Abstract
Clinical studies on heart failure with mildly reduced left ventricular ejection fraction (HFmrEF) have gradually increased. However, studies on the prognostic differences between men and women among patients with HFmrEF are few, and no evidence on sex differences in such patients exists. Therefore, we retrospectively assessed the data of patients with HFmrEF using propensity score-matched analysis (PSMA). A total of 1691 patients with HFmrEF were enrolled in the Outcome of Discharged HFmrEF Patients study (OUDI-HF study), which included 1095 men and 596 women. After propensity score matching, we compared the difference in cardiovascular (CV) events (cardiovascular death or heart failure readmission) and all-cause mortality at 90 days and 1 year after discharge between men and women using Kaplan–Meier analysis and Cox regression. After PSMA, men with HFmrEF were 2.2 times more likely to die at 90 days than women with HFmrEF [hazard ratio (HR) 1.88; 95% confidence interval (95% CI) 1.03–3.46; P = 0.041]. However, there was no difference in the 90-day CV events (HR 0.96; 95% CI 0.75–1.22; P = 0.718). Similarly, there was no difference in all-cause mortality (HR 1.16; 95% CI 0.81–1.65; P = 0.417) and CV events (HR 0.98; 95% CI 0.83–1.16; P = 0.817) between men and women after 1 year. Among the patients with HFmrEF, men had a higher 90-day risk of all-cause mortality than women after hospital discharge, and this risk disappeared after 1 year.
Clinical Trial Registration: URL: http://www.clinicaltrials.gov. Unique identifier: NCT05240118 (ESC Heart Failure. (2022). doi: https://doi.org/10.1002/ehf2.14044).
Similar content being viewed by others
Introduction
Cardiovascular disease is the most common cause of death in men and women worldwide1. Heart failure (HF) is a pandemic that has placed tremendous stress on patients, caregivers, and healthcare systems2,3. Based on the left ventricular ejection fraction (LVEF), heart failure can be categorized into heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). The range between these two fractions has been termed as “HF with mid-range ejection fraction (EF),” or “HF with mildly reduced EF” referring an LVEF of 41–49%4,5,6.
Studies have shown that men are more likely to have HFrEF, whereas women are more likely to have HFpEF7,8,9,10,11,12. However, only few studies exist on sex differences in patients with HFmrEF13. Most HF studies worldwide were conducted on men14, and information collected about men with HF cannot be assumed to apply equally to women. Therefore, we conducted a retrospective study to compare the differences in outcome events between men and women with HFmrEF.
Methods
Study population and data source
The study protocol was approved by the Ethics Committee of Xiangtan Central Hospital (Xiangtan, China, No. 20211036) and conformed to the principles outlined in the Declaration of Helsinki15. The Ethics Committee Review Board of Xiangtan Central Hospital waived the need for written informed consent. Consent was obtained from all patients or their guardians during follow-up. This study was based on the Outcome of Discharged HFmrEF Patients study (OUDI-HF study; a retrospective study). The OUDI-HF study included 1691 patients with HFmrEF who were admitted to our hospital from 1 January 2015 to 31 August 2020. The inclusion criteria were HF with an LVEF of 41% to 49% and a New York Heart Association HF score of II to IV.The exclusion criteria were malignancies or other non-cardiac diseases with expected survival of less than 1 year.
Outcomes
Demographic and procedural data were collected from patients' hospital charts or databases. All study participants were followed up on 31 August 2021. A panel of seven experienced physicians reviewed suspected CV events by examining the information obtained from hospital records and follow-ups, including clinical telephone interviews and community visits. The primary outcome of interest was all-cause death after discharge, and the secondary outcome was the composite of CV death and HF readmissions (CV events). Cardiovascular death is death from any cardiovascular mechanism: death from acute myocardial infarction, sudden cardiac death, death from heart failure, death from stroke, death from cardiovascular surgery, death from cardiovascular hemorrhage, and death from other cardiovascular causes. All-cause mortality is death from all causes, including cardiovascular death. Coronary heart disease was defined by coronary angiography evidenced > 50% stenosis of the left main stem, > 70% stenosis in a major coronary vessel, or 30% to 70% stenosis with fractional flow reserve ≤ 0.8. Myocardial infarction was defined by clinical history of ischemic type chest pain lasting for more than 20 min; changes in serial ECG tracings; rise and fall of serum cardiac biomarkers such as creatine kinase-MB fraction and troponin. PCI (percutaneous coronary intervention) referred to minimally invasive procedures used to open clogged coronary arteries.
Statistical analysis
Continuous variables are expressed as the mean ± standard deviation. The propensity score matching analysis was performed using a multivariate logistic regression model based on the following factors: age, body mass index, current smoker, hypertension, hyperlipidemia, diabetes, coronary heart disease, atrial fibrillation, previous stroke, chronic obstructive pulmonary disease, renal insufficiency, myocardial infarction, history of percutaneous coronary intervention, and New York heart function classification. Pairs of patients, men or women, were derived within a quarter of the standard deviation of the estimated propensity using 1:1 greedy nearest-neighbor matching. This strategy provided 530 matching pairs per group. A COX risk regression model was added to verify the reliability of the statistical results after propensity score matching.
Clinical characteristics between the groups were compared using t-tests for continuous measures and chi-squared tests for categorical variables. Non-parametric tests for continuous, not normally distributed variables. The Kaplan–Meier method was used to estimate the incidence of cumulative events. A Cox proportional hazards model was constructed to assess the hazard ratio for each event between the two groups. After propensity score matching, the balance of measured variables between groups was analyzed using paired t-tests for continuous measures and McNemar’s test for categorical variables. After propensity score matching, differences in cumulative event rates were analyzed using the stratified Cox procedure.
P-values were obtained using the Kruskal–Wallis rank-sum test for continuous variables and Fisher’s exact test for count variables. Results were considered significant when the P-value was less than 0.05. All analyses were performed using R (http://www.R-project.org) and EmpowerStats software (http://www.empowerstats.com, X&Y solutions, Inc. Boston MA).
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Xiangtan Central Hospital (Xiangtan, China, No. 20211036) and conformed to the principles outlined in the Declaration of Helsinki. The need for informed consent was waived by the ethics committee Review Board of Xiangtan Central Hospital, because of the retrospective nature of the study.
Results
Among the 1691 patients with HFmrEF, including 1095 men and 596 women, 530 matched pairs were obtained after propensity score matching analysis (Fig. 1). Table 1 shows patient profiles before and after propensity score matching. Before propensity score matching, men had higher rates of current smoking (P < 0.001), coronary heart disease (P = 0.024), chronic obstructive pulmonary disease (P < 0.001), myocardial infarction (P < 0.001), and percutaneous coronary intervention (P < 0.001) ratio than women. Differences in age (P < 0.001) and New York heart function class (P < 0.001) were also noted. Body mass index (P = 0.644), hypertension (P = 0.055), hyperlipidemia (P = 0.087), diabetes (P = 0.203), atrial fibrillation (P = 0.531), previous stroke (P = 0.637), and renal insufficiency (P = 0.596) were similar between the two groups. After propensity score matching, there were no differences in other variables between the two groups and the P-values were both > 0.05, indicating that there was no difference between the two groups and that they were comparable.
Table 2 supplements other baseline information not involved in propensity matching scores. The table shows no difference between male and female HFmrEF patients at baseline in Systolic blood pressure, Beta-blocker, angiotensin receptor blocker, angiotensin receptor neprilysin inhibitor, left ventricular ejection fraction, Left atrial size and interventricular septal depth. However, there are still differences in other indicators. However, most of the baselines became either no difference or a reduced difference after propensity matching scores.
Table 3 presents the risk of primary and secondary outcomes in patients before and after the propensity score-matched cohort. Before propensity score matching, risk of cardiovascular events was similar between men and women with HFmrEF within 90 days (event rate:22.6% vs. 23.0%, HR 0.98; 95% CI 0.79–1.21; P = 0.836) or 1 year (46.8% vs. 49.7%, HR 0.92; 95% CI 0.80–1.06; P = 0.269). There was no difference between males and females in the incidence of all-cause mortality at 90 days (4.2% vs. 3.4%, HR 1.25; 95% CI 0.74–2.11; P = 0.406) or 1 year (11.5% vs.11.6%, HR 0.99; 95% CI 0.74–1.33; P = 0.970).
After propensity score matching, men with HFmrEF were 1.88 times more likely to die at 90 days than women with HFmrEF (mortality: 5.7% vs. 3.0% for men and women, hazard ratio (HR) 1.88; 95% confidence interval (95% CI) 1.03–3.46; P = 0.041). The difference in all-cause mortality between men and women was not significant after 1 year of follow-up (12.3% vs. 10.8%, HR 1.16; 95% CI 0.81–1.65; P = 0.417) (Table 3). No difference was noted in 90-day or 1-year cardiovascular event rates between men and women (Table 3). The difference in the presence of all-cause mortality at 90 days between male and female HFmrEF persisted after COX multiple regression analysis and adjustment for confounders (HR 1.84; 95% CI 1.02–3.34; P = 0.045) (Table 4).
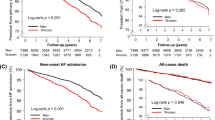
In Kaplan–Meier survival curves before propensity score matching was performed, there was no difference between male and female HFmrEF on 90 days all-cause mortality (P = 0.41) and one-year all-cause mortality (P = 0.97) (Fig. 2A, C). Figure 2B, D shows no difference in the incidence of cardiovascular events between men and women within 90 days (P = 0.84) and one-year (P = 0.27).
Kaplan–Meier curves of outcomes before and after PSM matching. (A) The cumulative 90-day all-cause mortality (before PSM matching). (B) The cumulative 90-day CV events (before PSM matching). (C) The cumulative 1 year all-cause death (before PSM matching). (D) The cumulative 1 year CV events (before PSM matching). (E) The cumulative 90-day all-cause mortality (after PSM matching). (F) The cumulative 90-day CV events (after PSM matching). (G) The cumulative 1 year all-cause death (after PSM matching). (H) The cumulative 1 year CV events (after PSM matching).
In Kaplan–Meier survival curves after propensity score matching, the cumulative 90-day all-cause mortality was higher in men than in women (P = 0.037) (Fig. 2E). The all-cause mortality difference between men and women gradually disappeared after a year (P = 0.42)(Fig. 2G). There was no difference in cardiovascular events within 90 days and one year between men and women, shown in Fig. 2F (P = 0.72) and Fig. 2H (P = 0.82).
Table 5 shows the subgroup analysis of male and female HFmrEF patients on 90-day all-cause mortality. Compared with women, this group of patients with a BMI < 30, no history of atrial fibrillation, no history of COPD and no history of PCI had a higher all-cause mortality rate at 90 days in the male HFmrEF (P < 0.05).
Discussion
The main finding of this study was that men with HFmrEF had a higher risk of all-cause mortality 90 days after discharge than women with HFmrEF, particularly in the interval of 20–80 days after discharge.
Previous studies showed that women with HF without further classification of LVEF were treated in smaller proportions but still had better outcomes than men 13,16,17,18,19,20. The Framingham Heart Study (FHS), which was conducted from 1990 to 1999, showed that women with HF without further classification of LVEF had better survival rates than men, with age-adjusted 5-year mortality rates of 45% and 59%, respectively 21. In HFrEF, the Prospective Comparison of Angiotensin Receptor Neprilysin Inhibitor with Angiotensin Converting Enzyme Inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure and Aliskiren Trial to Minimize Outcomes in Patients with Heart failure trials, which included a total of 12,058 men and 3,357 women, showed that all-cause mortality was lower in women than in men (adjusted HR: 0.68; 95% CI: 0.62–0.74; P < 0.001) 19. In the Irbesartan in Heart Failure with Preserved Ejection Fraction trial, which included 2491 women, showed a 20% reduction in the risk of all-cause mortality or hospitalization in women even after adjusting for age differences and other baseline characteristics22. Moreover, similar conclusions were drawn in studies such as the Candesartan in Heart failure: Assessment of Reduction in Mortality and Morbidity17, Beta-Blocker Evaluation of Survival Trial23, and Prevention of REnal and Vascular ENdstage Disease12. Studies such as FHS and ours demonstrated differences in outcomes between men and women with HF. However, Studies such as FHS failed to explain the sex differences in outcomes of HFmrEF, whereas we attempted to study the sex differences in HFmrEF. Indeed, some studies have reported different outcomes than those reported in the abovementioned studies. In the Olmsted County Heart Failure Events Study from 2000 to 2010, age-adjusted all-cause mortality was similar for women and men24. The Atherosclerosis Risk in Communities study (2005–2014) showed that age-adjusted 28-day and 1-year mortality was equally high among men and women hospitalized for acute HF25.
Pharmacokinetics is also different caused by differences in body composition between men and women26, which result in higher rates of adverse events in women using drugs according to HF guidelines27,28. Although the treatment of HF varies in some regions between men and women8,29, many disadvantageous factors still exist for women with HF. For instance, women with HF have a poorer quality of life and continue to receive suboptimal treatment19, even less access to a cardiologist30,31, and lower use of left ventricular assist devices32,33. Male heart failure patients were independently associated with cardiac death but not with a composite endpoint or all-cause mortality34. Although the annual mortality rate is higher in men, more women than men die of heart failure each year, and the clinical presentation of heart failure differs between men and women35.Therefore, more research is required to assess the different treatments available for HF between men and women. Moreover, it needs to stratify and recruit more women in HF trials.
Proportion of cardiovascular or noncardiovascular deaths were presented in the Table S1. Results showed that after PSM both cardiovascular and noncardiovascular death rates are both borderline higher in men than in women (P = 0.107 and 0.101, respectively), thus the higher all-cause deaths in men might be the jointly effects of borderline higher cardiovascular and noncardiovascular deaths in men.Our analysis showed that both cardiovascular and noncardiovascular deaths rates are borderline higher in men than in women within 90 days post discharge, the joint effects of cardiovascular and noncardiovascular deaths might explain the significantly higher all-cause death within 90 days post discharge in our cohort. It is to note that this study is a single center retrospective analysis, which suffers the nature of selection bias in this study setting, future prospective multi-center clinical trials are needed to validate our finding. The study also failed to explain why women had better outcomes than men in heart failure. Women have better heart failure outcomes, presumably related to different risk factors and hormone levels in men and women with heart failure31. For example, the leading cause of heart failure in male patients is ischaemic heart disease, while in female patients, the leading cause of heart failure is atrial fibrillation11. This is consistent with our baseline data, where male patients had less atrial fibrillation and more coronary heart disease than female patients (Table 1). In fact, our study showed that female patients had both borderline lower risk of cardiovascular and noncardiovascular death at 90 days post discharge. More research is needed to advance this area to improve the treatment of both female and male heart failure patients.
Limitations
This study has several limitations. First, this was a retrospective study to minimize bias in patient selection, but unobserved confounders remained. Second, our study exclusively recruited patients from China from an isolated population at a local heart center, thereby lacking diversity to justify the uniformity of the findings. Lastly, we could not include all variables that differed between men and women in the analysis of propensity matching scores. This difference may affect the outcome to some extent.
Conclusions
After propensity score matching, men with HFmrEF had a higher risk of all-cause mortality 90 days after discharge than women with HFmrEF. This risk disappeared after one year. This higher risk of all-cause mortality in men is mainly seen in those with less severe underlying disease. So, attention should be paid to short-term survival after discharge in men with HFmrEF, regardless of their severity. There were no differences in the 90-day and 1-year cardiovascular events between men and women with HFmrEF. Further research is warranted to understand the complex sex-related risk differences among patients with HF. A better understanding of sex-specific risk factors may help develop strategies to improve outcomes in this critical disease.
Data availability
The datasets generated and analyzed during the current study are not publicly available due the database owner is reluctant to make them public but are available from the corresponding author upon reasonable request.
Abbreviations
- HFmrEF:
-
Heart failure with mid-range or mildly reduced ejection fraction
- PSMA:
-
Propensity score-matched analysis
- CV:
-
Cardiovascular
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- HF:
-
Heart failure
- EF:
-
Ejection fraction
- LVEF:
-
Left ventricular ejection fraction
- HFrEF:
-
Heart failure reduced ejection fraction
- HFpEF:
-
Heart failure preserved ejection fraction
- BMI:
-
Body mass index
- COPD:
-
Chronic obstructive pulmonary disease
- NYHA:
-
New York Heart Association
- PCI:
-
Percutaneous coronary intervention
- FHS:
-
The Framingham Heart Study
- NT-proBNP:
-
Terminal pro-B type natriureti peptide
- eGFR:
-
Estimated glomerular filtration rate
- ACEi:
-
Angiotensin-converting enzyme inhibitor
- ARB:
-
Angiotensin receptor blocker
- ARNI:
-
Angiotensin receptor neprilysin inhibitor
- SGLT2i:
-
Sodium-dependent glucose transporters 2 inhibitor
- LAs:
-
Left atrial size
- LVd:
-
Left ventricle dimension
- IVSd:
-
Interventricular septal depth
- LVPWd:
-
Left ventricular posterior wall decreased
- RAs:
-
Right atrial size
- RVd:
-
Right ventricle dimension
- e/e:
-
Ratio between peak early diastolic velocity and early diastolic tissue velocity
- PASP:
-
Pulmonary artery systolic pressure
References
Yusuf, S. et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case–control study. Lancet 364(9438), 937–952 (2004).
Savarese, G. & Lund, L. H. Department of Cardiology KUHS, Division of Cardiology DOMK: Global public health burden of heart failure. Card. Fail. Rev. 3(1), 7–11 (2017).
Ponikowski, P. et al. Heart failure: Preventing disease and death worldwide. ESC Heart Fail. 1(1), 4–25 (2014).
Anderson, J. L. et al. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures. J. Am. Coll. Cardiol. 63(21), 2304–2322 (2014).
Heidenreich, P. A. et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure. J. Am. Coll. Cardiol. 79(17), e263–e421 (2022).
Bauersachs, J. & Soltani, S. Herzinsuffizienzleitlinien 2021 der ESC. Herz 47(1), 12–18 (2022).
Lam, C. S. P. et al. Sex differences in heart failure. Eur. Heart J. 40(47), 3859–3868 (2019).
Cleland, J. The EuroHeart Failure survey programme—A survey on the quality of care among patients with heart failure in Europe Part 1: Patient characteristics and diagnosis. Eur. Heart J. 24(5), 442–463 (2003).
Mahmoodzadeh, S. et al. Estrogen receptor alpha up-regulation and redistribution in human heart failure. FASEB J. 20(7), 926–934 (2006).
Regitz-Zagrosek, V., Brokat, S. & Tschope, C. Role of gender in heart failure with normal left ventricular ejection fraction. Prog. Cardiovasc. Dis. 49(4), 241–251 (2007).
Özlek, B. Gender disparities in heart failure with mid-range and preserved ejection fraction: results from APOLLON study. Anat. J. Cardiol. 2019, 242–252 (2019).
Meyer, S. et al. Sex differences in new-onset heart failure. Clin. Res. Cardiol. 104(4), 342–350 (2015).
Stolfo, D. et al. Sex-based differences in heart failure across the ejection fraction spectrum. JACC Heart Fail. 7(6), 505–515 (2019).
Marrone, D., Fabio, Z., Cristina, B., Alberto, Z. & Thiene, A. G. Clinical trial enrolment favours men. Eur. Heart J. 40(14), 1104–1105 (2019).
World Medical Association Declaration of Helsinki ethical principles for medical research involving human subjects. JAMA 310(20), 2191–2194 (2013).
Lenzen, M. J. et al. Management of patients with heart failure in clinical practice: Differences between men and women. Heart 94(3), 1–5 (2008).
O’Meara, E. et al. Sex differences in clinical characteristics and prognosis in a broad spectrum of patients with heart failure. Circulation 115(24), 3111–3120 (2007).
Ho, K. K., Anderson, K. M., Kannel, W. B., Grossman, W. & Levy, D. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation 88(1), 107–115 (1993).
Dewan, P. et al. Differential impact of heart failure with reduced ejection fraction on men and women. J. Am. Coll. Cardiol. 73(1), 29–40 (2019).
Russo, G. et al. Sex-related differences in chronic heart failure: A community-based study. J. Cardiovasc. Med. 22(1), 36–44 (2021).
Levy, D. et al. Long-term trends in the incidence of and survival with heart failure. N. Engl. J. Med. 347(18), 1397–1402 (2002).
Lam, C. S. P. et al. Sex differences in clinical characteristics and outcomes in elderly patients with heart failure and preserved ejection fraction: The Irbesartan in Heart Failure with Preserved Ejection Fraction (I-PRESERVE) trial. Circ. Heart Fail. 5(5), 571–578 (2012).
Ghali, J. K. et al. Gender differences in advanced heart failure: Insights from the BEST study. J. Am. Coll. Cardiol. 42(12), 2128–2134 (2003).
Gerber, Y. et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern. Med. 175(6), 996–1004 (2015).
Chang, P. P. et al. Trends in hospitalizations and survival of acute decompensated heart failure in four US communities (2005–2014). Circulation 138(1), 12–24 (2018).
Soldin, O. P. & Mattison, D. R. Sex Differences in pharmacokinetics and pharmacodynamics. Clin. Pharmacokinet. 48(3), 143–157 (2009).
Jochmann, N., Stangl, K., Garbe, E., Baumann, G. & Stangl, V. Female-specific aspects in the pharmacotherapy of chronic cardiovascular diseases. Eur. Heart J. 26(16), 1585–1595 (2005).
Petrie, M. C., Dawson, N. F., Murdoch, D. R., Davie, A. P. & McMurray, J. J. Failure of women’s hearts. Circulation 99(17), 2334–2341 (1999).
Reginster, J. Y. Miscellaneous and experimental agents. Am. J. Med. Sci. 313(1), 33–40 (1997).
Cook, N. L., Ayanian, J. Z., Orav, E. J. & Hicks, L. S. Differences in specialist consultations for cardiovascular disease by race, ethnicity, gender, insurance status, and site of primary care. Circulation 119(18), 2463–2470 (2009).
Boer, A. R. et al. Heart failure with preserved, mid-range, and reduced ejection fraction across health care settings: An observational study. ESC Heart Fail. 9(1), 363–372 (2022).
Hsich, E. M. Sex differences in advanced heart failure therapies. Circulation 139(8), 1080–1093 (2019).
Fluschnik, N. et al. Gender differences in characteristics and outcomes in heart failure patients referred for end-stage treatment. ESC Heart Fail. 8(6), 5031–5039 (2021).
Duca, F. et al. Gender-related differences in heart failure with preserved ejection fraction. Sci. Rep.-UK 8(1), 1080 (2018).
Hoppe, B. L. & Hermann, D. D. Sex differences in the causes and natural history of heart failure. Curr. Cardiol. Rep. 5(3), 193–199 (2003).
Acknowledgements
We thank Liwen Bianji (Edanz) (https://www.liwenbianji.cn) for editing the English text of a draft of this manuscript.
Funding
This study is supported by Scientific Bureau of Xiangtan City (SF-YB20201023), Xiangtan City, Hunan Province, China and Committee of Development and Reform of Hunan Province (2019-875), Changsha, Hunan Province, China.
Author information
Authors and Affiliations
Contributions
Z.L.,Y.Z., S.C.: main authors of the study, established the idea to study the heart failure with mildly reduced ejection fraction in Chinese population. Writing main ideas for this research, main results and discussion of the findings. Z.L. was a major contributor in writing the manuscript. M.W., H.H., K.P., L.Z. and J.F.: interpreted statistical analysis and conducted multivariate analysis to prove the main findings of this project. Z.L., W.Z., X.P., N.L., H.Z., Y.Z. and Y.P.: data collected and follow-up. J.Z.: corresponding author of the study, contributed on editing this manuscript and giving advice for the main authors to organize the manuscript and ideas of the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, Z., Zhu, Y., Chen, S. et al. Sex differences in patients with heart failure and mildly reduced left ventricular ejection fraction. Sci Rep 13, 6832 (2023). https://doi.org/10.1038/s41598-023-33733-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33733-8
This article is cited by
-
Cost-Effectiveness of Dapagliflozin in Heart Failure with Preserved or Mildly Reduced Ejection Fraction: the DELIVER Trial
Cardiovascular Drugs and Therapy (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.