Abstract
Blood malignancies arise from the dysregulation of haematopoiesis. The type of blood cell and the specific order of oncogenic events initiating abnormal growth ultimately determine the cancer subtype and subsequent clinical outcome. HOXA9 plays an important role in acute myeloid leukaemia (AML) prognosis by promoting blood cell expansion and altering differentiation; however, the function of HOXA9 in other blood malignancies is still unclear. Here, we highlight the biological switch and prognosis marker properties of HOXA9 in AML and chronic myeloproliferative neoplasms (MPN). First, we establish the ability of HOXA9 to stratify AML patients with distinct cellular and clinical outcomes. Then, through the use of a computational network model of MPN, we show that the self-activation of HOXA9 and its relationship to JAK2 and TET2 can explain the branching progression of JAK2/TET2 mutant MPN patients towards divergent clinical characteristics. Finally, we predict a connection between the RUNX1 and MYB genes and a suppressive role for the NOTCH pathway in MPN diseases.
Similar content being viewed by others
Introduction
Blood cancers are malignancies that can arise from any type of blood cell and dramatically affect haematopoiesis. Myeloproliferative neoplasms (MPNs) are chronic diseases of the myeloid lineage characterised by an excessive production of fully functional terminally differentiated blood cells. These have been classified into three types: polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF)1. Despite the relatively good prognosis of these diseases, MPN patients are at high risk of thrombosis and can develop a blast phase MPN (MPN-BP)2; a subtype of the blood cancer acute myeloid leukaemia (AML) with poor survival outcomes3. The frequency of MPN transformation to MPN-BP is highly related to the initial MPN disease type4,5,6. Therefore, a better understanding of the molecular events driving the different subtypes of MPNs is essential to help diagnose patients with higher risk of thrombosis and AML progression.
AML itself is an aggressive blood and bone marrow malignancy defined by the uncontrolled growth of myeloid progenitor cells along with a myeloid-lineage differentiation arrest7. As with MPN, there exist different types of AML with a broad range of morphologic, cytogenic, and immunologic features, all associated with diverse clinical outcomes8. Despite their similarities, prognosis, symptoms, and genetic alterations differ between AML and MPN. For example, JAK2 mutation is the main driver event of MPN diseases yet is rarely found in de novo AML9. However, myeloid-lineage dysregulation occurs in both MPN and AML, and alongside the ability of MPN to evolve to AML, this may suggest that both diseases share common biological mechanisms. The identification of these processes could help identify aberrant genes and pathways involved in both AML and MPN to detect MPN patients with higher risk of developing AML.
Better understanding of the patterns of genetic alterations in cancer cells can be used for the classification of blood diseases and prediction of progression into more severe forms of the disease10. How different combinations and orders of mutations lead to different subtypes of cancer remains a major open question11,12. The importance of mutation order has been demonstrated in MPN by Ortmann et al.13, who show that two subpopulations of patients with MPN can be distinguished by the order of mutation acquisition between the TET2 and JAK2 genes, and that these subpopulations have distinct clinical characteristics. Further analyses of these cohorts show that patients with JAK2 mutated before TET2 are younger at presentation of the disease in clinics, are more likely to present with PV, have a higher risk of thrombosis, and respond better to JAK2 inhibitor ruxolitinib. However, the molecular interplay between both mutations within cancer cells and how their order rather than their combination triggers dissimilar clinical characteristics have not been investigated.
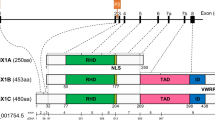
Overexpression of a single homeobox gene, HOXA9, has been reported as sufficient to quickly induce myeloproliferation, gradually followed by AML progression after a period of time14. Homeobox genes or HOX genes were first identified in the fruit fly Drosophila melanogaster as essential regulators of early embryogenesis15 and are thought to have a critical role in cancer development16. In the HOXA family, HOXA9 is the most described gene in literature and its expression was shown to be the single most highly correlating factor (out of 6817 genes tested) for poor prognosis in AML17. The importance of HOXA9 in AML has been widely explored; however, this has mainly focused on specific AML subtypes such as MLL-rearranged leukaemia18 and NUP98-HOXA9 induced leukaemia19, while its role in other blood malignancies such as MPN or other AML subtypes is poorly characterised. Recently, the oncogenic property of HOXA9 has been associated with its self-positive feedback loop in myeloid precursor cells as a result of its ability to bind its own promoter20. We hypothesise in this work that, as a consequence of the underlying gene network, the expression of HOXA9 could be used to stratify patients according to risk with blood cancers affecting the myeloid lineage.
In this study, we define a switch as a molecule that has the ability to self-sustain a positive feedback loop. Using public datasets from AML patients and MPN studies, we show that bimodal HOXA9 expression identifies two distinct cohorts of patients/mice, reflecting the gene acting as a binary switch in the cell. Firstly, HOXA9 bimodal expression in AML is associated with clinical features, such as age and WBC counts, but also patient classification into specific French-American-British (FAB) or molecular subtypes. Secondly, we design a computational network model that offers a mechanistic explanation of the distinct clinical features of MPN progression in patients with different orders of JAK2 and TET2 mutations (Fig. 1). Using our computational model and experimental validation, we argue that HOXA9 is downstream of JAK2 and TET2 and effectively stores their mutational history. This “memory” property of HOXA9 is induced by the presence of its self-activation, captured by a positive feedback loop in our model. This results in a phenotypic switch in double mutant cells with different mutation orders producing distinct subtypes of the disease. Finally, the network model also predicts a suppressive role for the NOTCH pathway in MPN and an interaction between RUNX1 and MYB.
Results
HOXA9 expression separates cohorts of AML patients with distinct clinical features
Ectopic expression of HOXA9 in AML has been widely demonstrated, but few studies have investigated the biological attributes of this transcription factor contributing to leukaemogenesis. Zhong et al.20 have shown that HOXA9 in cell lines can induce its own expression through a positive feedback loop, which promotes a continuous differentiation block and self-renewal leading to increase of hematopoietic stem cells and development of leukaemia. To validate HOXA9 self-activation and the oncogenic role in leukaemia in patients, we studied its expression in untreated de novo AML RNA sequencing data from The Cancer Genome Atlas (TCGA)21. We find that HOXA9 has bimodal expression in this data set (Fig. 2a). Whilst we find other HOX genes to also have a bimodal expression, they are correlated or anti-correlated with HOXA9 and to the best of our knowledge HOXA9 is uniquely downstream of both JAK2 and TET2. We further find two other genes with bimodal expression, APP and IGSF10, which are not clearly correlated to HOXA9 status. Correlation or anti-correlation with HOXA9 confounds survival analysis, limiting our ability to analyse the contribution of the second gene. We do, however, find within low or high HOXA9 cohorts no significant survival differences with IGSF10, and a survival difference between high/low APP expression within the cohort with low APP expression. To explore the differences between patients with different levels of HOXA9 expression and disregard external factors that could cause this bimodality, we separated patients into two cohorts, with 31 patients in the low expression peak, and 80 patients in the high expression peak. A survival analyses of both groups using Kaplan–Meier survival curves and the log-rank test confirmed that HOXA9 can be used as a marker of poor prognosis in AML (p < 0.001, Hazard Ratio 0.29 for low expression) (Fig. 2b) regardless of age (Fig. S3). This patient stratification based upon HOXA9 expression is consistent with the reported positive feedback loop characteristic of this gene and suggests that once activated or inhibited, the gene would maintain its expression level, leading to divergence in the disease progression.
a HOXA9 expression in AML patients is significantly bimodal (unimodality test rejected with \(p \; < \; 2.2\times {10}^{-16}\)), suggesting a role as a genetic switch. The low peak consists of 31 patients for HOXA9 expression between 0.005–1 log (TPM+1) and 80 patients in the high peak –4–5.5 log(TPM + 1). b HOXA9 high and low cohorts have divergent AML prognosis, consistent with known HOXA9 biology in AML (log-rank test, p = 6 × 10−5). TPM transcript per million. Source data are provided as a Source Data file.
To investigate if the switch role property of HOXA9 impacts AML subtypes, we looked at the distribution of FAB (named M0–M7) and molecular classifications among the two HOXA9 cohorts. We show that different HOXA9 expression cohorts exclude specific FAB subtypes (Fig. S4a). This suggests that HOXA9 expression is strongly coupled to some FAB subtypes.
In light of these findings, we looked to characterise the common features of HOXA9 expression cohorts. Cytogenic aberrations and gene rearrangements are frequent in AML and are known to alter the disease morphology as well as the clinical features and prognosis21. We found that HOXA9 expression separates patients with different molecular classification (Fig. S4b). MLL-induced leukaemia has been linked to high HOXA918, while M3 AML subtype is characterised by PML-RARα translocation and low HOXA9 in the literature22. Low HOXA9 expression in AML with RUNX1-RUNXT1 and CBFB-MYH11 abnormalities, which constitute the core binding factor (CBF) AML, has also been established in literature23. Our findings confirm these observations and further establish the correlation between high HOXA9 expression and the M0 and M5 subtypes in addition to complex cytogenetics. Finally, we searched for other clinical differences between cohorts, finding that HOXA9 expression correlates with age, white blood cell count (WBC) and blast percentage in the bone marrow (Fig. S4c). These divergent characteristics between cohorts suggest that the observed bimodality is not induced by external/sequencing factors.
PML-RARα, RUNX1-RUNXT1 (AML1-ETO), or CBFB-MYH11 chromosomal abnormalities predict good prognosis in AML patients24,25. All these aberrations are linked to low HOXA9 expression which also exhibits good survival prognosis among patients compared to high expression. To confirm that high HOXA9 is a marker of poor prognosis independently of its associated molecular aberrations or FAB subtypes, we studied survival outcomes within FAB classes. As M0, M3, and M5 are exclusively in one cohort, we examined the survival of patients within the M2 and M4 subtypes for high and low HOXA9 expression. Survival curves and log-rank tests within both subtypes confirms that high HOXA9 is a marker of poor prognosis HOXA9 (Fig. S8 and S9). Overall our findings are consistent with HOXA9 becoming trapped in high- or low- expression states through self-activation in AML diseases.
The JAK2/TET2/HOXA9 motif can explain divergent disease clinical outcomes in MPN
The identification of MPN patients at higher risk of developing AML remains a major clinical challenge. JAK2 is the most commonly mutated gene in many MPN patients, but different subtypes of the disease with distinct clinical traits are observed26. In contrast, TET2 was only recently identified in blood studies. First discovered in MPN in 2008 by Delhommeau et al.27, TET2 mutation resulting in its loss of function has been associated with diverse haematologic malignancies28. We have shown that HOXA9 can enable clinical stratification in AML, potentially due to the presence of a positive feedback loop. Ortmann13 describes a bifurcation among MPN patients that acquire JAK2 and TET2 mutations in different orders. This raises the question whether HOXA9 expression could also explain these divergent clinical symptoms and help stratify MPN patients with low and high risk to develop AML.
To address this question, we constructed a computational network model in a multistep process. In order to reproduce the branching in MPN patients, the underlying network of gene interactions must include genes that are sensitive to the mutation order29. This requires that parts of the network act a switch, capable of storing “memory” of previous events. This “memory” property can be encoded by a positive feedback loop acting on a gene that is downstream of both mutated genes30. This hypothetical gene must additionally respond differently to each of the mutations. That is to say, one mutation must activate the gene whilst the other reduces it, so that the gene can maintain its change in activity after the occurrence of the second mutation. The loop is necessary to induce this inheritable change in the presence of constitutive reset processes such as protein and RNA degradation.
We developed a computational model of this simple gene motif with JAK2 and TET2 genes and a hypothetical gene target with a positive feedback loop (Fig. 3a). TET2 and JAK2 have been indirectly and directly linked to HOXA9 activity. STAT5 is a well-known downstream target of JAK231, and it is also established that STAT5 and HOXA9 act as binding partners in hematopoietic cells32. Furthermore, it was recently shown that tyrosine phosphorylation of HOXA9 is JAK2-dependent33 and seems to increase the effect of HOXA9 on its downstream targets33. Regarding the interaction of TET2 with HOXA9, Bocker et al. found significantly reduced expression of HOXA genes when TET2 expression is lost34. In particular HOXA9 expression in kidney is significantly decreased by TET2 loss. HOXA9 is therefore activated by JAK2 and reduced by TET2 loss and possesses a self-positive feedback loop property20. Therefore, the JAK2/TET2/HOXA9 motif shares all the required properties for observing a clinical divergence in blood diseases.
a MPN patients with JAK2/TET2 mutations showing different clinical characteristics can be explained by a simple gene motif including a switching property. The model starts from a healthy state on the left (wild-type) and sequentially acquires mutations in JAK2 and TET2 genes. The first mutation affects the gene target expression (middle networks) which remains stable when the second mutation appears. The order in which mutations occur impacts on the gene target expression but also the phenotypes, common myeloid progenitor (CMP) expansion, and erythroid differentiation (networks on the right). b The JAK2/TET2/HOXA9 molecular network is built with the BioModelAnalyzer (BMA) tool and integrates six output phenotypes: stem cell (SC) self-renewal, CMP expansion, granulocyte-monocyte progenitor (GMP) expansion, GMP differentiation, erythroid differentiation, and megakaryocyte-erythroid progenitor (MEP) expansion. The bifurcation analysis identifies two stable states in the double mutant with different phenotype values that fit the mutation order characteristics observed in MPN patients with JAK2 and TET2 mutations. c BioModelAnalyzer simulation shows that RUNX1 expression is unchanged by JAK2 activation mutation following TET2 loss. d We select AML patients with lowest (30) and highest (30) JAK2 expression for the purpose of classification. Ranking of major cancer pathways determine the RTK-RAS pathway as the most correlatd to JAK2. This pathway contains JAK2 and so this result is as expected. The second pathway is NOTCH. The overall accuracy of the pathway is computed with the Matthews Correlation Coefficient. Box plots represent interquartile range and whiskers 1.5 × IQR. e We plot SHapley Additive exPlanations (SHAP) mean score of each model for the NOTCH pathway to determine which genes of the pathway have been important classifiers; that is, genes with an important expression correlation with JAK2. f The heatmap of the NOTCH pathway and HOXA family generated using MPN microarray datasets from43 validate NOTCH expression in our model. HOXA heatmap confirms HOXA bimodality. “JAK2” and “TET2” refer to the single mutant mouse models, “DM” the double mutant with JAK2 mutated first and “WT” the wild-type (no mutation) genotype. Source data are provided as a Source Data file.
Based on this JAK2/TET2/HOXA9 motif, we refined our computational model to reproduce the observed biological differences between patients with different combinations of JAK2 and TET2 mutations (Supplementary Data). To do so, we extended our computational network with six phenotypes relevant to cancer development: stem cell self-renewal, common myeloid progenitor (CMP) expansion, granulocyte-monocyte progenitor (GMP) expansion, GMP differentiation, erythroid differentiation and megakaryocyte-erythroid progenitor (MEP) expansion (Fig. 3b). We further included important hematopoietic markers in our computational model. We found that additional interactions such as the activation of MYB by RUNX1 are also required to reproduce the correct biological features of MPN (Table 1). A detailed literature review and full description of how we built the network model are available in Tables S1–3 and the Supplemental Methods.
Finally, four fundamental cancer genotypes are defined: the wild-type (no mutation), the TET2 single mutant, the JAK2 single mutant and the double mutant (in either order) (Table 1). The wild-type model illustrates haematopoiesis in its healthy state. The single mutants are defined using the literature (see Supplementary Information). The final genotype is the double mutant which can lead to one of two cancer endpoints (fixpoint attractors that represent one of the two clinical outcomes). Each fixpoint represents either TET2 first or JAK2 first double mutants and are defined from results presented by Ortmann et al.13. Our computational model as shown in Fig. 3b reproduces the expected behaviours described in Table 1 and therefore the clinical stratification observed in Ortmann et al.13. The model suggests that the elevated differentiation observed in the JAK2 first double mutants13 is induced by the increased expression of RUNX1, KLF1 and GATA1 as well as the downregulation of MYC not found in TET2 first double mutant. This gene expression difference between double mutants can partly explain the divergent clinical behaviours between the two groups of patients, including the increased risk of thrombosis and the faster diagnosis as a result of the abnormally high number of differentiated cells in these patients.
The self-loop on HOXA9 plays a fundamental role in determining model behaviour. To explore how it influences cell phenotypes, we tested three different possible outcomes of removing it from the model. Simply removing HOXA9 self-activation in our model results in its stable overexpression in the double mutant genotype (Fig. S5), as the impact of the JAK2 mutation overwhelms the effect of the TET2 mutation. However, the loss of this interaction could lead to more complex outcomes. For example, HOXA9 may be dependent on a basal level of self-activation to act in the cell. To explore this, we also tested the case where removal of the self-loop causes HOXA9 null activity (Fig. S6) and stabilisation of the double mutant. Finally, the impact of the mutations could compensate for one another in the absence of the self-loop, leading the double mutant to have wild-type activity levels. In this situation, the model is unstable due to the interactions between SPI1 and GATA1, though fewer variables are involved in the instability (Fig. S7). We conclude generally that loss of HOXA9 self-activation leads to the partial or total loss of bifurcation in the model and its responsiveness to the order of mutations. This reinforces the importance of the self-positive feedback loop in determining cell phenotype and the subsequent clinical separation of patients with differing orders of JAK2 and TET2 mutations.
MPN network predicts gene dynamics and interactions
The computational model identifies gene dynamics as part of the MPN disease progression. In the complete network model, HOXA9 requires both JAK2 and TET2 expression to remain active (Table S3). Upregulation of either JAK2 or HOXA9 results in the hyperactivation of HOXA9 while TET2 loss causes inactivation. Wild-type activity is maintained by the balance of these two genes. JAK2 activation mutation and TET2 loss both drive the system into a committed state. JAK2 activation raises HOXA9 activity to a level at which it can maintain its activity through control of its own expression. Subsequent loss of TET2 does not impact its activity as this hyperactivation makes it independent of TET2. Conversely, TET2 loss causes a loss of HOXA9 expression in the cell, rendering it insensitive to subsequent JAK2 activation. This occurs as HOXA9 expression drops, preventing a subsequent response to JAK2 activation due to low concentration of the protein in the cell. Therefore, a possible explanation of the order dependence could be a combination of mutual dependency between JAK2 and TET2 to activate HOXA9, combined with the positive feedback self-loop of HOXA9 itself.
One key feature of TET2-first MPN patients is their reduced sensitivity to Ruxolitinib, a JAK2 inhibitor drug13. Interestingly our computational model suggests that after TET2 loss, RUNX1 expression is unchanged by JAK2 activation mutation due to the “switching” property exerted by HOXA9 self-loop (Fig. 3c). However, this gene is affected by JAK2 mutation in the context of TET2 wild-type expression (Fig. S10). It follows that JAK2 inhibition is therefore inefficient for this important hematopoietic regulator which could explain the reduced effect of Ruxolitinib in TET2 first patients.
Whilst building single mutant phenotypes, we noticed a relationship between JAK2 and GMP expansion is required to match the increased number of myeloid progenitors observed in organisms with a JAK2 mutation. To explore possible pathways downstream of JAK2 that could explain this link to myeloid diseases, we applied a machine learning approach (XGBoost) to AML TCGA data as a relevant and closely related blood cancer. We found that JAK2 is highly correlated with the NOTCH pathway (Fig. 3d), which has been found to act as a tumour suppressor in leukaemia due to the large expansion of GMP cells after loss of NOTCH signalling35. From the SHAP scores (SHapley Additive exPlanations, which are feature contribution measurements) in the classification of NOTCH genes plotted in Fig. 3e, we identified ITCH to be among the top 5 genes with the highest mean SHAP scores in the NOTCH pathway and found a pathway linking JAK2 to ITCH from a search of the literature. ITCH controls the degradation of NOTCH36 and is found to be induced by JNK137 from the MAPK pathway which is a well-known downstream pathway of JAK2/STAT538. We therefore suggest that the JAK2 path to GMP expansion could be MAPK and NOTCH pathway dependent.
Another interaction predicted by our network model is the inhibition of MYB by RUNX1. The CMP are found to be differentially expanded between JAK2 and TET2 first patients in Ortmann et al13. In our initial model, we included an inhibition interaction between SPI1 and MYB, our CMP expansion marker, a connection which has been observed experimentally39. This inhibition and the stable SPI1 expression in the double mutant states prevented the known bifurcation in CMP expansion in double mutants. Further investigations lead us to suggest that the bifurcation could be obtained by replacing SPI1 by RUNX1 for MYB inhibition, and this additional set of interactions is supported by multiple studies. RUNX1 activates SPI1 and GATA1, and both are found to be inhibitors of MYB39,40. Additionally, conditional knockout of RUNX1 in mice results in enhanced CMP frequencies41,42 All together, these findings suggest that RUNX1 can be linked to CMP expansion via MYB inhibition.
Validation of the role of NOTCH pathway, HOXA9 bimodality and its link to prognosis, and the interaction of JAK2 with HOXA9 through public datasets and experiments
To validate the predictions arising from our MPN computational model, we compared our findings to public MPN data not used in the model construction. Chen et al. compare MPN with different JAK2 and TET2 mutational profiles using transcriptomic mouse data43. We compared the gene expression of pathways/gene subsets to those we have included in our model to determine if our model fits their data. We first find that the NOTCH pathway behaves as predicted (Fig. 3f). We also find that the trend in the expression of RUNX1, MYC, and MYB support our model (Fig. S11–13 and Table S2). HOXA9 expression also showed a “switching” behaviour in this mouse model, that is the first JAK2 mutation has locked HOXA9 into a specific expression level and the second mutation in the JAK2-first double mutant cohort does not subsequently cause it to revert to wild-type. Confusingly however, low expression of HOXA9 is associated with JAK2 mutations and high expression with TET2 mutations. To confirm this trend, we examine the expression of other HOX genes that are closely correlated to HOXA9 and find the same pattern.
Jeong et al.44 previously demonstrated the direct phosphorylation of TET2 by JAK2 in a combination of in vitro human/murine hematopoietic cell lines with erythroid characteristics. Once phosphorylated TET2 activates KLF1, an important positive regulator of erythropoiesis45. In this context, loss of TET2 implies reduced erythroid differentiation which is in agreement with our model. In the same study, the authors show in a murine cell line that JAK2 mutation leads to HOXA9 upregulation. These findings are consistent with our JAK2/TET2/HOXA9 motif but disagree with Chen’s microarray experiments where HOXA9 expression is lowered in JAK2 single and double mutants (Fig. 3f). Given the downstream genes follow the expected expression, this raises the question of whether the activations in the original motif should be replaced by a pair of inhibitions, to make the model consistent with Chen data. Whilst there exist possible routes to connect TET2 and HOXA9 through an inhibition, we are however unable to find evidence of inhibition of HOXA9 by JAK2. We further note that as the Jeong data are human derived, it may be a more representative experimental model system. Future work using experiments in human samples could resolve this discrepancy. Both datasets however support the role of HOXA9 as a binary switch in MPN.
In light of these observations, we sought to test the relationship between JAK2 and HOXA9 through experimentation. Our model predicts that mutation of JAK2 would lead to activation of HOXA9 through STAT5. HOXA9 activity has been linked to cell viability18 and inhibition of HOXA9 would be expected to lead to a reduction of the number of colonies formed in a plating assay. We would therefore predict that mutation of JAK2 would increase colony formation relative to wild-type when HOXA9 is inhibited. Using wild-type and JAK2 mutated stem and progenitor cells, we knocked down HOXA9 and observed a reduction in colony formation in wild-type cells. We do, however, see a slight significant increase in colony formation in JAK2-mutant cells relative to wild-type whether or not HOXA9 is inhibited (q = 0.0171). This finding is more consistent with our model, and the data set from Jeong et al.44, where JAK2 activates HOXA9. TET2 behaviour is more complex, making an unsignificant increase to viability in WT but apparently synergistically increasing survival when HOXA9 is inhibited (q = 0.0032, Fig. 4a, b). This suggests that colony formation is determined through complex HOXA9 and TET2 interactions, necessitating further study.
a The ratios of colonies produced per sample are expressed as Scrambled:shHOXA9 colony number ratio with means. b The normalised colony count per sample and per condition with means and interquartile ranges of the three replicates. Two-way ANOVA statistical tests using multiple comparisons with FDR correction indicate a significant increase of colonies for TET2 mutant versus WT cells with shHOXA9 \((q=0.0032)\) and JAK2 mutant cells in both WT (\(q=0.0171\)) and in shHOXA9 \((q=0.0171)\) contexts. Source data are provided as a Source Data file.
Discussion
Out of 6817 genes tested HOXA9 is the single most highly correlating factor for poor prognosis due to treatment failure in AML17. HOXA9 could be argued to influence clinical characteristics in a continuous way, for example, if there was a broad unimodal distribution of HOXA9 expression across patients and if HOXA9 expression correlated with survival. Here we have demonstrated that instead it acts in AML as a discrete switch rather than a spectrum. This impacts AML clinical characteristics such as classification and survival. We further propose the prognosis marker role of the HOXA9 gene to another blood disorder, MPN. While HOXA9 loss and overexpression are detrimental for normal cell development16, our model assumes an intermediate activity for HOXA9 in the healthy state. We show that in MPN diseases with JAK2/TET2 mutations, HOXA9 high expression is found in the JAK2 first patients while TET2 first patients display lower HOXA9 expression. As JAK2 first patients have a higher risk of developing thrombosis compared to TET2 first patients, and as thrombotic events are the main causes of death in MPNs patients46, this further suggests a deleterious influence of HOXA9 high expression on patient clinical outcomes in another myeloid disease and emphasise the role of HOXA9 as a marker of poor prognosis in blood malignancies.
In addition to providing insights into the regulatory control of cancer cell fate through HOXA9, our computational network model recapitulates the disease symptoms using well-known hematopoietic transcription factors. Further investigations of these genes could benefit clinicians by designing new drugs or applying already existing treatments to reduce symptoms and the risk of developing blast phase MPN. In addition to the specific claims of the model, several other clinical implications arise. Whilst JAK2 is the main driver mutation found in all MPN patients, different diseases with distinct clinical traits can be observed26. Until now, the source of this clinical diversity following JAK2 mutation was unclear. Here, we demonstrate that patients who first had a TET2 mutation have a reduced number of erythroid cells as a result of TET2 indirect downregulation of GATA1 and KLF1, which explains the reduced number of PV diseases in TET2 first patients despite the presence of JAK2 mutation13. While JAK2 dysregulation may be the principal driver of MPNs, other mutations shape the disease clinical type by altering the normal development of distinct hematopoietic subpopulations. Finally, we predict the involvement of the NOTCH pathway in MPN diseases. NOTCH shows both oncogenic and tumour suppressor roles in different tissues and in the hematopoietic system: NOTCH favours cancer growth in T acute lymphoblastic leukaemia through its MYC activation but is also found to augment the host immune response against cancer by activation of M1 macrophages47. The role of NOTCH in hematopoietic stem and progenitor cells is still an on-going debate, however, it seems that a certain level of NOTCH signalling is required to protect individuals from haematological malignancies48. We suggest that JAK2 increases GMP expansion through its inhibitory effect on NOTCH via the MAPK pathway and ITCH and so predict a tumour suppressor role for NOTCH in the GMP cell population.
In building these models, several choices were made that potentially limit the further interpretation. Firstly, whilst all gene interactions included in this model are derived from studies of blood, due to paucity of information individual interactions may come from either mouse and human studies. Secondly, the precise role of the self-loop on HOXA9 cannot be determined from our model alone. In the double mutant, the loss of the self-loop can lead to either abrogation (Fig. S6), wild-type (Fig. S7) or overexpression of HOXA9 as a result of JAK2 constitutive activity (Fig. S5). This wild-type scenario in which JAK2 and TET2 mutations balance out HOXA9 activity is able to respond to alternative orders of mutations through interactions between SPI1 and GATA1 (Fig. S12), albeit with phenotypes inconsistent with the disease13. Removing the HOXA9 positive feedback loop in our model leads to its overexpression and loss of the bifurcation in the double mutant, changing HOXA9 function in our model to obtain a wild-type expression restores the bifurcation in these cells (Fig. S12). However, CMP expansion is stable in both steady states which is not observed in patients with both mutations13. Finally, our model uses discrete values for gene expression and genomic data for validation, and represents a population of blood cells. Despite the historic successes of such approaches49 modelling this network with continuous methods could help validate the model and give additional insights. Future work could also include using asynchronous updates and modelling the decision-making processes of individual cells, to better understand cancer fate commitment.
Our network model suggests a mechanism for understanding how cancer fate can be determined through regulatory switches and highlights several new areas for further studies. It also allows us to identify potentially important discrepancies in experimental studies.
Methods
Our research complies with all relevant ethical regulations. The mouse study was undertaken under UK Home Office Licence granted to Dr. Kent (PEAD116C1) which was approved by the local AWERB committee and UK Home Office.
Analysis and visualisation of public cancer datasets
AML patient data contains RNA sequencing information from 173 patients. We used the logarithmic Transcripts Per Million (log2 TPM+ 1) normalised data. Low expressed genes are excluded (defined as a gene for which more than 50 samples have a TPM value <1). The R package multimode50 was used to determine the significance of gene expression bimodality and the modetest command to reject unimodality with the default ACR (Ameijeiras-Crujeiras-Rodríguez) method, a multimodality test combining the use of a critical bandwidth and an excess mass statistic51, using a p value of 0.05. We used the R package Survival52 to plot the survival curves and compute the p values of the log-rank test. We plotted Sankey diagrams with the Plotly Python Open Source Graphing library (available at https://plot.ly).
Differentially expressed genes in HOXA9 cohorts
We used a python script to separate patients between the two HOXA9 expression peaks found in the AML data from TCGA. In all, 40 patients are found in the low peak (Fig. 2a), in which we remove the nine patients with a null value for HOXA9 expression. We defined the high peak as the 80 patients with an expression between 4 and 5.5 for HOXA9. We found that subsequent analyses are robust to alternative high peak thresholds (Fig. S1). We compute the absolute difference of the mean expression of each gene between each cohort to find the genes which are most differentially expressed between the two groups of patients. We subsequently ranked the genes from the highest to the lowest absolute difference and take the top 30 genes from this list. This workflow was repeated using the fold change between cohorts. The top 30 genes from this set predominantly included either genes in the HOX family or genes with no determined role in haematopoiesis. This finding coincides with subsequent analyses of HOXA9 cohorts using the R package DESeq253 in which differentially expressed genes cannot be classified into specific hematopoietic functions (Fig. S2).
Microarray data analysis
While 12 samples are described in the paper we used for the MPN mouse transcriptomic data43, only 11 could be found in the public data, with one wild-type sample missing in the microarray.
For analysis, from the set of all transcripts in the microarray, the genes with a low detection p value (below 0.05) were filtered and transformed with quantile normalisation. The ComplexHeatmap R library was used to plot the heatmaps54.
XGBoost
XGBoost (eXtreme Gradient Boosting) was used to rank different gene pathways that have been well described in cancer to identify which pathways and genes amongst these pathways have the highest correlation with JAK2 and its expression level in the AML patients55. Thirteen pathways were chosen through the literature (Table S4). A model is trained and validated for each pathway. More details can be found in the Supplementary Information.
Executable network model of MPN
Computational models of MPN cancer fate determination were constructed as a qualitative network (QN) in the BioModelAnalyzer56. This process is described in more detail in Supplemental methods, but briefly QNs are constructed from reported gene interactions in the wider literature, and refined by testing model behaviour against reported phenotypes.
Experimental validation of JAK2/HOXA9 interaction
Full details are presented in Supplementary Methods. Briefly, all mice are originally on a C57/Bl6 background with the TET2 mice originally obtained via Prof. Anjana Rao (La Jolla, USA) and the JAK2 V617F mice obtained via Prof. Anthony Green (Cambridge, UK). Haemopoetic stem cells were isolated by flow cytometry cell sorting and cultured (Fig. S14, S15). For HOXA9 gene knockdown experiments, three biological replicates were generated from each genotype for two different conditions (noneffective scrambled control- and shHOXA9-transduced cells). Colony forming assays were performed, with colonies characterised and counted after 14 days. Normalised number of colonies grown in each replicate was calculated per 100 colonies plated into each well. Statistical analysis to determine statistically significant differences was done through an unpaired Student’s t test (GraphPad Prism, v 9.0.2).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The AML patient data were generated by TCGA and downloaded with Firebrowse (RNAseq, [http://firebrowse.org/]). The AML clinical data from TCGA was downloaded with cBioportal (www.cbioportal.com). The microarray dataset reported in ref. 43 is available in the ArrayExpress repository at European Molecular Biology Laboratory–European Bioinformatics Institute (http://www.ebi.ac.uk/arrayexpress/) and is accessible through the ArrayExpress accession number E-MTAB-2986. Raw colony count data are presented in the paper in full - images of colonies are available in Fig. S16. Source data are provided with this paper.
Code availability
Python and R scripts described in this section are available at ref. 57.
References
Spivak, J. L. Myeloproliferative neoplasms. N. Engl. J. Med. 376, 2168–2181 (2017).
Tefferi, A. et al. Blast phase myeloproliferative neoplasm: Mayo-agimm study of 410 patients from two separate cohorts. Leukemia 32, 1200–1210 (2018).
Yogarajah, M. & Tefferi, A. Leukemic transformation in myeloproliferative neoplasms: a literature review on risk, characteristics, and outcome. in Mayo Clinic Proceedings, vol. 92, pp. 1118–1128 (Elsevier, 2017).
Tefferi, A. et al. Long-term survival and blast transformation in molecularly annotated essential thrombocythemia, polycythemia vera, and myelofibrosis. Blood 124, 2507–2513 (2014).
Tefferi, A. et al. Survival and prognosis among 1545 patients with contemporary polycythemia vera: an international study. Leukemia 27, 1874–1881 (2013).
Barbui, T. et al. Survival and disease progression in essential thrombocythemia are significantly influenced by accurate morphologic diagnosis: an international study. J. Clin. Oncol. 29, 3179–3184 (2011).
Grove, C. S. & Vassiliou, G. S. Acute myeloid leukaemia: a paradigm for the clonal evolution of cancer?. Dis. Model. Mech. 7, 941–951 (2014).
Bacher, U. et al. Further correlations of morphology according to fab and who classification to cytogenetics in de novo acute myeloid leukemia: a study on 2235 patients. Ann. Hematol. 84, 785–791 (2005).
Aynardi, J. et al. Jak2 v617f-positive acute myeloid leukaemia (aml): a comparison between de novo aml and secondary aml transformed from an underlying myeloproliferative neoplasm. a study from the bone marrow pathology group. Br. J. Haematol. 182, 78–85 (2018).
Lindsley, R. C. Uncoding the genetic heterogeneity of myelodysplastic syndrome. Hematol. Am. Soc. Hematol. Educ. Program Book 2017, 447–452 (2017).
Kent, D. G. & Green, A. R. Order matters: the order of somatic mutations influences cancer evolution. Cold Spring Harb. Perspect. Med. 7, a027060 (2017).
Clarke, M. A., Woodhouse, S., Piterman, N., Hall, B. A. & Fisher, J. Using state space exploration to determine how gene regulatory networks constrain mutation order in cancer evolution in Automated reasoning for systems biology and medicine. pp. 133–153 (Springer, 2019).
Ortmann, C. A. et al. Effect of mutation order on myeloproliferative neoplasms. N. Engl. J. Med. 372, 601–612 (2015).
Bach, C. et al. Leukemogenic transformation by hoxa cluster genes. Blood 115, 2910–2918 (2010).
Lewis, E. W. A gene complex controlling segmentation in drosophila in Genes, development and cancer. pp. 205–217 (Springer, 1978).
Bhatlekar, S., Fields, J. Z. & Boman, B. M. Hox genes and their role in the development of human cancers. J. Mol. Med. 92, 811–823 (2014).
Golub, T. R. et al. Molecular classification of cancer: class discovery and class prediction by gene expression monitoring. Science 286, 531–537 (1999).
Faber, J. et al. Hoxa9 is required for survival in human mll-rearranged acute leukemias. Blood 113, 2375–2385 (2009).
Shima, Y., Yumoto, M., Katsumoto, T. & Kitabayashi, I. Mll is essential for nup98-hoxa9-induced leukemia. Leukemia 31, 2200–2210 (2017).
Zhong, X. et al. Hoxa9 transforms murine myeloid cells by a feedback loop driving expression of key oncogenes and cell cycle control genes. Blood Adv. 2, 3137–3148 (2018).
C. G. A. R. Network. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N. Engl. J. Med. 368, 2059–2074 (2013).
Rejlova, K. et al. Low hox gene expression in pml-rarα-positive leukemia results from suppressed histone demethylation. Epigenetics 13, 73–84 (2018).
Lasa, A. et al. Meis 1 expression is downregulated through promoter hypermethylation in aml1-eto acute myeloid leukemias. Leukemia 18, 1231–1237 (2004).
Byrd, J. C. et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from cancer and leukemia group b (calgb 8461) presented in part at the 43rd annual meeting of the american society of hematology, orlando, fl, december 10, 2001, and published in abstract form. 59. Blood 100, 4325–4336 (2002).
Wang, Z.-Y. & Chen, Z. Acute promyelocytic leukemia: from highly fatal to highly curable. Blood 111, 2505–2515 (2008).
Levine, R. L. et al. Activating mutation in the tyrosine kinase jak2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell 7, 387–397 (2005).
Delhommeau, F. et al. Mutation in tet2 in myeloid cancers. N. Engl. J. Med. 360, 2289–2301 (2009).
Chiba, S. Dysregulation of tet2 in hematologic malignancies. Int. J. Hematol. 105, 17–22 (2017).
Paterson, Y. Z. et al. A toolbox for discrete modelling of cell signalling dynamics. Integr. Biol. 10, 370–382 (2018).
Xiong, W. & Ferrell, J. E. A positive-feedback-based bistable memory module that governs a cell fate decision. Nature 426, 460–465 (2003).
Zhao, S. et al. Jak2, complemented by a second signal from c-kit or flt-3, triggers extensive self-renewal of primary multipotential hemopoietic cells. EMBO J. 21, 2159–2167 (2002).
de Bock, C. E. et al. Hoxa9 cooperates with activated jak/stat signaling to drive leukemia development. Cancer Discov. 8, 616–631 (2018).
Bei, L. et al. Regulation of cdx4 gene transcription by hoxa9, hoxa10, the mll-ell oncogene and shp2 during leukemogenesis. Oncogenesis 3, e135–e135 (2014).
Bocker, M. T. et al. Hydroxylation of 5-methylcytosine by tet2 maintains the active state of the mammalian hoxa cluster. Nat. Commun. 3, 1–12 (2012).
Klinakis, A. et al. A novel tumour-suppressor function for the notch pathway in myeloid leukaemia. Nature 473, 230–233 (2011).
Chastagner, P., Israel, A. & Brou, C. Aip4/itch regulates notch receptor degradation in the absence of ligand. PloS ONE 3, e2735 (2008).
Gallagher, E., Gao, M., Liu, Y.-C. & Karin, M. Activation of the e3 ubiquitin ligase itch through a phosphorylation-induced conformational change. Proc. Natl Acad. Sci. 103, 1717–1722 (2006).
de Freitas, R. M. & da Costa Maranduba, C. M. Myeloproliferative neoplasms and the jak/stat signaling pathway: an overview. Rev. Bras. Hematol. Hemoter. 37, 348–353 (2015).
Bellon, T., Perrotti, D. & Calabretta, B. Granulocytic differentiation of normal hematopoietic precursor cells induced by transcription factor pu. 1 correlates with negative regulation of the c-myb promoter. Blood 90, 1828–1839 (1997).
Zhao, W., Kitidis, C., Fleming, M. D., Lodish, H. F. & Ghaffari, S. Erythropoietin stimulates phosphorylation and activation of gata-1 via the pi3-kinase/akt signaling pathway. Blood 107, 907–915 (2006).
Ichikawa, M. et al. Aml-1 is required for megakaryocytic maturation and lymphocytic differentiation, but not for maintenance of hematopoietic stem cells in adult hematopoiesis. Nat. Med. 10, 299–304 (2004).
Ichikawa, M. et al. Aml1/runx1 negatively regulates quiescent hematopoietic stem cells in adult hematopoiesis. J. Immunol. 180, 4402–4408 (2008).
Chen, E. et al. Distinct effects of concomitant jak2v617f expression and tet2 loss in mice promote disease progression in myeloproliferative neoplasms. Blood 125, 327–335 (2015).
Jeong, J. J. et al. Cytokine-regulated phosphorylation and activation of tet2 by jak2 in hematopoiesis. Cancer Discov. 9, 778–795 (2019).
Lohmann, F. & Bieker, J. J. Activation of eklf expression during hematopoiesis by gata2 and smad5 prior to erythroid commitment. Development 135, 2071–2082 (2008).
Cervantes, F., Passamonti, F. & Barosi, G. Life expectancy and prognostic factors in the classic bcr/abl-negative myeloproliferative disorders. Leukemia 22, 905–914 (2008).
Aster, J. C., Pear, W. S. & Blacklow, S. C. The varied roles of notch in cancer. Annu. Rev. Pathol. 12, 245–275 (2017).
Lampreia, F. P., Carmelo, J. G. & Anjos-Afonso, F. Notch signaling in the regulation of hematopoietic stem cell. Curr. Stem Cell Rep. 3, 202–209 (2017).
Emmert-Streib, F., Dehmer, M. & Haibe-Kains, B. Gene regulatory networks and their applications: understanding biological and medical problems in terms of networks. Front. Cell Dev. Biol. 2, 38 (2014).
J. Ameijeiras-Alonso, J., Crujeiras, R. M. & Rodrguez-Casal, A. Multimode: an r package for mode assessment. J. Stat. Softw. 97, 1–32 (2018).
Ameijeiras-Alonso, J., Crujeiras, R. M. & Rodrguez-Casal, A. Mode testing, critical bandwidth and excess mass. Test 28, 900–919 (2019).
Therneau T. & Lumley, T. R survival package (2013).
Love, M., Anders, S. & Huber, W. Differential analysis of count data–the deseq2 package. Genome Biol. 15, 10–1186 (2014).
Gu, Z., Eils, R. & Schlesner, M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics 32, 2847–2849 (2016).
Chen T. & Guestrin, C. Xgboost: a scalable tree boosting system. In Proceedings of the 22nd acm sigkdd international conference on knowledge discovery and data mining, pp. 785–794 (2016).
Benque, D. et al. Bma: Visual tool for modeling and analyzing biological networks. In International Conference on Computer Aided Verification. pp. 686–692, Springer, 2012.
Talarmain, L. et al. HOXA9 has the hallmarks of a biological switch with implications in blood cancer. Zenodo https://doi.org/10.5281/zenodo.6913664 (2022).
Acknowledgements
We thank members of the Hall group, the Fisher group at the University College London Cancer Institute, and Aleksandra Watson at the University of Cambridge for valuable discussions. B.A.H. acknowledges support from the Royal Society (grant no. UF130039), the Medical Research Council (grant no. MR/S000216/1), and Microsoft Research. J.F. was supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre and Cancer Research UK. L.C.C. is supported by a CR-UK Programme Foundation award to D.G.K. (DCRPGF\100008). The D.G.K. laboratory is supported by an ERC Starting Grant (ERC-2016-STG-715371), a CR-UK Programme Foundation award (DCRPGF\100008), and an MRC-AMED joint award (MR/V005502/1).
Author information
Authors and Affiliations
Contributions
L.T. performed the experiments, analysed data, and wrote all versions of the manuscript. B.H. conceived, supervised the study, and wrote and edited the manuscript. D.S. supported data analysis. D.K. and L.C. performed experimental validation. L.T., M.C., D.S., L.C., D.K., J.F., and B.H. all edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Simon Mitchell and the other anonymous reviewer(s) for their contribution to the peer review of this work. Peer review reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Talarmain, L., Clarke, M.A., Shorthouse, D. et al. HOXA9 has the hallmarks of a biological switch with implications in blood cancers. Nat Commun 13, 5829 (2022). https://doi.org/10.1038/s41467-022-33189-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-022-33189-w
This article is cited by
-
Exploring the expression and clinical significance of the miR-140-3p-HOXA9 axis in colorectal cancer
Journal of Cancer Research and Clinical Oncology (2024)
-
Order-of-Mutation Effects on Cancer Progression: Models for Myeloproliferative Neoplasm
Bulletin of Mathematical Biology (2024)
-
HOXA9 transcription factor is a double-edged sword: from development to cancer progression
Cancer and Metastasis Reviews (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.