Abstract
Methyl-CpG-binding protein 2(MeCP2) is an important epigenetic regulatory factor that promotes many tumor developments, such as liver cancer, breast cancer, and colorectal cancer. So far, no pan-cancer analysis has been reported. Therefore, this study aims to explore pan-cancer's prognostic value, immune infiltration pattern, and biological function. We used bioinformatics methods to analyze the expression and prognostic significance of MeCP2, and the relationship between MeCP2 and clinicopathological parameters, genetic variation, methylation, phosphorylation, immune cell infiltration, and biological function in pan-cancer from using a public database. The results showed that expression of MeCP2 was up-regulated in 8 cancers and down-regulated in 2 cancers, which was remarkably correlated with the prognosis, pathological stage, grade and subtype of cancers. The promoter methylation level of MeCP2 DNA was decreased in bladder urothelial carcinoma (BLCA), breast invasive carcinoma (BRCA), liver hepatocellular carcinoma (LIHC), prostate adenocarcinoma (PRAD), uterine corpus endometrial carcinoma (UCEC), testicular germ cell tumors (TGCT), and stomach adenocarcinoma (STAD);decreased phosphorylation of S25, S90, S92, S241, S286, S325 and S435 was found in MeCP2, such as UCEC, lung adenocarcinoma (LUAD), ovarian serous cystadenocarcinoma (OV), colon adenocarcinoma (COAD), and kidney renal clear cell carcinoma (KIRC). Furthermore, MeCP2 expression was significantly associated with multiple immunomodulators and immune cell infiltration levels across most tumors. Therefore, our pan-cancer explored the prognostic markers and immunotherapeutic value of MeCP2 in different cancers.
Similar content being viewed by others
Introduction
Worldwide, the incidence and mortality of cancer are increasing rapidly year by year. According to World Health Organization (WHO) annual report, there are an estimated 19.3 million new cancer cases and nearly 10 million cancer deaths in the world in 2020, which is the leading cause of human death1. At present, although the clinical treatment of tumors mainly improves the survival of tumor patients through surgery combined with radiotherapy, chemotherapy, immunotherapy and targeted drug therapy, the cytotoxicity and drug resistance caused by side effects in the treatment process still make the survival rate of patients low1,2. Notably, early diagnosis and treatment of tumors can effectively improve the prognosis of patients3. Therefore, there is an urgent need for a novel diagnostic marker and therapeutic target molecule for cancer patients.
Methyl-CpG-binding protein 2(MeCP2) is an X-linked gene, belonging to one of the members of methyl CpG binding domain (MBD) family members. The structure contains MBD and transcriptional repression domain (TRD), which can inhibit or promote gene transcription4,5. Previous studies found that MeCP2, as a new oncogene, was amplified in cancer cell lines and played a role in tumor cell proliferation, cell cycle, apoptosis, and invasion in several cancer types, such as osteosarcoma and gastric cancer6,7,8. Notably, HDAC inhibitor-mediated MeCP2 can be used in the treatment of tumors. For example, HDAC inhibitor sodium butyrate-treated HeLa cells to induce global genomic histone acetylation, significantly reducing MeCP29,10,11. Additionally, pan-cancer analysis based on public databases can reasonably identify the common characteristics and heterogeneity of tumors, determine the biological functions of some genes in tumors, and provide new therapeutic targets for patient treatment12,13,14. Therefore, through pan-cancer analysis, it is found that the detection of HER2 can benefit from the precise diagnosis and targeted therapy of head and neck squamous cell carcinoma (HNSC), non-small cell lung cancer (NSCLC), (CESC), BLCA, and UCEC15.
In this study, the expression of MeCP2 and its prognostic value were analyzed by bioinformatics. Additionally, the effects of MeCP2 expression on tumor mutation load (TMB) and microsatellite instability (MSI) were analyzed, along with DNA methylation, protein phosphorylation, and immune cell infiltration in human tumors. Protein‑protein interaction (PPI), Gene Ontology (GO), Kyoto Encyclopedia of Genes and Genomes (KEGG) and gene set enrichment analysis (GSEA)analysis explore the biological function of MeCP2 in tumors, as demonstrated by the workflow of this study (Fig. 1). Collectively, the results of this study provide new insights for precise cancer diagnosis and targeted immunotherapy.
Methods
MeCP2 expression and prognostic values analysis
The Oncomine database (https://www.oncomine.org/resource/login.html) is an online platform for cancer microarray database and comprehensive data mining16, which is used to analyze the expression of MeCP2 in different types of tumor tissues and normal tissues (P value is 0.001, fold change is 1.5, and gene ranking of all). The expression of MeCP2 in various immune cells of blood was analyzed by the HPA database (http://www.proteinatlas.org/). The expression level of MeCP2 mRNA in pan-cancer and its correlation with clinicopathological parameters were analyzed using data obtained from the Cancer Genome Atlas (TCGA) (https://xena.ucsc.edu). All databases were accessed in January 2022. The expression, tumor stage, histological grade, and survival analysis are based on “ggplot2”,“survival”,“ggcorrplot”, “coxph”, and “forestplot”packages. A comparison of expression and regression analysis was performed with ANOVA. The survival analysis was evaluated using the Kaplan–Meier method and log-rank test. The COX analysis was used to explore the relationship between the expression of MeCP2 and the prognosis of pan-cancer. The P value < 0.05 was considered statistical significance.
MeCP2 genetic alteration analysis
MeCP2 genetic alteration analysis in pan-cancer was performed using cBioPortal (https://www.cbioportal.org/), a public database for visualizing and analyzing multidimensional cancer genomics data, accessed in January 2022. MeCP2 alterations data was downloaded from the cBioPortal online database to analyze the alterations of MeCP2 in Pan-cancer and its relationship with tumor mutation burden (TMB), Microsatellite Instability (MSI), and prognosis. Spearman's method performed a correlation analysis between cancer gene expression and TMB or MSI. P < 0.05 was considered to indicate a statistically significant difference.
MeCP2 epigenetic modification analysis
The UALCAN database (http://ualcan.pathuab.edu/analysis.html) contains 31 kinds of tumor RNA sequences and clinicopathological parameter data. By analyzing cancer omics data, we can deeply analyze the expression of Pan oncogenes17. In this study, the UALCAN database was used to analyze the methylation level and protein phosphorylation level of the MeCP2 promoter region in normal and cancer tissues, accessed in January 2022. The significance of differences was evaluated using a student’s t-test, in which P < 0.05 was considered significant (*P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.005, ns: P > 0.05).
MeCP2 immune mechanism analysis
We used the “pan-cancer”module in the Assistant for Clinical Bioinformatics online tool (https://www.aclbi.com/) to analyze the association between MeCP2 expression and tumor immune infiltration with data from the XCELL database. The TISIDB database (http://cis.hku.hk/TISIDB/index.php) can integrate various heterogeneous data types and can be used to explore the interaction of specific genes in different tumors-immune18. The relationship between MeCP2 expression and immunological modulators (immunosuppressants, immunostimulators, and MHC molecules), immune subtype, and molecular subtype were explored through the TISIDB database (P < 0.05 as a cut-off value). The Wilcox test performed two-group data, in which P values less than 0.05 were considered statistically significant, and all databases were accessed in 2022.
Functional and pathway of MeCP2 enrichment analysis
The STRING datasets (https://string-db.org/) were applied to assess the functional interaction between proteins and further understand the occurrence or development mechanism of diseases19. Subsequently, the PPI network of MeCP2 was constructed via the STRING database (minimum required interaction score: low confidence (0.150), max number of interactors to show: no more than 50 interactors). The GEPIA2 database (http://gepia2.cancer-pku.cn/) was used for similar gene detection of MeCP2. The top 50 similar genes of MeCP2 performed Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis in DAVID (http://david.abcc.ncifcrf.gov/). According to the threshold of significance set as P < 0.05, the top 5 GO domains (BP: biological process; MF: molecular function; CC: cellular component) and 6 KEGG pathways were identified. KEGG pathway enrichment analysis of MeCP2 was performed using GSEA software (iz), and the threshold was set at P < 0.05. The threshold was set at P < 0.05. A P < 0.05and a count > 2 were considered the threshold for significant differences, accessing all databases in 2022.
Results
MeCP2 expression in tissue and blood immune cells
To explore MeCP2 expression in multiple tumors and normal tissue types, we examined MeCP2 expression via the Oncomine database. The results indicated that MeCP2 expression was higher in the brain, esophageal, kidney, leukemia, lung, and lymphoma cancer, compared to the normal tissues, and lower expression in other different types of cancers, such as brain, breast leukemia, ovarian, and prostate cancers (Fig. 2A). Analysis of MeCP2 mRNA expression level between the tumor and adjacent normal tissues in TCGA database. MeCP2 expression was significantly upregulated in 8 cancers, including BRCA, CHOL, COAD, ESCA, HNSC, KICH, LIHC, and STAD, down-regulated in KIRP, PRAD, and THCA, P < 0.05 for all (Fig. 2B). The detail of 33 cancers abbreviations are available in Fig. S1. To further evaluate MeCP2 expression in various blood immune cells, we used the HPA databases. The analysis of immune cell type and lineage specificity showed that MeCP2 expression was enhanced in immune cells (basophils) and lineage-enriched cells (granulocytes; Fig. 2C).
The expression level of the MeCP2 gene in tumors and blood immune cells. (A) The expression level of MeCP2 in various cancer tissues compared with normal tissues in the Oncomine database. (B) The expression level of MeCP2 in various cancer tissues compared with normal tissues from the TCGA database. (C) The expression level of MeCP2 in various blood immune cells was obtained from the HPA dataset.
Correlation analysis between MeCP2 expression and clinicopathological parameters
To better understand the clinical value of MeCP2 expression in pan-cancer, we used the TCGA database to study the relationship between MeCP2 expression and clinicopathological parameters of tumor patients. High expression of MeCP2 was associated with tumor stage in cancers including CHOL, HNSC, KIRC, LIHC, and PAAD (P < 0.05) (Fig. S2A) and linked to histological grade in HNSC, KIRC, LGG, and STAD (P < 0.05) (Fig. S2B). Additionally, as shown in Fig. S2C, MeCP2 expression has significant correlations with cancer subtypes in most cancers, such as ACC, BRAC, COAD, PCPG, LGG, PRAD, STAD, OV, HNSC, and UCEC (P < 0.05).
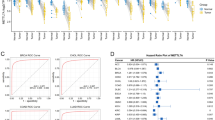
Moreover, the correlation analysis showed that MeCP2 expression had different prognostic values in various types of cancers (Fig. 3). High MeCP2 expression was associated with better overall survival (OS) in certain forms of cancers (BLCA, CESC, KIRC, MESO, LUAD, SARC, STAD, PAAD and UCEC), and worse OS in cancers (ACC, BRCA, DLBC, KICH, LIHC, LGG, HNSC, PRAD, THCA, UVW, COAD, and LAML), P < 0.05 for all (Fig. 3A). For disease-specific survival (DSS) outcomes, highly expressed MeCP2 was correlated with a better prognosis of DSS for cancers of BLCA, CESC, KIRC, LUAD, MESO, and UCEC, and was linked with poor prognosis of DSS for cancers of ACC, COAD, HNSC, KICH, LIHC, LUSC, SKCM, THCA, and UVW, P < 0.05 for all (Fig. S3A). For progression-free interval (PFI) better outcome, a positive association was apparent between high MeCP2 expression and PFI in CESC, KIRC, STAD, TGCT, and UCEC. In contrast, a negative association was noted in ACC, BRCA, CHOL, LGG, LIHC, LUSC, and UVW, P < 0.05 for all (Fig. S3B).
Correlation between MeCP2 gene expression and survival prognosis of pan cancers. (A) Survival curves of the relationship between MeCP2 Expression and OS in Pan-cancer. (P < 0.05). (B) The forest plots of Cox regression analyses MeCP2 Expression and Survival (OS, DFI, PFI, and DSS) (P < 0.05). OS overall survival, DFI disease free interval, PFI progression-free interval, DSS disease-specific survival, HR hazard ratio.
For disease-free interval (DFI) outcome, the better DFI in HNSC, KICH, LGG, OV, SARC, and TGCT were shown to correlate with higher MeCP2 expression, and low MeCP2 expression was related to better DFI in ACC, BRCA, COAD, KIRP, LUSC, and PCPG, P < 0.05 for all (Fig. S3C). We also used COX methods to analyze the relationship between MeCP2 and survival (OS, DFI, PFI, and DSS) for further validation. According to the forest plots (Fig. 3B), MeCP2 expression acted as a protective prognostic factor (HR < 1, P < 0.05) in CESC (OS), KIRC (OS, DSS, and PFI), and CESC (DSS). MeCP2 expression was considered a risk factor (HR > 1, P < 0.05), namely BRCA (OS), LUSC (PFI and DSS), LGG (OS and DSS), and KIRP (DFI and PFI).
Relationship between MeCP2 expression and genetic alteration
We investigated the MeCP2 alteration status of Pan cancers from the cBioPortal database. We found that the highest frequency of MeCP2 alteration was associated with amplification, deep deletion, and mutation. As shown in Fig. 4A, diffuse large B-cell lymphoma had the highest frequency of MeCP2 alterations, including amplification and deep deletion (> 10%), followed by stomach adenocarcinoma (> 6%) and uterine corpus endometrial carcinoma (> 6%). The main type of MeCP2 alteration is missense mutations (89), and R255*/Q was detected in UCEC (n = 2) and LSCC (n = 1) (Fig. 4B). Additionally, MeCP2 mutation was significantly correlated with MSI sensor score (10,054 samples) and mutation count (10,105 samples) in the TCGApan-cancer Atlas Studies (P < 0.0001) (Fig. 4C,D). The results of Fig. 4E–H showed that altered MeCP2 in UCEC had a better prognosis in disease-specific survival (P = 0.0306) than patients in the unaltered group but disease-free (0.942) overall survival (P = 0.0724) and progression-free survival (P = 0.055) were not different between the two groups. Hence, we investigated the relationship between MeCP2 expression and TMB/MSI in different types of cancer. Our results indicated that MeCP2 expression has significant negative correlations with TMB in STAD, UCEC, BRCA, and KIRC (P < 0.05) (Fig. 4I). Finally, we also found that MeCP2 expression has significant negative correlations with MSI in STAD and DLBC while positively correlated with that of ADD, LUAD, and LUSC (P < 0.05) (Fig. 4J).
Genetic alterations of MeCP2 in a variety of tumor types. (A) The alteration frequency of MeCP2 in different cancers. (B) The mutation site of the MeCP2 gene. (C,D) The correlation of MeCP2 mutation with MSI sensor score and Mutation count (P < 0.0001). (E,F) The correlation between MeCP2 mutation and Disease Free, Disease Specific (P < 0.05), Overall survival, and Progression Free. (I–J) Radar chart displays the correlation between MeCP2 and both TMB andMSI. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. TMB tumor mutational burden, MSI microsatellite instability.
MeCP2 DNA methylation and protein phosphorylation analysis
DNA methylation and protein phosphorylation directly affect the occurrence and progression of cancer. Using the UALCAN database, we analyzed DNA methylation and protein phosphorylation of MeCP2 in cancers. The results demonstrated that the promoter methylation level of MeCP2 was greatly decreased in BLCA, BRCA, LIHC, PRAD, TGCT, and STAD tissues, while increased in UCEC tissues compared to normal tissues (P < 0.05) (Fig. 5A). The schematic diagram of MeCP2 phosphorylation sites is displayed in Fig. 5B. Lower levels of phosphorylation of MeCP2 were observed in OV (S92, S241, and T491), KIRC (S325), COAD (S92, S286, and T491), UCEC (S25, S92, S286, and S435), and LUAD (S90, S92, S435, and T491) compared to normal samples (all P < 0.05) (Fig. 5C). The levels of phosphorylation of MeCP2 were no different in BRCA (S90, S92, and S241), and KIRC (S25, S90) (Fig. 5C).
DNA methylation and Phosphorylation analysis of MeCP2protein in several tumors via UALCAN database. (A) DNA Promoter methylation level of MeCP2 in BLAC, BRCA, LIHC, PRAD, TGCT and UCEC. (B) The schematic diagram of MeCP2 protein phosphoprotein sites. (C) The phosphorylation of MeCP2 protein was analyzed in BRCA, OV, KIRC, COAD, UCEC, and LUAD. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001, ns:no significance.
Association of MeCP2 expression and immune infiltration
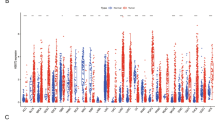
The level of tumor immune infiltration is essential for the survival and immunotherapy of cancer patients. Therefore, we investigated the correlations between MeCP2 expression and immune infiltration levels in 33 cancers using the XCELL database with Assitant for Clinical Bioinformatics online tool. As shown in Fig. 6A, MeCP2 expression was negatively correlated with the stromal score in GBM, LGG, and PCPG and positively correlated with the stromal score in BRCA, COAD, HNSC, KIRC, LAML, PAAD, and STAD (P < 0.01). In addition, MeCP2 expression negatively relates to immune scores in BRCA, GBM, KICH, SARC, SKCM, KIRC, KIRP, LAML, LGG, UCEC, LUSC, PCPG, THCA, and THYM, and positively relates to immune score in DLBC and PAAD (P < 0.05; Fig. 6A). We also analyzed the correlation between MeCP2 expression and 38 subtypes of immune cells, and the results indicated that MeCP2 expression negatively and significantly correlated with most subtypes in KIRC, KICH, KIRP, LUSC, SARC, SKCM, THCA, THYM, and UCEC, and the expression of MeCP2 were positively and significantly associated with levels of T cell NK, Th1, Th2, M1, M2, B cell plasm, T cell CD4 + central memory, and dendritic cells (all P < 0.05; Fig. 6A).
Correlation analysis between MeCP2 expression and immune infiltration. (A) The MeCP2 expression correlated with the infiltration levels of various immune cells. (B) The MeCP2 expression correlated with the immune inhibitors. (C) The MeCP2 expression correlated with the immune stimulators. (D) The MeCP2 expression correlated with the MHC molecules. Dot plots displayed the top1 strongest positive correlation. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
Furthermore, we explored the correlation between MeCP2 expression and three kinds of immunomodulators (immune inhibitor, immunostimulator, and MHC molecule) in cancers via the TISIDB database. Figure 6B shows MeCP2 expression negatively correlated with immune inhibitors in KICH, MESO, and UCEC and positively correlated with immune inhibitors in PCPG (P < 0.05). The correlation analyses of immune stimulators indicated that MeCP2 expression was positively associated with PVR in KICH (P < 0.05: Fig. 6C). The correlation of MeCP2 expression with MHC molecule was also investigated, UVW, UCS, TGCT, and OV exhibited positive correlations, and KICH, KIRP, LGG, BRCA, and THCAexhibited negative correlation (P < 0.05; Fig. 6D). Immune subtypes include wound healing (C1), IFN-γ dominant (C2), inflammatory (C3), lymphocyte depletion (C4), immunologically quiet (C5), and TGF-β dominant (C6). We also found a significant correlation between MeCP2 expression and immune subtypes in most cancers, such as BLCA, BRCA, COAD, HNSC, LGG, LIHC, LUAD, LUSC, KIRC, KIRP, OV, PAAD, PRAD, SARC, PCPG, THCA, STAD and UCEC (P < 0.05; Fig. S4).
PPI, GO, KEGG and GSEA enrichmen analysis of MeCP2-related gene
Considering the robust correlation between the expression of MeCP2 and the analysis results of immune infiltration, TMB, and MSI in STAD, related functional enrichment analyses of MeCP2 were performed via PPI, GO, KEGG and GSEA. Using the STRING online tool, we obtained 50 MeCP2-binding proteins (PPI enrichment p-value < 0.05), which have been verified by experiments (Fig. 7A). The top 50 similar genes of MeCP2 were obtained from the GEPIA2 database (all PCC > 0.4:Fig. 7B). By combining the similar genes of MeCP2 and MeCP2-binding proteins, GO, and KEGG pathway enrichment analysis were performed using the DAVID database. The top 15 GO terms are displayed in Fig. 7C. The results indicated that MeCP2-related genes mainly correlated with the biological processes (BP), cellular component (CC), and molecular function (MF), such as transcription factor binding, DNA binding, protein binding, transcriptional repressor complex, positive or negative regulation of transcription DNA templated, and positive or negative regulation of transcription from RNA polymerase II promote (P < 0.05). KEGG signaling pathway analysis results revealed that most of these genes were mainly enriched in transcriptional misregulation in cancer, alcoholism, thyroid hormone signaling pathways, Huntington's disease, pathways in cancer, and viral carcinogenesis (P < 0.05; Fig. 7D).
Enrichment analysis of MeCP2-related genes. (A) PPI network analysis of MeCP-binding proteins based on STRING database. (B) The top 50 similar genes of MeCP2 using the GEPIA2 online tool. (C) GO enrichment analysis of MeCP2-related genes. (D) KEGG pathway enrichment analysis of MeCP2-related genes. PPI protein–protein interaction, PCC Pearson correlation coefficient, GO Gene Ontology, BP biological process, CC cell component, MF molecular function, KEGG Kyoto Encyclopedia of Genes and Genomes.
To further explore the complex functions of MeCP2 in STAD, the MeCP2 mRNA data of TCGA were analyzed using GSEA analysis of KEGG pathways. The KEGG enrichment analysis results indicated that the high MeCP2 group demonstrated significant positive enrichment in KEGG_BASAL_CELL_CARCINOMA, KEGG_MTOR_SIGNALING_PATHWAY, WNT_SIGNALING_PATHWAY, KEGG_MAPK_SIGNALING_PATHWAY, KEGG_HEDGEHOG_SIGNALING_PATHWAY, and KEGG_PATHWAYS_IN_CANCER (all P < 0.05;Fig. S5A). In contrast, the low MeCP2 group demonstrated significant enrichment in KEGG_PROTEASOME,
KEGG_AMINOACYL_TRNA_BIOSYNTHESIS, and KEGG_SPLICEOSOME (all P < 0.05;Fig. S5B).
Discussion
Pan-cancer research can cross the boundaries between tumor types and provide new intervention strategies for clinical trials. Notably, pscreening pan-cancer biomarkers in blood or other body fluids has become a useful, routine, and economic screening tool for better understanding the role of these biomarkers12,20. Until recently, the function of MeCP2 in tumor progression has not been extensively studied nor well understood. Although not clearly understood, many studies have shown that MeCP2 can promote tumor progression and metastasis,such as breast cancer,liver cancer,and colorectal cancer5,21,22. To better understand the mechanism of MeCP2 in different tumors,we used a series of bioinformatics methods to comprehensively analyze the molecular features of gene expression,genetic alteration,epigenetic modification,and the relationship between MeCP2 expression and survival,TMB,MSI,and immune infiltration in 33 tumor types.
In this study,we first investigated the level of MeCP2 in tissues and blood, combing Oncomine,TCGA,and HPA databases MeCP2 was significantly upregulated in BRCA,CHOL,COAD,E SCA, HNSC, KICH, LIHC, and STAD, but low expression in KIRP, PRAD, and THCA compared with normal tissues (Fig. 2B). In blood immune cells, the MeCP2 lineage is enriched in granulocytes and highly expressed in basophils (Fig. 2C). Interestingly, increased MeCP2 expression is associated with tumor stage, histological grade, and tumor subtype in STAD, HNSC, KIRC, and LGG (Fig. S2). Similar results have also indicated that high MeCP2 expression can promote the proliferation and metastasis of tumor cells, such as gastric cancer, colorectal cancer, and renal cell carcinoma8,22,23,24. Additionally, MeCP2 expression was positively and significantly correlated with the TNM stages, subtypes, and histological types of gastric and breast cancer25,26. Furthermore, we found that high MeCP2 expression was correlated with a worse prognosis of OS, DSS, PFI, and DFI in ACC, BRCA, COAD, LIHC, and UVW (Fig. 3A and Fig. S3), and MeCP2 expression served as a prognostic factor in some types of cancer, based on Cox analyses (Fig. 3B). Based on the above results, MeCP2 may be a potential prognostic biomarker for several cancer types and provide a new targeted treatment strategy for various tumor treatments.
Somatic mutations can cause developmental disorders, and the gradual accumulation of mutations in the body can induce cancer27. Specific gene mutations are important biomarkers of patient prognosis, which is beneficial in evaluating the effect of drug therapy in cancer patients28,29. MeCP2 has a high mutation frequency in diffuse large B-cell lymphomas, such as amplification and deep deletion (Fig. 4A). The main mutation site is R255*/Q in UCEC, and altered MeCP2 is linked to MSI sensor score, mutation count, and survival of disease-specific survival (Fig. 4B–H). It is reported that TMB is a biomarker of the pan-cancer genome, and the level of TMB is related to the production of immunogenic peptides and the efficacy of immune checkpoint inhibitors (ICIs). Additionally, a high level of TMB helps to improve the efficacy of ICIs and OS30,31,32,33. Our study found that MeCP2 expression was related to TMB of STAD, UCEC, BRCA, and KIRC and linked to MSI of STAD, DLBC, ADD, LUAD, and LUSC (Fig. 4I–J). However, TMB and MSI levels were associated with new antibody production, and TMB levels were elevated in patients with high microsatellite instability (MSI-H)13,34, findings consistent with previous experimental results. TMB is an important independent biomarker in MSI-H mCRC, which is used to stratify the possibility of patients' response to ICPIs and plays an essential role in patients' immunotherapy35. The high expression of MeCP2 in tumors is related to MSI and TMB, indicating that MeCP2 may be a valuable prognostic biomarker that will benefit immunotherapy and prolonged survival.
Epigenetics can regulate the occurrence and proliferation of cancer, and epigenetic modification is gradually regarded as the key target of tumor research that can better discover the mechanism of tumorigenesis and provide biomarkers for early detection, diagnosis, and treatment of tumor patients36. DNA methylation is a critical factor in regulating gene expression, and abnormal DNA methylation can lead to the occurrence and proliferation of cancer37. Low DNA methylation levels are remarkably linked to the high MeCP2 expression in BRCA, LIHC, and STAD (Fig. 5A). Previous studies have shown that DNA methylation is a well-characterized epigenetic hallmark of tumors, which can improve the efficacy of chemotherapy for gastric cancer and hepatocellular carcinoma38,39. In addition, protein phosphorylation is one of the main post-translational modifications (PTM), including almost all life processes, such as cell division, decomposition, signal transduction, gene expression regulation, and protein interaction. Consequently, mutations in protein phosphorylation sites can lead to tumorigenesis40,41. Interestingly, our study showed that the protein phosphorylation level of MeCP2 was decreased in most common cancers, the S241and S286 locus within the TRD in OV, COAD, and UCEC (Fig. 5B,C). A previous study found that the decreased level of phosphorylated PDK-S241 can regulate the protein phosphorylation of the cell cycle and affect the proliferation of prostate cancer42. Therefore, the relationship between MeCP2 expression, DNA methylation, and protein phosphorylation needs to be further verified by experiments in tumorigenesis.
To further study the potential value of MeCP2 in pan cancers, we explored the correlation between MeCP2 expression and immune cell infiltration and immunomodulators. MeCP2 expression was correlated with stromal score and immune score in most cancers, and it was significantly associated with levels of immune cells, such as T cell NK, Th1, M1, T cell CD4 + central memory, and dendritic cells (Fig. 6A). Similar results have reported the expression of PD-L1 can promote the strong immune response of tumor-infiltrating immune cells and is significantly correlated with the overall survival in ovarian cancer43. In most immune inhibitors, immunostimulators, and MHC molecules, MeCP2 expression was positively associated with CD274(PD-L1), PVR, and TAPBP (Fig. 6C). With the breakthrough of tumor-related immune inhibitors, immunostimulators, and MHC molecules, ICIs have been widely used in tumor immunotherapy and achieved remarkable results. Meanwhile, PD-1/PD-L1 ICIS has been approved as a drug for treating various malignant tumors, including melanoma, lymphoma, lung cancer, HNSC, KIRC, and LIHC30,44. Therefore, it is reasonable to speculate that MeCP2 expression may regulate the infiltration level of tumor immune cells and immune responses and ultimately affect the prognosis of tumor patients.
Additionally,100 MeCP2-related genes were performed for functional enrichment analysis in STAD. For the GO terms, MeCP2-related genes are mainly enriched in transcription factor binding, DNA binding, protein binding, regulation of transcription DNA templated, and regulation of transcription from RNA polymerase II (Fig. 7C). MeCP2 dysfunction leads to changes in the expression level of thousands of genes, about 15% inhibited and 85% activated. For example, MeCP2 recruitment of CREB1 can activate the transcription of downstream genes45. KEGG pathway enrichment analysis showed that MeCP2 was mainly enriched in pathways related to tumorigenesis, such as transcriptional misregulation in cancer and pathways in cancer. Interestingly, the GSEA results also showed that MeCP2 was significantly related to the signal pathway of tumorigeneses, such as KEGG_PATHWAYS_IN_CANCE, KEGG_BASAL_CELL_CARCINOMA, and WNT_SIGNALING_PATHWAY. Emerging evidence demonstrates that PI3K/AKT/mTOR signaling pathway is significantly correlated with the occurrence, prognosis, and metastasis of gastric cancer, and the PI3K/AKT/mTOR signaling pathway may be a molecular target and potential therapeutic strategy for the clinical diagnosis of gastric cancer46. However, further studies are needed to determine the mechanism of MeCP2 and these signaling pathways and to explore whether it can be used as an indicator of tumor diagnosis and prognosis.
Conclusions
In summary, the results of this study show that MeCP2 expression is significantly related to pathological stage, tumor grade, clinical prognosis, DNA methylation, protein phosphorylation, and immune cell infiltration in CHOL, HNSC, KIRC, LIHC, and STAD. In addition, MeCP2 expression is related to the status of immunotherapy-associated signatures. Therefore, MeCP2 can be used as a prognostic biomarker of pan-cancer and provide a new strategy for treating tumor ICIs.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 Countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 69(1), 7–34 (2019).
Nguyen, T. B., Do, D. N., Nguyen-Thanh, T., Tatipamula, V. B. & Nguyen, H. T. Identification of five hub genes as key prognostic biomarkers in liver cancer via integrated bioinformatics analysis. Biology (Basel). 10(10), 957 (2021).
Vieira, J. P. et al. Variant Rett syndrome in a girl with a pericentric X-chromosome inversion leading to epigenetic changes and overexpression of the MECP2 gene. Int. J. Dev. Neurosci. 46, 82–87 (2015).
Tong, D. et al. MeCP2 facilitates breast cancer growth via promoting ubiquitination-mediated P53 degradation by inhibiting RPL5/RPL11 transcription. Oncogenesis. 9(5), 56 (2020).
Meng, G., Lv, Y., Dai, H., Zhang, X. & Guo, Q. N. Epigenetic silencing of methyl-CpG-binding protein 2 gene affects proliferation, invasion, migration, and apoptosis of human osteosarcoma cells. Tumour Biol. 35(12), 11819–11827 (2014).
Neupane, M. et al. MECP2 is a frequently amplified oncogene with a novel epigenetic mechanism that mimics the role of activated RAS in malignancy. Cancer Discov. 6(1), 45–58 (2016).
Zhao, L. et al. MeCP2 promotes gastric cancer progression through regulating FOXF1/Wnt5a/β-catenin and MYOD1/caspase-3 signaling pathways. EBioMedicine 16, 87–100 (2017).
Yoshida, M. et al. Histone deacetylase as a new target for cancer chemotherapy. Cancer Chemother. Pharmacol. 48(Suppl 1), S20–S26 (2001).
Johnstone, R. W. Histone-deacetylase inhibitors: Novel drugs for the treatment of cancer. Nat. Rev. Drug Discov. 1(4), 287–299 (2002).
Ishibashi, T., Thambirajah, A. A. & Ausió, J. MeCP2 preferentially binds to methylated linker DNA in the absence of the terminal tail of histone H3 and independently of histone acetylation. FEBS Lett. 582(7), 1157–1162 (2008).
Cancer Genome Atlas Research Network, Weinstein JN, Collisson EA, et al. The Cancer Genome Atlas Pan-Cancer analysis project. Nat. Genet. 2013;45(10):1113–1120.
Liu, J. N. et al. An integrated pan-cancer analysis of TFAP4 aberrations and the potential clinical implications for cancer immunity. J. Cell Mol. Med. 25(4), 2082–2097 (2021).
Cancer Cell Line Encyclopedia Consortium; Genomics of Drug Sensitivity in Cancer Consortium. Pharmacogenomic agreement between two cancer cell line data sets. Nature. 2015;528(7580):84–87.
Li, Z. et al. A pan-cancer analysis of HER2 index revealed transcriptional pattern for precise selection of HER2-targeted therapy. EBioMedicine 62, 103074 (2020).
Rhodes, D. R. et al. Oncomine 3.0: Genes, pathways, and networks in a collection of 18,000 cancer gene expression profiles. Neoplasia 9(2), 166–180 (2007).
Chen, F., Chandrashekar, D. S., Varambally, S. & Creighton, C. J. Pan-cancer molecular subtypes revealed by mass-spectrometry-based proteomic characterization of more than 500 human cancers. Nat. Commun. 10(1), 5679 (2019).
Ru, B. et al. TISIDB: An integrated repository portal for tumor-immune system interactions. Bioinformatics 35(20), 4200–4202 (2019).
Li, L., Lei, Q., Zhang, S., Kong, L. & Qin, B. Screening and identification of key biomarkers in hepatocellular carcinoma: Evidence from bioinformatic analysis. Oncol. Rep. 38(5), 2607–2618 (2017).
Ching, T. et al. Pan-cancer analyses reveal long intergenic non-coding RNAs relevant to tumor diagnosis, subtyping and prognosis. EBioMedicine 7, 62–72 (2016).
Wang, L. et al. MeCP2 drives hepatocellular carcinoma progression via enforcing HOXD3 promoter methylation and expression through the HB-EGF/EGFR pathway. Mol. Oncol. 15(11), 3147–3163 (2021).
Luo, D. & Ge, W. MeCP2 promotes colorectal cancer metastasis by modulating ZEB1 transcription. Cancers (Basel). 12(3), 758 (2020).
Zhao, L. Y. et al. MeCP2, a target of miR-638, facilitates gastric cancer cell proliferation through activation of the MEK1/2-ERK1/2 signaling pathway by upregulating GIT1. Oncogenesis. 6(7), e368 (2017).
Liu, H. et al. Silencing miR-454 suppresses cell proliferation, migration and invasion via directly targeting MECP2 in renal cell carcinoma [published correction appears in Am J Transl Res. 2020 Nov 15;12(11):7620–7624]. Am. J. Transl. Res. 12(8), 4277–4289 (2020).
Zhang, J. et al. MECP2 expression in gastric cancer and its correlation with clinical pathological parameters. Medicine (Baltimore) 96(31), e7691 (2017).
Jiang, W. et al. MeCP2 inhibits proliferation and migration of breast cancer via suppression of epithelial-mesenchymal transition. J. Cell Mol. Med. 24(14), 7959–7967 (2020).
Martincorena, I. & Campbell, P. J. Somatic mutation in cancer and normal cells. Science 349(6255), 1483–1489 (2015).
Allegra, C. J. et al. Extended RAS gene mutation testing in metastatic colorectal carcinoma to predict response to anti-epidermal growth factor receptor monoclonal antibody therapy: American society of clinical oncology provisional clinical opinion update 2015. J. Clin. Oncol. 34(2), 179–185 (2016).
Sanz-Garcia, E., Argiles, G., Elez, E. & Tabernero, J. BRAF mutant colorectal cancer: Prognosis, treatment, and new perspectives. Ann. Oncol. 28(11), 2648–2657 (2017).
Miao, Y. et al. Prognostic value and immunological role of PDCD1 gene in pan-cancer. Int. Immunopharmacol. 89(Pt B), 107080 (2020).
Samstein, R. M. et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat. Genet. 51(2), 202–206 (2019).
Wu, H. X. et al. Tumor mutational and indel burden: A systematic pan-cancer evaluation as prognostic biomarkers. Ann. Transl. Med. 7(22), 640 (2019).
Havel, J. J., Chowell, D. & Chan, T. A. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat. Rev. Cancer. 19(3), 133–150 (2019).
Chalmers, Z. R. et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 9(1), 34 (2017).
Schrock, A. B. et al. Tumor mutational burden is predictive of response to immune checkpoint inhibitors in MSI-high metastatic colorectal cancer. Ann. Oncol. 30(7), 1096–1103 (2019).
Pan, Y., Liu, G., Zhou, F., Su, B. & Li, Y. DNA methylation profiles in cancer diagnosis and therapeutics. Clin. Exp. Med. 18(1), 1–14 (2018).
Klutstein, M., Nejman, D., Greenfield, R. & Cedar, H. DNA methylation in cancer and aging. Cancer Res. 76(12), 3446–3450 (2016).
Fattahi, S. et al. DNA methyltransferases and gastric cancer: Insight into targeted therapy. Epigenomics 10(11), 1477–1497 (2018).
Xu, R. H. et al. Circulating tumour DNA methylation markers for diagnosis and prognosis of hepatocellular carcinoma. Nat. Mater. 16(11), 1155–1161 (2017).
Humphrey, S. J., James, D. E. & Mann, M. Protein phosphorylation: A major switch mechanism for metabolic regulation. Trends Endocrinol. Metab. 26(12), 676–687 (2015).
Arrington, J. V., Hsu, C. C., Elder, S. G. & Andy, T. W. Recent advances in phosphoproteomics and application to neurological diseases. Analyst. 142(23), 4373–4387 (2017).
Lin, C. Y. et al. Histone demethylase KDM4C stimulates the proliferation of prostate cancer cells via activation of AKT and c-Myc. Cancers (Basel). 11(11), 1785 (2019).
Buderath, P. et al. Prognostic significance of PD-1 and PD-L1 positive tumor-infiltrating immune cells in ovarian carcinoma. Int. J. Gynecol. Cancer. 29(9), 1389–1395 (2019).
Gong, J., Chehrazi-Raffle, A., Reddi, S. & Salgia, R. Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: A comprehensive review of registration trials and future considerations. J. Immunother. Cancer. 6(1), 8 (2018).
Chahrour, M. et al. MeCP2, a key contributor to neurological disease, activates and represses transcription. Science 320(5880), 1224–1229 (2008).
Fattahi, S., Amjadi-Moheb, F., Tabaripour, R., Ashrafi, G. H. & Akhavan-Niaki, H. PI3K/AKT/mTOR signaling in gastric cancer: Epigenetics and beyond. Life Sci. 262, 118513 (2020).
Acknowledgements
We thank Prof. Huang Chen (Key Laboratory of Environment and Gene Related to Diseases, Xi’an Jiaotong University Health Science Center, China) for his kind assistance. The authors thank AiMi Academic Services (www.aimieditor.com) for English language editing and review services.
Funding
The National Natural Science Foundation of China (Grant Nos. 81860444, 81760510, 82060521, and 81760484), Shaanxi Province Key Science and Technology Innovation team (2020TD-039, Natural Science Basic Research Program of Shaanxi Province (2021JQ-637), Yan’an Key Laboratory of Chronic Disease Prevention and Research, Yan’an University Scientific Research Projects (No. YD2020-22). Science and technology breakthrough plan project of Yan'an Science and Technology Bureau (2018KS-6), and General special project of Shaanxi Provincial Department of Education (17JK0878).
Author information
Authors and Affiliations
Contributions
Y.F.W., Y.Q.Z. and F.H.W. were responsible for conceptualization. Y.F.W., T.L.,H.H.Z., H.M.J. and J.Q.H. contributed to the data collection. Y.F.W., T.L., X.Q.S., H.Y.S. and J.D. conducted the analysis and produced the results and figures. D.D.T. and J.Z. drafted the Manuscript. All authors were involved in themanuscript review
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Zhang, Y., Wang, F. et al. Bioinformatics analysis of prognostic value and immunological role of MeCP2 in pan-cancer. Sci Rep 12, 18518 (2022). https://doi.org/10.1038/s41598-022-21328-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-21328-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.












