Abstract
A methanol poisoning outbreak occurred in Iran during the initial months of coronavirus disease 2019 (COVID-19) pandemic. We aimed to evaluate the epidemiology of the outbreak in terms of hospitalizations and deaths. A cross-sectional linkage study was conducted based on the hospitalization data collected from thirteen referral toxicology centers throughout Iran as well as mortality data obtained from the Iranian Legal Medicine Organization (LMO). Patient data were extracted for all cases aged > 19 years with toxic alcohol poisoning during the study period from February until June 2020. A total of 795 patients were hospitalized due to methanol poisoning, of whom 84 died. Median [interquartile ratio; IQR] age was 32 [26, 40] years (range 19–91 years). Patients had generally ingested alcohol for recreational motives (653, 82.1%) while 3.1% (n = 25) had consumed alcohol-based hand sanitizers to prevent or cure COVID-19 infection. Age was significantly lower in survivors than in non-survivors (P < 0.001) and in patients without sequelae vs. with sequelae (P = 0.026). Twenty non-survivors presented with a Glasgow Coma Scale (GCS) score > 8, six of whom were completely alert on presentation to the emergency departments. The time from alcohol ingestion to hospital admission was not significantly different between provinces. In East Azerbaijan province, where hemodialysis was started within on average 60 min of admission, the rate of sequelae was 11.4% (compared to 19.6% average of other provinces)—equivalent to a reduction of the odds of sequelae by 2.1 times [95% CI 1.2, 3.7; p = 0.009]. Older patients were more prone to fatal outcome and sequelae, including visual disturbances. Early arrival at the hospital can facilitate timely diagnosis and treatment and may reduce long-term morbidity from methanol poisoning. Our data thus suggest the importance of raising public awareness of the risks and early symptoms of methanol intoxication.
Similar content being viewed by others
Introduction
Iran was the epicenter of the early COVID-19 pandemic in the Middle East, with 1,194,963 cases and 54,574 deaths reported by January 17th 20211. In the absence of effective treatments for the infection, the World Health Organization (WHO) and the United States (US) Centers for Disease Control and Prevention (CDC)2,3 recommended wearing face masks, social distancing, and hand sanitization using soap or alcoholic hand sanitizers as key preventive strategies to contain viral spread2,3. According to WHO and CDC guidelines, effective alcohol-based hand sanitizers should contain at least 60% ethanol (ethyl alcohol) or 70% isopropanol (isopropyl alcohol)4,5.
In Iran, however, false beliefs about supposed COVID-19-protective effects of the ingestion of herbal products, vitamins, trace elements, spices, opium, disinfectants, and sanitizers were common. The high consumer demand for hand sanitizers led to the production of counterfeit and non-standard alcohol-based sanitizers which could be classified into two groups: hand sanitizers with inappropriate proportion of ethanol (< 60%) and hand sanitizers containing methanol6.
When misused, alcohol-based sanitizers may be toxic to human health. Ingestion of low-concentrated hydrogen peroxides may result in gastrointestinal (GI) tract irritation. Isopropyl alcohol consumption may lead to severe respiratory and central nervous system depression, and ethanol toxicity may result in a set of common complications4,7. When added to hand sanitizers, the serious toxic effects of methanol can occur through inhalational, oral, or dermal exposure4,7.
The increased availability of alcohol through hand sanitizers resulted in a mass methanol poisoning in Iran8,9, as all provinces reported methanol-poisoned patients from March 7th to April 8th, 2020. Deaths due to methanol poisoning were reported in 26 out of 31 Iranian provinces10. In the single province of Fars alone, 797 cases of methanol poisoning and 97 deaths were reported11. The 2020 methanol outbreak in Iran thus exceeds the 2013 outbreak in Libya with 1,066 victims and approximately 100 fatalities12, previously considered to be the largest outbreak reported.
In an earlier publication, we reported on the epidemiology of the 2020 methanol outbreak in Iran, including total number of deaths (approx. 800) and cases (> 5,800) nationwide, but did not have access to patient data at the time of reporting13.
In order to address this gap of knowledge, we conducted a multicenter linkage study, with the aim to investigate the epidemiology of the 2020 methanol poisoning outbreak based on patient data reported by 13 referral toxicology centers and the Iranian Legal Medicine Organization (LMO).
Materials and methods
Design
This cross-sectional linkage study was conducted on data collected from 13 referral toxicology centers in affiliation with eleven academic centers (medical universities), as well as mortality data obtained from the LMO. The latter provided the death toll from toxic alcohol poisonings in Iran during the study period from February until May 2020, i.e. during the first wave of COVID-19.
Setting
Data collection took place at the following 13 referral toxicology centers distributed throughout 11 of the 31 provinces in Iran: Tehran (Loghman Hakim Hospital), Tabriz (Sina Hospital), Isfahan (Alzahra Hospital), Yazd (Shahid Beheshti and Shah Vali Hospital), Ghaemshahr (Vali-e-Asr Hospital), Urmia (Imam Khomeini Hospital), Mashhad (Imam Reza Hospital), Qazvin (Booali-Sina Hospital), Rasht (Razi Hospital), Hamadan (Be’sat Hospital), and Ahvaz (Imam Hospital).
Participants
Convenience sampling was used to recruit all patients who met the eligibility criteria, without prior calculation of sample size.
Inclusion criteria
All alcohol-poisoned patients older than 19 years with a history of illicit alcoholic beverage/hand sanitizer consumption and manifestations of alcohol intoxication including GI symptoms, visual disturbances (VDs), dyspnea, and central nervous system (CNS) signs/symptoms presenting to one of the participating referral toxicology centers between February 22nd and June 30th 2020 were included. Methanol poisoning was diagnosed based on a serum methanol level of 6.25 mmol/L (20 mg/dL) or higher, or a high clinical suspicion of methanol poisoning based on clinical features and a pH < 7.3 and serum bicarbonate < 20 mmol/L14.
Exclusion criteria
Patients with signs and symptoms and lab tests purely indicative of ethanol poisoning (inebriation without typical GI, VD, and CNS symptoms of methanol poisoning as well as a normal or near normal blood gas analysis) were considered to be ethanol-intoxicated and excluded because serum ethanol concentration could not be routinely measured in the emergency department setting in any of the involved toxicology centers.
Treatment protocol
All methanol-poisoned patients supposed to be treated according to existing national- and international guidelines14,15. Bicarbonate therapy (to correct metabolic acidosis), ethanol therapy (to prevent metabolism of methanol to toxic byproducts), folinic acid (or folic acid in the absence of folinic acid) administration (to facilitate resolving of metabolic acidosis), and hemodialysis (to eliminate methanol, the toxic byproducts, and further correct the acidosis) are the mainstay of treatment. Fomepizole is approved in Iran, but is not available due to high cost.
Measures
Referral toxicology centers
A questionnaire was filled out for every single patient on admission, recording the following: Patients’ demographic characteristics including age, gender, and city (province) of admission, route of exposure (ingestion, inhalation, dermal), cause of consumption (accidental, recreational, suicidal attempt, prevention of COVID-19 infection), place of purchase (pharmacies, supermarkets, herbal shops, hygiene shops, vendors), history of recreational alcohol consumption (chronic users), time elapsed between consumption and hospital presentation (if available), Glasgow Coma Scale (GCS) on admission, need for intubation and hemodialysis (HD), and final outcome (death, survival with- or without sequalae). The time from alcohol intake to hospital admission and the time from arrival to initiation of treatment (see above) were recorded to study possible correlations to outcomes.
Referral toxicology centers were categorized based of the percentage of mortality and sequelae into low and high mortality/sequela rate to make the comparison of sociodemographic and treatments possible.
Legal Medicine Organization (LMO)
Since the LMO is responsible for issuing death certificates in cases of unnatural deaths including deaths due to alcohol intoxication, we matched all fatalities due to methanol poisoning reported by the toxicology centers with the mortality data from the LMO during the same period using the patients’ national identification numbers16.
Data analysis
The data was rechecked by two co-authors (SE and PZ) after the questionnaire had been collected electronically from the referral centers to minimize the missing data. Inappropriate and incomplete data were excluded. Data was analyzed using Statistical Package For Social Sciences (SPSS) software version 26, with a significance level of P < 0.05. Mann–Whitney U test was used for analysis of non-normally distributed quantitative data. Kruskal Wallis test was applied to see the continuous data differences among age groups, provinces, and treatments done. A bivariate regression analysis was applied to assess possible variables which independently affect the main outcomes (i.e. death vs. survival and sequelae vs. no-sequelae). We used ROC curve to define the best cut-off for continuous variables based on sensitivity and specificity. A hazard index heatmap was generated by Excel software to show the most vulnerable age and sex groups in every 100,000 inhabitants in each province. The number of inhabitants was retrieved from the statistical center of Iran (https://www.amar.org.ir/english) and was calculated for the study period based on the growth rate in each province.
Research ethics
The study was approved by the local ethics committee at Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1399.149). Need for written informed consent from the patients or their relatives was waived by ethics committee at Shahid Beheshti University of Medical Sciences due to the fact that the research presented was purely observational and involved no procedures for which written informed consent is normally required. (no 33127).
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (IR.SBMU.RETECH.REC.1399.149). All experiments were in accordance with Helsinki declaration.
Results
Hospitalizations
During the study period, a total of 795 adult patients were hospitalized in thirteen referral toxicology centers (see Table 1). The median age among patients was 32 years [IQR 26, 40] (range 19–91). Males were more commonly admitted due to alcohol poisoning compared to females (P < 0.001), as 90.3% (718 cases) of the patients were male.
Deaths
In total, there were 84 fatalities among the 795 hospitalized patients (case-fatality rate of 10.6%) prior to discharge (Table1). All 84 deaths due to methanol poisoning were matched between hospital records and LMO mortality reports using the patients’ national identification number. The non-survivors were significantly older than patients who survived methanol poisoning (39 vs. 31 years, P < 0.001). Among the survivors, those who experienced sequelae were also significantly older that other patients without sequelae (33 vs. 30 years, P = 0.026).
Variation by age and geography
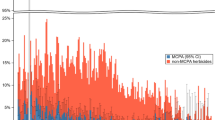
The number of patients and the mortality rate varied between age groups and the various provinces (Supplementary Table 1, Tables 2 and 3). Overall, 20- to 24-year-old patients had the lowest mortality rate (0.05/100,000), whereas 40- to 44-year-old cases had the highest (0.48/100,000). The capital city (Tehran) had the highest total number of referrals and deaths (Figs. 1 and Supplementary Fig. 1), whereas, after adjustment for population size, Yazd province had the highest rate of referrals among 25- to 30-year-old males (25.49 patients/100,000 population). The highest mortality rate was registered among 40- to 44-year old males in East Azerbaijan with 4.24 deaths/100,000 population. Figure 2 shows the trend of methanol poisoning in the first 4 months following COVID-19 in Iran.
Number of alive (left) and dead (right) patients referred to 11 out of 31 Iranian provinces. Data visualizations were performed using Tableau Desktop, version 2020.1, an interactive data visualization software. (Tableau Software. Seattle, WA; Available through: https://www.tableau.com/).
Source of exposure
Patients had mostly ingested adulterated alcoholic beverages (92.2%), whereas 7.8% had ingested hand sanitizers and industrial alcohols. Among the 706 (88.8%) cases with complete dataset, the most common cause of ingestion was recreational (82.1%), whereas accidental consumption (3.5%) or intake to prevent COVID-19 (3.1%) were also reported. The cause of alcohol consumption remained undetermined in the remaining 89 cases (11.2%).
Most patients reported having purchased the alcoholic beverages and hand sanitizers from street vendors (465; 58.5%), followed by supermarkets (75; 9.4%), hygiene shops (18; 2.3%), pharmacies (7; 0.9%), and herbal shops (2; 0.3%).
Time of admission post-ingestion
Among the 684 (86.0%) cases with defined time of exposure, statistical differences were found between fatalities vs. survivors (24 vs. 48 h, P = 0.014, Table 3). The correlation remained significant when comparing fatalities vs. survivors with sequelae (24 vs. 48 h, P = 0.004) as well as fatalities vs. survivors without sequelae (24 vs. 45 h, P = 0.031). After removing the fatalities from the analysis, the time of admission post-ingestion was not different among survivors with sequelae vs. survivors with no sequelae (48 vs. 45 h, P = 0.068). None of the fatalities were admitted sooner than 6 h.
Clinical symptoms
Among the 338 (42.5%) patient files with complete review, gastro-intestinal symptoms, nausea and/or vomiting (314; 92.89%) were most commonly found. A total of 566/738 patients (76.7%) with complete visual examination had VDs on arrival to the medical care facilities. The examination was not possible in 57 patients who was admitted with loss of consciousness (LOC), unless their family members reported witnessed VDs before LOC of the patient. Five patients became legally blind during the hospital stay, one of whom later died due to complications of methanol toxicity. On presentation, 568 (71.5%) were fully awake with GCS 15/15. Among the fatalities, 20/84 (23.8%) had GCS > 8 on admission. Among these, 6/84 were completely alert (GCS 15) and presented only with GI-symptoms and VDs.
Treatment
Table 4 shows four different treatments in 716 patients with available data on three major outcomes. There was no significant differences from ingestion to admission time in 13 toxicology centers, while the time of initiation of treatments after arrival were different.
Dialysis was performed in 582 (73.2%) of the patients: Among the fatalities, 64/84 (76.2%) had one dialysis-session, and 30/84 (35.7%) had two sessions due to persistent acidosis and/or concomitant VD. Among the survivors, 518/711 (72.9%) had one HD-session, and 109/711 (15.3%) had two sessions (P < 0.001). No other significant differences were detected between the two groups of deaths and survivors. Among the 479 survived cases with documented VDs on arrival and visual examination on discharge, 343 (71.6%) were treated with HD and medical management, and their VD were resolved [OR 55.6 (95%CI, 7.6, 333.3); p < 0.001].
Comparing survivors with and without sequela (n = 632), those provinces (East Azerbaijan) that started hemodialysis within average 60 min post admission (Table 4), the rate of sequelae was 11.4% (compared to 19.6% average of other provinces). This shows odds of 2.1 times less sequelae in East Azerbaijan [95% CI 1.2, 3.7, p = 0.009] compared to other provinces.
Discharge
Among the survivors, 492/632 (77.8%) had no sequelae on discharge, whereas 133/632 (21.1%) had visual disturbances and 7/632 (1.1%) had neurological complications. The data on health status was not available in 79/795 (9.9%) cases as they left the hospital against medical advice, or were transferred to other hospitals essentially due to lack of ICU beds.
Bivariate regression analysis
Table 5 displays regression analysis for the two main outcomes of death (alive/dead) and sequelae among survivors (present/not present). For death, a GCS score equal or below 9 points and age > 36 years were independent predictors. A GCS score equal or below 9 points, age > 31 years, and provenance from any province except for East Azerbaijan (with a sequela rate of 11.4% vs. average sequelae of 19.6%) independently predicted presence of sequelae on discharge. Yazd and Khorsan Razavi (with mortality rate of 0.9%) were significantly different from other provinces with average mortality of 10.6% (OR 15.2, 95% CI 2.1, 110.3, p < 0.001) in univariate analysis. However, in regression analysis, the patient’s province of residence did not predict mortality.
Discussion
In this study, we report on 795 adult patients who were hospitalized for methanol poisoning in thirteen Iranian referral toxicology centers, of whom 84 patients died.
In methanol poisoning, the outcome is typically defined by the level of consciousness on arrival, the severity of the acidosis, and also ability of respiratory compensation of metabolic acidosis. Vice versa, a lack of ability to hyperventilate when acidotic has been shown as a poor prognostic factor15,17,18.
Our findings are unexpected in that they show a difference in outcome between the age groups, and suggest that early admission was associated with fatal outcome. Older patients were more prone to late complications and death, possibly due to reluctance to seek medical aid or due to background diseases.
Paradoxically, the fatalities in our study arrived earlier compared to survivors (24 h vs. 45–48 h). Death from methanol poisoning requires metabolism to—and accumulation of—formate, and it takes time to reach fatal levels. A possible explanation is that the dead cases consumed pure methanol to a greater degree, whereas survivors might have ingested a blend of ethanol and methanol (which may have caused them to deteriorate and seek medical care later). However, due to lack of laboratory confirmation of ethanol, methanol, and byproducts, we are unable to test this hypothesis in this study, and any interpretations remain speculative.
The current data shows how methanol poisoning affects patients as young as in their twenties who, if they survive with sequelae, will face many years of disability due to visual impairment (see Table 3). Further, the high fatality rate (approximately 10%) and the fact that six of the fatalities were completely alert on admission, illustrates the difficulties of diagnostic- and therapeutic strategies of methanol poisoning. Limited facilities to treat methanol poisoning during the COVID-19 pandemic may have worsened the situation, and limitations in diagnostic facilities may have further added to the high death toll8,12. Moreover, patient fears of COVID-19 infection in the hospital setting may have led to late presentations.
Iran is one of the countries where methanol mass poisonings occur frequently, likely due to limited access to legal alcohol. This has become a major health concern in recent years14,15. Alcohol availability in Iran has become further complicated after the price of standard manufactured alcoholic beverages significantly increased due to the economic sanctions against the country introduced by the US administration in 201719,20,21,22. Major outbreaks had previously been reported in Iran, e.g. in 2013 and 2018, the latter involving 768 patients and 96 deaths in 21 provinces21. In none of the outbreaks before COVID-19, hand sanitizers had any role as a source of methanol poisoning.
Since the beginning of the COVID-19 pandemic, many reports have been published warning about the dangers of methanol content in hand-sanitizers and in bootlegged alcohol sold for consumption in Iran8,13,22. However, clinical complications from drinking hand-sanitizers is a global challenge, including Asian countries as well as the US23, as false beliefs about preventing COVID-19 infection by ingestion of alcoholic hand sanitizers have claimed numerous human lives24,25.
With limited access to standard alcoholic beverages and hand sanitizers, Muslim countries like Iran, Malaysia, and Indonesia are more vulnerable to these sub-standard products25. Worldwide reports of methanol outbreaks during the pandemic (https://msf.no/mpi, accessed 29th Sept 2021) should prompt urgent action to address the issue.
On April 5th 2020, a warning was issued by WHO on the hazardous effects of ingestion of bleach and alcoholic hand-sanitizers26. More efforts are however warranted to prevent methanol poisoning by ingestion of non-standard alcohols all around the world.
The healthcare burden of methanol poisoning becomes especially apparent during mass poisonings with high volume of patients referring with a possible diagnosis of methanol poisoning. The system may then become inefficient or even collapse15. Lack of access to antidotes (ethanol or fomepizole) and other treatment facilities (including hemodialysis and ICU capacities) are other concerns that should be addressed to ensure better preparedness for future events. A stronger focus on “active case finding” through traditional and social media27 is likely to prove beneficial in a majority of cases. Treatment should be initiated as early as possible to reduce the risk of sequelae and death.
Limitations
The reported fatality rates are based on the data recorded in thirteen toxicology referral hospitals that agreed to take part in this study. These patient data are not exhaustive, as the hospitals only represent eleven of the 31 provinces in Iran. As a result, our sample size (n = 795 patients) is only a fraction of the total count of 5,876 hospitalizations due to methanol poisoning during the first quarter of COVID-19 that we reported on in an earlier publication20.
Fatalities due to methanol poisoning may have occurred without patient referral to a toxicological referral centers, suggesting that the mortality rate presented in this study is a conservative estimate. Also, some of the methanol intoxicated patients had concomitant COVID-19 infection, and if they died, their bodies were not sent to LMO for autopsy due to infection. Their death certificate would be issued by the health care authorities, and thus not entered into the LMO data.
Lack of analyses for methanol, ethanol and formic acid in the current study may reduce the internal validity of data. Furthermore, the time to admission was based on patient (or family member) self-reporting, and thus likely subject to recall and social desirability biases. Similarly, time to admission does not equal to time to treatment in most of the cases (especially for HD). Finally, possible variations in in the treatment and data collection practices between the eleven provinces mean that direct comparisons may not be feasible.
Conclusion
Our results suggest that older patients were more prone to fatal outcome, whereas younger patients were more likely to survive. However, in the absence of laboratory data of methanol and ethanol concentrations on admission, this finding needs to be interpreted with great caution. Generally speaking, early arrival at the hospital can facilitate timely diagnosis and treatment and may reduce long-term morbidity from methanol poisoning. Our data thus suggest the importance of raising public awareness of the risks and early symptoms of methanol intoxication.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABHRs:
-
Alcohol-based Hand Rubs
- CDC:
-
Centers for Disease Control and Prevention
- CI:
-
Confidence interval
- GCS:
-
Glasgow Coma Scale
- HD:
-
Hemodialysis
- OR:
-
Odds ration
- SPSS:
-
Statistical Package for the Social Sciences
- TGA:
-
Therapeutic Goods Administration
- VDs:
-
Visual disturbances
- WHO:
-
World Health Organization
References
World Health Organization. Weekly epidemiological updates- 17 January. https://www.who.int/publications/m/item/weekly-epidemiological-update---17-January-2021. (2021).
Centers for Disease Control and Prevention. Prevention of Coronavirus Disease 2019 (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/prepare/prevention.html. [Accessed 30 December 2020]
World Health Organization. Recommendations to Member States to Improve Hand Hygiene Practices to Help Prevent the Transmission of the COVID-19 Virus: Interim Guidance. https://www.who.int/publications/m/item/interim-recommendations-on-obligatory-hand-hygiene-against-transmission-of-covid-19. [Accessed 30 December 2020] (2020).
Mahmood, A. et al. COVID-19 and frequent use of hand sanitizers; human health and environmental hazards by exposure pathways. Sci. Total Environ. 742, 140561 (2020).
Yip, L. et al. Serious adverse health events, including death, associated with ingesting alcohol-based hand sanitizers containing methanol - Arizona and New Mexico, May-June 2020. MMWR Morb. Mortal. Wkly Rep. 69(32), 1070–1073 (2020).
Jairoun, A. A., Al-Hemyari, S. S. & Shahwan, M. The pandemic of COVID-19 and its implications for the purity and authenticity of alcohol-based hand sanitizers: The health risks associated with falsified sanitizers and recommendations for regulatory and public health bodies. Res. Soc. Adm. Pharm. 17, 2050–2051 (2020).
Chan, A. P. L. & Chan, T. Y. K. Methanol as an unlisted ingredient in supposedly alcohol-based hand rub can pose serious health risk. Int. J. Environ. Res. Public Health 15, 6–11 (2018).
Delirrad, M. & Mohammadi, A. B. New methanol poisoning outbreaks in Iran following COVID-19 pandemic. Alcohol Alcohol. 55, 347–348 (2020).
Iranpour, P., Firoozi, H. & Haseli, S. Methanol poisoning emerging as the result of COVID-19 outbreak; radiologic perspective. Acad. Radiol. 27, 755–756 (2020).
Aghababaeian, H., Hamdanieh, L. & Ostadtaghizadeh, A. Alcohol intake in an attempt to fight COVID-19: A medical myth in Iran. Alcohol 88, 29–32 (2020).
Sefidbakht, S. et al. Methanol toxicity outbreak: When fear of COVID-19 goes viral. Emerg. Med. J. 37, 416 (2020).
Rostrup, M. et al. The methanol poisoning outbreaks in Libya 2013 and Kenya 2014. PLoS ONE 11(3), e0152676 (2016).
Hassanian-Moghaddam, H., Zamani, N., Kolahi, A. A., McDonald, R. & Hovda, K. E. Double trouble: Methanol outbreak in the wake of the COVID-19 pandemic in Iran-a cross-sectional assessment. Crit. Care 24(1), 402 (2020).
Hassanian-Moghaddam, H. & Zamani, N. A brief review on toxic alcohols: Management strategies. Iran J. Kidney Dis. 10(6), 344–350 (2016).
Hassanian-Moghaddam, H. et al. Consensus statements on the approach to patients in a methanol poisoning outbreak. Clin. Toxicol. (Phila). 57(12), 1129–1136 (2019).
Kordrostami, R. et al. Forensic toxicology analysis of self-poisoning suicidal deaths in Tehran, Iran; trends between 2011–2015. DARU J. Pharm. Sci. 25, 15 (2017).
Paasma, R. et al. Risk factors related to poor outcome after methanol poisoning and the relation between outcome and antidotes: A multicenter study. Clin. Toxicol. (Phila). 50(9), 823–831 (2012).
Zakharov, S. et al. The impact of co-morbidities on a 6-year survival after methanol mass poisoning outbreak: Possible role of metabolic formaldehyde. Clin. Toxicol. 58(4), 241–253 (2020).
Nikoo, M. H. et al. Electrocardiographic findings of methanol toxicity: A cross-sectional study of 356 cases in Iran. BMC Cardiovasc. Disord. 20, 1–8 (2020).
Shadnia, S., Rahimi, M., Soltaninejad, K. & Nilli, A. Role of clinical and paraclinical manifestations of methanol poisoning in outcome prediction. J. Res. Med. Sci. 18(10), 865–869 (2013).
Aghababaeian, H., Ahvazi, L. A. & Ostadtaghizadeh, A. The methanol poisoning outbreaks in Iran 2018. Alcohol Alcohol. 54, 128–130 (2019).
Mehrpour, O. & Sadeghi, M. Toll of acute methanol poisoning for preventing COVID-19. Arch. Toxicol. 42, 2–3 (2020).
Overbeek, D. L., Watson, C. J., Castañeda, N. R. & Ganetsky, M. A geographically distinct case of fatal methanol toxicity from ingestion of a contaminated hand sanitizer product during the COVID-19 pandemic. J. Med. Toxicol. 17(2), 218–221. https://doi.org/10.1007/s13181-021-00824-9 (2021).
Dear, K., Grayson, L. & Nixon, R. Potential methanol toxicity and the importance of using a standardised alcohol-based hand rub formulation in the era of COVID-19. Antimicrob. Resist. Infect Control 9(1), 129. https://doi.org/10.1186/s13756-020-00788-5 (2020).
“In Iran, False Belief Toxic Methanol Fights Coronavirus Kills Hundreds.” South China Morning Post, 27 Mar. 2020. www.scmp.com/news/world/middle-east/article/3077284/coronavirus-iran-false-belief-toxic-methanol-fights-covid-19. [Accessed 24 January 2021]
Coronavirus Disease (COVID-19) Advice For The Public: Mythbusters. Retrieved from Mythbusters (who.int). Accessed 27 September 2021.
Hassanian-Moghaddam, H. et al. Methanol mass poisoning in Iran: Role of case finding in outbreak management. J. Public Health 37(2), 354–359 (2015).
Acknowledgements
The authors wish to thank Mrs Somaye Sohrabi Ph.D. Student of Medical Education from Social Determinants of Health Research Center, for her great assistance in data entering and matching.
Funding
The authors report no relevant disclosures. This study was supported by Shahid Beheshti University of Medical Sciences (award number 33127).
Author information
Authors and Affiliations
Contributions
A.A.K., S.A.M. and H.H.M. participated in the study design. M.A. and M.G. participated in the acquisition and interpretation of data in Legal Medicine Research Center. The acquisition and interpretation of data in eleven provinces was done by F.G., A.O., A.D., M.M., M.R.T., M.D., N.M., S.A., S.E., P.Z., N.K., A.M.K., H.F., T.B., F.S., S.K.H., M.H., J.M., F.J. and B.D. M.A. and M.R.M. checked the accuracy of data and designed the figures. N.Z. wrote the first draft of manuscript. N.Z., R.M., and K.E.H. critically revised the manuscript. All the authors have read the journal’s authorship agreement and the manuscript has been reviewed and approved by all named authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahdavi, S.A., Zamani, N., McDonald, R. et al. A cross-sectional multicenter linkage study of hospital admissions and mortality due to methanol poisoning in Iranian adults during the COVID-19 pandemic. Sci Rep 12, 9741 (2022). https://doi.org/10.1038/s41598-022-14007-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-14007-1
This article is cited by
-
Tertiary referral hospital experience of methanol poisoning in the COVID-19 era: a cross-sectional study in Northwestern Iran
Bulletin of the National Research Centre (2023)
-
The danger of the toxicity and inefficacy of alcohol-based hand rubs in Iran during COVID-19: a cross-sectional study
Antimicrobial Resistance & Infection Control (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.