Abstract
Greater adherence to the Mediterranean diet has beneficial effects on the prevention of chronic diseases. In the current study, we investigated the association between the Mediterranean diet score (MDS) and the 6-year incidence of chronic kidney disease (CKD), conducted in the framework of the Tehran Lipid and Glucose Study with 1212 adults, aged 30–71 years. Dietary intake was assessed using a valid and reliable food-frequency questionnaire, and all subjects received scores between 0 and 8 points based on the traditional MDS. The components of the MDS were fruits and nuts, vegetables, legumes, cereals, fish, meat, dairy products and the monounsaturated to saturated fatty acid ratio. The odds ratio (OR) for the occurrence of CKD according to the quartiles of the MDS was assessed by multivariable logistic regression. The mean (s.d.) age of participants (51% male) at baseline was 43.5 (9.4) years. The median (25–75 interquartile range) of MDS for all subjects was 4 (3–5).The incidence of CKD was 19%. After adjustment for all potential confounding variables, individuals in the highest quartile of the MDS were 51% less likely to have CKD than those in the lowest quartile (OR=0.49; 95% confidence interval (CI): 0.30–0.82). Additionally, after further adjustment for baseline estimated glomerular filtration rate (GFR), the inverse association between the MDS and the 6-year incidence of CKD remained significant (OR=0.53; 95% CI: 0.31–0.91). Our findings demonstrate a significant inverse association between the MDS and the risk of incident CKD, indicating that adherence to the Mediterranean diet has favorable effects on the prevention of kidney dysfunction.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a major public health problem characterized by the presence of albuminuria, a glomerular filtration rate (GFR) <60 ml min−1 1.73 m−2 for ⩾3 months and structural and functional damage to the kidney.1, 2 The prevalence and incidence of CKD are rising rapidly worldwide, highlighting it as one of the greatest contributors to the global burden of disease by increasing the risk of cardiovascular disease and mortality.3, 4 Hypertension, diabetes and obesity are multifactorial abnormalities that are readily treatable risk factors for the most common causes of mortality and morbidity, in particular, CKD.2, 5 In the recent global data, the prevalence of diabetes was estimated to be 10.9%, and it is projected to increase to 11.3% by 2035;6 prevalence of hypertension was >20%7 in the Middle East and Africa. Moreover, other genetic and environmental factors, including nutritional factors and dietary patterns, are major contributing risk factors for CKD.8, 9, 10
Most of the meals consumed consist of a wide variety of foods with a mixture of nutrients; therefore, assessing the role of dietary patterns in the pathogenesis of a chronic disease instead of a single food or nutrient is far more important and valuable. One such dietary pattern is the Mediterranean diet, characterized as follows: a high intake of vegetables, legumes, fruits and cereals, and the unsaturated fatty acids/saturated fatty acids ratio; a moderately high intake of fish; a low-to-moderate intake of dairy products; a low intake of meat and poultry; and a regular but moderate amount of wine.11 This dietary pattern has received much attention recently for its benefits in the prevention of cardiovascular disease, diabetes, metabolic syndrome, neurological diseases and cancer and in the reduction of overall mortality.12, 13, 14
Currently, limited controversial data are available on the relationship between the Mediterranean diet and kidney function markers.15, 16, 17, 18 Some previous studies indicated that the possible beneficial effects of adherence to the Mediterranean diet include the prevention of albuminuria,17 GFR decline15 and reductions in serum levels of urea and creatinine.16 However, in one controlled clinical trial study, the long-term favorable effects of the Mediterranean dietary pattern on kidney function were not confirmed.18 To the best of our knowledge, only one study investigated the association between the adherence to the Mediterranean dietary pattern and the incidence of CKD, indicating the positive role of this dietary pattern in decreasing the risk of CKD;19 however, because this study was conducted on old men, it may not be extensible to the general population.
Considering data on the high incidence of CKD in Iranian populations and the beneficial effects of the Mediterranean diet on kidney function, derived predominantly from investigations performed in developed countries and the lack of data from developing ones viz. from the MENA (Middle East and North Africa) region, we aimed to examine the association between the adherence to the Mediterranean dietary pattern and the risk of incident CKD among Tehranian adults.
Methods
Subjects
The present study was performed within the framework of the Tehran Lipid and Glucose Study (TLGS), a population-based prospective study conducted to determine the risk factors for non-communicable diseases among a representative urban population of Tehran, including 15 005 participants aged ⩾ 3 years.20 This study was performed using multistage cluster random sampling methods. The first phase of the TLGS began in March 1999 and data collection, conducted at 3-year intervals, is ongoing; the baseline survey was a cross-sectional study conducted from 1999 to 2001, and surveys 2 (2002–2005), 3 (2006–2008), 4 (2009–2011) and 5 (2012–2015) were prospective follow-up surveys. In the third survey of the TLGS (2006–2008), from the 12 523 participants, 3462 were randomly selected and agreed to complete the dietary assessment.
For the current study, a total of 1905 individuals, aged 30–70 years, with complete data in the third survey of the TLGS (baseline examination) were enrolled and followed to the fifth survey (outcome examination) (median follow-up: 6.1 years). Subjects who under- or over-reported dietary intakes (<800 kcal per day or >4200 kcal per day respectively) or who were on specific diets (n=88), those with a history of myocardial infraction, cerebral vascular accident and cancers (n=30) and those with CKD (n=439) were excluded. Of the 1348 non-CKD subjects at baseline, 1212 participants remained for the final analysis after a 6.1-year follow-up (follow-up rate: 90%, Figure 1).
The study protocol was approved by the ethics committee of the Research Institute for Endocrine Sciences, affiliated with the Shahid Beheshti University of Medical Sciences, Tehran, Iran. Written informed consent was obtained from all of the subjects.
Dietary intake assessment
A valid and reliable 168-item semi-quantitative food-frequency questionnaire was used to assess the food intake of subjects over the previous year.21 Trained dietitians, with at least 5 years of experience in the TLGS survey, asked participants to designate their consumption frequency for each food item during the previous year on a daily, weekly or monthly basis. The portion sizes of consumed foods were reported in household measures and then converted to grams. The dietary intakes from the third survey of the TLGS were considered to be the dietary intake exposure at baseline.
The Mediterranean diet score (MDS) was determined according to Trichopoulou et al.,11 focusing on the following eight components: a high intake of legumes, vegetables, nuts and fruits, and cereals; a high dietary ratio of monounsaturated fatty acid (MUFA) to saturated fatty acid (SFA); a moderately high intake of fish; a low-to-moderate intake of dairy products, mostly in the form of cheese or yogurt; and a low intake of meat and poultry. Each food component was energy adjusted using the energy density method (g per 1000 kcal) to determine the MDS. The sex-specific median intake in the population was considered as the cutoff for each of the eight food components of a typical Mediterranean diet; a value of 1 was assigned to a high intake (⩾median) of each of the desirable components, that is, fruits and nuts, vegetables, legumes, cereals and fish, or to a low intake (< median) of each of the detrimental foods, that is, meat and dairy products. Additionally, individuals whose consumption was at or above the median for detrimental foods and below the median for desirable foods were assigned a value of 0. For fat intake, we used the ratio of daily consumption (in grams) of MUFA to SFA; a value of 1 was assigned if this ratio was greater than the sex-specific median value and a value of zero was assigned for consumption less than the median.22 For religious reasons, alcohol consumption is not common in Iranian populations, and because of under-reporting, alcohol consumption cannot be properly estimated in our country. Therefore, alcohol consumption was not considered to be a food component. We then summed up the points for all eight items to calculate the MDS. Thus, the total MDS ranged from zero (no adherence) to 8 (maximal adherence).
Physical activity assessment
The Modifiable Activity Questionnaire, used for assessing the physical activity levels of participants, has been previously modified and validated among Iranians.23 Individuals were asked to report and identify the frequency and time spent during the past 12 months on activities of light, moderate, hard, and very hard intensity, according to a list of common activities of daily life; the physical activity levels were expressed as metabolic equivalent hours per week (MET-h per week).
Clinical and biological measurements
The participants were interviewed by trained interviewers using pretested questionnaires. Information on age, sex, medical history, medication use and smoking habits was collected. Anthropometric measures, including weight, height and waist circumference, were measured, and body mass index (BMI) was calculated. Weight was measured and recorded while the subjects were minimally clothed, without shoes or socks, using a digital scale with an accuracy of up to 100. Height was measured in a standing position without shoes, using a stadiometer with a minimum measurement of 1 mm, while the shoulders were in normal alignment. BMI was computed as weight in kilograms divided by height in meters squared. Waist circumference was measured at the level of the umbilicus, over light clothing, using an unstretched shape tape meter without any pressure to the body surface, and the measurements were recorded to the nearest 0.1 cm. Blood pressure was measured twice on the right arm after resting for at least 15 min while sitting on chair with a minimum interval of 30 s, using a mercury sphygmomanometer and the Korotkoff sound technique with an accuracy of 2 mm Hg; the average of the two measurements was considered to be the final pressure. We recorded the systolic blood pressure when the first sound was heard and the diastolic blood pressure when the sound disappeared. A blood sample was taken after 12–14 h of overnight fasting in a sitting position according to the standard protocol and centrifuged within 30–45 min of collection. All of the blood analyses were performed at the TLGS research laboratory on the day of blood collection. The samples were analyzed using the Selectra 2 auto-analyzer (Vital Scientific, Spankeren, The Netherlands). Fasting plasma glucose (FPG) was measured using an enzymatic colorimetric method with glucose oxidase. Both inter- and intra-assay coefficient variations were 2.2% for FPG. For the oral glucose tolerance test, 82.5 g of glucose monohydrate solution (equivalent to 75 g anhydrous glucose) was administered orally to subjects, aged >20 years, except for diabetics on medication. A second blood sample was taken 2 h after glucose ingestion. The serum creatinine levels were assayed according to the standard colorimetric Jaffe Kinetic reaction method. Both intra- and inter-assay coefficient variations were <3.1%. These analyses were performed using commercial kits (Pars Azmoon, Tehran, Iran).
Definitions
According to the criteria of the American Diabetes Association, subjects with FPG ⩾126 mg dl−1, with a 2-h post 75 g glucose load ⩾200 mg dl−1 or who were on current therapy for a definite diagnosis of diabetes were defined as having diabetes.24 Hypertension was defined as any of the following: systolic blood pressure ⩾140, diastolic blood pressure ⩾90 or taking antihypertensive medications.25 Smoking status included smokers (subjects who smoked cigarettes daily or occasionally) and non-smokers.
For this study, the MDRD (Modification of Diet in Renal Disease) equation formula was used to express estimated GFR (eGFR) in ml min−1 1.73 m−2 of body surface area.26 The abbreviated MDRD study equation is as follows:

Using national kidney foundation guidelines, the subjects were classified based on their eGFR levels as follows: eGFR ⩾60 ml min−1 1.73 m−2 for the non-CKD group and eGFR <60 ml min−1 1.73 m−2 for the CKD group.
Statistical analysis
The Statistical Package for Social Sciences (version 15.0; SPSS, Chicago, IL, USA) was used for the analysis. To assess the normality of the variables, histogram charts and a Kolmogorov–Smirnov analysis were used, indicating that all of the variables had a normal distribution. The baseline characteristics of the subjects were expressed as the mean ± s.d. for continuous variables and percentages for categorical variables. Chi-square and independent sample t-tests were used for the comparison of qualitative and quantitative variables, respectively, between subjects with and without CKD. Subjects were categorized according to quartiles of MDS cutoff points. To estimate the risk of 6-year incident outcomes, multivariable logistic regression models were used with CKD as the dependent variable and MDS as an independent variable; the odds ratio (OR) and 95% confidence interval (CI) were reported. Logistic regression models were adjusted for sex, age, smoking status, physical activity, total calorie intake, BMI, diabetes, hypertension and baseline eGFR. P-values <0.05 were considered to be statistically significant.
Results
The mean (s.d.) age of the study population (51% male) was 43.50 (9.40) years. The median (25–75 interquartile range) of the MDS was 4 (3–5) for all subjects, and the incidence of CKD was 19% after 6.1 years of follow-up.
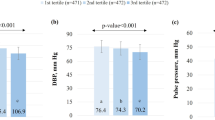
The baseline characteristics of the study population are shown in Table 1. Compared with non-CKD subjects, participants with CKD were significantly older, had lower eGFR and higher prevalence of diabetes and hypertension at baseline (P<0.05). Non-CKD participants also spent less time on leisure physical activity (P <0.05). No significant differences in smoking status and BMI were observed between subjects in the CKD and non-CKD groups. Regarding baseline characteristics of subjects according to quartiles of the MDS, subjects in the upper quartile had higher systolic blood pressure and FPG compared with those in the lowest, whereas there were no significant differences in all of the other factors according to MDS quartiles (Table 2).
The energy-adjusted (g per 1000 kcal) means (s.d.) for dietary intakes across the quartiles of the MDS are shown in Table 3. The dietary intakes of cereals, fruit and nut, fish, vegetables and legumes were significantly increased across the quartiles of the total MDS (P<0.05), whereas dairy and meat intakes were significantly decreased in subjects across the quartiles of the MDS (P<0.001). Participants in the highest quartile of MDS had a lower intake of protein, total fat, SFA and calcium than those in the lowest. In contrast, total energy intake, carbohydrate, polyunsaturated fatty acids, potassium, magnesium and total dietary fiber were all increased across the quartiles of the MDS (P<0.001).
The association between MDS and risk of incident CKD is shown in Table 4. In the multivariable-adjusted model, after adjustment for potential confounding variables, including sex, age, smoking status, physical activity, total calorie intake, BMI, diabetes and hypertension, subjects in the highest quartile had a 51% lower risk of CKD compared with those in the lowest quartile of the MDS (OR=0.49; 95% CI, 0.30–0.82). After further adjustment for baseline eGFR, the inverse association between high MDS and 6-year incidence of CKD remained significant (OR=0.53; 95% CI, 0.31–0.91). Furthermore, every 1-point increase in the MDS was associated with an 11% reduced risk of incident CKD at follow-up ((OR=0.89; 95% CI, 0.80–1.00), P=0.05).
Discussion
In the current prospective cohort study with a median follow-up of 6 years, we found that a greater adherence to the Mediterranean dietary pattern was associated with a 50% lower risk of incident CKD, independent of BMI, diabetes and hypertension, among an urban population of Tehran. In addition, the association between the MDS and the risk of CKD remained significant after controlling for the effect of baseline eGFR.
Similar to the above findings, Huang et al.19 indicated that subjects in the highest quartile of the Mediterranean dietary pattern had a 42% decreased risk of CKD; although, in contrast to ours, their study was conducted among elderly men and the effect of baseline eGFR was not adjusted Their results were in agreement with those of a cohort study that also reported on the protective role of the Mediterranean diet on the reduction of incident CKD in an elderly population.15 Some epidemiologic studies, however, show inconsistent findings regarding the effects of the Mediterranean dietary pattern on kidney function markers, including serum urea and creatinine levels and albuminuria.16, 17, 18 The Leontio Lyceum Albuminuria (3L study), a study of Greek adolescents, documented the beneficial effects of a higher adherence to the Mediterranean diet by showing that it was a protective factor against increased levels of urinary albumin excretion.17 Additionally, the ATTICA study indicated a reduction in serum levels of urea and creatinine and an increase in creatinine-clearance rates as markers of kidney function in healthy individuals with a higher adherence to the Mediterranean diet.16 However, in a controlled clinical trial study with 1-year dietary intervention, Díaz-López et al.18 found no beneficial effects of the Mediterranean diet on kidney function, explained by a limitation, that is, the length of intervention was not enough to detect protective effects of dietary patterns.18
The dietary intakes of subjects across the quartiles of the MDS suggest that a higher adherence to the MDS is accompanied with healthier and favorable food patterns that are rich in potassium, magnesium, vitamins, dietary fiber, omega-3 fatty acids and antioxidant compounds. However, subjects in the lower quartiles of the MDS had a dietary pattern similar to the Western pattern, which is rich in red and processed meat, animal fat, sweets and desserts and poor in fruits, vegetables, legumes and fiber,27 leading to an increase in sodium and animal protein intake, and high net endogenous acid production and heightening the workload for the kidneys.28 The Western-style diet is also positively related to inflammatory factors, such as C-reactive protein, interleukin-6, increased levels of urine albumin excretion and a decline in GFR.28, 29 Therefore, the beneficial effect of the MDS on CKD may be due to its relatively unknown but inherent dietary factors.
Some components of the MDS, including fruits, vegetables and nuts, which are rich in antioxidant compounds (including vitamins (vitamins C and E, α-tocopherol, β-carotene), selenium and polyphenols) may explain the positive effects of the MDS, as they are believed to have potential roles in preventing or improving cardiovascular risk factors and promoting health status.30 Additionally, a high consumption of animal protein damages kidney function;27 adherence to the Mediterranean diet, a low animal protein diet, that is, a moderate intake of dairy and red meat and a high intake of some micronutrients (including vitamins C, E, cobalamin, folate, magnesium and potassium), prevents the reduction of GFR, renal failure and promote kidney function.16, 31, 32 People with great adherence to the Mediterranean diet have a higher intake of fish. It has been reported that the omega-3 fatty acid content of fish and a high MUFA/SFA ratio improve plasma lipid profiles, insulin resistance, endothelial function, and reduce blood pressure, creatinine-clearance rate and inflammatory markers.33, 34, 35 Plant-derived foods (fruit, vegetables, legumes and whole-grains) are Mediterranean diet components with a high fiber content, low glycemic index and load; strong evidence supports the protective effects of these foods against potential CKD risk factors, such as obesity, diabetes and cardiovascular disease.36, 37 Additionally, fiber-rich components of the Mediterranean diet, which induce satiety and reduce energy intake, prevent or control CKD risk factors, including obesity and diabetes.38 Finally, sodium intake, an important factor in decreasing GFR, creatinine-clearance rate and raising blood pressure,39 was reported to be lower in individuals with a higher adherence to the Mediterranean diet.40
The Mediterranean diet and its components, which are rich in antioxidant foods and nutrients (vitamins, minerals, fibers, omega-3 fatty acids and phytochemicals), may prevent CKD and its potential risk factors, such as hypertension, diabetes and obesity, through the improvement of lipid profiles, HbA1c, plasma glucose, blood pressure, insulin sensitivity, endothelial function, inflammatory biomarkers (CRP, interleukin-6, interleukin-18 and tumor necrosis factor-α) and oxidative stress.41, 42, 43, 44, 45, 46 Additionally, due to its low content of salt, animal protein, phosphate and acid load, this diet can decrease the workload of nephrons and improve endothelial function.19, 43
Some limitations of the current study should be noted. Although, it has been recommended that creatinine should be measured three times to enhance the accuracy, to detect CKD, we measured creatinine only once, as is conducted in most epidemiologic studies. Additionally, the findings of the current study are not applicable to Mediterranean countries; however, these results can be generalized to non-Mediterranean countries, such as those in the Middle East and North Africa. Furthermore, despite adjusting for the confounding effects of various variables in our analysis, residual confounding due to unknown or unmeasured confounders, such as household income, occupation status, albuminuria/proteinuria, fluid intakes, HBA1c and fat free mass, cannot be excluded. Despite these limitations, to date, this is the first population-based cohort study that examined the association between the MDS and the incidence of CKD conducted in the MENA region. Furthermore, its long duration of follow-up and use of a valid and reliable food-frequency questionnaire and physical activity questionnaire are other strengths of this study.
In conclusion, the present findings indicate that a higher adherence to the Mediterranean dietary pattern is associated with a decreased risk of CKD in non-Mediterranean countries, such as Iran, and may be a useful strategy for the prevention of CKD. Further population-based studies and randomized controlled trials with longer durations are recommended to confirm these findings.
References
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002; 39: S1–266.
Levey AS, Coresh J . Chronic kidney disease. Lancet (London, England) 2012; 379: 165–180.
Grams ME, Chow EKH, Segev DL, Coresh J . Lifetime incidence of CKD stages 3-5 in the United States. Am J Kidney Dis 2013; 62: 245–252.
Zhang Q-L, Rothenbacher D . Prevalence of chronic kidney disease in population-based studies: systematic review. BMC Public Health 2008; 8: 117.
Kanzaki G, Tsuboi N, Haruhara K, Koike K, Ogura M, Shimizu A, Yokoo T . Factors associated with a vicious cycle involving a low nephron number, hypertension and chronic kidney disease. Hypertens Res 2015; 38: 633–641.
Majeed A, El-Sayed AA, Khoja T, Alshamsan R, Millett C, Rawaf S . Diabetes in the Middle-East and North Africa: an update. Diabetes Res Clin Pract 2014; 103: 218–222.
Arnaout MS, Almahmeed W, Ibrahim M, Ker J, Khalil MT, Van Wyk CT, Mancia G, Al Mousa E . Hypertension and its management in countries in Africa and the Middle East, with special reference to the place of beta-blockade. Curr Med Res Opin 2011; 27: 1223–1236.
Gopinath B, Harris DC, Flood VM, Burlutsky G, Mitchell P . A better diet quality is associated with a reduced likelihood of CKD in older adults. Nutr Metab Cardiovasc Dis 2013; 23: 937–943.
Wakasugi M, Kazama JJ, Yamamoto S, Kawamura K, Narita I . A combination of healthy lifestyle factors is associated with a decreased incidence of chronic kidney disease: a population-based cohort study. Hypertens Res 2013; 36: 328–333.
Jain N, Reilly RF . Effects of dietary interventions on incidence and progression of CKD. Nat Rev Nephrol 2014; 10: 712–724.
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D . Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 2003; 348: 2599–2608.
Giugliano D, Esposito K . Mediterranean diet and metabolic diseases. Curr Opin Lipidol 2008; 19: 63–68.
Sofi F, Abbate R, Gensini GF, Casini A . Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr 2010; 92: 1189–1196.
Mirmiran P, Moslehi N, Mahmoudof H, Sadeghi M, Azizi F . A longitudinal study of adherence to the Mediterranean dietary pattern and metabolic syndrome in a non-Mediterranean population. Int J Endocrinol Metab 2015; 13: e26128.
Khatri M, Moon YP, Scarmeas N, Gu Y, Gardener H, Cheung K, Wright CB, Sacco RL, Nickolas TL, Elkind MS . The association between a Mediterranean-style diet and kidney function in the Northern Manhattan Study cohort. Clin J Am Soc Nephrol 2014; 9: 1868–1875.
Chrysohoou C, Panagiotakos DB, Pitsavos C, Skoumas J, Zeimbekis A, Kastorini CM, Stefanadis C . Adherence to the Mediterranean diet is associated with renal function among healthy adults: the ATTICA study. J Ren Nutr 2010; 20: 176–184.
Mazaraki A, Tsioufis C, Dimitriadis K, Tsiachris D, Stefanadi E, Zampelas A, Richter D, Mariolis A, Panagiotakos D, Tousoulis D, Stefanadis C . Adherence to the Mediterranean diet and albuminuria levels in Greek adolescents: data from the Leontio Lyceum ALbuminuria (3L study). Eur J Clin Nutr 2011; 65: 219–225.
Díaz-López A, Bullo M, Martinez-Gonzalez MA, Guasch-Ferre M, Ros E, Basora J, Covas MI, del Carmen Lopez-Sabater M, Salas-Salvado J . Effects of Mediterranean diets on kidney function: a report from the PREDIMED trial. Am J Kidney Dis 2012; 60: 380–389.
Huang X, Jimenez-Moleon JJ, Lindholm B, Cederholm T, Arnlov J, Riserus U, Sjogren P, Carrero JJ . Mediterranean diet, kidney function, and mortality in men with CKD. Clin J Am Soc Nephrol 2013; 8: 1548–1555.
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, Mehrabi Y, Zahedi-Asl S . Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials 2009; 10: 5.
Asghari G, Rezazadeh A, Hosseini-Esfahani F, Mehrabi Y, Mirmiran P, Azizi F . Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran Lipid and Glucose Study. Br J Nutr 2012; 108: 1109–1117.
Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, Vassilakou T, Lipworth L, Trichopoulos D . Diet and overall survival in elderly people. BMJ 1995; 311: 1457–1460.
Momenan AA, Delshad M, Sarbazi N, Rezaei Ghaleh N, Ghanbarian A, Azizi F . Reliability and validity of the Modifiable Activity Questionnaire (MAQ) in an Iranian urban adult population. Arch Iran Med 2012; 15: 279–282.
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2003; 26 (Suppl 1): S5–S20.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ . Committee tNHBPEPC. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206–1252.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D . A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 1999; 130: 461–470.
Odermatt A . The Western-style diet: a major risk factor for impaired kidney function and chronic kidney disease. Am J Physiol Renal Physiol 2011; 301: F919–F931.
Hariharan D, Vellanki K, Kramer H . The Western diet and chronic kidney disease. Curr Hypertens Rep 2015; 17: 1–9.
Lin J, Fung TT, Hu FB, Curhan GC . Association of dietary patterns with albuminuria and kidney function decline in older white women: a subgroup analysis from the Nurses' Health Study. Am J Kidney Dis 2011; 57: 245–254.
Slavin JL, Lloyd B . Health benefits of fruits and vegetables. Adv Nutr 2012; 3: 506–516.
Yuzbashian E, Asghari G, Mirmiran P, Hosseini FS, Azizi F . Associations of dietary macronutrients with glomerular filtration rate and kidney dysfunction: Tehran lipid and glucose study. J Nephrol 2015; 28: 173–180.
Farhadnejad H, Asghari G, Mirmiran P, Yuzbashian E, Azizi F . Micronutrient intakes and incidence of chronic kidney disease in adults: Tehran Lipid and Glucose Study. Nutrients 2016; 8: 217.
Rasmussen BM, Vessby B, Uusitupa M, Berglund L, Pedersen E, Riccardi G, Rivellese AA, Tapsell L, Hermansen K . Effects of dietary saturated, monounsaturated, and n-3 fatty acids on blood pressure in healthy subjects. Am J Clin Nutr 2006; 83: 221–226.
Widmer RJ, Flammer AJ, Lerman LO, Lerman A . The Mediterranean diet, its components, and cardiovascular disease. Am J Med 2015; 128: 229–238.
Chrysohoou C, Pitsavos C, Panagiotakos D, Skoumas J, Lazaros G, Oikonomou E, Galiatsatos N, Striggou M, Xynogala M, Stefanadis C . Long-term fish intake preserves kidney function in elderly individuals: the Ikaria study. J Ren Nutr 2013; 23: e75–e82.
Estruch R, Salas-Salvadó J . Towards an even healthier mediterranean diet. Nutr Metab Cardiovasc Dis 2013; 23: 1163–1166.
Williams PG, Grafenauer SJ, O'Shea JE . Cereal grains, legumes, and weight management: a comprehensive review of the scientific evidence. Nutr Rev 2008; 66: 171–182.
Howarth NC, Saltzman E, Roberts SB . Dietary fiber and weight regulation. Nutr Rev 2001; 59: 129–139.
Liu X, Wang W, Chen W, Jiang X, Zhang Y, Wang Z, Yang J, Jones JE, Jose PA, Yang Z . Regulation of blood pressure, oxidative stress and AT1R by high salt diet in mutant human dopamine D5 receptor transgenic mice. Hypertens Res 2015; 38: 394–399.
Lin J, Hu FB, Curhan GC . Associations of diet with albuminuria and kidney function decline. Clin J Am Soc Nephrol 2010; 5: 836–843.
Sleiman D, Al-Badri MR, Azar ST . Effect of Mediterranean diet in diabetes control and cardiovascular risk modification: a systematic review. Front Public Health 2015; 3: 69.
Bekkouche L, Bouchenak M, Malaisse WJ, Yahia DA . The Mediterranean diet adoption improves metabolic, oxidative, and inflammatory abnormalities in Algerian metabolic syndrome patients. Horm Metab Res 2014; 46: 274–282.
Chiva-Blanch G, Badimon L, Estruch R . Latest evidence of the effects of the Mediterranean diet in prevention of cardiovascular disease. Curr Atheroscler Rep 2014; 16: 1–7.
Richard C, Couture P, Desroches S, Lamarche B . Effect of the Mediterranean diet with and without weight loss on markers of inflammation in men with metabolic syndrome. Obesity (Silver Spring) 2013; 21: 51–57.
Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, D'Armiento M, D'Andrea F, Giugliano D . Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA 2004; 292: 1440–1446.
Holt EM, Steffen LM, Moran A, Basu S, Steinberger J, Ross JA, Hong CP, Sinaiko AR . Fruit and vegetable consumption and its relation to markers of inflammation and oxidative stress in adolescents. J Am Diet Assoc 2009; 109: 414–421.
Acknowledgements
We express their appreciation to the participants in the Tehran Lipid and Glucose Study for their enthusiastic support and to the staff of the Research Institute for Endocrine Sciences, Tehran Lipid and Glucose Study Unit for their valuable help. We also wish to acknowledge Ms N Shiva for critically editing the English grammar and syntax of the manuscript. This work was funded by a grant from the Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran. All of the authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Asghari, G., Farhadnejad, H., Mirmiran, P. et al. Adherence to the Mediterranean diet is associated with reduced risk of incident chronic kidney diseases among Tehranian adults. Hypertens Res 40, 96–102 (2017). https://doi.org/10.1038/hr.2016.98
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.98
Keywords
This article is cited by
-
A Therapeutic Approach in the Management of Chronic Kidney Disease: Plant-Based Dietary Models and Associated Parameters
Current Nutrition Reports (2024)
-
High dietary and lifestyle inflammatory scores are associated with increased risk of chronic kidney disease in Iranian adults
Nutrition Journal (2023)
-
A Mediterranean diet is associated with improved total antioxidant content of human breast milk and infant urine
Nutrition Journal (2023)
-
Dietary and lifestyle indices for hyperinsulinemia with the risk of obesity phenotypes: a prospective cohort study among Iranian adult population
BMC Public Health (2022)
-
Dietary intakes of total polyphenol and its subclasses in association with the incidence of chronic kidney diseases: a prospective population‐based cohort study
BMC Nephrology (2021)