Abstract
Elevated circulating fatty acid-binding protein 4 (FABP4/A-FABP/aP2), an adipokine, is associated with obesity, insulin resistance, hypertension and cardiovascular events. However, how circulating FABP4 level is modified by pharmacological agents remains unclear. We here examined the effects of angiotensin II receptor blockers (ARBs) on serum FABP4 level. First, essential hypertensives were treated with ARBs: candesartan (8 mg day−1; n=7) for 2 weeks, olmesartan (20 mg day−1; n=9) for 12 weeks, and valsartan (80 mg day−1; n=94) or telmisartan (40 mg day−1; n=91) for 8 weeks added to amlodipine (5 mg day−1). Treatment with ARBs significantly decreased blood pressure and serum FABP4 concentrations by 8–20% without significant changes in adiposity or lipid variables, though the M value determined by hyperinsulinemic–euglycemic glucose clamp, a sensitive index of insulin sensitivity, was significantly increased by candesartan. Next, alterations in FABP4 secretion from 3T3-L1 adipocytes were examined under several agents. Lipolytic stimulation of the β-adrenoceptor in 3T3-L1 adipocytes by isoproterenol increased FABP4 secretion, and conversely, insulin suppressed FABP4 secretion. However, treatment of 3T3-L1 adipocytes with angiotensin II or ARBs for 2 h had no effect on gene expression or secretion of FABP4 regardless of β-adrenoceptor stimulation. In conclusion, treatment with structurally different ARBs similarly decreases circulating FABP4 concentrations in hypertensive patients as a class effect of ARBs, which is not attributable to blockade of the angiotensin II receptor in adipocytes. Reduction of FABP4 levels by ARBs might be involved in suppression of cardiovascular events.
Similar content being viewed by others
Introduction
Fatty acid-binding proteins (FABPs) are about 14–15-kDa predominantly cytosolic proteins that can reversibly bind hydrophobic ligands, such as saturated and unsaturated long chain fatty acids.1, 2 FABPs have been proposed to facilitate the transport of lipids to specific compartments in the cell. Among FABPs, fatty acid-binding protein 4 (FABP4), also known as adipocyte FABP (A-FABP) or aP2, is mainly expressed in both adipocytes and macrophages and has an important role in the development of insulin resistance and atherosclerosis.3, 4, 5 Furthermore, it has been shown that a small molecule FABP4 inhibitor could be a therapeutic strategy against diabetes mellitus and atherosclerosis.6
Recent studies have shown that FABP4 is secreted from adipocytes in association with lipolysis regulated by adenyl cyclase-protein kinase A and guanylyl cyclase-protein kinase G signaling via a non-classical secretion pathway,7, 8, 9 though there are no typical secretory signal peptides in the sequence of FABP4.1 It has also been shown that FABP4 acts as an adipokine for the development of hepatic insulin resistance8 and cardiodepressant effect10 in experimental models. Furthermore, elevated serum concentration of FABP4 has been shown to be associated with obesity, insulin resistance, hypertension, atherosclerosis, cardiac dysfunction and cardiovascular events.7, 11, 12, 13, 14, 15, 16, 17 However, little is known about the modulation of FABP4 concentration by drugs, including antihypertensive agents. Here we investigated the effects of angiotensin II receptor blockers (ARBs) on circulating FABP4 level in hypertensive patients and secretion of FABP4 from adipocytes with and without lipolytic stimulation, which is known to increase secretion of FABP4 from adipocytes.8
Methods
The present study consisted of three human studies (Studies 1–3) and one in vitro study using 3T3-L1 adipocytes (Study 4). Human studies (Studies 1–3) conformed to the principles outlined in the Declaration of Helsinki and were performed with the approval of the Ethical Committee of Sapporo Medical University. Written informed consent was received from all of the subjects. Experimental procedures for Study 4 were performed with approval from the Animal Care and Experiments Committee of Sapporo Medical University.
Study 1: Effects of candesartan on FABP4 levels
Mild-to-moderate essential hypertensive patients (n=7; M/F: 3/4; mean age: 56.1±6.4 years) were enrolled in Study 1 to examine the effect of candesartan on serum FABP4 level and its relationship with insulin sensitivity. Entry criteria were no medication for at least 2 weeks before the study and no evidence of complications, such as endocrine or metabolic disturbances, cerebrovascular or cardiovascular disease or renal disease. The patients were treated with 8 mg day−1 candesartan, an ARB, for 2 weeks in hospital. Insulin sensitivity was evaluated as the M value (metabolic clearance of glucose, mg m−2 min−1) by the hyperinsulinemic–euglycemic glucose clamp technique before and after treatment with candesartan. Before the clamp study, blood pressure was measured, and blood samples were obtained from all of the patients.
Study 2: Effects of olmesartan on FABP4 levels
Nine essential hypertensives (M/F: 4/5; mean age: 56.6±1.8 years) were enrolled from clinics affiliated with the Sapporo Medical University. Entry criteria were no treatment with antihypertensive agents, lipid-lowering agents or anti-diabetic agents and the absence of serious hepatic disease, renal disease or atherosclerosis. Patients were treated with 20 mg day−1 olmesartan, an ARB, for 12 weeks in outpatient clinics. Before and after the 12-week treatment, blood pressure was measured and blood samples were collected.
Study 3: Effects of telmisartan and valsaltan as add-on agents on FABP4 levels
In the SPEED (Sapporo study to prove efficacies of telmisartan and valsartan for early-morning blood pressure as add-on therapy) study (UMIN000003922),18 designed as a PROBE trial, 414 hypertensive patients in the age range of 40–79 years were enrolled from 36 clinical sites in a 4-week run-in period when amlodipine (5 mg day−1) was administered. Patients whose home systolic blood pressure in the morning was ⩾135 mm Hg but <160 mm Hg were randomized to a valsartan (80 mg day−1) group or to a telmisartan (40 mg day−1) group for an 8-week add-on therapy. Exclusion criteria were allergy to telmisartan or valsartan, pregnancy, severe liver dysfunction, serum creatinine >3.0 mg dl−1, malignant hypertension and secondary hypertension. Patients with chronic heart failure, atrial fibrillation, history of myocardial infarction, proteinuria, diabetes mellitus or metabolic syndrome were also excluded from enrollment in the run-in period. A total of 258 patients (128 patients in the valsartan group and 130 patients in the telmisartan group) contributed to the SPEED study as previously reported.18 In the present analysis, 73 of the SPEED study subjects who had been taking any drugs except amlodipine, valsartan and telmisartan were excluded, and data from 185 patients (94 patients in the valsartan group and 91 patients in the telmisartan group) were used for determining the effects of valsaratan and telmisartan on serum FABP level.
Measurements in Studies 1–3
Body mass index (BMI) was calculated as body weight (in kilograms) divided by the square of body height (in meters). Serum and plasma samples were analyzed immediately or stored at −80 °C until biochemical analyses. Serum concentration of FABP4 was measured using a commercially available Enzyme-Linked Immunosorbent Assay Kit for FABP4 (Biovendor R&D, Modrice, Czech Republic). The accuracy, precision and reproducibility of the kit have been described previously.7 As an index of renal function, estimated glomerular filtration rate was calculated by an equation for Japanese19: estimated glomerular filtration rate (ml min−1 1.73 m−2)=194 × Cr(−1.094) × age(−0.287) × 0.739 (if female). Homeostasis model assessment ratio (HOMA-R), an index of insulin resistance, was calculated by the previously reported formula: insulin (μU ml−1) × glucose (mg dl−1)/405.
Hyperinsulinemic–euglycemic glucose clamp in Study 1
In Study 1, a 2-h hyperinsulinemic–euglycemic glucose clamp was performed according to the method previously described.20, 21 The mean rate of glucose infusion for the last 30 min of the clamp was used as an index of insulin sensitivity (M value). The M value was expressed as milligrams of glucose per square meter of body surface area.
Study 4: Effects of ARBs on FABP4 secretion from 3T3-L1 adipocytes
All biochemical reagents were purchased from Sigma-Aldrich (St Louis, MO, USA) unless otherwise indicated. Preadipocyte 3T3-L1 cells were obtained from Health Science Research Resources Bank (Osaka, Japan). Differentiation of 3T3-L1 cells was performed as previously described.9 After overnight serum depletion by 0.5% bovine serum albumin in Dulbecco’s modified Eagle’s medium, the differentiated 3T3-L1 adipocytes were stimulated for 2 or 24 h with 1–10 μM angiotensin II, 0.5 μg ml−1 insulin, 10 μM ARB (olmesartan (Daiichi Sankyo, Tokyo, Japan), valsartan or telmisartan) or 10 μM troglitazone in the presence and absence of 10 μM isoproterenol in Dulbecco’s modified Eagle’s medium supplemented with 0.5% bovine serum albumin. The doses of reagents and incubation periods varied according to the experimental protocol. Each experiment was done in at least triplicate.
Quantitative real-time PCR
Total RNA was isolated using Trizol Reagent (Invitrogen, Carlsbad, CA, USA). One microgram of total RNA was reverse-transcribed by using the high-capacity cDNA Archive Kit (Applied Biosystems, Foster City, CA, USA). Quantitative real-time PCR analysis was performed using SYBR Green in the real-time PCR system (Applied Biosystems). The thermal cycling program was 10 min at 95 °C for enzyme activation and 40 cycles of denaturation for 15 s at 95 °C, 30-s annealing at 58 °C and 30-s extension at 72 °C. Two pairs of specific primers used are as follows: 5′-AAGGTGAAGAGCATCATAACCCT-3′ and 5′-TCACGCCTTTCATAACACATTCC-3′ for FABP4 and 5′-AGTCCCTGCCCTTTGTACACA-3′ and 5′-CGATCCGAGGGCCTCACTA-3′ for 18S rRNA as an internal control gene.
Western blotting analysis
The conditioned medium (CM) from adipocytes was filtered to obtain 10–50-kDa fractions of proteins using the Amicon Ultra 10 and 50K devices (Millipore, Billerica, MA, USA). Total protein content of the cell lysate (CL) was assessed by a microplate protein assay (Bio-Rad, Hercules, CA, USA). Western blotting analysis using primary antibodies for FABP4 (Abcam, Tokyo, Japan) and GAPDH (glyceraldehyde 3-phosphate dehydrogenase; Santa Cruz Biotechnology, Santa Cruz, CA, USA) was performed as previously described.9 Densitometry was performed using the ImageJ software (http://imagej.nih.gov/ij/).
Statistical analysis
Numeric variables are expressed as means±s.e.m. or medians (interquartile ranges). The distribution of each parameter was tested for its normality using Shapiro–Wilk W test, and non-normally distributed parameters were logarithmically transformed for regression analyses. The correlation between two variables was evaluated using Pearson’s correlation coefficient. Comparison between two groups was done with Wilcoxon signed-rank test for paired samples and Mann–Whitney’s U test for unpaired samples. A P-value of <0.05 was considered statistically significant. All data were analyzed by using JMP 9 for Macintosh (SAS Institute, Cary, NC, USA).
Results
Study 1
Characteristics of the patients in Study 1 are shown in Table 1. There were no significant differences in BMI, pulse rate or levels of fasting plasma glucose, total cholesterol, HDL cholesterol, LDL cholesterol or triglycerides before and after treatment with candesartan for 2 weeks. Treatment with candesartan significantly decreased mean blood pressure (101.9±4.8 vs. 91.2±5.0 mm Hg, P=0.004) and increased the M value (157.6±9.8 vs. 216.2±25.5 mg m−2 min−1, P=0.043). Fasting insulin level (4.9±0.6 vs. 3.2±0.2 μU ml−1, P=0.052) and HOMA-R (1.01±0.14 vs. 0.65±0.03, P=0.064) tended to decrease after treatment with candesartan. Candesartan significantly decreased serum FABP4 concentration by 14.5% (23.3±2.7 vs. 19.9±1.8 ng ml−1, P<0.05) (Figure 1a). Change in FABP4 level was not significantly correlated with change in the M value (r=0.234, P=0.613) or mean blood pressure (r=0.547, P=0.204).
Effects of candesartan and olmesartan on FABP4 levels (Studies 1 and 2). (a and b) Treatment with candesartan (8 mg day−1; n=7; M/F: 3/4) for 2 weeks (a) or olmesartan (20 mg day−1; n=9; M/F: 4/5) for 12 weeks (b) significantly decreased FABP4 levels in hypertensive patients. Open circle: male, closed circle: female. *P<0.05.
Study 2
Characteristics of the patients in Study 2 are shown in Table 2. Treatment with olmesartan for 12 weeks significantly decreased systolic blood pressure (162.9±4.3 vs. 141.7±6.8 mm Hg, P=0.007) and diastolic blood pressure (97.8±3.9 vs. 79.3±3.0 mm Hg, P=0.003), but no significant differences were found before and after treatment in BMI, waist circumference, pulse rate or levels of total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, fasting plasma glucose, insulin or HOMA-R. Olmesartan significantly decreased serum FABP4 level by 19.9% (13.8±1.5 vs. 11.1±1.3 ng ml−1, P=0.012; Figure 1b). Change in FABP4 level was not significantly correlated with change in systolic blood pressure (r=0.653, P=0.071), diastolic blood pressure (r=0.643, P=0.062) or other variables.
Study 3
Characteristics of the patients in Study 3 are shown in Table 3. There was no significant difference in BMI, waist circumference, blood pressure or pulse rate at baseline between the valsartan and telmisartan groups. Treatment with valsartan or telmisartan for 8 weeks added to amlodipine therapy significantly decreased systolic blood pressure (143.9±1.1 vs. 130.9±1.9 mm Hg, P<0.001 and 143.8±1.3 vs. 133.8±1.7 mm Hg, P<0.001, respectively) and diastolic blood pressure (83.1±0.9 vs. 75.9±1.4 mm Hg, P<0.001 and 84.2±1.0 vs. 77.9±1.1 mm Hg, P<0.001, respectively). However, no significant difference in the blood pressure level was observed between the valsartan and telmisartan groups before or after the add-on therapy. There was no significant difference in change in pulse rate or biochemical variables, including glucose and lipid metabolism or renal function, with valsartan or telmisartan treatment (Table 3).
When baseline data from all patients were pooled, logarithmically transformed FABP4 (log FABP4) level was positively correlated with BMI (r=0.451, P<0.001) and waist circumference (r=0.359, P<0.001) and was negatively correlated with estimated glomerular filtration rate (r=−0.374, P<0.001) as previously reported.7, 14 There were no significant correlations between log FABP4 and blood pressure, pulse rate, plasma glucose or lipid variables.
In the combined data from male and female subjects, serum FABP4 levels were significantly decreased by treatment with valsartan by 14.6% (15.8±0.6 vs. 13.5±0.6 ng ml−1, P<0.001) and by treatment with telmisartan by 8.4% (16.5±0.7 vs. 15.1±0.7 ng ml−1, P<0.001) (Figure 2a). However, no significant difference in change in FABP4 levels was found between the valsartan and telmisartan groups (Figure 2b). When divided into male and female subjects, reduction in FABP4 levels by valsartan and telmisartan was similarly observed (Figures 2c and d). However, change in FABP4 level in male subjects (Figure 2e), but not in female subjects (Figure 2f), was significantly greater in the valsartan group than in the telmisartan group. Change in FABP4 level was not significantly correlated with change in blood pressures or other variables.
Effects of valsartan and telmisartan on FABP4 levels (Study 3). (a) Serum FABP4 levels before and after treatment with valsartan (80 mg day−1; n=94; M/F: 49/45) or telmisartan (40 mg day−1; n=91; M/F: 46/45) for 8 weeks in addition to treatment with amlodipine (5 mg day−1) in hypertensive patients. (b) Change in FABP4 levels with valsartan and telmisartan treatment in all patients. (c and d) Serum FABP4 levels before and after treatment with valsartan and telmisartan in addition to treatment with amlodipine in male (c) and female (d) patients. (e and f) Change in FABP4 levels with valsartan and telmisartan treatment in male (e) and female (f) patients. Open circle and bar: valsartan group, closed circle and bar: telmisartan group. *P<0.05, **P<0.01 vs. Pretreatment.
Study 4
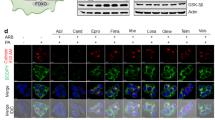
Treatment with several ARBs at the dose of 10 μM, including candesartan, olmesartan, valsartan and telmisartan, as well as 10 μM troglitazone, a peroxisome proliferator-activated receptor γ (PPARγ) agonist, for 2 h did not change gene expression of FABP4 in differentiated 3T3-L1 adipocytes (Figure 3a). However, when treatment was continued for 24 h, a significant increase in gene expression of FABP4, a target of PPARγ,1 was detected for telmisartan, an ARB with an action of a partial PPARγ agonist,22, 23 and troglitazone (Figure 3b).
Gene expression and secretion of FABP4 in 3T3-L1 adipocytes treated with ARBs (Study 4). (a and b) Gene expression of FABP4 was determined by quantitative real-time PCR in differentiated 3T3-L1 adipocytes treated with DMSO alone as a control (Con), 10 μM angiotensin II receptor blockers (ARBs), including candesartan (Can), olmesartan (Olm), valsartan (Val) and telmisartan (Tel), and 10 μM troglitazone (Tro) for 2 h (a) and 24 h (b) (n=3 each group). *P<0.01 vs. Con. (c–g) Western blotting analysis of FABP4 and GAPDH using the cell lysate (CL) and conditioned medium (CM) of 3T3-L1 adipocytes treated with several agents for 2 h (n=3 each group): (c) 10 μM isoproterenol (Iso) and 0.5 μg ml−1 insulin; (d) 10 μM Can, Olm, Val, Tel and Tro in the absence of Iso; (e) 10 μM Can, Olm, Val, Tel and Tro in the presence of 10 μM Iso; (f) 0–10 μM angiotensin II (Ang II) in the absence and presence of 10 μM Iso; and (g) 1 μM Ang II and 10 μM Olm in the absence and presence of 10 μM Iso. FABP4 secretion was relatively expressed as densitometry of FABP4 in the CM divided by those of FABP4 in the CL and GAPDH in the CL. AU, arbitrary unit. M, Marker of molecular weight. Error bars show s.e.m. in the graphs.
To assess secretion of FABP4 from differentiated 3T3-L1 adipocytes, the cells were treated with test agents for 2 h, and the levels of FAPB4 in CL and CM were determined. Western blotting analysis showed that FABP4 was present in both the CL and CM of 3T3-L1 adipocytes and that GAPDH, a non-secretory protein, was present in the CL but not in the CM (Figure 3c), indicating that FABP4 is indeed secreted from adipocytes with intact cell membranes. FABP4 secretion was induced by lipolytic stimulation with 10 μM isoproterenol, a pan-β-adrenergic agonist, and the increased FABP4 secretion was inhibited by 0.5 μg ml−1 insulin (Figure 3c), as previously reported.8, 9 Treatment with ARBs or troglitazone did not affect FABP4 secretion from adipocytes in the absence (Figure 3d) or presence (Figure 3e) of 10 μM isoproterenol.
Angiotensin II at the dose of 1–10 μM did not induce FABP4 secretion from 3T3-L1 adipocytes with or without stimulation of 10 μM isoproterenol (Figure 3f). No significant modulation in the level of FABP secretion was observed by treatment with olmesartan upon isoproterenol and/or angiotensin II stimulation (Figure 3g).
Discussion
The present study showed that treatment with structurally different and popular ARBs, including candesartan, olmesartan, valsartan and telmisartan, for 2–12 weeks similarly decreased serum FABP4 concentrations in hypertensive subjects, indicating a class effect of ARBs on circulating FABP4 levels. Our findings are consistent with the results of a previous study showing that longer treatment with olmesartan for 6 months decreased serum FABP4 levels in 30 patients with essential hypertension.24 In the present study, in vitro experiments showed that treatment with ARBs or angiotensin II for 2 h did not directly modulate FABP4 secretion from 3T3-L1 adipocytes under basal or isoproterenol-induced lipolytic conditions. The findings in adipocytes in vitro suggest that decline in serum FABP4 levels after ARB treatment is not a result of direct inhibition of FABP4 secretion from adipose tissue.
The precise mechanisms by which ARBs lead to a decrease in circulating FABP4 levels are unclear, but there are a few possibilities. First, suppression of sympathetic nerve activity and/or inflammatory cytokines by ARBs may indirectly suppress FABP4 release from adipose tissue. ARBs have been shown to reduce sympathetic nerve activation25 and inflammatory cytokines,26, 27 such as tumor necrosis factor-α, which are known to increase lipolysis in adipocytes.28 As FABP4 secretion is associated with lipolysis,8, 9 reduction of sympathetic tone possibly reduces FABP secretion. In that respect, the efficacy of FABP4 reduction by ARBs may be more effective in hypertensive patients with obesity who may have high sympathetic nerve activation. Second, improvement of insulin sensitivity by ARBs might be responsible for reduction in serum FABP4 level. As shown in Table 1, candesartan increased the M value, a sensitive index of insulin sensitivity as previously reported for several ARBs,21, 29, 30, 31 though HOMA-R, a less sensitive index of insulin sensitivity, was not significantly changed by ARBs used in the present study. Modest improvement in insulin sensitivity by ARBs may decrease FABP4 secretion from adipocytes via anti-lipolytic action of insulin. Finally, increase in small insulin-sensitive adipocytes by ARB treatment may result in decreased expression and secretion of FABP4. It has been hypothesized by Sharma et al.32 that blockade of the renin–angiotensin system promotes the recruitment and differentiation of preadipocytes and that increased formation of small insulin-sensitive adipocytes produce more adiponectin, a cell-protective adipokine, and less tumor necrosis factor-α, thereby improving insulin sensitivity. In fact, it has been reported that renin–angiotensin system blockade decreases adipocyte size in hypertensive and insulin-resistant rats33 and increases insulin sensitivity and serum levels of adiponectin in patients with essential hypertension.21
Telmisartan has been reported to have an action of a partial agonist of PPARγ.22, 23 In fact, gene expression of FABP4, a target of PPARγ,1 was increased by chronic (24 h), but not short-term (2 h), treatment with telmisartan as well as troglitazone, a PPARγ agonist, in 3T3-L1 adipocytes (Figures 3a and b). It has been reported that thiazolidinediones, PPARγ agonists, increase circulating FABP4 concentrations.34 Relatively small reduction in FABP4 level by telmisartan compared with that by valsartan (Figure 2a) might reflect increased FABP4 expression by telmisartan in adipocytes, which partly cancelled ARB-induced reduction in serum FABP4 levels.
Although ARBs reduced serum FABP4 level in both genders, valsartan-induced reduction in FABP4 level was significantly larger than the reduction by telmisartan in male subjects (Figure 2e) but not in female subjects (Figure 2f). It is also notable that baseline FABP4 level was higher in females than in males and that its level tended to be higher in the female telmisartan group than in the female valsartan group. Thus it is not clear whether gender difference in the baseline level of serum FABP4 or in response to each ARB underlies the finding that valsartan had a greater impact on serum FABP4 level than did telmisartan in males but not in females.
Recent clinical trials suggest that ARBs substantially lower the risk for type 2 diabetes and decrease cardiovascular events.35 Together with accumulating evidence indicating a significant role of FABP4 in insulin resistance and atherosclerosis, results of the present study support the notion that suppression of circulating FABP4 level is one of the important mechanisms by which ARBs prevent diabetes in high-risk hypertensive patients and the development of cardiovascular events.
The present study has some limitations. The number of subjects enrolled in Study 1 and Study 2 was small, and the possibility of type 1 error in statistical tests cannot be excluded. In Study 3, amlodipine taken before starting treatment with ARBs might have modulated the expression and secretion of FABP4, though there were no previous reports about such an effect. Additionally, the present study lacked a placebo control group. Interventional studies using larger number of subjects and a placebo-control design are necessary for determining the impact of ARB therapy on circulating FABP4 level and the relationship between change in FABP4 level and clinical benefit of ARBs. Finally, we performed in vitro experiments using mouse 3T3-L1 adipocytes, a well-used cell line of adipocytes, but there might be a difference between mouse and human in regulation of FABP4 secretion by ARBs.
In conclusion, ARBs decrease serum FABP4 concentrations in hypertensive patients as a class effect of ARBs, which is not attributable to blockade of the angiotensin II receptor in adipocytes. Reduction of FABP4 levels might contribute to the suppression of cardiovascular events as a pleiotropic effect of ARBs. Further understanding of drug-induced modulation of FABP4 secretion from adipocytes will enable the development of new therapeutic strategies for cardiovascular and metabolic diseases.
References
Furuhashi M, Hotamisligil GS . Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat Rev Drug Discov 2008; 7: 489–503.
Furuhashi M, Ishimura S, Ota H, Miura T . Lipid chaperones and metabolic inflammation. Int J Inflam 2011; 2011: 642612.
Hotamisligil GS, Johnson RS, Distel RJ, Ellis R, Papaioannou VE, Spiegelman BM . Uncoupling of obesity from insulin resistance through a targeted mutation in aP2, the adipocyte fatty acid binding protein. Science 1996; 274: 1377–1379.
Makowski L, Boord JB, Maeda K, Babaev VR, Uysal KT, Morgan MA, Parker RA, Suttles J, Fazio S, Hotamisligil GS, Linton MF . Lack of macrophage fatty-acid-binding protein aP2 protects mice deficient in apolipoprotein E against atherosclerosis. Nat Med 2001; 7: 699–705.
Furuhashi M, Fucho R, Gorgun CZ, Tuncman G, Cao H, Hotamisligil GS . Adipocyte/macrophage fatty acid-binding proteins contribute to metabolic deterioration through actions in both macrophages and adipocytes in mice. J Clin Invest 2008; 118: 2640–2650.
Furuhashi M, Tuncman G, Gorgun CZ, Makowski L, Atsumi G, Vaillancourt E, Kono K, Babaev VR, Fazio S, Linton MF, Sulsky R, Robl JA, Parker RA, Hotamisligil GS . Treatment of diabetes and atherosclerosis by inhibiting fatty-acid-binding protein aP2. Nature 2007; 447: 959–965.
Xu A, Wang Y, Xu JY, Stejskal D, Tam S, Zhang J, Wat NM, Wong WK, Lam KS . Adipocyte fatty acid-binding protein is a plasma biomarker closely associated with obesity and metabolic syndrome. Clin Chem 2006; 52: 405–413.
Cao H, Sekiya M, Ertunc ME, Burak MF, Mayers JR, White A, Inouye K, Rickey LM, Ercal BC, Furuhashi M, Tuncman G, Hotamisligil GS . Adipocyte lipid chaperone AP2 is a secreted adipokine regulating hepatic glucose production. Cell Metab 2013; 17: 768–778.
Mita T, Furuhashi M, Hiramitsu S, Ishii J, Hoshina K, Ishimura S, Fuseya T, Watanabe Y, Tanaka M, Ohno K, Akasaka H, Ohnishi H, Yoshida H, Saitoh S, Shimamoto K, Miura T . FABP4 is secreted from adipocytes by adenyl cyclase-PKA- and guanylyl cyclase-PKG-dependent lipolytic mechanisms. Obesity 2015; 23: 359–367.
Lamounier-Zepter V, Look C, Alvarez J, Christ T, Ravens U, Schunck WH, Ehrhart-Bornstein M, Bornstein SR, Morano I . Adipocyte fatty acid-binding protein suppresses cardiomyocyte contraction: a new link between obesity and heart disease. Circ Res 2009; 105: 326–334.
Xu A, Tso AW, Cheung BM, Wang Y, Wat NM, Fong CH, Yeung DC, Janus ED, Sham PC, Lam KS . Circulating adipocyte-fatty acid binding protein levels predict the development of the metabolic syndrome: a 5-year prospective study. Circulation 2007; 115: 1537–1543.
Yeung DC, Xu A, Cheung CW, Wat NM, Yau MH, Fong CH, Chau MT, Lam KS . Serum adipocyte fatty acid-binding protein levels were independently associated with carotid atherosclerosis. Arterioscler Thromb Vasc Biol 2007; 27: 1796–1802.
Ota H, Furuhashi M, Ishimura S, Koyama M, Okazaki Y, Mita T, Fuseya T, Yamashita T, Tanaka M, Yoshida H, Shimamoto K, Miura T . Elevation of fatty acid-binding protein 4 is predisposed by family history of hypertension and contributes to blood pressure elevation. Am J Hypertens 2012; 25: 1124–1130.
Ishimura S, Furuhashi M, Watanabe Y, Hoshina K, Fuseya T, Mita T, Okazaki Y, Koyama M, Tanaka M, Akasaka H, Ohnishi H, Yoshida H, Saitoh S, Miura T . Circulating levels of fatty acid-binding protein family and metabolic phenotype in the general population. PLoS ONE 2013; 8: e81318.
Fuseya T, Furuhashi M, Yuda S, Muranaka A, Kawamukai M, Mita T, Ishimura S, Watanabe Y, Hoshina K, Tanaka M, Ohno K, Akasaka H, Ohnishi H, Yoshida H, Saitoh S, Shimamoto K, Miura T . Elevation of circulating fatty acid-binding protein 4 is independently associated with left ventricular diastolic dysfunction in a general population. Cardiovasc Diabetol 2014; 13: 126.
Furuhashi M, Ishimura S, Ota H, Hayashi M, Nishitani T, Tanaka M, Yoshida H, Shimamoto K, Hotamisligil GS, Miura T . Serum fatty acid-binding protein 4 is a predictor of cardiovascular events in end-stage renal disease. PLoS ONE 2011; 6: e27356.
von Eynatten M, Breitling LP, Roos M, Baumann M, Rothenbacher D, Brenner H . Circulating adipocyte fatty acid-binding protein levels and cardiovascular morbidity and mortality in patients with coronary heart disease: a 10-year prospective study. Arterioscler Thromb Vasc Biol 2012; 32: 2327–2335.
Yoshida H, Akasaka H, Saitoh S, Shimamoto K, Miura T . Comparative effects of telmisartan and valsartan as add-on agents for hypertensive patients with morning blood pressure insufficiently controlled by amlodipine monotherapy. Hypertens Res 2014; 37: 225–231.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A, Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53: 982–992.
DeFronzo RA, Tobin JD, Andres R . Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 1979; 237: E214–E223.
Furuhashi M, Ura N, Higashiura K, Murakami H, Tanaka M, Moniwa N, Yoshida D, Shimamoto K . Blockade of the renin-angiotensin system increases adiponectin concentrations in patients with essential hypertension. Hypertension 2003; 42: 76–81.
Benson SC, Pershadsingh HA, Ho CI, Chittiboyina A, Desai P, Pravenec M, Qi N, Wang J, Avery MA, Kurtz TW . Identification of telmisartan as a unique angiotensin II receptor antagonist with selective PPARgamma-modulating activity. Hypertension 2004; 43: 993–1002.
Schupp M, Janke J, Clasen R, Unger T, Kintscher U . Angiotensin type 1 receptor blockers induce peroxisome proliferator-activated receptor-gamma activity. Circulation 2004; 109: 2054–2057.
Miyoshi T, Doi M, Hirohata S, Kamikawa S, Usui S, Ogawa H, Sakane K, Izumi R, Ninomiya Y, Kusachi S . Olmesartan reduces arterial stiffness and serum adipocyte fatty acid-binding protein in hypertensive patients. Heart Vessels 2011; 26: 408–413.
Krum H . Differentiation in the angiotensin II receptor 1 blocker class on autonomic function. Curr Hypertens Rep 2001; 3 (Suppl 1): S17–S23.
Takagi H, Mizuno Y, Yamamoto H, Goto SN, Umemoto T, All-Literature Investigation of Cardiovascular Evidence G. Effects of telmisartan therapy on interleukin-6 and tumor necrosis factor-alpha levels: a meta-analysis of randomized controlled trials. Hypertens Res 2013; 36: 368–373.
Hasan AU, Ohmori K, Hashimoto T, Kamitori K, Yamaguchi F, Ishihara Y, Ishihara N, Noma T, Tokuda M, Kohno M . Valsartan ameliorates the constitutive adipokine expression pattern in mature adipocytes: a role for inverse agonism of the angiotensin II type 1 receptor in obesity. Hypertens Res 2014; 37: 621–628.
Lafontan M, Langin D . Lipolysis and lipid mobilization in human adipose tissue. Prog Lipid Res 2009; 48: 275–297.
Shimoda S, Goto R, Furukawa N, Tsuruzoe K, Kawashima J, Iwashita S, Maeda T, Ichimori S, Ichinose K, Nishida K, Araki E . Effects of olmesartan, an angiotensin II receptor blocker, on peripheral insulin sensitivity in Japanese subjects with type 2 diabetes and hypertension. Intern Med 2012; 51: 2091–2096.
van der Zijl NJ, Moors CC, Goossens GH, Hermans MM, Blaak EE, Diamant M . Valsartan improves {beta}-cell function and insulin sensitivity in subjects with impaired glucose metabolism: a randomized controlled trial. Diabetes Care 2011; 34: 845–851.
Fogari R, Zoppi A, Ferrari I, Mugellini A, Preti P, Lazzari P, Derosa G . Comparative effects of telmisartan and eprosartan on insulin sensitivity in the treatment of overweight hypertensive patients. Horm Metab Res 2009; 41: 893–898.
Sharma AM, Janke J, Gorzelniak K, Engeli S, Luft FC . Angiotensin blockade prevents type 2 diabetes by formation of fat cells. Hypertension 2002; 40: 609–611.
Furuhashi M, Ura N, Takizawa H, Yoshida D, Moniwa N, Murakami H, Higashiura K, Shimamoto K . Blockade of the renin-angiotensin system decreases adipocyte size with improvement in insulin sensitivity. J Hypertens 2004; 22: 1977–1982.
Cabre A, Lazaro I, Girona J, Manzanares JM, Marimón F, Plana N, Heras M, Masana L . Fatty acid binding protein 4 is increased in metabolic syndrome and with thiazolidinedione treatment in diabetic patients. Atherosclerosis 2007; 195: e150–e158.
Elliott WJ, Meyer PM . Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet 2007; 369: 201–207.
Acknowledgements
We thank the members of SPEED investigators group for their cooperation in collection of data. MF has been supported by grants from JSPS KAKENHI, Uehara Memorial Foundation, SENSHIN Medical Research Foundation, Japan Diabetes Foundation, Takeda Medical Research Foundation, Ono Medical Research Foundation, Takeda Science Foundation, Akiyama Life Science Foundation and Yamaguchi Endocrine Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Furuhashi, M., Mita, T., Moniwa, N. et al. Angiotensin II receptor blockers decrease serum concentration of fatty acid-binding protein 4 in patients with hypertension. Hypertens Res 38, 252–259 (2015). https://doi.org/10.1038/hr.2015.2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.2
Keywords
This article is cited by
-
Glomerular expression and urinary excretion of fatty acid-binding protein 4 in IgA nephropathy
Journal of Nephrology (2023)
-
Elevated circulating FABP4 concentration predicts cardiovascular death in a general population: a 12-year prospective study
Scientific Reports (2021)
-
Detection of significantly high vitreous concentrations of fatty acid-binding protein 4 in patients with proliferative diabetic retinopathy
Scientific Reports (2021)
-
Treatment with anagliptin, a DPP-4 inhibitor, decreases FABP4 concentration in patients with type 2 diabetes mellitus at a high risk for cardiovascular disease who are receiving statin therapy
Cardiovascular Diabetology (2020)
-
The association between serum adipocyte fatty acid–binding protein and 3-month disability outcome after aneurysmal subarachnoid hemorrhage
Journal of Neuroinflammation (2020)