Abstract
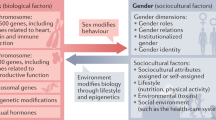
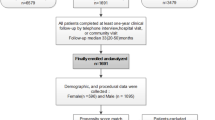
Although sex-related differences in the epidemiology, risk factors, clinical characteristics and outcomes of heart failure are well known, investigations in the past decade have shed light on an often overlooked aspect of heart failure: the influence of sex on treatment response. Sex-related differences in anatomy, physiology, pharmacokinetics, pharmacodynamics and psychosocial factors might influence the response to pharmacological agents, device therapy and cardiac rehabilitation in patients with heart failure. In this Review, we discuss the similarities between men and women in their response to heart failure therapies, as well as the sex-related differences in treatment benefits, dose–response relationships, and tolerability and safety of guideline-directed medical therapy, device therapy and cardiac rehabilitation. We provide insights into the unique challenges faced by men and women with heart failure, highlight potential avenues for tailored therapeutic approaches and call for sex-specific evaluation of treatment efficacy and safety in future research.
Key points
-
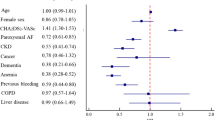
Men and women with heart failure with reduced ejection fraction derive similar benefits from pharmacotherapy with renin–angiotensin system inhibitors, angiotensin receptor–neprilysin inhibitors, β-blockers, mineralocorticoid receptor antagonists and sodium–glucose cotransporter 2 inhibitors.
-
In patients with heart failure with preserved ejection fraction, treatment heterogeneity by sex has been observed with angiotensin receptor–neprilysin inhibitors and spironolactone, whereby women seem to derive greater benefit than men.
-
Optimal doses of renin–angiotensin–aldosterone system inhibitors and β-blockers might be lower in women than in men, whereas adverse effects, such as dry cough and angio-oedema with angiotensin-converting enzyme inhibitors, might be more common in women than in men.
-
Among patients with left bundle branch block, women derive greater benefit from cardiac resynchronization therapy at a shorter QRS duration for reducing mortality than men.
-
In relation to the patient-oriented outcomes of quality of life and functional status, women derive similar benefits from baroreceptor activation therapy but less benefit from mitral valve intervention compared with men.
-
Women with heart failure might derive greater benefit from cardiac rehabilitation than men but have lower rates of enrolment and adherence.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Lam, C. S. P. et al. Sex differences in heart failure. Eur. Heart J. 40, 3859–3868c (2019).
Vaduganathan, M. et al. Do women and men respond similarly to therapies in contemporary heart failure clinical trials? JACC Heart Fail. 7, 267–271 (2019).
Butler, J. et al. Systolic blood pressure and incident heart failure in the elderly. The Cardiovascular Health Study and the Health, Ageing and Body Composition Study. Heart 97, 1304–1311 (2011).
He, J. et al. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch. Intern. Med. 161, 996–1002 (2001).
Magnussen, C. et al. Sex-specific epidemiology of heart failure risk and mortality in Europe: results from the biomarCaRE consortium. JACC Heart Fail. 7, 204–213 (2019).
Savji, N. et al. The association of obesity and cardiometabolic traits with incident HFpEF and HFrEF. JACC Heart Fail. 6, 701–709 (2018).
Uijl, A. et al. Risk factors for incident heart failure in age- and sex-specific strata: a population-based cohort using linked electronic health records. Eur. J. Heart Fail. 21, 1197–1206 (2019).
Lala, A. et al. Sex differences in heart failure. J. Card. Fail. 28, 477–498 (2022).
Ho, J. E. et al. Predicting heart failure with preserved and reduced ejection fraction: the international collaboration on heart failure subtypes. Circ. Heart Fail. 9, e003116 (2016).
Paulus, W. J. & Tschope, C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J. Am. Coll. Cardiol. 62, 263–271 (2013).
Sorimachi, H. et al. Pathophysiologic importance of visceral adipose tissue in women with heart failure and preserved ejection fraction. Eur. Heart J. 42, 1595–1605 (2021).
Stolfo, D. et al. Sex-based differences in heart failure across the ejection fraction spectrum: phenotyping, and prognostic and therapeutic implications. JACC Heart Fail. 7, 505–515 (2019).
Templin, C. et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N. Engl. J. Med. 373, 929–938 (2015).
Sliwa, K. et al. Clinical characteristics of patients from the worldwide registry on peripartum cardiomyopathy (PPCM): EURObservational Research Programme in conjunction with the Heart Failure Association of the European Society of Cardiology Study Group on PPCM. Eur. J. Heart Fail. 19, 1131–1141 (2017).
Denfeld, Q. E. et al. Characterizing sex differences in physical frailty phenotypes in heart failure. Circ. Heart Fail. 14, e008076 (2021).
Dewan, P. et al. Differential impact of heart failure with reduced ejection fraction on men and women. J. Am. Coll. Cardiol. 73, 29–40 (2019).
Ravera, A. et al. Quality of life in men and women with heart failure: association with outcome, and comparison between the Kansas City Cardiomyopathy Questionnaire and the EuroQol 5 dimensions questionnaire. Eur. J. Heart Fail. 23, 567–577 (2021).
McDonagh, T. A. et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42, 3599–3726 (2021).
Kittleson, M. M. et al. 2023 ACC expert consensus decision pathway on management of heart failure with preserved ejection fraction: a report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 81, 1835–1878 (2023).
McDonagh, T. A. et al. 2023 Focused update of the 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 44, 3627–3639 (2023).
Soldin, O. P. & Mattison, D. R. Sex differences in pharmacokinetics and pharmacodynamics. Clin. Pharmacokinet. 48, 143–157 (2009).
Tamargo, J. et al. Gender differences in the effects of cardiovascular drugs. Eur. Heart J. Cardiovasc. Pharmacother. 3, 163–182 (2017).
Soldin, O. P., Chung, S. H. & Mattison, D. R. Sex differences in drug disposition. J. Biomed. Biotechnol. 2011, 187103 (2011).
Anderson, G. D. Sex differences in drug metabolism: cytochrome P-450 and uridine diphosphate glucuronosyltransferase. J. Gend. Specif. Med. 5, 25–33 (2002).
Greenblatt, D. J. & von Moltke, L. L. Gender has a small but statistically significant effect on clearance of CYP3A substrate drugs. J. Clin. Pharmacol. 48, 1350–1355 (2008).
McDonough, A. A., Harris, A. N., Xiong, L. I. & Layton, A. T. Sex differences in renal transporters: assessment and functional consequences. Nat. Rev. Nephrol. 20, 21–36 (2023).
Bairey Merz, C. N. et al. Sex and the kidneys: current understanding and research opportunities. Nat. Rev. Nephrol. 15, 776–783 (2019).
Vree, T. B. et al. Lack of male-female differences in disposition and esterase hydrolysis of ramipril to ramiprilat in healthy volunteers after a single oral dose. ScientificWorldJournal 3, 1344–1358 (2003).
Michel, M. C., Foster, C., Brunner, H. R. & Liu, L. A systematic comparison of the properties of clinically used angiotensin II type 1 receptor antagonists. Pharmacol. Rev. 65, 809–848 (2013).
Vachharajani, N. N., Shyu, W. C., Smith, R. A. & Greene, D. S. The effects of age and gender on the pharmacokinetics of irbesartan. Br. J. Clin. Pharmacol. 46, 611–613 (1998).
Miller, J. A. et al. Gender differences in the renal response to renin-angiotensin system blockade. J. Am. Soc. Nephrol. 17, 2554–2560 (2006).
Luzier, A. B. et al. Gender-related effects on metoprolol pharmacokinetics and pharmacodynamics in healthy volunteers. Clin. Pharmacol. Ther. 66, 594–601 (1999).
Thurmann, P. A. et al. Tolerability of β-blockers metabolized via cytochrome P450 2D6 is sex-dependent. Clin. Pharmacol. Ther. 80, 551–553 (2006).
Labbe, L. et al. Effect of gender, sex hormones, time variables and physiological urinary pH on apparent CYP2D6 activity as assessed by metabolic ratios of marker substrates. Pharmacogenetics 10, 425–438 (2000).
Eugene, A. R. Metoprolol dose equivalence in adult men and women based on gender differences: pharmacokinetic modeling and simulations. Med. Sci. 4, 18 (2016).
McMurray, J. J. V. et al. Effects of sacubitril-valsartan versus valsartan in women compared with men with heart failure and preserved ejection fraction: insights from PARAGON-HF. Circulation 141, 338–351 (2020).
Berg, D. D. et al. Efficacy and safety of sacubitril/valsartan by dose level achieved in the PIONEER-HF Trial. JACC Heart Fail. 8, 834–843 (2020).
Wikstrand, J. et al. Dose of metoprolol CR/XL and clinical outcomes in patients with heart failure: analysis of the experience in metoprolol CR/XL randomized intervention trial in chronic heart failure (MERIT-HF). J. Am. Coll. Cardiol. 40, 491–498 (2002).
Lam, C. S. P. et al. Age, sex, and outcomes in heart failure with reduced EF: insights from the VICTORIA trial. JACC Heart Fail. 11, 1246–1257 (2023).
Granger, C. B. et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme inhibitors: the CHARM-Alternative trial. Lancet 362, 772–776 (2003).
McMurray, J. J. et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting-enzyme inhibitors: the CHARM-Added trial. Lancet 362, 767–771 (2003).
McMurray, J. J. V. et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 371, 993–1004 (2014).
Rossello, X. et al. Sex differences in mineralocorticoid receptor antagonist trials: a pooled analysis of three large clinical trials. Eur. J. Heart Fail. 22, 834–844 (2020).
Butt, J. H. et al. Efficacy and safety of dapagliflozin in men and women with heart failure with reduced ejection fraction: a prespecified analysis of the dapagliflozin and prevention of adverse outcomes in heart failure trial. JAMA Cardiol. 6, 678–689 (2021).
Zannad, F. et al. SGLT2 inhibitors in patients with heart failure with reduced ejection fraction: a meta-analysis of the EMPEROR-Reduced and DAPA-HF trials. Lancet 396, 819–829 (2020).
Shekelle, P. G. et al. Efficacy of angiotensin-converting enzyme inhibitors and beta-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status: a meta-analysis of major clinical trials. J. Am. Coll. Cardiol. 41, 1529–1538 (2003).
Garg, R. & Yusuf, S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE Inhibitor Trials. JAMA 273, 1450–1456 (1995).
Young, J. B. et al. Mortality and morbidity reduction with candesartan in patients with chronic heart failure and left ventricular systolic dysfunction: results of the CHARM low-left ventricular ejection fraction trials. Circulation 110, 2618–2626 (2004).
Ghali, J. K., Piña, I. L., Gottlieb, S. S., Deedwania, P. C. & Wikstrand, J. C. Metoprolol CR/XL in female patients with heart failure: analysis of the experience in Metoprolol Extended-Release Randomized Intervention Trial in Heart Failure (MERIT-HF). Circulation 105, 1585–1591 (2002).
Zannad, F. et al. Eplerenone in patients with systolic heart failure and mild symptoms. N. Engl. J. Med. 364, 11–21 (2011).
Packer, M. et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N. Engl. J. Med. 383, 1413–1424 (2020).
Swedberg, K. et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 376, 875–885 (2010).
O’Meara, E. et al. Sex differences in clinical characteristics and prognosis in a broad spectrum of patients with heart failure: results of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) program. Circulation 115, 3111–3120 (2007).
Lam, C. S. P. et al. Sex differences in clinical characteristics and outcomes in elderly patients with heart failure and preserved ejection fraction: the Irbesartan in Heart Failure with Preserved Ejection Fraction (I-PRESERVE) trial. Circulation. Heart Fail. 5, 571–578 (2012).
Cleland, J. G. F. et al. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur. Heart J. 27, 2338–2345 (2006).
Vaduganathan, M. et al. SGLT-2 inhibitors in patients with heart failure: a comprehensive meta-analysis of five randomised controlled trials. Lancet 400, 757–767 (2022).
Dewan, P. et al. Interactions between left ventricular ejection fraction, sex and effect of neurohumoral modulators in heart failure. Eur. J. Heart Fail. 22, 898–901 (2020).
Pitt, B. et al. Spironolactone for heart failure with preserved ejection fraction. N. Engl. J. Med. 370, 1383–1392 (2014).
Merrill, M., Sweitzer, N. K., Lindenfeld, J. & Kao, D. P. Sex differences in outcomes and responses to spironolactone in heart failure with preserved ejection fraction: a secondary analysis of TOPCAT trial. Jacc. Heart Fail. 7, 228–238 (2019).
Solomon, S. D. et al. Influence of ejection fraction on outcomes and efficacy of spironolactone in patients with heart failure with preserved ejection fraction. Eur. Heart J. 37, 455–462 (2016).
Chung, A. K. et al. Women have higher left ventricular ejection fractions than men independent of differences in left ventricular volume: the Dallas Heart Study. Circulation 113, 1597–1604 (2006).
Poppe, K. K. et al. Ethnic-specific normative reference values for echocardiographic LA and LV size, LV mass, and systolic function: the EchoNoRMAL study. JACC: Cardiovasc. Imaging 8, 656–665 (2015).
Dewan, P. et al. Sex-related differences in heart failure with preserved ejection fraction. Circulation. Heart Fail. 12, e006539 (2019).
Benedict, C. R. et al. Comparative neurohormonal responses in patients with preserved and impaired left ventricular ejection fraction: results of the Studies of Left Ventricular Dysfunction (SOLVD) Registry. The SOLVD Investigators. J. Am. Coll. Cardiol. 22, 146A–153A (1993).
Gori, M. et al. Sex-specific cardiovascular structure and function in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 16, 535–542 (2014).
Rathore, S. S., Wang, Y. & Krumholz, H. M. Sex-based differences in the effect of digoxin for the treatment of heart failure. N. Engl. J. Med. 347, 1403–1411 (2002).
Adams, K. F. et al. Relationship of serum digoxin concentration to mortality and morbidity in women in the digitalis investigation group trial: a retrospective analysis. J. Am. Coll. Cardiol. 46, 497–504 (2005).
Group, C. T. S. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N. Engl. J. Med. 316, 1429–1435 (1987).
Packer, M. et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N. Engl. J. Med. 334, 1349–1355 (1996).
Pitt, B. et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N. Engl. J. Med. 341, 709–717 (1999).
Santema, B. T. et al. Identifying optimal doses of heart failure medications in men compared with women: a prospective, observational, cohort study. Lancet 394, 1254–1263 (2019).
Packer, M. et al. Comparative effects of low and high doses of the angiotensin-converting enzyme inhibitor, lisinopril, on morbidity and mortality in chronic heart failure. ATLAS Study Group. Circulation 100, 2312–2318 (1999).
Ferreira, J. P. et al. Dosing of losartan in men versus women with heart failure with reduced ejection fraction: the HEAAL trial. Eur. J. Heart Fail. 23, 1477–1484 (2021).
Rosano, G. M. C. et al. Gender differences in the effect of cardiovascular drugs: a position document of the Working Group on Pharmacology and Drug Therapy of the ESC. Eur. Heart J. 36, 2677–2680 (2015).
Zopf, Y. et al. Women encounter ADRs more often than do men. Eur. J. Clin. Pharmacol. 64, 999–1004 (2008).
Kando, J. C., Yonkers, K. A. & Cole, J. O. Gender as a risk factor for adverse events to medications. Drugs 50, 1–6 (1995).
Rodenburg, E. M., Stricker, B. H. & Visser, L. E. Sex differences in cardiovascular drug-induced adverse reactions causing hospital admissions. Br. J. Clin. Pharmacol. 74, 1045–1052 (2012).
Hreiche, R., Morissette, P. & Turgeon, J. Drug-induced long QT syndrome in women: review of current evidence and remaining gaps. Gend. Med. 5, 124–135 (2008).
Tromp J, E. J. et al. Global variations according to sex in patients hospitalized for heart failure in the REPORT-HF registry. JACC: Heart Fail. 11, 1262–1271 (2023).
Rademaker, M. Do women have more adverse drug reactions? Am. J. Clin. Dermatol. 2, 349–351 (2001).
Bots, S. H. et al. Adverse drug reactions to guideline-recommended heart failure drugs in women: a systematic review of the literature. Jacc. Heart Fail. 7, 258–266 (2019).
Kostis, J. B. et al. Adverse effects of enalapril in the studies of left ventricular dysfunction (SOLVD). SOLVD investigators. Am. Heart J. 131, 350–355 (1996).
Do, T. P. et al. A database cohort study to assess the risk of angioedema among patients with heart failure initiating angiotensin-converting enzyme inhibitors in the USA. Am. J. Cardiovasc. Drugs 18, 205–211 (2018).
Lopes, R. J., Lourenço, A. P., Mascarenhas, J., Azevedo, A. & Bettencourt, P. Safety of spironolactone use in ambulatory heart failure patients. Clin. Cardiol. 31, 509–513 (2008).
Wang, X. et al. Sex differences in characteristics, outcomes, and treatment response with dapagliflozin across the range of ejection fraction in patients with heart failure: insights from DAPA-HF and DELIVER. Circulation 147, 624–634 (2023).
Lam, C. S. P. How to incorporate sex and gender into the design of cardiovascular clinical trials. Circulation 145, 499–501 (2022).
Gaborit, N. et al. Gender-related differences in ion-channel and transporter subunit expression in non-diseased human hearts. J. Mol. Cell Cardiol. 49, 639–646 (2010).
Odening, K. E. & Koren, G. How do sex hormones modify arrhythmogenesis in long QT syndrome? Sex hormone effects on arrhythmogenic substrate and triggered activity. Heart Rhythm. 11, 2107–2115 (2014).
Liu, S., Yuan, S., Kongstad, O. & Olsson, S. B. Gender differences in the electrophysiological characteristics of atrioventricular conduction system and their clinical implications. Scand. Cardiovasc. J. 35, 313–317 (2001).
Macfarlane, P. W., McLaughlin, S. C., Devine, B. & Yang, T. F. Effects of age, sex, and race on ECG interval measurements. J. Electrocardiol. 27, 14–19 (1994).
Hnatkova, K., Smetana, P., Toman, O., Schmidt, G. & Malik, M. Sex and race differences in QRS duration. Europace 18, 1842–1849 (2016).
Rautaharju, P. M. et al. Sex differences in the evolution of the electrocardiographic QT interval with age. Can. J. Cardiol. 8, 690–695 (1992).
Rautaharju, P. M., Mason, J. W. & Akiyama, T. New age- and sex-specific criteria for QT prolongation based on rate correction formulas that minimize bias at the upper normal limits. Int. J. Cardiol. 174, 535–540 (2014).
Kurokawa, J., Kodama, M., Clancy, C. E. & Furukawa, T. Sex hormonal regulation of cardiac ion channels in drug-induced QT syndromes. Pharmacol. Ther. 168, 23–28 (2016).
Okura, H. et al. Age- and gender-specific changes in the left ventricular relaxation: a Doppler echocardiographic study in healthy individuals. Circ. Cardiovasc. Imaging 2, 41–46 (2009).
Krumholz, H. M., Larson, M. & Levy, D. Sex differences in cardiac adaptation to isolated systolic hypertension. Am. J. Cardiol. 72, 310–313 (1993).
Cheng, S. et al. Correlates of echocardiographic indices of cardiac remodeling over the adult life course: longitudinal observations from the Framingham Heart Study. Circulation 122, 570–578 (2010).
Umetani, K., Singer, D. H., McCraty, R. & Atkinson, M. Twenty-four hour time domain heart rate variability and heart rate: relations to age and gender over nine decades. J. Am. Coll. Cardiol. 31, 593–601 (1998).
Ramaekers, D., Ector, H., Aubert, A. E., Rubens, A. & Van de Werf, F. Heart rate variability and heart rate in healthy volunteers. Is the female autonomic nervous system cardioprotective? Eur. Heart J. 19, 1334–1341 (1998).
Huikuri, H. V. et al. Sex-related differences in autonomic modulation of heart rate in middle-aged subjects. Circulation 94, 122–125 (1996).
Liao, D. et al. Age, race, and sex differences in autonomic cardiac function measured by spectral analysis of heart rate variability – the ARIC study. Atherosclerosis risk in communities. Am. J. Cardiol. 76, 906–912 (1995).
Al-Khatib, S. M. et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 138, e272–e391 (2018).
Zeppenfeld, K. et al. 2022 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 43, 3997–4126 (2022).
Chia, Y. M. F. et al. Disparity between indications for and utilization of implantable cardioverter defibrillators in Asian patients with heart failure. Circ. Cardiovasc. Qual. Outcomes 10, e003651 (2017).
Camm, A. J. & Nisam, S. European utilization of the implantable defibrillator: has 10 years changed the ‘enigma’? Europace 12, 1063–1069 (2010).
Curtis, L. H. et al. Sex differences in the use of implantable cardioverter-defibrillators for primary and secondary prevention of sudden cardiac death. JAMA 298, 1517–1524 (2007).
Hernandez, A. F. et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA 298, 1525–1532 (2007).
MacFadden, D. R., Tu, J. V., Chong, A., Austin, P. C. & Lee, D. S. Evaluating sex differences in population-based utilization of implantable cardioverter-defibrillators: role of cardiac conditions and noncardiac comorbidities. Heart Rhythm. 6, 1289–1296 (2009).
Mezu, U., Ch, I., Halder, I., London, B. & Saba, S. Women and minorities are less likely to receive an implantable cardioverter defibrillator for primary prevention of sudden cardiac death. Europace 14, 341–344 (2012).
Al-Khatib, S. M. et al. Trends in use of implantable cardioverter-defibrillator therapy among patients hospitalized for heart failure: have the previously observed sex and racial disparities changed over time? Circulation 125, 1094–1101 (2012).
Patel, N. J. et al. Gender, racial, and health insurance differences in the trend of implantable cardioverter-defibrillator (ICD) utilization: a United States experience over the last decade. Clin. Cardiol. 39, 63–71 (2016).
Bradfield, J., Warner, A. & Bersohn, M. M. Low referral rate for prophylactic implantation of cardioverter-defibrillators in a tertiary care medical center. Pacing Clin. Electrophysiol. 32, S194–S197 (2009).
Johnson, A. E., Bell, Y. K., Hamm, M. E., Saba, S. F. & Myaskovsky, L. A qualitative analysis of patient-related factors associated with implantable cardioverter defibrillator acceptance. Cardiol. Ther. 9, 421–432 (2020).
Hess, P. L. et al. Response by Hess et al. to letter regarding article, “Sex and race/ethnicity differences in implantable cardioverter-defibrillator counseling and use among patients hospitalized with heart failure: findings from the Get With The Guidelines-Heart Failure Program”. Circulation 135, e22–e23 (2017).
Gravelin, L. M. et al. Use of a screening tool improves appropriate referral to an electrophysiologist for implantable cardioverter-defibrillators for primary prevention of sudden cardiac death. Circ. Cardiovasc. Qual. Outcomes 4, 152–156 (2011).
Thalappillil, A. et al. Impact of an automated best practice alert on sex and race disparities in implantable cardioverter-defibrillator therapy. J. Am. Heart Assoc. 11, e023669 (2022).
Buxton, A. E. et al. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial investigators. N. Engl. J. Med. 341, 1882–1890 (1999).
Moss, A. J. et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N. Engl. J. Med. 346, 877–883 (2002).
Kadish, A. et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N. Engl. J. Med. 350, 2151–2158 (2004).
Hohnloser, S. H. et al. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N. Engl. J. Med. 351, 2481–2488 (2004).
Bardy, G. H. et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N. Engl. J. Med. 352, 225–237 (2005).
Steinbeck, G. et al. Defibrillator implantation early after myocardial infarction. N. Engl. J. Med. 361, 1427–1436 (2009).
Køber, L. et al. Defibrillator implantation in patients with nonischemic systolic heart failure. N. Engl. J. Med. 375, 1221–1230 (2016).
Russo, A. M. et al. Influence of gender on arrhythmia characteristics and outcome in the Multicenter UnSustained Tachycardia Trial. J. Cardiovasc. Electrophysiol. 15, 993–998 (2004).
Russo, A. M. et al. Primary prevention with defibrillator therapy in women: results from the Sudden Cardiac Death in Heart Failure Trial. J. Cardiovasc. Electrophysiol. 19, 720–724 (2008).
Albert, C. M. et al. Sex differences in outcome after implantable cardioverter defibrillator implantation in nonischemic cardiomyopathy. Am. Heart J. 156, 367–372 (2008).
Ghanbari, H. et al. Effectiveness of implantable cardioverter-defibrillators for the primary prevention of sudden cardiac death in women with advanced heart failure: a meta-analysis of randomized controlled trials. Arch. Intern. Med. 169, 1500–1506 (2009).
Santangeli, P. et al. Gender differences in clinical outcome and primary prevention defibrillator benefit in patients with severe left ventricular dysfunction: a systematic review and meta-analysis. Heart Rhythm. 7, 876–882 (2010).
Barra, S. et al. Do women benefit equally as men from the primary prevention implantable cardioverter-defibrillator? Europace 20, 897–901 (2018).
Sticherling, C. et al. Sex differences in outcomes of primary prevention implantable cardioverter-defibrillator therapy: combined registry data from eleven European countries. Europace 20, 963–970 (2018).
Zeitler, E. P. et al. Primary prevention implantable cardioverter-defibrillators and survival in older women. JACC Heart Fail. 3, 159–167 (2015).
Tompkins, C. M. et al. Sex differences in inappropriate ICD device therapies: MADIT-II and MADIT-CRT. J. Cardiovasc. Electrophysiol. 28, 94–102 (2017).
Knops, R. E. et al. Subcutaneous or transvenous defibrillator therapy. N. Engl. J. Med. 383, 526–536 (2020).
Gold, M. R. et al. Primary results from the understanding outcomes with the S-ICD in primary prevention patients with low ejection fraction (UNTOUCHED) trial. Circulation 143, 7–17 (2021).
Han, J. K. & Russo, A. M. Underrepresentation of women in implantable cardioverter defibrillator trials. Am. Heart J. Plus 14, 100120 (2022).
Epstein, A. E. et al. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation 127, e283–e352 (2013).
Glikson, M. et al. 2021 ESC guidelines on cardiac pacing and cardiac resynchronization therapy. Eur. Heart J. 42, 3427–3520 (2021).
Abraham, W. T. et al. Cardiac resynchronization in chronic heart failure. N. Engl. J. Med. 346, 1845–1853 (2002).
Bristow, M. R. et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N. Engl. J. Med. 350, 2140–2150 (2004).
Cleland, J. G. et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N. Engl. J. Med. 352, 1539–1549 (2005).
Moss, A. J. et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N. Engl. J. Med. 361, 1329–1338 (2009).
Tang, A. S. et al. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N. Engl. J. Med. 363, 2385–2395 (2010).
Linde, C. et al. Randomized trial of cardiac resynchronization in mildly symptomatic heart failure patients and in asymptomatic patients with left ventricular dysfunction and previous heart failure symptoms. J. Am. Coll. Cardiol. 52, 1834–1843 (2008).
Linde, C., Gold, M., Abraham, W. T. & Daubert, J. C. Baseline characteristics of patients randomized in the resynchronization reverses remodeling in systolic left ventricular dysfunction (REVERSE) study. Congest. Heart Fail. 14, 66–74 (2008).
Arshad, A. et al. Cardiac resynchronization therapy is more effective in women than in men: the MADIT-CRT (Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy) trial. J. Am. Coll. Cardiol. 57, 813–820 (2011).
Zabarovskaja, S. et al. Women have better long-term prognosis than men after cardiac resynchronization therapy. Europace 14, 1148–1155 (2012).
Zusterzeel, R. et al. Sex-specific mortality risk by QRS morphology and duration in patients receiving CRT: results from the NCDR. J. Am. Coll. Cardiol. 64, 887–894 (2014).
Hsu, J. C. et al. Predictors of super-response to cardiac resynchronization therapy and associated improvement in clinical outcome: the MADIT-CRT (multicenter automatic defibrillator implantation trial with cardiac resynchronization therapy) study. J. Am. Coll. Cardiol. 59, 2366–2373 (2012).
Linde, C. et al. The interaction of sex, height, and QRS duration on the effects of cardiac resynchronization therapy on morbidity and mortality: an individual-patient data meta-analysis. Eur. J. Heart Fail. 20, 780–791 (2018).
Ali, N. et al. Comparison of methods for delivering cardiac resynchronization therapy: an acute electrical and haemodynamic within-patient comparison of left bundle branch area, His bundle, and biventricular pacing. Europace 25, 1060–1067 (2023).
Ezzeddine, F. M. et al. Outcomes of conduction system pacing for cardiac resynchronization therapy in patients with heart failure: a multicenter experience. Heart Rhythm. 20, 863–871 (2023).
Loring, Z. et al. Left bundle branch block predicts better survival in women than men receiving cardiac resynchronization therapy: long-term follow-up of ∼ 145,000 patients. JACC Heart Fail. 1, 237–244 (2013).
Zusterzeel, R. et al. Cardiac resynchronization therapy in women: US Food and Drug Administration meta-analysis of patient-level data. JAMA Intern. Med. 174, 1340–1348 (2014).
Woods, B. et al. Individual patient data network meta-analysis of mortality effects of implantable cardiac devices. Heart 101, 1800–1806 (2015).
Lee, N. S., Lin, F. & Birgersdotter-Green, U. Should women have different ECG criteria for CRT than men? J. Cardiol. 70, 1–6 (2017).
Zusterzeel, R. et al. Toward sex-specific guidelines for cardiac resynchronization therapy? J. Cardiovasc. Transl. Res. 9, 12–22 (2016).
Wilkoff, B. L. et al. Adaptive versus conventional cardiac resynchronisation therapy in patients with heart failure (AdaptResponse): a global, prospective, randomised controlled trial. Lancet 402, 1147–1157 (2023).
Linde, C. Will the results from the AdaptResponse trial boost CRT use? Lancet 402, 1110–1112 (2023).
Varma, N. et al. Sex-specific response to cardiac resynchronization therapy: effect of left ventricular size and QRS duration in left bundle branch block. JACC Clin. Electrophysiol. 3, 844–853 (2017).
Zweerink, A. et al. Size matters: normalization of QRS duration to left ventricular dimension improves prediction of long-term cardiac resynchronization therapy outcome. Circ. Arrhythm. Electrophysiol. 11, e006767 (2018).
Lund, L. H. et al. Association between demographic, organizational, clinical, and socio-economic characteristics and underutilization of cardiac resynchronization therapy: results from the Swedish Heart Failure Registry. Eur. J. Heart Fail. 19, 1270–1279 (2017).
Chatterjee, N. A. et al. Increasing sex differences in the use of cardiac resynchronization therapy with or without implantable cardioverter-defibrillator. Eur. Heart J. 38, 1485–1494 (2017).
Gadler, F., Valzania, C. & Linde, C. Current use of implantable electrical devices in Sweden: data from the Swedish pacemaker and implantable cardioverter-defibrillator registry. Europace 17, 69–77 (2015).
Linde, C. et al. Gender, underutilization of cardiac resynchronization therapy, and prognostic impact of QRS prolongation and left bundle branch block in heart failure. Europace 17, 424–431 (2015).
Dickstein, K. et al. The European cardiac resynchronization therapy survey. Eur. Heart J. 30, 2450–2460 (2009).
Mullens, W. et al. Optimized implementation of cardiac resynchronization therapy: a call for action for referral and optimization of care: a joint position statement from the Heart Failure Association (HFA), European Heart Rhythm Association (EHRA), and European Association of Cardiovascular Imaging (EACVI) of the European Society of Cardiology. Eur. J. Heart Fail. 22, 2349–2369 (2020).
Baldasseroni, S. et al. Left bundle-branch block is associated with increased 1-year sudden and total mortality rate in 5517 outpatients with congestive heart failure: a report from the Italian network on congestive heart failure. Am. Heart J. 143, 398–405 (2002).
Raatikainen, M. J. et al. Statistics on the use of cardiac electronic devices and electrophysiological procedures in the European Society of Cardiology countries: 2014 report from the European Heart Rhythm Association. Europace 17, i1–i75 (2015).
Dickstein, K. et al. CRT Survey II: a European Society of Cardiology survey of cardiac resynchronisation therapy in 11 088 patients – who is doing what to whom and how? Eur. J. Heart Fail. 20, 1039–1051 (2018).
Thorvaldsen, T. & Lund, L. H. Focusing on referral rather than selection for advanced heart failure therapies. Card. Fail. Rev. 5, 24–26 (2019).
Salden, F. et al. Short-term hemodynamic and electrophysiological effects of cardiac resynchronization by left ventricular septal pacing. J. Am. Coll. Cardiol. 75, 347–359 (2020).
Liang, Y. et al. Left bundle branch pacing versus biventricular pacing for acute cardiac resynchronization in patients with heart failure. Circ. Arrhythm. Electrophysiol. 15, e011181 (2022).
Arnold, A. D. et al. His resynchronization versus biventricular pacing in patients with heart failure and left bundle branch block. J. Am. Coll. Cardiol. 72, 3112–3122 (2018).
Diaz, J. C. et al. Left bundle branch area pacing versus biventricular pacing as initial strategy for cardiac resynchronization. JACC Clin. Electrophysiol. 9, 1568–1581 (2023).
Chung, M. K. et al. 2023 HRS/APHRS/LAHRS guideline on cardiac physiologic pacing for the avoidance and mitigation of heart failure. Heart Rhythm. 20, e17–e91 (2023).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT05650658 (2023).
Giustino, G. et al. Sex-based differences in outcomes after mitral valve surgery for severe ischemic mitral regurgitation: from the cardiothoracic surgical trials network. JACC Heart Fail. 7, 481–490 (2019).
Acker, M. A. et al. Mitral-valve repair versus replacement for severe ischemic mitral regurgitation. N. Engl. J. Med. 370, 23–32 (2014).
Goldstein, D. et al. Two-year outcomes of surgical treatment of severe ischemic mitral regurgitation. N. Engl. J. Med. 374, 344–353 (2016).
Kosmidou, I. et al. Sex-specific outcomes of transcatheter mitral-valve repair and medical therapy for mitral regurgitation in heart failure. JACC Heart Fail. 9, 674–683 (2021).
Joshi, A. A. et al. Sex-based differences in left ventricular assist device utilization: insights from the nationwide inpatient sample 2004 to 2016. Circ. Heart Fail. 12, e006082 (2019).
Ahmed, A. et al. Gender differences in outcomes after implantation of left ventricular assist devices. Ann. Thorac. Surg. 109, 780–786 (2020).
Kenigsberg, B. B. et al. Sex-associated differences in cardiac reverse remodeling in patients supported by contemporary left ventricular assist devices. J. Card. Fail. 26, 494–504 (2020).
Joseph, S. M. et al. Women with cardiogenic shock derive greater benefit from early mechanical circulatory support: an update from the cVAD registry. J. Interv. Cardiol. 29, 248–256 (2016).
Abraham, W. T. et al. Baroreflex activation therapy for the treatment of heart failure with a reduced ejection fraction. JACC Heart Fail. 3, 487–496 (2015).
Georgakopoulos, D., Little, W. C., Abraham, W. T., Weaver, F. A. & Zile, M. R. Chronic baroreflex activation: a potential therapeutic approach to heart failure with preserved ejection fraction. J. Card. Fail. 17, 167–178 (2011).
Lindenfeld, J. et al. Response by sex in patient-centered outcomes with baroreflex activation therapy in systolic heart failure. JACC Heart Fail. 9, 430–438 (2021).
Gold, M. R. et al. Vagus nerve stimulation for the treatment of heart failure: the INOVATE-HF trial. J. Am. Coll. Cardiol. 68, 149–158 (2016).
Premchand, R. K. et al. Autonomic regulation therapy via left or right cervical vagus nerve stimulation in patients with chronic heart failure: results of the ANTHEM-HF trial. J. Card. Fail. 20, 808–816 (2014).
Zannad, F. et al. Chronic vagal stimulation for the treatment of low ejection fraction heart failure: results of the NEural Cardiac TherApy foR Heart Failure (NECTAR-HF) randomized controlled trial. Eur. Heart J. 36, 425–433 (2015).
Anand, I. S. et al. Comparison of symptomatic and functional responses to vagus nerve stimulation in ANTHEM-HF, INOVATE-HF, and NECTAR-HF. Esc. Heart Fail. 7, 75–83 (2020).
Russo, A. M. et al. Gender and outcomes after primary prevention implantable cardioverter-defibrillator implantation: findings from the National Cardiovascular Data Registry (NCDR). Am. Heart J. 170, 330–338 (2015).
MacFadden, D. R. et al. Sex differences in implantable cardioverter-defibrillator outcomes: findings from a prospective defibrillator database. Ann. Intern. Med. 156, 195–203 (2012).
Moore, K. et al. Sex differences in acute complications of cardiac implantable electronic devices: implications for patient safety. J. Am. Heart Assoc. 8, e010869 (2019).
Kirkfeldt, R. E., Johansen, J. B., Nohr, E. A., Jørgensen, O. D. & Nielsen, J. C. Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur. Heart J. 35, 1186–1194 (2014).
Amuthan, R. & Curtis, A. B. Sex-specific considerations in drug and device therapy of cardiac arrhythmias: JACC focus seminar 6/7. J. Am. Coll. Cardiol. 79, 1519–1529 (2022).
Blendea, D. et al. Variability of coronary venous anatomy in patients undergoing cardiac resynchronization therapy: a high-speed rotational venography study. Heart Rhythm. 4, 1155–1162 (2007).
Russo, A. M. et al. Impact of gender on clinical outcomes associated with subcutaneous implantable cardioverter defibrillators [abstract]. Circulation 134, A19607 (2016).
Werner, N. et al. Gender-related differences in patients undergoing transcatheter mitral valve interventions in clinical practice: 1-year results from the German TRAMI registry. Catheter. Cardiovasc. Interv. 95, 819–829 (2020).
Estévez-Loureiro, R. et al. Effect of gender on results of percutaneous edge-to-edge mitral valve repair with MitraClip system. Am. J. Cardiol. 116, 275–279 (2015).
Magnussen, C. et al. Gender differences and outcomes in left ventricular assist device support: the European Registry for Patients with Mechanical Circulatory Support. J. Heart Lung Transpl. 37, 61–70 (2018).
Bozkurt, B. et al. Cardiac rehabilitation for patients with heart failure: JACC expert panel. J. Am. Coll. Cardiol. 77, 1454–1469 (2021).
Heidenreich, P. A. et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 145, e895–e1032 (2022).
Alter, D. A., Oh, P. I. & Chong, A. Relationship between cardiac rehabilitation and survival after acute cardiac hospitalization within a universal health care system. Eur. J. Cardiovasc. Prev. Rehabil. 16, 102–113 (2009).
Anderson, L. et al. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J. Am. Coll. Cardiol. 67, 1–12 (2016).
Colella, T. J. et al. Sex bias in referral of women to outpatient cardiac rehabilitation? A meta-analysis. Eur. J. Prev. Cardiol. 22, 423–441 (2015).
Oosenbrug, E. et al. Sex differences in cardiac rehabilitation adherence: a meta-analysis. Can. J. Cardiol. 32, 1316–1324 (2016).
Samayoa, L. et al. Sex differences in cardiac rehabilitation enrollment: a meta-analysis. Can. J. Cardiol. 30, 793–800 (2014).
Khadanga, S., Savage, P. D., Gaalema, D. E. & Ades, P. A. Predictors of cardiac rehabilitation participation: opportunities to increase enrollment. J. Cardiopulm. Rehabil. Prev. 41, 322–327 (2021).
Sbolli, M., Fiuzat, M., Cani, D. & O’Connor, C. M. Depression and heart failure: the lonely comorbidity. Eur. J. Heart Fail. 22, 2007–2017 (2020).
Hsich, E. M. et al. Sex differences in in-hospital mortality in acute decompensated heart failure with reduced and preserved ejection fraction. Am. Heart J. 163, 430–437.e3 (2012).
O’Connor, C. M. et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 301, 1439–1450 (2009).
Pina, I. L. et al. Effects of exercise training on outcomes in women with heart failure: analysis of HF-ACTION (Heart Failure–A Controlled Trial Investigating Outcomes of Exercise TraiNing) by sex. JACC Heart Fail. 2, 180–186 (2014).
Suaya, J. A., Stason, W. B., Ades, P. A., Normand, S. L. & Shepard, D. S. Cardiac rehabilitation and survival in older coronary patients. J. Am. Coll. Cardiol. 54, 25–33 (2009).
Kitzman, D. W. et al. Physical rehabilitation for older patients hospitalized for heart failure. N. Engl. J. Med. 385, 203–216 (2021).
Mentz, R. J. et al. Rehabilitation intervention in older patients with acute heart failure with preserved versus reduced ejection fraction. JACC Heart Fail. 9, 747–757 (2021).
Jin, X. et al. Women’s participation in cardiovascular clinical trials from 2010 to 2017. Circulation 141, 540–548 (2020).
Van Spall, H. G. C. et al. Ending gender inequality in cardiovascular clinical trial leadership: JACC review topic of the week. J. Am. Coll. Cardiol. 77, 2960–2972 (2021).
Kao, D. P., Trinkley, K. E. & Lin, C. T. Heart failure management innovation enabled by electronic health records. JACC Heart Fail. 8, 223–233 (2020).
Riggio, J. M. et al. Effectiveness of a clinical-decision-support system in improving compliance with cardiac-care quality measures and supporting resident training. Acad. Med. 84, 1719–1726 (2009).
Ballard, D. J. et al. Impact of a standardized heart failure order set on mortality, readmission, and quality and costs of care. Int. J. Qual. Health Care 22, 437–444 (2010).
Krive, J., Shoolin, J. S. & Zink, S. D. Effectiveness of evidence-based congestive heart failure (CHF) CPOE order sets measured by health outcomes. AMIA Annu. Symp. Proc. 2014, 815–824 (2014).
Stromberg, A. The crucial role of patient education in heart failure. Eur. J. Heart Fail. 7, 363–369 (2005).
Lobato, L. et al. Impact of gender on the decision to participate in a clinical trial: a cross-sectional study. BMC Public. Health 14, 1156 (2014).
Concannon, T. W. et al. A systematic review of stakeholder engagement in comparative effectiveness and patient-centered outcomes research. J. Gen. Intern. Med. 29, 1692–1701 (2014).
Shannon, G. et al. Gender equality in science, medicine, and global health: where are we at and why does it matter? Lancet 393, 560–569 (2019).
van Diemen, J. et al. The importance of achieving sex- and gender-based equity in clinical trials: a call to action. Eur. Heart J. 42, 2990–2994 (2021).
Pelletier, R. et al. Sex-related differences in access to care among patients with premature acute coronary syndrome. CMAJ 186, 497–504 (2014).
Pelletier, R. et al. Sex versus gender-related characteristics: which predicts outcome after acute coronary syndrome in the young? J. Am. Coll. Cardiol. 67, 127–135 (2016).
Ballering, A. V., Bonvanie, I. J., Olde Hartman, T. C., Monden, R. & Rosmalen, J. G. M. Gender and sex independently associate with common somatic symptoms and lifetime prevalence of chronic disease. Soc. Sci. Med. 253, 112968 (2020).
Ghali, J. K. Sex-related differences in heart failure and beta-blockers. Heart Fail. Rev. 9, 149–159 (2004).
SOLVD Investigators Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N. Engl. J. Med. 325, 293–302 (1991).
Wenger, N. K., Speroff, L. & Packard, B. Cardiovascular health and disease in women. N. Engl. J. Med. 329, 247–256 (1993).
Majahalme, S. K. et al. Comparison of treatment benefit and outcome in women versus men with chronic heart failure (from the Valsartan Heart Failure Trial). Am. J. Cardiol. 95, 529–532 (2005).
Massie, B. M. et al. Irbesartan in patients with heart failure and preserved ejection fraction. N. Engl. J. Med. 359, 2456–2467 (2008).
Solomon, S. D. et al. Sacubitril/valsartan across the spectrum of ejection fraction in heart failure. Circulation 141, 352–361 (2020).
Simon, T., Mary-Krause, M., Funck-Brentano, C. & Jaillon, P. Sex differences in the prognosis of congestive heart failure: results from the Cardiac Insufficiency Bisoprolol Study (CIBIS II). Circulation 103, 375–380 (2001).
MERIT-HF Study Group Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial-in Congestive Heart Failure (MERIT-HF). Lancet 353, 2001–2007 (1999).
Packer, M. et al. Effect of carvedilol on survival in severe chronic heart failure. N. Engl. J. Med. 344, 1651–1658 (2001).
McMurray, J. J. V. et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N. Engl. J. Med. 381, 1995–2008 (2019).
Butler, J. et al. Effects of empagliflozin in women and men with heart failure and preserved ejection fraction. Circulation 146, 1046–1055 (2022).
Solomon, S. D. et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N. Engl. J. Med. 387, 1089–1098 (2022).
Jhund, P. S. et al. Dapagliflozin across the range of ejection fraction in patients with heart failure: a patient-level, pooled meta-analysis of DAPA-HF and DELIVER. Nat. Med. 28, 1956–1964 (2022).
Digitalis Investigation Group The effect of digoxin on mortality and morbidity in patients with heart failure. N. Engl. J. Med. 336, 525–533 (1997).
Deswal, A. & Bozkurt, B. Comparison of morbidity in women versus men with heart failure and preserved ejection fraction. Am. J. Cardiol. 97, 1228–1231 (2006).
Cleland, J. G. et al. An individual patient meta-analysis of five randomized trials assessing the effects of cardiac resynchronization therapy on morbidity and mortality in patients with symptomatic heart failure. Eur. Heart J. 34, 3547–3556 (2013).
Stone, G. W. et al. Transcatheter mitral-valve repair in patients with heart failure. N. Engl. J. Med. 379, 2307–2318 (2018).
Zile, M. R. et al. Baroreflex activation therapy in patients with heart failure with reduced ejection fraction. J. Am. Coll. Cardiol. 76, 1–13 (2020).
Author information
Authors and Affiliations
Contributions
The authors contributed substantially to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
J.B. has received consultancy and/or research fees from Abbott, American Regent, Amgen, Applied Therapeutics, AskBio, Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, Boston Scientific, Bristol Myers Squibb, Cardiac Dimension, Cardiocell, Cardior, CSL Behring, CVRx, Cytokinetics, Daxor, Edwards, Element Science, Faraday, Foundry, G3P, Innolife, Impulse Dynamics, Imbria, Inventiva, Ionis, Lexicon, Eli Lilly, LivaNova, Janssen, Medtronics, Merck, Occlutech, Owkin, Novartis, Novo Nordisk, Pharmacosmos, Pharmain, Pfizer, Prolaio, Regeneron, Renibus, Roche Diagnostics, Salamandra, Sanofi, SC Pharma, Secretome, Sequana, SQ Innovation, Tenex, Tricog, Ultromics, Vifor, and Zoll. A.A.V. has received consultancy and/or research fees from Anacardio, AstraZeneca, Bayer, Bristol Myers Squibb, Boehringer Ingelheim, Cytokinetics, Corteria, Eli Lilly, Moderna, Novartis, Novo Nordisk, Pfizer and Roche Diagnostics. C.S.P.L. is supported by a Clinician Scientist Award from the National Medical Research Council of Singapore; has received research support from Novo Nordisk and Roche Diagnostics; has served as consultant or on the Advisory Board/Steering Committee/Executive Committee for Alleviant Medical, Allysta Pharma, Amgen, AnaCardio AB, Applied Therapeutics, AstraZeneca, Bayer, Boehringer Ingelheim, Boston Scientific, Bristol Myers Squibb, CardioRenal, Cytokinetics, Darma Inc., EchoNous Inc, Eli Lilly, Impulse Dynamics, Intellia Therapeutics, Ionis Pharmaceutical, Janssen Research & Development LLC, Medscape/WebMD Global LLC, Merck, Novartis, Novo Nordisk, Prosciento, Quidel Corporation, Radcliffe Group, Recardio, ReCor Medical, Roche Diagnostics, Sanofi, Siemens Healthcare Diagnostics and Us2.ai; and serves as co-founder and non-executive director of Us2.ai. J.Y.C. has received consultancy fees from Medtronic. H.Q. has no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Harriette Van Spall, Theresa McDonagh, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chyou, J.Y., Qin, H., Butler, J. et al. Sex-related similarities and differences in responses to heart failure therapies. Nat Rev Cardiol (2024). https://doi.org/10.1038/s41569-024-00996-1
Accepted:
Published:
DOI: https://doi.org/10.1038/s41569-024-00996-1