Abstract
Leprosy, a progressive, mutilating and highly stigmatized disease caused by Mycobacterium leprae (ML), continues to prevail in the developing world. This is due to the absence of rapid, specific and sensitive diagnostic tools for its early detection since the disease gets notified only with the advent of physical scarring in patients. This study reports the development of a Loop-mediated isothermal amplification (LAMP) technique for fast, sensitive and specific amplification of 16S rRNA gene of ML DNA for early detection of leprosy in resource-limited areas. Various parameters were optimized to obtain robust and reliable amplification of ML DNA. Blind clinical validation studies were performed which showed that this technique had complete concurrence with conventional techniques. Total absence of amplification of negative control DNA confirmed the specificity of this test. Various visual detection methods viz. colorimetric, turbidity differentiation and bridge flocculation were standardized to establish easy-to-read and rapid diagnosis. This technique eliminates the lack of accuracy and sensitivity in skin smear tests in patients and the requirement for expensive lab equipments and trained technicians. The technique holds promise for further expansion and has the potential to cater to the unmet needs of society for a cheap, highly-sensitive and robust rapid diagnosis of ML.
Similar content being viewed by others
Introduction
Leprosy, also known as Hansen’s disease, is a debilitating dermato-neurological disease caused by Mycobacterium leprae (ML). After the introduction of Multi-drug Therapy by World Health Organisation in 1984, attempts were made to curb the disease and several countries declared elimination of leprosy in the successive years. However, since 2019, an emergence of 2, 02, 226 new global cases have been observed, mainly in developing countries1. This figure is almost stable since the last decade which shows that a perpetuating reservoir of infection still exists. It indicates that the burden and transmission of this neglected tropical disease is still a major health concern all over the world. Preliminary diagnosis of leprosy is conventionally made by symptomatic observations, like hypo-pigmented patches on skin, ulcers, lesions, loss of sensations, limb and facial deformities2. The slit skin smear (SSS) test for acid fast bacilli (AFB) and histopathological examination is done for further confirmation of ML infection3, 4. Apart from taking days to obtain results and requirement of lab facilities and skilled technicians, major limitations with these diagnostic methods are lack of sensitivity (at least 104 AFB per gram of tissue is required for positive identification), false negatives and false diagnosis of Mycobacterium tuberculosis (MTB). Studies have shown that many patients who show negative AFB count in SSS test are actually positive for AFB load in the granuloma5. The genomic and morphological makeup of MTB is highly similar to ML as they share the same evolutionary lineage. This leads to misdiagnosis and mistreatment of patients for MTB instead of ML6.
An early and specific diagnosis of ML is, therefore, urgently required to prevent physical damage, morbidity and transmission. Researchers have come up with several advanced molecular methods including detection of specific markers of ML. Antibodies directed against the ML-specific phenolic glycolipid I (PGL-I) and leprosy IDRI diagnostic-1 (LID-1) make the basis of many serological tests7. Hooij et al.8 evaluated two recently designed field-friendly lateral flow assays (LFAs- the OnSite Leprosy Ab Rapid test and the in-house developed PGL-I up-converting phosphor (UCP)-LFA). PCR techniques and nucleic acid amplification techniques have proven to be great tools for diagnosing ML with high sensitivity and specificity. Recently, Beissner et al.9 developed a combined RT-qPCR method which simultaneously uses two PCR assays on different genes for increased efficiency. Cabral et al.10 detected the nasal carriage of ML in the household contacts of infected persons by using PCR. Similarly, several PCR and immunoassay based techniques have been explored to develop early and rapid diagnostic tools11,12,13,14,15,16,17. However, the use of these methods for rapid diagnosis of leprosy is limited due to drawbacks such as (i) lack of specificity, (ii) false negatives due to low bacterial load, (iii) false positives due to co-circulating antibodies from other infections and (iv) requirement of expensive equipments and trained labor. Even the newest detection techniques fail to detect 60% of paucibacillary ML infections3. As leprosy is endemic in areas where resources are poor, it is even more imperative to develop a test which, besides being sensitive and specific, is economical, rapid and user friendly.
Isothermal amplification methods are favored over traditional PCR methods for developing cheap, effective and rapid diagnostics as the requirement of expensive laboratory equipments like thermocyclers is eliminated, without compromising efficiency or sensitivity. Hence, isothermal amplification techniques have better scope and potential to be used in rapid diagnostics in developing economies. Over several isothermal-based techniques, the loop-mediated isothermal amplification technique (LAMP) has many applications in the field of point-of-care (POC) testing. It utilizes four to six primers to identify specific regions of the template which can be amplified at constant temperature, using DNA polymerase with high strand displacement activity. Therefore, DNA amplification can be completed in a single step by incubating the mixture of primers with polymerase and template in a reaction buffer using a simple heat block or water bath18. It can typically produce results with high yield and specificity in less than 30 min at a single temperature. These features make the technique rapid and portable which further add to the purpose of on-field applications using simple devices. LAMP technique is known to be well-suited for several molecular diagnostic applications ranging from the laboratory and POC screening of infectious agents for various diseases, food testing, environmental testing, etc.19,20,21. Diagnostic kits and techniques using LAMP have been developed for rapid detection of several difficult pathogenic agents for highly infectious diseases like tuberculosis22, leishmaniasis23, dengue24, HIV/AIDS25, zika virus disease 26, salmonellosis27, etc. More importantly, the advent of LAMP has led to improved diagnosis of neglected tropical diseases all over the world28,29,30,31.
The laboratory detection method for any nucleic acid amplification technique is generally post-reaction agarose gel electrophoresis. However, for on-field, simple, rapid and user-friendly endpoint detection, various amplicon detection methods have been explored by researchers that can be combined with LAMP technique to produce immediate and easy to read results. Esmatabadi et al.32 has reviewed a variety of detection techniques such as colorimetry, turbidometry, hybridization probes, lateral flow dipsticks, ELISA, functionalized gold nanoparticles, etc. that have potential to be combined with LAMP method for easy detection of amplification products. The objective of the present study was to make the ML detection technique rapid, easy to read as well as affordable. Therefore, different detection techniques like colorimetry, turbidity evaluation and bridge flocculation methods have been used for detection of LAMP amplification products.
Since, ML is uncultivable in vitro and possesses a highly reduced genome that has a high degree of identity with MTB genome, specific LAMP technique for ML detection has not been forthcoming, despite its innately unique benefits as a diagnostic tool for disease detection in poor and remote areas of the world. To our knowledge, current study is the first report on presenting LAMP as an efficient diagnostic tool for ML.
Methods
Institute approvals
This work was carried out with proper approval from the Institutional Ethics Committee (IEC) of Jamia Hamdard, New Delhi (Reference No. 3/19 dated March 14, 2019). Blood samples were obtained from leprosy patients after obtaining written informed consent at HAHC Hospital, Jamia Hamdard, New Delhi. Sample collection protocols and all methods in the study were performed with strict adherence to the guidelines and regulations of IEC, Jamia Hamdard, New Delhi. Work was also approved by Institutional Bio-Safety Committee (IBSC), Jamia Hamdard, New Delhi (Reference No. 3.1 dated May 15, 2019).
Materials
QIAamp Blood mini kit (Qiagen, India) was used for DNA extraction from clinical blood samples. Bacillus stearothermophillus DNA Polymerase 3.0 (New England Biolabs, UK) and primers (Integrated DNA Technologies, USA) were used for the nucleic acid amplification. Escherichia coli (strain MG1655, JH-Institute of Molecular Medicine, Jamia Hamdard, New Delhi) was used as double negative control. MTB DNA (strain H37RV, National Institute of Immunology, New Delhi) was used as negative control. Ethidium bromide (Sigma-Aldrich, USA), propidium iodide (Merck, USA) and SPRI (solid phase reversible immobilization) magnetic beads (Canvax, Spain) were used for detection of amplification products. All other chemicals, unless otherwise specified, were from Sigma-Aldrich (USA).
DNA Extraction
ML DNA was extracted from SSS samples of leprosy-positive subjects using the Proteinase K method33. Concentration of the extracted DNA was measured using microvolume spectrophotometer (NanoDrop 3300). Blood samples from patients were obtained in EDTA tubes and 300 μl of blood samples was used for genomic DNA extraction. DNA of E.coli was extracted using phenol–chloroform method as described by F. He with slight modifications34.
LAMP target selection and primer designing
LAMP assay utilizes three sets of primers viz. forward and backward outer primers (F3, B3), inner primers (FIP, BIP) and loop primers (LF, LB). These promote formation of ‘hairpin-like’ loop structures at the start of the reaction, making way for high degree of self-priming for DNA synthesis and the reaction becomes self-sustaining, producing robust template amplification35. For determining ML target sequences for primer designing, available literature was searched for DNA amplification methods, mainly PCR. Several gene sequences such as RLEP and its subtypes (RLEP2, RLEP3, RLEP4), 18-kDa, 16S rRNA, SodA, rpoT, Pra, etc. have been reported and used by researchers to design primers for PCR detection of ML36,37,38,39,40,41,42,43,44. As per the literature available, isothermal technique has not yet been used for DNA amplification for detection of ML DNA. RLEP, a short repetitive sequence of only 129 bp, has shown high specificity for ML detection amongst all PCR-based studies. But due to its extremely short length it is a difficult target for designing six primers required for LAMP technique and appropriate primers could not be obtained by any primer designer software. We therefore searched other gene targets using LAMP primer designer software (Optigene version 1.12, UK) and the selected primers are enlisted in Table 1.
Nucleic acid amplification and optimization
Detailed LAMP amplification technique is described by Nagamine et al.18. Briefly, 25 μl reaction mixture contained 0.2 μM outer primers (F3 and B3), 0.4 μM loop primers (LF and LB), 0.8 μM inner primers (FIP and BIP), optimized reaction buffer (20 mM Tris–HCl, 10 mM (NH4)2SO4, 150 mM KCl, 2 mM MgSO4, 0.1% Tween 20; pH 8.8), 200 nM dNTPs, 8 U Bacillus stearothermophilus DNA polymerase I and 2 μl template DNA. The reaction was incubated at 66 °C for 1 h and amplicons were initially analyzed by agarose gel electrophoresis using ethidium bromide (EtBr) staining. The method was optimized for reaction conditions such as reaction duration, temperature and heat source for the most efficient amplification conditions.
LAMP sensitivity and specificity
LAMP was performed using serial dilutions of template DNA to evaluate the sensitivity. The specificity of LAMP primers was determined by using MTB and E. coli DNA as negative controls to nullify any chance of cross reactivity.
Comparison with conventional method
To determine the rapidity and efficiency of LAMP as a nucleic acid amplification technique for ML detection, a comparison was made with conventional PCR method using protocol and PCR primers described by Donoghue et al. and Truman et al.38, 45. In brief, primers for ML-specific RLEP gene (RF: 5′ TGCATGTCATGGCCTTGAGG 3′, RR: 5′ CACCGATACCAGCGGCAGAA 3′) along with PCR reagents (reaction buffer, Taq polymerase, dNTPs) and samples were mixed and incubated in a thermocycler (Bio Rad, USA) with cycling conditions as follows: initial denaturation at 95° C for 10 min followed by one cycle of 94° C for 2 min, 58° C for 2 min and 72° C for 2 min. This was followed by 40 cycles of 94° C for 30 s, 60° C for 30 s and 72° C for 45 s. Final extension was done at 72° C for 10 min. The amplicons were visualized by 2% agarose gel electrophoresis.
Validation using clinical samples
Blind studies were done using random blood samples from eighteen ML and MTB infected patients to validate the LAMP method of detection. Of these, four were females and fourteen were males. Samples from patients were taken before the start of any therapy. Diagnosis was made based on their symptoms, microscopic detection and SSS test. Children and pregnant ladies were excluded from the study. DNA from blood samples were isolated using DNA extraction kit and LAMP was performed along with controls. Results were analyzed using EtBr-based gel electrophoresis.
Statistical analysis
Based on observations and outcomes, the sensitivity, specificity, positive predicted value (PPV) and negative predicted value (NPV) of clinical studies were calculated to determine the efficiency of LAMP method for ML detection.
Visual detection methods
Rapidity of a technique includes fast and convenient assessment of results. User-friendly visual detection methods for qualitative determination of DNA amplification methods were used apart from time-intensive conventional gel electrophoresis.
Colorimetric detection
DNA intercalating dye propidium iodide was used to differentiate between positive and negative reaction samples 1 μl of 1 mg/ml stock solution of the dye was used for each reaction mixture after amplification and incubated at room temperature for 1 min before visualizing under UV transilluminator.
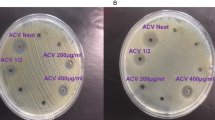
Visual detection of turbidity
Visual as well as spectroscopic detection of turbidity which is caused by release of free pyrophosphates during DNA multiplication was performed using increasing concentrations of magnesium ions in solution, as described by Esmatabadi et al.32.
Bridge flocculation assay
This method employs use of SPRI (solid phase reversible immobilization) beads where amplicons, if present, bind with the nanosized-magnetic beads and form a pellet, in contrast to the dispersed beads in the absence of amplified products46. The procedure was followed as described by Benjamin et al.47 with slight modification. 5 μl of amplified product was mixed and incubated with 1.5–1.8 times (v/v) bead solution at room temperature for 5 min. After magnetic separation of beads and 80% ethanol wash, 30 μl of flocculation buffer (100 mM sodium acetate and 1% v/v Tween20, pH 4.4) was added to the beads. Tubes were observed for flocculation immediately.
Results
LAMP primer design
To identify ML- specific LAMP primers, we designed primers for 16S rRNA and other genes (Table 1). None of the listed primers except those for 16S rRNA gave discernible template amplification. Therefore, we used the 16S rRNA primers for detection of ML. However, 16S rRNA-N primers showed amplification with both ML and MTB DNA samples, showing that these primers are not specific for ML. To overcome this, Basic Local Alignment Search Tool (NCBI BLAST) analysis of 16S rRNA gene of ML (GenBank Accession No. X53999) was done and the sequence was aligned with MTB 16S rRNA gene sequence (GenBank Accession No. NR_102810). Mismatched regions between the 16S rRNA sequences of both species were identified and these sequences were used to design specific LAMP primers (3 sets) for ML (16S rRNA-S: Table 1), using Optigene LAMP designer 1.15 software. Bioinformatic analysis of the targeted sequence showed no overlap with any other Mycobacterial species sequence. These primers selectively amplified ML, but not MTB, DNA thereby providing the distinguishing specificity to be used for further studies. Figure 1 shows the location of the 16S rRNA-S LAMP primers in the 16S rRNA genomic sequence.
Optimization of LAMP parameters
Optimization of the LAMP method was done by varying the reaction conditions to identify a set of conditions which would provide robust amplification signals, as described below.
-
(a)
Reaction temperature: LAMP reactions were performed at different temperatures (65° to 70 °C) to determine the optimum temperature necessary for the amplification. As shown in Fig. 2(a), beyond 66 °C amplification efficiency was greatly reduced, followed by no amplification at all at 70 °C. The temperature associated with highest amplification signal i.e. 66 °C was chosen for our method.
-
(b)
Reaction time: LAMP was carried out for different incubation periods (0 min, 15 min, 30 min, 45 min and 60 min) to specify the shortest time for amplification. After every time point, the reaction was ceased by denaturing the polymerase at 80 °C for 2 min. Figure 2(b) shows that 1 h reaction time is the minimum period for LAMP amplification.
-
(c)
Determination of sensitivity: The sensitivity of the method was evaluated by using various concentrations of template DNA for LAMP reactions. Lowest detectable DNA concentration governs the sensitivity of the method. The results, as indicated in Fig. 2(c), show the detection limit in picograms, with 5 pg/μl being the lowest concentration showing strong amplification. This anchors the robustness of the technique towards early diagnosis of ML infection even with low bacterial DNA load.
-
(d)
Source of heating: Assays were performed using different thermal sources viz. heat block and water bath, to identify the feasibility of the assay in poor resource settings. Figure 2(d) shows the comparison of heat sources depicting similar amplification results in both cases.
-
(e)
Specificity determination: The main aim of our study was to develop a LAMP detection method specific to ML to avoid cross-detection of MTB, a common and persistent technical obstacle. Our LAMP primers did not show any amplification signal with MTB DNA (Fig. 2e). Even at concentrations of 20 ng/μl of template MTB DNA, no amplification was observed, confirming the high degree of specificity of our ML-specific primers. Cross reactivity for primers was tested using E. coli as double negative control in each study.
Gel electrophoresis analysis of amplification reactions under different LAMP parameters. (a) Temperature optimization. Lanes: (M) Ladder, (1) 65 °C, (2) 66 °C, (3) 67 °C, (4) 68 °C, (5) 69 °C and (6) 70 °C (b) Reaction time optimization. Lanes: (1) 0 min, (2) 15 min, (3) 30 min, (4) 45 min and (5) 60 min, (c) Template concentration optimization. Lanes: (1) 1 ng, (2) 0.5 ng, (3) 0.1 ng, (4) 0.05 ng, (5) 0.01 ng, (6) 5 pg, (7) 1 pg, (d) Comparison of reaction heat source. Lanes 1–3: Heat block, Lanes 4–6: Water bath. (Lanes 1 & 4) ML DNA, (Lanes 2 & 5) MTB control, (Lanes 3 & 6) E.coli control, Lane M ladder, (e) Specificity of 16S rRNA-S primers. Lanes 1–3: 16S rRNA-S primers, Lanes 4–6: 16S rRNA-N primers. (Lanes 1 & 4) ML DNA, (Lanes 2 & 5) MTB control, (Lanes 3 & 6) E.coli control, Lane M is ladder.
Standardization of intensity vs. concentration
The intensity of amplification was detected by spectrophotometrically measuring absorbance of tenfold serial dilutions of amplified DNA at 400 nm. A calibration curve (Fig. 3) was obtained showing increasing amplification intensity with rise in DNA concentration. The R2 value of the curve was determined to be 0.995. Linear curve fitting was done to fit the amplification intensity response on increasing the input concentration. The equation for the best fit line was x = [(y − 0.018)/0.473] where x represents the input DNA concentration and y represents the absorbance at 400 nm, indicating the intensity of amplification.
Evaluation of LAMP technique in clinical samples
To validate the technique in clinical samples, blind studies were performed using random blood samples from patients diagnosed with either ML or MTB. Blood samples were selected for evaluation of this assay instead of skin smears so as to make this technique less painful and more convenient. Eighteen clinical samples were assessed with the LAMP technique and the results were cross-validated with the conventional detection method, as described in Materials and Methods. DNA extracted from blood samples, along with positive and negative controls, were screened for LAMP amplification (Fig. 4). Around twelve samples were found to be positive and six negative for ML by LAMP method. The same samples were tested by conventional method and the observation details along with results are given in Table 2. The results show complete diagnostic concurrence between LAMP technique and conventional technique, with 100% clinical specificity. The PPV and NPV too was 100% in LAMP as compared with conventional method.
Comparison of LAMP with regular PCR
So far, PCR has been seen as the only nucleic acid amplification technique available for molecular diagnosis of ML. We compared the efficiency and sensitivity of our LAMP technique with traditional PCR method. Figure 5 shows that LAMP gave similar results as regular PCR and, in fact, better visual bands in 60 min using a simple water bath. In contrast, PCR took more than two and a half hours using a thermocycler for detectable bands. This implies that LAMP is more efficient with regards to rapidity, resource utilization, and ease of detection as compared to conventional PCR method.
Comparative analysis between LAMP and regular PCR. Amplification was done using positive control and a suspected clinical sample by LAMP in lanes 1 and 2 and by PCR in Lanes 7 and 8, respectively. Others are negative controls viz. MTB control (Lanes 3 and 9), E.coli control (Lanes 4 and 10), no primer (Lanes 5 and 11) & no template (Lanes 6 and 12), Lanes L and M are ladders.
In recent years, several PCR methods with varying sensitivities and specificities using different target sequences have been published. A side-by-side comparison was made (Table 3) between some of those published studies with our LAMP technique of detection. It can be noted that LAMP has the quickest turnaround time to amplify the bacterial DNA in clinical blood samples and has eliminated the risk of false positives or false negatives. In Table 3, many of the references have used biopsy samples which are painful to collect and take 2 h or more for target amplification. Moreover, they were unable to achieve high sensitivity and specificity in their studies. The method by Beissner et al. reported comparable sensitivity and specificity but it used a combination of two techniques which made the procedure more complex and cost- and time-intensive. Therefore, it can be concluded that the LAMP method has the potential to be developed for clinical use for its rapidity, portability, high sensitivity and specificity.
Methods for detection of LAMP amplicons
-
(a)
Colorimetric detection: Apart from conventional gel electrophoresis for detecting DNA amplification, other detection methods for visual identification of amplified products were also used in order to enhance the ease and cost of operation. Propidium iodide was used to qualitatively identify positive LAMP amplification reactions without gel electrophoresis. This fluorescent dye intercalates between DNA strands and gives fluorescence under UV wavelength. Figure 6 shows propidium iodide dye detection of LAMP products where positive sample with amplified product fluoresced bright pink while negative samples appeared orange in color.
-
(b)
Turbidity visualization: During the amplification reaction, pyrophosphate ions are produced which, in the presence of magnesium ions, form magnesium pyrophosphate that precipitates in solution. The resulting turbidity can be visually detected. Difference in visual turbidity was observed between positive samples and negative controls (Fig. 7), constituting another basis of visual detection of amplification results.
-
(c)
Bridge flocculation method: This method is generally used to purify DNA amplicons by using SPRI magnetic beads. But here, it is re-purposed as a detection technique to determine the presence of LAMP amplification products. In the presence of magnetic field, the beads aggregate and amplified DNA get entangled with the beads forming floccules which prevent their re-dispersion after removal of the magnetic field. In the absence of amplification, beads re-disperse in the solution after removal of the magnetic field. Figure 8(a) shows the visual difference between positive and negative LAMP reactions using SPRI beads. Sensitivity of this detection method was also determined by using different dilutions of DNA for LAMP amplification and performing bridge flocculation assay for detection of products. Figure 8(b) shows visible flocculation with as low as 5 pg/μl template concentration. This shows the potential of this detection assay in combination with LAMP technique for easy and rapid point-of-care detection of ML DNA.
Detection by bridge flocculation method. (a) Visual flocculation of amplified product. Positive sample (1) shows distinct flocculation whereas MTB control (2) and No template control (3) appear brown with no flocculation (b) Sensitivity determination of flocculation method. Different dilutions, 1 ng/μl (1), 0.5 ng/μl (2), 0.05 ng/μl (3), 5 pg/μl (4), 0.5 pg/μl (5) template DNA were used for LAMP and bridge flocculation detection alongwith No template control (6).
Discussion
Early and accurate detection of ML is crucial not only for proper treatment regimen but also to lower the burden and transmission in endemic areas, which in almost all cases are in socioeconomically-deprived and access-limited regions of the world. Furthermore, specificity of ML detection is often compromised due to the presence of homologous sequences in other Mycobacterium species, most notably MTB. We report the development and standardization of a rapid, sensitive and economical method of detecting ML DNA using an optimized LAMP technique. Primers were designed that specifically amplified target regions of 16S rRNA gene of ML these primers could differentiate ML from closely-related MTB samples, forming the basis of a sensitive and specific diagnostic tool. Blind studies using 18 clinical samples, including both positive and negative samples, established the efficiency and robustness of the technique with 100% sensitivity, specificity, PPV and NPV. An intrinsic methodical limitation of this study is the small number of clinical samples used to validate our in vitro results. Although the challenges in identification and recruitment of patients in early stages of ML infection remain high, expanding the clinical sample size in future studies will help in eliminating any possible bias or inaccuracy in our proposed technique. The technique is suitable for detecting ML DNA even at picogram concentrations, making it highly sensitive to low bacterial load and can be applied for early diagnosis of the disease before any permanent physical mutilation. It has an additional advantage of having a short turnaround time to produce results using regular bench equipments like water bath or heat block. Point-wise analysis of our LAMP technique with prevalent and published conventional PCR methods indicates that this technique shows equivalent, if not enhanced, sensitivity for ML genomic DNA detection. Additionally, this technique can be combined with rapid detection methods like colorimetry, turbidometry and bridge flocculation assay for naked-eye visualization of positive reaction products, further making this diagnostic technique for point-of-care use easily readable and user-friendly. In resource-poor settings where rapid, inexpensive and on-site testing is required to detect the potential source of infection and transmission, this method could be utilized for improved and simplified monitoring of potential leprosy patients at early stages of infection. Besides early diagnosis of infection, this technique may prove to be useful in monitoring the reduction in bacterial load during the course of multi-drug therapy in infected patients. Also, this technique could be applied for transmission studies to investigate human-to-human transmission in household and community contacts.
Currently, leprosy is preliminarily diagnosed through observation of physical manifestations and slit skin smear test. Apart from being painful, skin biopsy-based tests are lengthy, lack sensitivity, require an equipped lab and trained personnel and often result in false positives or false negatives. Sophisticated molecular diagnostic techniques like quantitative real-time PCR are not suitable alternatives for simple, cheap and reliable on-field testing tools. Unlike most other pathogens, detection of ML is difficult due to the fact that the bacillus cannot be cultured in vitro. The LAMP technique for ML detection using blood samples and readily available, simple instruments alongside quick visible detection methods we have described in this study, has the scope to be further developed as a point-of-care testing unit in field settings that can complement or even replace traditional diagnostic methods.
References
https://www.who.int/data/gho/data/indicators/indicator-details/GHO/number-of-new-leprosy-cases. Accessed 11 Dec 2020.
Rodrigues, L. C. & Lockwood, D. N. Leprosy now: epidemiology, progress, challenges, and research gaps. Lancet Infect. Dis. 11(6), 464–470. https://doi.org/10.1016/S1473-3099(11)70006-8 (2011).
Sengupta, U. Recent laboratory advances in diagnostics and monitoring response to treatment in leprosy. Indian Dermatol. Online J. 10(2), 106. https://doi.org/10.4103/idoj.IDOJ_260_18 (2019).
Lastória, J. C. & de Abreu, M. A. M. M. Leprosy: a review of laboratory and therapeutic aspects-part 2. An. Bras. Dermatol. 89(3), 389. https://doi.org/10.1590/abd1806-4841.20142460 (2014).
Kumaran, S. M., Bhat, I. P., Madhukara, J., Rout, P. & Elizabeth, J. Comparison of bacillary index on slit skin smear with bacillary index of granuloma in leprosy and its relevance to present therapeutic regimens. Indian J. Dermatol. 60(1), 51–54. https://doi.org/10.4103/0019-5154.147791 (2015).
Britton, W. J. & Lockwood, D. N. J. Leprosy. Lancet Lond. Engl. 363(9416), 1209–1219. https://doi.org/10.1016/S0140-6736(04)15952-7 (2004).
Fabri, et al. Integrative literature review of the reported uses of serological tests in leprosy management. Rev. Soc. Bras. Med. Trop. 49(2), 158–164. https://doi.org/10.1590/0037-8682-0226-2015 (2016).
Hooij, et al. Field-friendly serological tests for determination of M. leprae -specific antibodies. Sci. Rep. 7(1), 8868. https://doi.org/10.1038/s41598-017-07803-7 (2017).
Beissner, et al. Development of a combined RLEP/16S rRNA (RT) qPCR assay for the detection of viable M. leprae from nasal swab samples. BMC Infect. Dis. 19(1), 753. https://doi.org/10.1186/s12879-019-4349-9 (2019).
Cabral, et al. Anti-PGL1 salivary IgA/IgM, serum IgG/IgM, and nasal Mycobacterium leprae DNA in individuals with household contact with leprosy. Int. J. Infect. Dis. 17(11), e1005–e1010. https://doi.org/10.1016/j.ijid.2013.05.011 (2013).
Wichitwechkarn et al. (1995) Detection of Mycobacterium leprae infection by PCR. J. Clin. Microbiol. 33(1): 45–49
Torres, et al. Comparison of PCR mediated amplification of DNA and the classical methods for detection of Mycobacterium leprae in different types of clinical samples in leprosy patients and contacts. Lepr. Rev. 74(1), 18–30 (2003).
Santos, et al. Use of the polymerase chain reaction in the diagnosis of leprosy. J. Med. Microbiol. 46(2), 170–172. https://doi.org/10.1099/00222615-46-2-170 (1997).
Chaitanya, et al. Mycobacterium leprae specific genomic target in the promoter region of probable 4-alpha-glucanotransferase (ML1545) gene with potential sensitivity for polymerase chain reaction based diagnosis of leprosy. Int. J. Mycobacteriol. 5(2), 135–141. https://doi.org/10.1016/j.ijmyco.2016.01.002 (2016).
Caleffi, et al. Use of the polymerase chain reaction to detect Mycobacterium leprae in urine. Braz. J. Med. Biol. Res. 45(2), 153–157. https://doi.org/10.1590/S0100-879X2012007500011 (2012).
Rudeeaneksin, et al. LightCyclerTM real-time PCR for rapid detection and quantitation of Mycobacterium leprae in skin specimens. FEMS Immunol. Med. Microbiol. 54(2), 263–270. https://doi.org/10.1111/j.1574-695X.2008.00472.x (2008).
Almeida, et al. Detection of Mycobacterium leprae DNA by polymerase chain reaction in the blood and nasal secretion of Brazilian household contacts. Mem. Inst. Oswaldo Cruz 99(5), 509–511. https://doi.org/10.1590/S0074-02762004000500009 (2004).
Nagamine, K., Hase, T. & Notomi, T. Accelerated reaction by loop-mediated isothermal amplification using loop primers. Mol. Cell. Probes 16(3), 223–229. https://doi.org/10.1006/mcpr.2002.0415 (2002).
Li, Y., Fan, P., Zhou, S. & Zhang, L. Loop-mediated isothermal amplification (LAMP): a novel rapid detection platform for pathogens. Microb. Pathog. 107, 54–61. https://doi.org/10.1016/j.micpath.2017.03.016 (2017).
Martzy, et al. Challenges and perspectives in the application of isothermal DNA amplification methods for food and water analysis. Anal. Bioanal. Chem. 411(9), 1695–1702. https://doi.org/10.1007/s00216-018-1553-1 (2019).
Karanis, et al. Development and preliminary evaluation of a loop-mediated isothermal amplification procedure for sensitive detection of cryptosporidium oocysts in fecal and water samples. Appl. Environ. Microbiol. 73(17), 5660–5662. https://doi.org/10.1128/AEM.01152-07 (2007).
WHO | The use of loop-mediated isothermal amplification (TB-LAMP) for the diagnosis of pulmonary tuberculosis: policy guidance. WHO. http://www.who.int/tb/publications/lamp-diagnosis-molecular/en/. Accessed 19 Apr 2020.
Nzelu, C. O., Kato, H. & Peters, N. C. Loop-mediated isothermal amplification (LAMP): an advanced molecular point-of-care technique for the detection of Leishmania infection. PLoS Negl. Trop. Dis. 13(11), e0007698. https://doi.org/10.1371/journal.pntd.0007698 (2019).
Parida, et al. Rapid detection and differentiation of dengue virus serotypes by a real-time reverse transcription-loop-mediated isothermal amplification assay. J. Clin. Microbiol. 43(6), 2895–2903. https://doi.org/10.1128/JCM.43.6.2895-2903.2005 (2005).
Singleton, et al. Electricity-free amplification and detection for molecular point-of-care diagnosis of HIV-1. PLoS ONE 9(11), e113693. https://doi.org/10.1371/journal.pone.0113693 (2014).
da Silva, et al. Development and validation of reverse transcription loop-mediated isothermal amplification (RT-LAMP) for rapid detection of ZIKV in mosquito samples from Brazil. Sci. Rep. 9(1). https://doi.org/10.1038/s41598-019-40960-5 (2019).
Kokkinos, P. A., Ziros, P. G., Bellou, M. & Vantarakis, Loop-mediated isothermal amplification (LAMP) for the detection of salmonella in food. Food Anal. Methods 7(2), 512–526. https://doi.org/10.1007/s12161-013-9748-8 (2014).
Njiru, et al. Loop-mediated isothermal amplification (LAMP) method for rapid detection of trypanosoma brucei rhodesiense. PLoS Negl. Trop. Dis. 2(2), e147. https://doi.org/10.1371/journal.pntd.0000147 (2008).
Diego, et al. Progress in loop-mediated isothermal amplification assay for detection of Schistosoma mansoni DNA: towards a ready-to-use test. Sci. Rep. 9(1). https://doi.org/10.1038/s41598-019-51342-2 (2019).
Seki, et al Loop-mediated isothermal amplification methods for diagnosis of bacterial meningitis. Front. Pediatr. 6. https://doi.org/10.3389/fped.2018.00057 (2019).
Cai, Z. H., Dai, Y. Y., Huang, L. Y., Zhang, W. S. & Guo, X. G. Diagnosis of mycoplasma pneumoniae by loop-mediated isothermal amplification: systematic review and meta-analysis. BMC Infect. Dis. 19(1), 173. https://doi.org/10.1186/s12879-019-3799-4 (2019).
Esmatabadi, et al. Techniques for evaluation of LAMP amplicons and their applications in molecular biology. Asian Pac. J. Cancer Prev. 16(17), 7409–7414. https://doi.org/10.7314/APJCP.2015.16.17.7409 (2015).
Jadhav, et al. Simplified PCR detection method for nasal Mycobacterium leprae. Int. J. Lepr. Mycobact. Dis. Off. Organ Int. Lepr. Assoc. 69(4), 299–307 (2001).
He, F. E. coli Genomic DNA Extraction. BIO-Protoc. 1(14). https://doi.org/10.21769/BioProtoc.97 (2011).
Notomi, et al. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 28(12), e63 (2000).
Turankar, et al. Comparative evaluation of PCR amplification of RLEP, 16S rRNA, rpoT and Sod A gene targets for detection of M. leprae DNA from clinical and environmental samples. Int. J. Mycobacteriol. 4(1), 54–59. https://doi.org/10.1016/j.ijmyco.2014.11.062 (2015).
Scollard, D. M., Gillis, T. P. & Williams, D. L. Polymerase chain reaction assay for the detection and identification of Mycobacterium leprae in patients in the United States. Am. J. Clin. Pathol. 109(5), 642–646. https://doi.org/10.1093/ajcp/109.5.642 (1998).
Donoghue, H. D., Holton, J. & Spigelman, M. PCR primers that can detect low levels of Mycobacterium leprae DNA. J. Med. Microbiol. 50(2), 177–182. https://doi.org/10.1099/0022-1317-50-2-177 (2001).
Yoon, et al. Evaluation of polymerase chain reaction amplification of Mycobacterium leprae-specific repetitive sequence in biopsy specimens from leprosy patients. J. Clin. Microbiol. 31(4), 895–899 (1993).
Banerjee, et al. Multiplex PCR technique could be an alternative approach for early detection of leprosy among close contacts - a pilot study from India. BMC Infect. Dis. 10, 252. https://doi.org/10.1186/1471-2334-10-252 (2010).
Jamil, et al. Use of polymerase chain reaction to assess efficacy of leprosy chemotherapy. The Lancet 342(8866), 264–268. https://doi.org/10.1016/0140-6736(93)91816-5 (1993).
Job, C. K., Jayakumar, J., Williams, D. L. & Gillis, T. P. Role of polymerase chain reaction in the diagnosis of early leprosy. Int. J. Lepr. Mycobact. Dis. Off. Organ Int. Lepr. Assoc. 65(4), 461–464 (1997).
Kampirapap, K., Singtham, N., Klatser, P.R. & Wiriyawipart, S. DNA amplification for detection of leprosy and assessment of efficacy of leprosy chemotherapy. Int. J. Lepr. Mycobact. Dis. Off. Organ Int. Lepr. Assoc. 66(1), 16–21 (1998).
Lini, N., Shankernarayan, N. P. & Dharmalingam, K. Quantitative real-time PCR analysis of Mycobacterium leprae DNA and mRNA in human biopsy material from leprosy and reactional cases. J. Med. Microbiol. 58(Pt 6), 753–759. https://doi.org/10.1099/jmm.0.007252-0 (2009).
Truman et al. Enumeration of Mycobacterium leprae Using Real-Time PCR. PLoS Negl. Trop. Dis. 2(11), e328. https://doi.org/10.1371/journal.pntd.0000328 (2008).
Wee, E. J. H., Lau, H. Y., Botella, J. R. & Trau, M. Re-purposing bridging flocculation for on-site, rapid, qualitative DNA detection in resource-poor settings. Chem. Commun. 51(27), 5828–5831. https://doi.org/10.1039/C4CC10068A (2015).
Ng, B. Y. C., Wee, E. J. H. , West, N. P. & Trau M. Rapid DNA detection of Mycobacterium tuberculosis-towards single cell sensitivity in point-of-care diagnosis. Sci. Rep. 5(1). https://doi.org/10.1038/srep15027 (2015).
Tiwari, et al. Evaluation of polymerase chain reaction in nerve biopsy specimens of patients with Hansen’s disease. J. Neurol. Sci. 380, 187–190. https://doi.org/10.1016/j.jns.2017.07.038 (2017).
Chaitanya, et al Analysis of a novel multiplex polymerase chain reaction assay as a sensitive tool for the diagnosis of indeterminate and tuberculoid forms of leprosy. http://www.ijmyco.org/article.asp?issn=2212-5531;year=2017;volume=6;issue=1;spage=1;epage=8;aulast=Chaitanya. Accessed 26 Mar 2020.
Azevedo, et al. qPCR detection of Mycobacterium leprae in biopsies and slit skin smear of different leprosy clinical forms. Braz. J. Infect. Dis. 21(1), 71–78. https://doi.org/10.1016/j.bjid.2016.09.017 (2017).
Acknowledgements
The authors thankfully acknowledge Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi for providing ML infected patient samples and National Institute of Immunology, New Delhi, for providing MTB DNA for the research work. The authors also acknowledge DST PURSE program and Jamia Hamdard Silver Jubilee PDF for providing support to the research.
Funding
Department of Science and Technology, Ministry of Science and Technology, India Grant No. SR/WOS-A/LS-294/2018.
Author information
Authors and Affiliations
Contributions
Conceptualization and supervision: S.K., F.J.A. Investigation and Methodology: N.G. Resources: N.G., U.S. Validation and analysis: U.S., S.K. Writing- Original draft: N.G. Writing- Review and editing: S.K., U.S., F.J.A.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Garg, N., Sahu, U., Kar, S. et al. Development of a Loop-mediated isothermal amplification (LAMP) technique for specific and early detection of Mycobacterium leprae in clinical samples. Sci Rep 11, 9859 (2021). https://doi.org/10.1038/s41598-021-89304-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-89304-2
This article is cited by
-
Development of a loop-mediated isothermal amplification (LAMP) assay for rapid visual detection of snakehead vesiculovirus (SHVV) in snakehead
Fisheries Science (2024)
-
Highly sensitive and rapid determination of Mycobacterium leprae based on real-time multiple cross displacement amplification
BMC Microbiology (2023)
-
Polymerase chain reaction and loop-mediated isothermal amplification targeting lic13162, lic20239, and lipL32 genes for leptospirosis diagnosis
Brazilian Journal of Microbiology (2022)
-
RLEP LAMP for the laboratory confirmation of leprosy: towards a point-of-care test
BMC Infectious Diseases (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.