Abstract
Genetic testing for cancer predisposition has been curtailed by the cost of sequencing, and testing has been restricted by eligibility criteria. As the cost of sequencing decreases, the question of expanding multi-gene cancer panels to a broader population arises. We evaluated how many additional actionable genetic variants are returned by unrestricted panel testing in the private sector compared to those which would be returned by adhering to current NHS eligibility criteria. We reviewed 152 patients referred for multi-gene cancer panels in the private sector between 2014 and 2016. Genetic counselling and disclosure of all results was standard of care provided by the Consultant. Every panel conducted was compared to current eligibility criteria. A germline pathogenic / likely pathogenic variant (P/LP), in a gene relevant to the personal or family history of cancer, was detected in 15 patients (detection rate of 10%). 46.7% of those found to have the P/LP variants (7 of 15), or 4.6% of the entire set (7 of 152), did not fulfil NHS eligibility criteria. 46.7% of P/LP variants in this study would have been missed by national testing guidelines, all of which were actionable. However, patients who do not fulfil eligibility criteria have a higher Variant of Uncertain Significance (VUS) burden. We demonstrated that the current England NHS threshold for genetic testing is missing pathogenic variants which would alter management in 4.6%, nearly 1 in 20 individuals. However, the clinical service burden that would ensue is a detection of VUS of 34%.
Similar content being viewed by others
Introduction
Background
The landscape of genetic testing for germline cancer predisposition has shifted from single gene testing to multi-gene panels. While the National Health Service (NHS) has integrated some cancer gene panel testing into routine clinical care1, there remains debate regarding which of our patients we should be testing. Historically, extensive genetic testing has been curtailed by the cost of DNA sequencing, leading to the establishment of gatekeeping eligibility criteria. With the advent of multiplexed high-throughput sequencing, the cost continues to decline, opening the possibility of testing hereditary cancer predisposition in a wider population1, so much so, that some groups have questioned the relevance of genetic testing guidelines altogether2,3.
Genetic testing criteria are often based upon a combination of family history, personal demographic and cancer data, and features consistent with cancer syndromes4. The National Institute for Health and Care Excellence (NICE) also publishes testing guidelines operating on family history models, and generally sets the cost-effectiveness threshold for gene testing as a carrier probability of 10% or more5. NHS England have specified which tests are commissioned by the NHS, and publish criteria-based cancer genetic testing guidelines. Although eligibility criteria for genetic testing assist resource management within the NHS, such criteria remain flawed for the following reasons (Box 1):
Apparently sporadic cancers may actually be hereditary, missed by family history criteria as modern pedigrees have gradually become smaller and more blended6. Although germline BRCA1 and BRCA2 (BRCA1/2) pathogenic variants account for a large proportion of Hereditary Breast and Ovarian Cancer (HBOC), a Scottish study on BRCA1/2 testing in ovarian cancer revealed that 48% of pathogenic variants did not fulfil family history criteria for testing7. The new Scottish policy of unselected testing of all patients with non-mucinous ovarian cancer increased the annual rate of BRCA1/2 variant detection five-fold7. Similarly, a single-centre study on RET gene testing revealed that more than half of patients with a Medullary Thyroid Carcinoma (MTC) and a RET pathogenic variant did not have a significant family history of cancer8. This discrepancy may also be attributed to de novo cases9. Similar studies outside the UK have supported this, with up to 54% of variant carriers being missed due to restrictions of family history criteria7,10.
Multiple studies have identified the underuse of genetic testing in cancer patients, despite recommendations8,11,12,13,14,15,16. While testing for BRCA1/2 variants has gained significant traction12, for women with breast cancer meeting eligibility criteria, uptake ranges from 30 to 65%13. In American literature, women of African American or Hispanic origin are less likely to be referred to genetics services12 and eligibility criteria do not always reflect ancestry-dependent cancer risks17. Although it is universally indicated, BRCA1/2 testing was performed in only 31% of males with breast cancer, and 17.4% of women with ovarian cancer in a study of commercially insured patients in the USA13. A study of compliance with testing for Multiple Endocrine Neoplasia Type 2 (MEN2) in patients with MTC revealed 40% did not have RET gene testing, which is indicated for all patients with an MTC8. A similar story of under-testing and possible under-diagnosis also applies to colorectal cancer14,15,18. The misalignment of testing guidelines with clinical practice may be due to a variety of reasons, such as a healthcare professional’s lack of awareness of testing guidelines, resource availability, and population-level behavioural differences leading to patient refusal or non-compliance12.
A multi-generational family history is paramount to identification of patients with high-risk cancer susceptibility19,20,21. As genetic testing is integrated into standard practice, a process known as ‘mainstreaming’, the onus is increasingly falling on non-geneticists to take the family history. Prior studies suggest the process of taking a family history can be suboptimal19,22, with one study identifying only 61.5% take a family history up to second-degree relatives11. Family history criteria often rely on information provided by relatives as electronic records are incomplete and inaccessible across institutions. Situations where difficulties arise include abdominal cancers which are notoriously poorly reported, forms of the disease which are not highly-penetrant9, or the patient’s lack of knowledge of their family medical history23. Systemic barriers include limited time for the physician or genetic counsellor (GC) to collect a full family history, as well as time-consuming data collection tools23.
The landscape of pathogenic variants
On average, genomic predisposition contributes to 5–10% of all cancers24,25,26, however for certain cancers in certain populations this can be higher (even as high as 30%)8. Recognition of this heritability has ever-increasing clinical implications with personalised therapies, as well as ramifications for family cancer surveillance and prophylactic procedures4. The spectrum of pathogenic variants associated with cancer ranges from very rare but highly-penetrant, rare moderate-penetrance, to common low-penetrance variants27. Rare alleles with higher effect size, such as variants in BRCA1/2, are more easily identified27,28. For low and moderately penetrant variants, the individual relative risk conferred is smaller, but in combination of multiple variants, the cumulative risk increases29,30.
Traditional germline testing has been restricted to high-risk predisposition genes, such as BRCA1/2, and mismatch repair (MMR) genes, where classification and management guidelines are better defined. Which genes to include in these panels is determined both at local and regional levels by healthcare institutions and policymakers31. Factors influencing this decision include access to funding1, known population variants, acceptability to patients, and importantly, the pillars of appropriate test use defined by the ACCE Framework: Analytical validity, Clinical validity, Clinical utility, and Ethical, legal and social implications31 (Box 2).
Tests for an expanding array of high and moderate risk genes are becoming available, but the clinical validity of lower-penetrance or newly-identified variants is open to interpretation21. Each test can have its unique implications for patients and their families and there are UK-wide attempts to standardise care nationally1,33. The UK Cancer Genetics Group published guidelines on which genes to include in cancer panels based on clinical validity (Fig. 1), and provided management proposals1. To assist counselling on clinical validity, predictive computer programs incorporating personal history and family history to calculate risk, such as BOADICEA for breast and ovarian cancer in women, have expanded to include some moderate-risk genes28.
The American College of Medical Genetics and Genomics (ACMG) has developed guidelines for more robust variant classification into five categories (Box 3), which relies on multiple factors including population frequency, segregation data, functional and computational modelling, and variant data34.
Studies that have forgone family history-based testing criteria
Researchers and healthcare professionals have explored the ramifications of simplifying access to testing, and eligibility criteria across a range of populations (Table 1).
Our Aim
Our aim was to determine the extent to which more actionable genetic variants are returned by panel testing compared to those that would be returned by criteria-dependent NHS testing of the same genes.
Methods
Participants
This study was conducted at a private oncogenetics clinic in London. Patients were included in the study if they underwent cancer predisposition genetic testing between 2014 and 2016. Genetic pre and post-test counselling was provided to all patients as part of standard clinical care. During clinical consultations, discussion of ancestry, particularly Ashkenazi Jewish ancestry, was highlighted as this influenced targeted testing for pathogenic founder variants. Based on the suspected cancer predisposition, specific gene tests were requested for patients. All patients gave their informed consent to have the panel test undertaken by the clinician, and no additional blood samples were taken for this study.
Illumina sequencing was conducted in a UKAS-accredited private laboratory. Variant classification and interpretation were delivered to patients as part of their standard clinical care. The ACGS/ACGM classification was used for this period, prior to the availability of CanVig classification guidelines. Approval for this study was obtained from the Royal Marsden Hospital audit committee. All methods were performed in accordance with hospital guidelines.
Data collection
Electronic medical records and pedigrees were retrospectively reviewed for information on demographics, and oncological history including age at diagnosis. All patients had an associated family pedigree where data on cancer family history was gathered at the time of the consultation. Box 4 shows information collected on all patients.
Every panel undertaken was compared to the 2020/2021 National Genomic Test Directory Testing Criteria for Rare and Inherited Disease39 using the patient information available at the time of the clinical consultation.
Data analysis
R version 3.5.0 was used for all statistical analysis, and most graphical representations. Microsoft Excel version 16.10 was utilised for the remaining graphics.
Results
Patient characteristics
Between 1st January 2014 to 31st December 2016, 152 individuals underwent multi-gene panel testing at an oncogenetics clinic, the majority of whom were of white ancestry (119 patients [78%]). Details on demographics and oncological history are in Table 2.
There were 54 unaffected patients (35.5%) who underwent testing, and 98 individuals with single or multiple cancers (64.5%) undergoing diagnostic testing. Of the 98 patients affected, the median age at cancer onset was 49 years, ranging from 16 to 82 years of age.
Clinical characteristics of cancers
The cancer incidence was a total of 104 tumours in 98 patients. The most frequent tumour types were breast cancer (44, [42.3%]), followed by colorectal cancer (24, [23.0%]), prostate cancer (11, [10.6%]), and ovarian cancer (5, [4.8%]).
Gene panels tested
Based on personal and/or family history of the patient, the clinician selected the relevant panels and genes to be tested. The 3 commonest panels were breast, colorectal, and ovarian cancer panels. Others were familial renal cancer, Fanconi anaemia, familial melanoma, neurofibromatosis, familial pancreatic cancer, Multiple Endocrine Neoplasia (MEN) syndromes, phaeochromocytoma and paraganglioma, retinoblastoma, and DICER1 gene testing (‘Pleuropulmonary blastoma/Goitre, multinodular 1, with or without Sertoli-Leydig cell tumours’). Supplementary Table 1 outlines the genes tested for each patient.
Gene panel findings
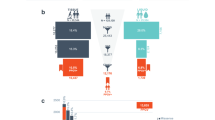
Gene panel sequencing yielded variants in 67 individuals. No variant was detected in 85 individuals (56%), while 34% of people had at least one VUS, and 10% had variants which were P/LP (Fig. 2).
Cancer genes implicated
In 67 individuals, a total of 82 variants were detected in 24 known cancer predisposition genes (Fig. 3). 81.7% of variants were VUS (67 of 82), and 18.3% were P/LP (15 of 82). Focusing on the P/LP variants, these were detected in the following 11 cancer predisposition genes: APC, BRCA1, BRCA2, CHEK2, MLH1, MSH2, MSH6, MUTYH, PALB2, RAD51D, RET. All P/LP variants were actionable, warranting a change in care for both the patient and/or their family.
Group comparisons
Using our demographic and variant data, we compared different groups to determine if there is a difference of statistical significance.
-
I.
Individuals Affected by Cancer vs. Unaffected Individuals
The VUS rate was similar (34% affected, 35% unaffected). In unaffected individuals undergoing testing, there was a higher P/LP rate (13%) compared to affected patients (8%), however this was not statistically significant with a Chi-square test p-value of 0.58.
-
II.
Age of Cancer Onset in Affected Individuals
The 98 patients undergoing diagnostic testing were divided into 2 groups: age of onset of cancer ≤ 50, and > 50, and the variants in each category were assessed. Associations between age and the following two variables were analysed: the number of P/LP variants observed, and the distribution of specific genes detected. Chi-square tests were both not statistically significant: P = 0.32 for the number of P/LP detected, and P = 0.55 for the distribution of the specific genes across age. In conclusion, there were no significant differences in gene panel results based on age at cancer onset in this study.
-
III.
Fulfilment of Eligibility Criteria
All individuals in this study who underwent panel testing in the private sector were compared against eligibility criteria utilised by the NHS. 37% of patients (56 of 152) fulfilled NHS eligibility criteria. Summary statistics are displayed in Fig. 4. Comparing these two groups, there was a statistically significant difference in variant classification rates between those who were eligible for testing and those who were not, as expected.
Focusing on the pathogenic/likely pathogenic variants
Of the 15 P/LP variants detected by panel testing, 7 fulfilled criteria, 7 did not fulfil criteria, and 1 person was adopted. 46.7% of patients who received positive results in this study did not fulfil NHS testing criteria (Fig. 5).
A closer look at the families of the 7 patients with P/LP variants who were not eligible for testing: In 2 cases where an APC pathogenic variant was detected in patients who did not fulfil criteria, a different member of their family did. Conversely, the remaining 5 families, although there was a history of cancer, also did not fulfil testing criteria.
Management of VUS outcomes
For the 52 individuals whose gene panel test yielded a VUS, all patients were informed and received pre and post-test counselling. The subject’s records were placed under annual review of VUS status. It is worth noting that some patients with VUS required additional cancer surveillance based on family history criteria, not the detection of a VUS. Over the 3-year period, only 1 VUS in BRCA1 was re-classified to benign in a patient with triple negative breast cancer. The VUS rate in individuals from a non-European origin was 39%, versus 33% in Europeans.
No P/LP variants were unexpected
Patients in whom P/LP variants were detected, the findings were consistent with either the personal or family history. There were 2 patients with breast cancer and heterozygous variants in MLH1 and MUTYH. This, however, was consistent with their family histories of colorectal cancer.
Clinical utility—Effect on the tested individual
13 of 15 P/LP results changed management for the patient (Fig. 6). The first exception was a woman with breast cancer with a heterozygous pathogenic variant in MUTYH. Due to the autosomal recessive inheritance of the syndrome, neither prophylactic surgery nor cancer screening was recommended. However, the genetic testing did trigger predictive testing of her partner, due to implications for their child. The second exception was a patient in the palliative stages of advanced colorectal cancer.
Clinical utility—Effect on the family
15 of 15 P/LP results changed management for the families of the patients. Members of all families were referred for predictive family testing and/or cancer surveillance. Clinical letters included documentation and counselling on implications for the family. One patient discussed the potential for pre-implantation genetic diagnosis with the physician.
Discussion
How does the rate of P/LP and VUS compare?
Of 152 patients, the variant detection rate was 10% for P/LP variants, and 34% for VUS. This is consistent with other researchers who have forgone testing criteria and achieved this variant threshold2,3,30,35,40,41,42,43,44. An example Tung et al.’s study on 488 women with breast cancer reports a P/LP rate of 10.7% and a VUS rate of 34%41. The P/LP frequency of 10% fulfils the threshold upon which many guidelines and family history-based criteria operate5.
All VUS detected in our study were reviewed yearly and patients were contacted by letter if any management was altered. Limitations of generalising this practice in the UK are that this degree of follow-up is not currently possible on the NHS. The additional resource burden associated with VUS may also entail familial segregation studies, tumour studies and functional testing. International academic institutions are working to define a standardised approach in clinical practice and policy45. Research groups are also endeavouring to assign degrees of risk of deleteriousness to VUS, which may aid clinical decision-making. Following the ACGS variant classification guidance published in 2020, the threshold for reporting VUS is now higher, and only ‘hot’ VUS should be reported after MDT discussion46. Current reporting policy offers promise in reducing the extent of the burden of VUS outcomes. Many VUS transpire to be benign on further follow-up.
Eligibility criteria
Current tests offered in the NHS are restricted to patients who fulfil eligibility criteria. From our study, unrestricted testing of patients returns more actionable genetic variants than current eligibility criteria allow. Our study returned double the number of actionable genetic variants than NHS criteria. Overall, 7 additional P/LP variants were detected in the private clinic, in addition to the 7 that would have been detected on the NHS. Missing this proportion of P/LP variants (46.7%) is supported by prior research47.
Given that these eligibility criteria are evidence-based and designed to identify high-risk patients48, the higher P/LP detection rate and lower VUS rate in the group who fulfilled criteria was expected.
Number needed to screen and risk reduction
Number needed to treat is a common statistical method used for assessing robustness of interventions, from drugs to screening programmes. A similar statistical method applicable to screening is the Number Needed to Screen (NNS)49,50. We applied this statistic to our data to identify how many patients need to undergo gene panel testing to find 1 P/LP variant. Results and calculations are shown in Fig. 7.
Although the same number of P/LP variants were found in both patients who fulfilled and did not fulfil NHS criteria, 6 additional patients were screened in the ineligible cohort. Overall, only 3 additional patients needed to be screened to find a P/LP variant.
We also tried to model to what extent additional testing is likely to improve survival. A large-scale meta-analysis conducted by Rebbeck et al. investigated the risk reduction of prophylactic salpingo-oophorectomy in carriers of P/LP variants in BRCA1 and BRCA251. Prophylactic surgery conferred a reduction in breast cancer (hazard ratio = 0.49) and ovarian and fallopian tube cancers (hazard ratio = 0.21)51. In other words, there is a 79% risk reduction in ovarian and fallopian tube cancers in pathogenic BRCA1/2 carriers with risk-reducing surgery. Utilising this data, as well as mortality figures of ovarian cancer in pathogenic BRCA1/2 carriers, mortality is reduced 4.7-fold for BRCA1, and 46-fold for BRCA2. All calculations are demonstrated in Tables 3 and 4 for BRCA1 and BRCA2 respectively, and were based on the following assumptions: everyone will have had a prophylactic oophorectomy, patients have the same survival benefit as the documented literature, and all P/LP variants behave the same way.
In this study, there were four P/LP BRCA1/2 variants detected, one of whom was not eligible for testing and tested positive for a pathogenic BRCA2 variant which would have otherwise been undetected. Her risk of death from ovarian cancer was reduced 46-fold according to the above calculation (Table 4).
Unexpected findings
In two patients with breast cancer, heterozygous P/LP variants were detected in MLH1 and MUTYH. Although a pattern of colorectal cancer was apparent in their family history, recent evidence does not define an association with breast cancer, except possibly in MUTYH carriers of two pathogenic alleles54,55. Both variants prompted cancer surveillance and/or family screening. An important note is that both of these genes are on the UK consensus of genes for medically-actionable conditions1. By and large, UK experts, drawing on their experience of the 100,000 Genomes Project, urge for clearer policy on the interpretation and reporting of secondary findings to patients56 and this is an avenue for future research.
Clinical utility
The question posed here was as follows: will the variant alter clinical management compared with management based on family history alone? It is important to recognise that even without a detected variant, patients can be at an increased risk of cancer due to family history27,28. For example, if a 20-year-old woman has a first degree relative with breast cancer and an ATM pathogenic variant, and her own test is negative, her risk is still raised above the population28.
In our study, 87% (13 of 15) of results changed management for the patient. Even the two patients who had already received prophylactic surgery were additionally enrolled into cancer surveillance programmes. As aforementioned, the patients in which the results were not clinically actionable were a patient undergoing colorectal cancer treatment with a P/LP MSH6 variant, and a heterozygous carrier of MUTYH (an autosomal recessive condition). However, 100% (all 15) of P/LP variants changed management for the families. This high rate of actionability is not discovered in all cancer gene panel studies57.
Limitations
Demographics. As with any scientific study, this study too is not without limitations. These limitations are important to understand to enable critical review so that future studies may tackle what is left unanswered. The demographics are not representative of a general UK population: of 152 patients, 75.7% were female, and some ethnic minorities were over-represented. This is compounded by the small sample size. The skewed demographic may explain why common European P/LP variants, such as CHEK2 1100delC30,58, were not detected.
Additionally, we only included private patents from a single centre, and as such, local socioeconomic factors such as income and educational attainment could influence behaviour. Unlike on the NHS, all patients attending the centre were actively seeking testing. We also recognise that NHS eligibility criteria serve as guidance to healthcare professionals, and eligibility is also reviewed on a case-by-case basis30. Other differences in genetic testing between the NHS and private care include patient refusal, and not attending clinic appointments.
Data Collection and Analysis. We were limited by our reliance on family history and medical records which are not always complete. To evaluate psychosocial burdens, future studies including patient concern and satisfaction levels would be of value.
Cancer gene panels: promise and pitfalls
The promise of cancer gene panel testing
Panels tests for germline testing have generated enthusiasm amongst clinical genetics services and increased our knowledge base of cancer genotype–phenotype associations21,78.
Gene panels offer the promise of time-efficiency by testing multiple genes simultaneously59, which is especially useful for genetically heterogeneous conditions48,60 and in patients who have previously tested negative in genetic tests21. Massively parallel sequencing is also cost-efficient utilising current advances in technology and requiring a smaller amount of DNA1,6,21,61.
Panel testing is paving a path towards the future of personalised medicine. Detecting clinically-relevant information through gene panels leads to early cancer detection and possible changes in management45, more so than conventional gene testing30,62. Risk stratification32 and clinical outcome prediction31 could be more accurate through the use of panel tests. Identification of variant status also has prognostic and therapeutic benefits. For example, carriers of P/LP BRCA1/2 variants with breast cancer display sensitivity to platinum chemotherapy and PARP inhibitors7.
Pitfalls of cancer gene panels
The major challenge to gene panels is that our ability to interpret lags far behind our ability to sequence. The detection of VUS both in predictive and diagnostic testing renders the process more complex, both in terms of clinical management and counselling45. VUS have ramifications for clinical genetics services, with need for pre and post-test counselling, and our inability to explain ambiguous results of unknown deleteriousness to patients may cause more patient concern45,63,64. Studies on patient perspectives regarding gene panels have demonstrated their concerns about VUS rates, while recognising the potential positive impact on their health65, and the trust they place in healthcare professionals communicating genetic testing information66. The latter highlights the need for a more genome-educated medical community64,66,67, and dedicating resources to pre and post-test genetic counselling to help cope with the practical and psychological burdens associated with gene testing21.
Although standardisation of variant classification has proven difficult in the past34,68,69 The Cancer Variant Interpretation Group UK (CanVIG-UK) as well as the 2020 ACGS46 approach facilitate a standardised approach to classification and data sharing within NHS diagnostic labs. Internationally, the Clinical Genome (ClinGen) is striving to standardise approaches to variant classification, with gene-specific expert panels and a forum to resolve discrepant classifications.
There is also a need to standardise diagnostic reports on VUS to clarify to healthcare professionals the medical guidance associated with that variant64. Due to disparities in access to both research and genetic testing12, non-white ancestries have higher VUS rates70 as their reference panels are less well-defined, and ancestral branches differ in their genetic variation. Another area of ongoing research is the contribution of multiple variants to predisposition29.
VUS aside, detection of a P/LP variant is not always straightforward. If the variant is moderate risk, or is in a moderate-risk gene, parameters including risk estimates, phenotypic features, and actionability are not well-defined29. A discrepancy between genotype and phenotype may be detected, such as a moderate-risk gene in a high-risk family, or a highly pathogenic variant in a patient with unrelated symptoms. Such incidental or secondary findings are well described in the literature6,30,31. A well-known example is demonstrated by the Ohio Colorectal Cancer Prevention Initiative, where a high number of individuals with colorectal cancer had BRCA1/2 variants18, despite evidence showing BRCA1/2 does not confer a colorectal cancer risk.
Finally, there is concern that use of gene panels will raise ethical tensions, and large-scale implementation of gene panels needs to be both fair and appropriate. Factors to consider are financial sustainability, regulatory factors, and issues of equity71,72. At the rate at which gene tests are becoming available, it can be difficult to evaluate the genetic tests by the ACCE Framework, and their economic sustainability in universal healthcare systems such as the NHS73.
Key points
Eligibility criteria attempt to strike a balance between identifying high-risk patients and minimising the level of uncertainty. We have demonstrated that cancer predisposition variants are not always associated with a significant family or personal history. Almost half of all patients with a P/LP result would not have fulfilled eligibility criteria for genetic testing and would therefore have been missed. Our results support a genetic testing policy that is less stringent, but testing for genes with a high degree of association with personal or family histories.
Looking to the future: proceed, but with caution
There are multiple arguments to be made in favour of a broad approach to gene panel testing. Sequencing a larger number of affected and unaffected patients, then collating variants and associated features into a database will, in the long term, lead to enhanced classification of variants and understanding of their associated phenotypes across a multi-ethnic population1,30,45. Laboratories contribute coded germline findings to the Public Health England cancer registry, which is becoming an increasingly useful resource in practice, informing both prospective variant classification and assisting with review of existing classifications. The full potential of linking genetic data to the cancer registry has yet to be realised.
Limiting sequencing to patients with a strong personal or family history biases risk estimates, whereas a broad approach may reduce oversampling of severe cases and allow more reliable quantification of risks32,79. As our knowledge of individual variants and ability to call phenotypic consequences progresses, eligibility criteria may become more of a hindrance to both clinicians and patients32. Finally, we have yet to tap into the full scope of actionability of such variants. Development of targeted therapies74,75 and cancer screening algorithms based on genetic profiling76 are active areas of research.
There is disagreement on how to broaden our scope; how we go about simplifying access to genetic testing. This is an important area of future research. One approach is enhancing current policies on diagnostic testing of patients with cancer to enable more efficient and cost-effective cascade testing26. Delivering cancer predisposition gene testing through mainstreaming into routine oncological care would require remodelling of educational curricula and diagnostic clinical procedures, but can simplify access to genetic testing and benefit more patients77. The UK cancer genetics community is broadly in support of mainstreaming as specialist cancer genetics services do not have the capacity for the increasing demand33. Another approach is population-based screening to identify a cancer susceptibility gene, which may be a costly process, but it is argued to realise the true potential of screening47.
Our major bottleneck is accurate variant interpretation in the new era of big data. This bottleneck is the root of healthcare professionals’ hesitancy in embracing gene panels: ambiguous variant classification may trigger anxiety in patients, and at worst, lead to inappropriate tests and interventions21. The powerbrokers are bioinformaticians with an understanding of biology, or healthcare professionals and researchers equipped with the tools for understanding big data, who can transform raw primary sequences into variants with nuanced interpretations. This is another important area of future research.
To build a UK community of experts to deal with the influx in big genomic data, the Chief Medical Officer Professor Dame Sally Davies published her report ‘Generation Genome’, proposing some policies to lead the UK into the genomics era. These include centralised data analysis, harmonising genomics information across healthcare institutions, focusing on patient partnerships in patient-centric trials, and a focus on genomic education67. Some of these policies have sprouted with the 100,000 Genomes Project, helping us tap into the benefits of our single point-of-access system. Future local and regional UK-based research would provide a better idea of the current state, and where changes may be implemented.
There remain concerns about a less-restrictive policy which would need to be validated and reproduced prior to integration into clinical care. However, the only way to ensure the robustness of our data is to undertake more testing and validate this data. If validated, we have shown that for every 11 people tested, we find one P/LP variant which would alter management.
Data availability
The datasets generated during and analysed during the current study are not publicly available as although anonymised, they contain information that could in theory be identifiable. They are available from the corresponding author on reasonable request.
References
Taylor, A., Brady, A. F,, Frayling, I. M., Hanson, H., Tischkowitz, M., Turnbull, C., Side, L. & Group UKCG. Consensus for genes to be included on cancer panel tests offered by UK genetics services: Guidelines of the UK Cancer Genetics Group. J. Med. Genet. 16, 16. https://doi.org/10.1136/jmedgenet-2017-105188 (2018).
Beitsch, P. D. et al. Underdiagnosis of hereditary breast cancer: Are genetic testing guidelines a tool or an obstacle?. J. Clin. Oncol. 37(6), 453–460. https://doi.org/10.1200/JCO.18.01631 (2019).
Samadder, N. J. et al. Comparison of universal genetic testing vs guideline-directed targeted testing for patients with hereditary cancer syndrome. JAMA Oncol. 7(2), 230–237. https://doi.org/10.1001/jamaoncol.2020.6252 (2021).
Whitworth, J. et al. Comprehensive cancer-predisposition gene testing in an adult multiple primary tumor series shows a broad range of deleterious variants and atypical tumor phenotypes. Am. J. Human Genet. 12, 12. https://doi.org/10.1016/j.ajhg.2018.04.013 (2018).
National Collaborating Centre for Cancer (UK). Familial Breast Cancer: Classification and Care of People at Risk of Familial Breast Cancer and Management of Breast Cancer and Related Risks in People with a Family History of Breast Cancer. Cardiff (UK): National Collaborating Centre for Cancer (UK); 2013 Jun. (NICE Clinical Guidelines, No. 164.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK247567/
Walsh, T. et al. Mutations in 12 genes for inherited ovarian, fallopian tube, and peritoneal carcinoma identified by massively parallel sequencing. Proc. Natl. Acad. Sci. U.S.A. 108, 18032–18037. https://doi.org/10.1073/pnas.1115052108 (2011).
Rust, K. et al. Routine germline BRCA1 and BRCA2 testing in patients with ovarian carcinoma: analysis of the Scottish real-life experience. BJOG: Int. J. Obst. Gynaecol. 20, 20. https://doi.org/10.1111/1471-0528.15171 (2018).
Parkhurst, E., Calonico, E. & Abboy, S. Utilization of genetic testing for RET mutations in patients with medullary thyroid carcinoma: A single-center experience. J. Genet. Couns. 27, 27. https://doi.org/10.1007/s10897-018-0273-1 (2018).
Romei, C. et al. Twenty years of lesson learning: How does the RET genetic screening test impact the clinical management of medullary thyroid cancer?. Clin. Endocrinol. 82, 892–899. https://doi.org/10.1111/cen.12686 (2015).
Alsop, K. et al. Bowtell D and Mitchell G (2012) BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group [Erratum appears in J Clin Oncol. 2012 Nov 20;30(33):4180]. J. Clin. Oncol. 30, 2654–2663. https://doi.org/10.1200/JCO.2011.39.8545 (2012).
Wood, M. E. et al. Quality of cancer family history and referral for genetic counseling and testing among oncology practices: A pilot test of quality measures as part of the American Society of Clinical Oncology Quality Oncology Practice Initiative. J. Clin. Oncol. 32, 824–829. https://doi.org/10.1200/JCO.2013.51.4661 (2014).
Levy, D. E. et al. Underutilization of BRCA1/2 testing to guide breast cancer treatment: Black and Hispanic women particularly at risk. Genet. Med. 13, 349–355. https://doi.org/10.1097/GIM.0b013e3182091ba4 (2011).
Wright, J. D. et al. Underuse of BRCA testing in patients with breast and ovarian cancer. Am. J. Obstet. Gynecol. 214, 761–763. https://doi.org/10.1016/j.ajog.2016.02.011 (2016).
Deanna Cross, A. R. et al. Lynch syndrome screening patterns in colorectal cancer patients in a large multi-institutional cohort. Current Med. Res. 10, 146. https://doi.org/10.3121/cmr.2012.1100.ps1-08 (2012).
Lowery, J. T. et al. Understanding the contribution of family history to colorectal cancer risk and its clinical implications: A state-of-the-science review. Cancer 122, 2633–2645. https://doi.org/10.1002/cncr.30080 (2016).
Febbraro, T. et al. Adherence patterns to National Comprehensive Cancer Network (NCCN) guidelines for referral to cancer genetic professionals. Gynecol. Oncol. 138, 109–114. https://doi.org/10.1016/j.ygyno.2015.04.029 (2015).
Fiscella, K., Winters, P., Farah, S., Sanders, M. & Mohile, S. G. Do lung cancer eligibility criteria align with risk among Blacks and Hispanics?. PLoS ONE [Electronic Resource]. 10, e0143789. https://doi.org/10.1371/journal.pone.0143789 (2015).
Pearlman, R., Frankel, W. L., Swanson, B., Zhao, W., Yilmaz, A., Miller, K., Bacher, J., Bigley, C., Nelsen, L., Goodfellow, P. J., Goldberg, R. M., Paskett, E., Shields, P. G., Freudenheim, J. L., Stanich, P. P., Lattimer, I., Arnold, M., Liyanarachchi, S., Kalady, M., Heald, B., Greenwood, C., Paquette, I., Prues, M., Draper, D. J., Lindeman, C., Kuebler, J. P., Reynolds, K., Brell, J. M., Shaper, A. A., Mahesh, S., Buie, N., Weeman, K., Shine, K., Haut, M., Edwards, J., Bastola, S., Wickham, K., Khanduja, K. S., Zacks, R., Pritchard, C. C., Shirts, B. H., Jacobson, A., Allen, B., de la Chapelle, A., Hampel, H. and Ohio Colorectal Cancer Prevention Initiative Study G. Prevalence and spectrum of germline cancer susceptibility gene mutations among patients with early-onset colorectal cancer. JAMA Oncology. 3, 464–471. https://doi.org/10.1001/jamaoncol.2016.5194 (2016).
Fiederling, J., Shams, A. Z. & Haug, U. Validity of self-reported family history of cancer: A systematic literature review on selected cancers. Int. J. Cancer 139, 1449–1460. https://doi.org/10.1002/ijc.30203 (2016).
Albright, F. et al. Prostate cancer risk prediction based on complete prostate cancer family history. Prostate 75, 390–398. https://doi.org/10.1002/pros.22925 (2015).
Stanislaw, C., Xue, Y. & Wilcox, W. R. Genetic evaluation and testing for hereditary forms of cancer in the era of next-generation sequencing. Cancer Biol. Med. 13, 55–67. https://doi.org/10.28092/j.issn.2095-3941.2016.0002 (2016).
Augustinsson, A., Ellberg, C., Kristoffersson, U., Borg, A. & Olsson, H. Accuracy of self-reported family history of cancer, mutation status and tumor characteristics in patients with early onset breast cancer. Acta Oncol. 57, 595–603. https://doi.org/10.1080/0284186X.2017.1404635 (2018).
Lu, K. H., Wood, M. E., Daniels, M., Burke, C., Ford, J., Kauff, N. D., Kohlmann, W., Lindor, N. M., Mulvey, T. M., Robinson, L., Rubinstein, W. S., Stoffel, E. M., Snyder, C., Syngal, S., Merrill, J. K., Wollins, D. S., Hughes, K. S. and American Society of Clinical O. American Society of Clinical Oncology Expert Statement: Collection and use of a cancer family history for oncology providers. J. Clin. Oncol. 32, 833–840. https://doi.org/10.1200/JCO.2013.50.9257 (2014).
Mucci, L. A., Hjelmborg, J. B., Harris, J. R., Czene, K., Havelick, D. J., Scheike, T., Graff, R. E., Holst, K., Moller, S., Unger, R. H., McIntosh, C., Nuttall, E., Brandt, I., Penney, K. L., Hartman, M., Kraft, P., Parmigiani, G., Christensen, K., Koskenvuo, M., Holm, N. V., Heikkila, K., Pukkala, E., Skytthe, A., Adami, H. O., Kaprio, J. & Nordic Twin Study of Cancer C. Familial Risk and Heritability of Cancer Among Twins in Nordic Countries.[Erratum appears in JAMA. 2016 Feb 23;315(8):822; PMID: 26903347]. 1, 68–76 (2016).
Anand, P. et al. Cancer is a preventable disease that requires major lifestyle changes. Pharm. Res. 25, 2097–2116. https://doi.org/10.1007/s11095-008-9661-9 (2008).
Hampel, H. Genetic counseling and cascade genetic testing in Lynch syndrome. Fam. Cancer 15, 423–427. https://doi.org/10.1007/s10689-016-9893-5 (2016).
Manolio, T. A. et al. Finding the missing heritability of complex diseases. Nature 461, 747–753. https://doi.org/10.1038/nature08494 (2009).
Lee, A. J. et al. Incorporating truncating variants in PALB2, CHEK2, and ATM into the BOADICEA breast cancer risk model. Genet. Med. 18, 1190–1198. https://doi.org/10.1038/gim.2016.31 (2016).
Stratton, M. R. & Rahman, N. The emerging landscape of breast cancer susceptibility. Nat. Genet. 40, 17–22 (2008).
Prapa, M., Solomons, J. & Tischkowitz, M. The use of panel testing in familial breast and ovarian cancer. Clin. Med. 17, 568–572. https://doi.org/10.7861/clinmedicine.17-6-568 (2017).
Burke, W. Genetic tests: clinical validity and clinical utility. Current Protocols Human Genet. 81, 11–18. https://doi.org/10.1002/0471142905.hg0915s81 (2014).
Easton, D. F. et al. Gene-panel sequencing and the prediction of breast-cancer risk. N. Engl. J. Med. 372, 2243–2257. https://doi.org/10.1056/NEJMsr1501341 (2015).
Slade, I. et al. Development of cancer genetic services in the UK: A national consultation. Genome Med. 7, 18. https://doi.org/10.1186/s13073-015-0128-4 (2015).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424. https://doi.org/10.1038/gim.2015.30 (2015).
George, A. et al. Implementing rapid, robust, cost-effective, patient-centred, routine genetic testing in ovarian cancer patients. Sci. Rep. 6, 29506. https://doi.org/10.1038/srep29506 (2016).
Manchanda, R. et al. Cost-effectiveness of population screening for BRCA mutations in Ashkenazi Jewish women compared with family history-based testing. J. Natl. Cancer Inst. 107, 380. https://doi.org/10.1093/jnci/dju380 (2015).
Manchanda, R. et al. Cost-effectiveness of Population-Based BRCA1, BRCA2, RAD51C, RAD51D, BRIP1, PALB2 Mutation Testing in Unselected General Population Women. J. Natl. Cancer Inst. 18, 18. https://doi.org/10.1093/jnci/djx265 (2018).
Kentwell, M. et al. Mainstreaming cancer genetics: A model integrating germline BRCA testing into routine ovarian cancer clinics. Gynecol. Oncol. 145, 130–136. https://doi.org/10.1016/j.ygyno.2017.01.030 (2017).
National Genomic Test Directory. Testing Criteria for Rare and Inherited Disease. Available from: https://www.england.nhs.uk/publication/national-genomic-test-directories/.
Yang, S. et al. Underdiagnosis of hereditary breast and ovarian cancer in medicare patients: Genetic testing criteria miss the mark. Ann. Surg. Oncol. 25(10), 2925–2931. https://doi.org/10.1245/s10434-018-6621-4 (2018).
Tung, N. et al. Frequency of germline mutations in 25 cancer susceptibility genes in a sequential series of patients with breast cancer. J. Clin. Oncol. 34, 1460–1468. https://doi.org/10.1200/JCO.2015.65.0747 (2016).
Gardner, S. A. et al. Evaluation of a 27-gene inherited cancer panel across 630 consecutive patients referred for testing in a clinical diagnostic laboratory. Hereditary Cancer Clin. Pract. 16, 1. https://doi.org/10.1186/s13053-017-0083-8 (2018).
Muller, C. et al. Underdiagnosis of hereditary colorectal cancers among medicare patients: genetic testing criteria for lynch syndrome miss the mark. JCO Precis Oncol. 5, 1103. https://doi.org/10.1200/PO.21.00132 (2021).
Uson, P. L. S. Jr. et al. Germline cancer susceptibility gene testing in unselected patients with colorectal adenocarcinoma: A multicenter prospective study. Clin. Gastroenterol. Hepatol. 20, S1542-3565. https://doi.org/10.1016/j.cgh.2021.04.013 (2021).
Cheon, J. Y., Mozersky, J. & Cook-Deegan, R. Variants of uncertain significance in BRCA: A harbinger of ethical and policy issues to come?. Genome Medicine. 6, 121. https://doi.org/10.1186/s13073-014-0121-3 (2014).
Ellard, S., Baple, E., Callaway, A., Berry, I., Forrester, N., Turnbull, C., Owens, M., Eccles, D. M., Abbs, S., Scott, R., Deans, Z. C., Lester, T., Campbell, J., Newman, W. G., Ramsden, S. & McMullan, D. J. ACGS Best Practice Guidelines for Variant Classification in Rare Disease 2020. https://www.acgs.uk.com/media/11631/uk-practice-guidelines-for-variant-classification-v4-01-2020.pdf.
Foulkes, W. D., Knoppers, B. M. & Turnbull, C. Population genetic testing for cancer susceptibility: founder mutations to genomes. Nat. Rev. Clin. Oncol. 13, 41–54. https://doi.org/10.1038/nrclinonc.2015.173 (2016).
Kurian, A. W. et al. Clinical evaluation of a multiple-gene sequencing panel for hereditary cancer risk assessment. J. Clin. Oncol. 32, 2001–2009. https://doi.org/10.1200/JCO.2013.53.6607 (2014).
Rembold, C. M. Number needed to screen: development of a statistic for disease screening. BMJ 317, 307–312 (1998).
Auvinen, A. et al. Absolute effect of prostate cancer screening: Balance of benefits and harms by center within the european randomized study of prostate cancer screening [Erratum appears in Clin Cancer Res. 2016 Jul 15;22(14):3702; PMID: 27422205]. Clin. Cancer Res. 22, 243–249. https://doi.org/10.1158/1078-0432.CCR-15-0941 (2016).
Rebbeck, T. R., Kauff, N. D. & Domchek, S. M. Meta-analysis of risk reduction estimates associated with risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. J. Natl Cancer Inst. 101, 80–87. https://doi.org/10.1093/jnci/djn442 (2009).
Antoniou, A. et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies [Erratum appears in Am J Hum Genet. 2003 Sep;73(3):709]. Am. J. Human Genet. 72, 1117–1130 (2003).
Zhong, Q., Peng, H. L., Zhao, X., Zhang, L. & Hwang, W. T. Effects of BRCA1- and BRCA2-related mutations on ovarian and breast cancer survival: A meta-analysis. Clin. Cancer Res. 21, 211–220. https://doi.org/10.1158/1078-0432.CCR-14-1816 (2015).
Rennert, G. et al. MutYH mutation carriers have increased breast cancer risk. Cancer 118, 1989–1993. https://doi.org/10.1002/cncr.26506 (2012).
Out, A. A. et al. MUTYH gene variants and breast cancer in a Dutch case-control study. Breast Cancer Res. Treat. 134, 219–227. https://doi.org/10.1007/s10549-012-1965-0 (2012).
Ormondroyd, E. et al. “Not pathogenic until proven otherwise”: Perspectives of UK clinical genomics professionals toward secondary findings in context of a Genomic Medicine Multidisciplinary Team and the 100,000 Genomes Project. Genet. Med. 20, 320–328. https://doi.org/10.1038/gim.2017.157 (2018).
Johns, A. L. et al. Lost in translation: returning germline genetic results in genome-scale cancer research. Genome Med. 9, 41. https://doi.org/10.1186/s13073-017-0430-4 (2017).
Consortium CBCC-C. CHEK2 1100delC and susceptibility to breast cancer: A collaborative analysis involving 10,860 breast cancer cases and 9,065 controls from 10 studies. Am. J. Human Genet. 74, 1175–1182 (2004).
Buys, S. S. et al. A study of over 35,000 women with breast cancer tested with a 25-gene panel of hereditary cancer genes. Cancer 123, 1721–1730. https://doi.org/10.1002/cncr.30498 (2017).
LaDuca, H. et al. Utilization of multigene panels in hereditary cancer predisposition testing: Analysis of more than 2,000 patients. Genet. Med. 16, 830–837. https://doi.org/10.1038/gim.2014.40 (2014).
Payne, K., Gavan, S. P., Wright, S. J. & Thompson, A. J. Cost-effectiveness analyses of genetic and genomic diagnostic tests. Nat. Rev. Genet. 19, 235–246. https://doi.org/10.1038/nrg.2017.108 (2018).
Desmond, A. et al. Clinical actionability of multigene panel testing for hereditary breast and ovarian cancer risk assessment. JAMA Oncol. 1, 943–951. https://doi.org/10.1001/jamaoncol.2015.2690 (2015).
Domchek, S. M., Bradbury, A., Garber, J. E., Offit, K. & Robson, M. E. Multiplex genetic testing for cancer susceptibility: Out on the high wire without a net?. J. Clin. Oncol. 31, 1267–1270. https://doi.org/10.1200/JCO.2012.46.9403 (2013).
Eccles, B. K., Copson, E., Maishman, T., Abraham, J. E. & Eccles, D. M. Understanding of BRCA VUS genetic results by breast cancer specialists. BMC Cancer 15, 936. https://doi.org/10.1186/s12885-015-1934-1 (2015).
Frost, C. J. et al. Assessing patient readiness for personalized genomic medicine. J. Community Genet. 26, 26. https://doi.org/10.1007/s12687-018-0365-5 (2018).
Roberts, M. C., Taber, J. M. & Klein, W. M. Engagement with genetic information and uptake of genetic testing: The role of trust and personal cancer history. J. Cancer Educ. 33, 893–900. https://doi.org/10.1007/s13187-016-1160-9 (2018).
Davies S. Chief Medical Officer annual report 2016: Generation Genome. Department of Health and Social Care.
Amendola, L. M. et al. Performance of ACMG-AMP variant-interpretation guidelines among nine laboratories in the clinical sequencing exploratory research consortium [Erratum for Am J Hum Genet. 2016 Jun 2;98 (6):1067–1076; PMID: 27181684]. Am. J. Human Genet. 99, 247. https://doi.org/10.1016/j.ajhg.2016.06.001 (2016).
Balmana, J. et al. Conflicting Interpretation of genetic variants and cancer risk by commercial laboratories as assessed by the prospective registry of multiplex testing. J. Clin. Oncol. 34, 4071–4078 (2016).
Eggington, J. M. B. L. et al. Current Variant of Uncertain Significance Rates in BRCA1/2 and Lynch Syndrome Testing (MLH1, MSH2, MSH6, PMS2, EPCAM) (Myriad Genetic Laboratories Inc, 2012).
Botkin, J. R. et al. Points to consider: Ethical, legal, and psychosocial implications of genetic testing in children and adolescents. Am. J. Hum. Genet. 97, 6–21. https://doi.org/10.1016/j.ajhg.2015.05.022 (2015).
Minari, J., Brothers, K. B. & Morrison, M. Tensions in ethics and policy created by National Precision Medicine Programs. Hum. Genomics 12, 22. https://doi.org/10.1186/s40246-018-0151-9 (2018).
Pitini, E. et al. How is genetic testing evaluated? A systematic review of the literature. Eur. J. Hum. Genet. 26, 605–615. https://doi.org/10.1038/s41431-018-0095-5 (2018).
Diaz, L. A. Jr. & Le, D. T. PD-1 blockade in tumors with mismatch-repair deficiency. N. Engl. J. Med. 373, 1979. https://doi.org/10.1056/NEJMc1510353 (2015).
Le, D. T. et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science 357, 409–413. https://doi.org/10.1126/science.aan6733 (2017).
Dias, A., Kote-Jarai, Z., Mikropoulos, C. & Eeles, R. Prostate cancer germline variations and implications for screening and treatment. Cold Spring Harb. Perspect. Med. 03, 03. https://doi.org/10.1101/cshperspect.a030379 (2017).
Rahman, N. Mainstreaming genetic testing of cancer predisposition genes. Clin. Med. 14, 436–439. https://doi.org/10.7861/clinmedicine.14-4-436 (2014).
Breast Cancer Association Consortium. Breast cancer risk genes - association analysis in more than 113,000 women. N. Engl. J. Med. 384, 428–439. https://doi.org/10.1056/NEJMoa1913948 (2021).
Hu, C. et al. A population-based study of genes previously implicated in breast cancer. N. Engl. J. Med. 384, 440–451. https://doi.org/10.1056/NEJMoa2005936 (2021).
Acknowledgements
This study was supported by NIHR funding to The Biomedical Research Centre at The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust. Approval for this study was obtained from the Royal Marsden Hospital audit committee.
Author information
Authors and Affiliations
Contributions
T.A. wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
Professor Rosalind Eeles: 1. GU-ASCO meeting in San Francisco - Jan 2016 – Honorarium as speaker $500 2. RMH FR meeting – Nov 2017 – support from Janssen, honorarium as speaker £1100 (Title: Genetics and Prostate Cancer) 3. University of Chicago invited talk May 2018 – Honorarium as speaker $1000 4. EUR 200 educational honorarium paid by Bayer & Ipsen to attend GU Connect “Treatment sequencing for mCRPC patients within the changing landscape of mHSPC” at a venue at ESMO, Barcelona, 28 September 2019 5. Prostate Dx Advisory Panel – Member of external Expert Committee. 30th June 2002/3 hours/ £900. The remaining authors have no conflicts of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Andoni, T., Wiggins, J., Robinson, R. et al. Half of germline pathogenic and likely pathogenic variants found on panel tests do not fulfil NHS testing criteria. Sci Rep 12, 2507 (2022). https://doi.org/10.1038/s41598-022-06376-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-06376-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.