretation needs caution as it is also possible that heavy online activities, which could have increased OPPC as well, led to poor mental health48. Although we cannot confirm the directions of associations observed in this cross-sectional study, our findings signaled that digital device-based communications could be a tool and provide additional opportunities to care for individuals with mental distress. Suggested interventions could include related stakeholders (e.g., healthcare clinics and public health practitioners) widely informing the public about the available digital device-based communication channels for those with mental distress49. Potentially, social media could also play a role in the dissemination of relevant information and online communication options47.
We observed that sub-optimal PCC was associated with poor psychological distress, which aligned with previous findings among cancer survivors during COVID-1928. This may highlight the role of PCC as a potential channel to address psychological distress28. However, notably, more optimal PCC was associated with chronic depression in our study. While further studies are needed to understand the factors underlying this association, it might have related to more encounters with providers (e.g., for depression treatment or comorbidity care) among those with chronic depression, as frequent office visits have shown association with optimal PCC, previously37.
Consistent with prior studies21,25,26,50,51, we also found that lower education level and income were associated with poor mental health. Overall wealth also has been associated with resilience during COVID-19, with those with resilience having lower odds of depression and anxiety in a longitudinal study52. In addition, COVID-19 pandemic-related loss of employment income was associated with worsened mental health53. Multifaceted approaches will need to be considered to relieve the poor mental health of those with low SES and address the root cause of the issue in the long-term50. Approaches could include partnering with already available community programs (e.g., Special Supplemental Nutrition Program for Women, Infants, and Children, WIC) or local governments (e.g., State Employment Development Department, EDD) to reach out to those in need, including low-income families or those who experienced unemployment during the pandemic, to gauge the mental health care needs and design tailored mental health care interventions54,55.
We also found that younger individuals and females were more likely to have poor mental health, which aligned with the previous literature12,25,26. These consistent associations highlight the need for targeted interventions for younger individuals and females. A prior study found that younger individuals had a lower level of resilience and poor sleep quality, mediators for depression and anxiety symptoms, and were more vulnerable to perceived stress, which was strongly associated with depression and anxiety symptoms during COVID-1956. Evidence-based life skills training (e.g., support for stress management, resilience training, sleep quality improvement) may need to be considered. Moreover, we observed that non-Hispanic Whites were more likely to experience poor mental health than non-Hispanic Black/African Americans, Asians, and Hispanics. This is in contrast to prior findings that found Black/African Americans to have poorer mental health3,57,58. Previously, stressful life events, including health, financial, or job problems in the past 30 days, had stronger associations with depression among non-Hispanic White men than non-Hispanic Black/African Americans in a national survey59. Thus, it is possible that non-Hispanic Whites were more vulnerable to poor mental health during the early COVID-19 pandemic, although further investigations in the extended and post-pandemic period are warranted to determine whether these differences persist.
Last, those who had chronic lung disease were more likely to have poor mental health, a finding that has been reported previously and is likely related to the poor quality of life among those with chronic lung disease60,61. Similarly, we also observed that those with poor general health status were more likely to have poor mental health, which is consistent with a previous report that considered depression and anxiety among cancer survivors25. Given that COVID-19 is a respiratory infectious disease, which disproportionately affected those with compromised health status, our finding highlights a vulnerable group to target for improving mental health.
Our study has some limitations. First, we were not able to confirm the direction of associations with factors in mental health as we used cross-sectional survey data. Second, even though HINTS data are high-quality and national, they might have some inevitable weaknesses originated from self-reporting, including reporting bias. For example, people might not report mental distress intentionally (hesitancy) or unintentionally (lack of awareness or knowledge). Third, we were not able to account for other cancer-related clinical information (e.g., cancer status, recurrence) as the HINTS did not collect this information. Fourth, the COVID-19 (2020) sample size was smaller than the pre-COVID-19 (2017–2019) sample size, as 2020 was the only available COVID-19 data from the HINTS. Lastly, COVID-19 data were collected from February to June 2020, hence the findings will need to be interpreted in the context of the early pandemic.
Despite these limitations, this study is among the first studies, to our knowledge, that examined the impact of the COVID-19 pandemic and cancer survivorship on mental health taking into consideration patient-provider communication at the population-level. The associations of PCC quality and digital device use for patient-provider communications with mental health have been rarely studied in spite of its potential role in online mental health care. Thus, our findings serve as a basis for future studies examining the dynamics of online health activities, the quality of communication, and mental health, as the use of online tools become widespread in health care, including telehealth.
A high proportion of adults in our study experienced poor mental health prior to and during the early COVID-19 in the U.S., yet neither the pandemic, nor cancer survivorship was related. Instead, OPPC use and lower socioeconomic status showed strong associations with poor mental health. Our findings highlight the importance of targeted approaches for these vulnerable subgroups, such as through partnering with communities or local governments, involving related stakeholders, or applying life skills training.
Data availability
The data used for this study is publicly available at https://hints.cancer.gov/data/download-data.aspx.
Code availability
The code used to analyze the data is available from the corresponding author upon reasonable request.
References
Mental Health. https://www.who.int/en/news-room/fact-sheets/detail/mental-health-strengthening-our-response (accessed Mar 2023).
Mitchell, A. J., Ferguson, D. W., Gill, J., Paul, J. & Symonds, P. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol. 14, 721–732 (2013).
Parikh, R. B. et al. Long-term depression incidence and associated mortality among African American and White prostate cancer survivors. Cancer 127, 3476–3485 (2021).
Berchuck, J. E. et al. Association oF Mental Health Treatment with Outcomes for US veterans diagnosed with non-small cell lung cancer. JAMA Oncol. 6, 1055–1062 (2020).
Jarrett, N. et al. Informing future research priorities into the psychological and social problems faced by cancer survivors: a rapid review and synthesis of the literature. Eur. J. Oncol. Nurs. 17, 510–520 (2013).
Roland, K. B., Rodriguez, J. L., Patterson, J. R. & Trivers, K. F. A literature review of the social and psychological needs of ovarian cancer survivors. Psychooncology 22, 2408–2418 (2013).
Cancer Statistics-National Cancer Institute. https://www.cancer.gov/about-cancer/understanding/statistics (accessed Jan 2022).
Mols, F., Schoormans, D., de Hingh, I., Oerlemans, S. & Husson, O. Symptoms of anxiety and depression among colorectal cancer survivors from the population-based, longitudinal PROFILES Registry: Prevalence, predictors, and impact on quality of life. Cancer 124, 2621–2628 (2018).
Bhuiyan, N., Linden-Carmichael, A. N., Lanza, S. T., Schmitz, K. H. & Mama, S. K. Age-varying associations between physical activity and psychological outcomes among rural cancer survivors. J. Behav. Med. 44, 484–491 (2021).
Andrykowski, M. A., Steffens, R. F., Bush, H. M. & Tucker, T. C. Disparities in mental health outcomes among lung cancer survivors associated with ruralness of residence. Psychooncology 23, 428–436 (2014).
Burris, J. L. & Andrykowski, M. Disparities in mental health between rural and nonrural cancer survivors: a preliminary study. Psychooncology 19, 637–645 (2010).
Andrykowski, M. A. et al. Low socioeconomic status and mental health outcomes in colorectal cancer survivors: Disadvantage? advantage?⋯ or both? Psychooncology 22, 2462–2469 (2013).
Zachariae, R. et al. Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. Br. J. Cancer 88, 658 (2003).
Epstein, R. M. & Street, R. L. Patient Centered Communication in Cancer Care. Promoting Healing and Reducing Suffering. (U.S. Department of Health and Human Services, 2007).
Jiang, S. How does online patient-provider communication heal? Examining the role of patient satisfaction and communication experience in China. Health Commun. 34, 1637–1644 (2019).
McCue, M. et al. Mobile app to enhance patient activation and patient-provider communication in major depressive disorder management: collaborative, randomized controlled pilot study. JMIR Form. Res. 6. https://doi.org/10.2196/34923 (2022).
Roter, D. L., Larson, S., Sands, D. Z., Ford, D. E. & Houston, T. Can e-mail messages between patients and physicians be patient-centered? Health Commun 23, 80–86 (2008).
Wibe, T., Ekstedt, M., Hellesø, R., Varsi, C. & Ruland, C. ‘You are not at all bothersome’-nurses’ online communication with testicular cancer patients. NI 2012 11th Int Congr Nurs Informatics, June 23-27, 2012, Montr Canada Int Congr Nurs Informatics (11th 2012 Montr Quebec) 2012, 453 (2012).
Pfefferbaum, B. & North, C. S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 383, 510–512 (2020).
Salari, N. et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health 16, 1–11 (2020).
Ettman, C. K. et al. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open 3. https://doi.org/10.1001/JAMANETWORKOPEN.2020.19686 (2020).
Choobin, M. H. et al. The impact of COVID-19 outbreak on emotional and cognitive vulnerability in Iranian women with breast cancer. Front. Psychol. 12. https://doi.org/10.3389/FPSYG.2021.663310 (2021).
Ayubi, E., Bashirian, S. & Khazaei, S. Depression and anxiety among patients with cancer during COVID-19 pandemic: a systematic review and meta-analysis. J. Gastrointest. Cancer 52, 499–507 (2021).
Han, J., Zhou, F., Zhang, L., Su, Y. & Mao, L. Psychological symptoms of cancer survivors during the COVID-19 outbreak: a longitudinal study. Psychooncology 30, 378–384 (2021).
Adzrago, D. et al. Assessment of anxiety/depression among cancer patients before and during the COVID-19 pandemic. Psychooncology 31, 1681–1691 (2022).
Islam, J. Y., Vidot, D. C. & Camacho-Rivera, M. Evaluating mental health–related symptoms among cancer survivors during the COVID-19 pandemic: an analysis of the COVID impact survey. JCO Oncol. Pract. 17, e1258 (2021).
Rentscher, K. E. et al. Loneliness and mental health during the COVID-19 pandemic in older breast cancer survivors and noncancer controls. Cancer 127, 3671–3679 (2021).
Street, R. L. et al. Managing uncertainty and responding to difficult emotions: cancer patients’ perspectives on clinician response during the COVID-19 pandemic. Patient Educ. Couns. 105, 2137–2144 (2022).
Zhou, X. et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed. J. E. Health 26, 377–379 (2020).
Backhaus, A. et al. Videoconferencing psychotherapy: a systematic review. Psychol. Serv. 9, 111–131 (2012).
Bokolo, A. J. Application of telemedicine and eHealth technology for clinical services in response to COVID‑19 pandemic. Health Technol. (Berl) 11, 359–366 (2021).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann. Intern. Med. 147, 573–577 (2007).
Survey Instruments | HINTS. https://hints.cancer.gov/data/survey-instruments.aspx (accessed Aug 2021).
Westat. Health Information National Trends Survey 5 (HINTS 5) Cycle 4 Methodology Report. (Westat, 2020).
Kroenke, K., Spitzer, R. L., Williams, J. B. W. & Löwe, B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics 50, 613–621 (2009).
Löwe, B. et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 122, 86–95 (2010).
Blanch-Hartigan, D. et al. Trends in cancer survivors’ experience of patient-centered communication: results from the Health Information National Trends Survey (HINTS). J. Cancer Surviv. 10, 1067–1077 (2016).
Spooner, K. K., Salemi, J. L., Salihu, H. M. & Zoorob, R. J. Disparities in perceived patient-provider communication quality in the United States: trends and correlates. Patient Educ. Couns. 99, 844–854 (2016).
Jiang, S., Hong, Y. A. & Liu, P. L. Trends of online patient-provider communication among cancer survivors from 2008 to 2017: a digital divide perspective. J Cancer Surviv. 13, 197–204 (2019).
Social Determinants of Health-Healthy People 2030 | health.gov. https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed Aug 2021).
Cohen, S. A., Kunicki, Z. J., Nash, C. C., Drohan, M. M. & Greaney, M. L. Rural-Urban differences in caregiver burden due to the COVID-19 pandemic among a National Sample of Informal Caregivers. Gerontol. Geriatr. Med. 7. https://doi.org/10.1177/23337214211025124 (2021).
Dimick, J. B. & Ryan, A. M. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA 312, 2401–2402 (2014).
Perneger, T. V. What’s wrong with Bonferroni adjustments. BMJ 316, 1236–1238 (1998).
Rothman, K. J. No adjustments are needed for multiple comparisons-PubMed. Epidemiology. https://pubmed.ncbi.nlm.nih.gov/2081237/ (accessed Mar 2023).
Soriano, E. C. et al. Psychosocial impact of cancer care disruptions in women with breast cancer during the COVID-19 pandemic. Front. Psychol. 12. https://doi.org/10.3389/FPSYG.2021.662339 (2021).
Chen, G. et al. Fear of disease progression and psychological stress in cancer patients under the outbreak of COVID-19. Psychooncology 29, 1395–1398 (2020).
Ye, J., Wang, Z. & Hai, J. Social networking service, patient-generated health data, and population health informatics: national cross-sectional study of patterns and implications of leveraging digital technologies to support mental health and well-being. J. Med. Intern. Res. 24. https://doi.org/10.2196/30898 (2022).
Robbins, R. et al. Digital communications technology use and feelings of anxiety, depression, and loneliness among older adults during the COVID-19 pandemic. J. Appl. Gerontol. https://doi.org/10.1177/07334648231169086/ASSET/IMAGES/LARGE/10.1177_07334648231169086-FIG1.JPEG (2023).
Nahum-Shani, I. et al. Just-in-Time Adaptive Interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann. Behav. Med. A Publ. Soc. Behav. Med. 52, 446 (2018).
Zare, H., Meyerson, N. S., Nwankwo, C. A. & Thorpe, R. J. How income and income inequality drive depressive symptoms in U.S. adults, does sex matter: 2005–2016. Int. J. Environ. Res. Public Health 19, 2005–2016 (2022).
Ettman, C. K., Cohen, G. H., Vivier, P. M. & Galea, S. Savings, home ownership, and depression in low-income US adults. Soc. Psychiatry Psychiatr. Epidemiol. 56, 1211 (2021).
Kimhi, S., Eshel, Y., Marciano, H., Adini, B. & Bonanno, G. A. Trajectories of depression and anxiety during COVID-19 associations with religion, income, and economic difficulties. J. Psychiatr. Res. 144, 389 (2021).
Huato, J. & Chavez, A. Household income, pandemic-related income loss, and the probability of anxiety and depression. East Econ. J. 47, 546 (2021).
Bolea, S. The courage to be anxious. Paul Tillich’s existential interpretation of anxiety. J. Educ. Cult. Soc. 6, 20–25 (2020).
Klawetter, S. et al. Perinatal depression in low-income women: a literature review and innovative screening approach. Curr. Psychiatry. Rep. 22, 1–8 (2020).
Varma, P., Junge, M., Meaklim, H. & Jackson, M. L. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog. Neuropsychopharmacol. Biol. Psychiatry 109, 110236 (2021).
Assari, S. Race, depression, and financial distress in a nationally representative sample of american adults. Brain Sci. 9. https://doi.org/10.3390/BRAINSCI9020029 (2019).
Matthews, T. A. et al. Associations of COVID-19 related work stressors with psychological distress: racial and ethnic disparities in Californian workers. Int. J. Environ. Res. Public Heal. 2023 20, 144 (2022).
Assari, S. & Lankarani, M. M. Association between stressful life events and depression; intersection of race and gender. J. Racial Ethn. Heal. Disparities 3, 349–356 (2016).
Goodwin, R. D., Chuang, S., Simuro, N., Davies, M. & Pine, D. S. Association between lung function and mental health problems among adults in the United States: findings from the First National Health and Nutrition Examination Survey. Am. J. Epidemiol. 165, 383–388 (2007).
Hanania, N. A. et al. Improvement in lung function and patient-reported outcomes in patients with COPD with comorbid anxiety and depression receiving nebulized glycopyrrolate in the GOLDEN 3 and 4 studies. Int. J. Chron. Obstruct. Pulmon. Dis. 16, 865–875 (2021).
Acknowledgements
Funding information and the role of the funders: T.H.K.’s time was supported, in part, by the UC Davis Comprehensive Cancer Center and National Cancer Institute of the National Institutes of Health under award number P30CA093373. E.L. is supported by the National Institutes of Health: Mid-career Investigator Award in Patient-Oriented Research (K24AR075060) and Research Project Grant (R01AR082109). M.S.D. was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR001860 and linked award KL2 TR001859. These funding sources did not have any roles in study design, in the collection, analysis, and interpretation of data, in the writing of the report, and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
J.K. conceived and J.K. and T.H.K. designed the study. J.K. prepared the materials, curated the data, and analyzed the data, and T.H.K. contributed to the data analysis. J.K. and T.H.K. primarily interpreted the results and M.S.D. and E.L. contributed to data interpretation. J.K. drafted the first manuscript, J.K. and T.H.K. revised the previous versions of the manuscript, and M.S.D., E.L., and J.S.H. reviewed and revised the manuscript until the final. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, J., Linos, E., Dove, M.S. et al. Impact of COVID-19, cancer survivorship and patient-provider communication on mental health in the US Difference-In-Difference. npj Mental Health Res 2, 14 (2023). https://doi.org/10.1038/s44184-023-00034-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44184-023-00034-x