Abstract
Saroglitazar is a dual PPAR-α/γ agonist approved for the treatment of diabetic dyslipidemia. In addition to reduction in atherogenic lipids, it may also contribute to improvement in insulin sensitivity through PPAR-α/γ agonism, which remains unexplored. We conducted a randomized, double-blind, placebo-controlled trial in treatment-naive T2DM individuals with serum triglyceride >150 mg/dL. Participants were randomized to receive either saroglitazar 4 mg or placebo (1:1) daily for 4 months (n = 30). Insulin sensitivity (SIclamp) was studied using hyperinsulinemic-euglycemic clamp at baseline and at 4 months. We observed a significant reduction in TG (p = 0.001), HbA1c (p = 0.019) and fasting plasma glucose (p = 0.019) and significant increase in HDL-C levels (p < 0.01) with saroglitazar compared to placebo. Further, patients on saroglitazar had a greater improvement in SIclamp (p = 0.026) with the effect persisting despite adjusting for baseline weight, TG, HDL-C and HbA1c (p = 0.002). This was accompanied with significant increase in HOMA-β (p = 0.01) in the saroglitazar group and change in HOMA-β showed a trend towards significance with SIclamp (r = 0.503, p = 0.056). However, change in SIclamp did not significantly correlate with reduction in HbA1c and TG. We conclude that saroglitazar effectively reduces hypertriglyceridemia and improves insulin sensitivity along with β-cell function by reduction in gluco-lipotoxicity and possibly directly through PPAR-γ agonism in patients ofT2DM with hypertriglyceridemia.
Similar content being viewed by others
Introduction
Diabetic dyslipidemia, also known as atherogenic dyslipidemia comprises a triad of “raised triglycerides1, higher proportion of small dense low density lipoprotein-cholesterol (sdLDL-C) and low high density lipoprotein cholesterol-(HDL-C)2”. The presence of small dense LDL-C particles lead to accelerated atherosclerosis resulting in increased cardiovascular (CV) morbidity and mortality3. Statins, fibrates and omega-3 fatty acids are used for the management of diabetic dyslipidemia. While statins reduce cardiovascular events and decrease mortality, considerable residual cardiovascular risk persists despite receiving statin therapy4. Several studies designed to target this residual CV risk have shown variable outcomes. The AIM-HIGH (Atherothrombosis Intervention in Metabolic Syndrome With Low HDL/High Triglycerides)5 and HPS2-THRIVE (Heart Protection Study 2-Treatment of HDL to Reduce the Incidence of Vascular Events)trials6 aimed at raising HDL-C with niacin but failed to demonstrate the reduction in CV mortality.
Hypertriglyceridemia increases CV risk by resulting in remodelling of HDL-C and LDL-C particles rendering them smaller and denser. sdLDL-C particles are more atherogenic and sd HDL-C particles are dysfunctional, therefore increasing the CV disease risk7. A rise in TG levels by 1 mmol/l is estimated to raise the CV risk by 32% and 76% in men and women, respectively8,9. In addition, a global case-control study showed that microvascular disease odds ratio increased by a factor of 1.16 (95% confidence interval, 1.11–1.22) for every 0.5 mmol/L increase in triglycerides10, which make increased TGs a worthy target for treatment.
Fibrates through their action on PPAR-α are the “traditional” drug of choice to target hypertriglyceridemia. However, initial enthusiasm was dampened mainly owing to the results of two studies: the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study11 and the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study12. Both these studies could not demonstrate a significant reduction in CV risk either alone11 or in combination with statins12.
Glitazars are a group of drugs with dual PPAR- α/γ agonist action. A number of glitazars were developed, however, they could not make their position in the management of dyslipidemia owing to unacceptable adverse effects such as peripheral edema (faglitazar)13, carcinogenic potential (ragaglitazar)14, cardiovascular side-effects (muraglitazar)15 and bone marrow and renal toxicity (tesaglitazar).
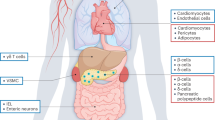
Saroglitazar is a novel PPAR-α/γ agonist, recently approved for diabetic dyslipidemia in India. As PPAR-α are predominantly expressed in the liver, it effectively reduces circulating atherogenic lipids and consequent decrease in lipotoxicity. Saroglitazar also reduces HbA1c partly through reduction in lipotoxicity as well as through its moderate PPAR-γ agonistic activity. A previous study showed that saroglitazar as an add-on to metformin had a greater lowering of TG and HbA1c, as compared to fenofibrate16. However, its efficacy in improving insulin sensitivity has been studied only in animal models till now10 and remains unexplored in human subjects. Therefore, we planned to study the effect of saroglitazar on insulin sensitivity in patients with type 2 diabetes mellitus (T2DM) with hypertriglyceridemia by hyperinsulinemic-euglycemic clamp.
Methods
Study design
It was designed as a double-blind placebo controlled randomised trial. The trial was registered at http://ctri.nic.in on 31 October 2017 (CTRI/2017/10/010306). The study was approved by the Institutional Ethics Committee of Post Graduate Institute of Medical Education and Research, Chandigarh. Written signed informed consent was obtained from all the patients included in the study. Participants were closely monitored to detect and promptly manage adverse events. The study was conducted following the principles of Declaration of Helsinki and Good clinical Practice as laid down by Indian Council of Medical Research17.
Patients
Treatment-naïve T2DM patients were recruited from the outpatient clinic at a tertiary care referral centre in India. Patients aged between 30 and 60 years, with disease duration <5 years, GAD-65 antibody negative, HbA1c 7.0–9.0%, serum fasting triglyceride >150 mg/dL and BMI 23–35 Kg/m2 were included.
Patients with type 1 diabetes mellitus or secondary diabetes, past history of diabetic ketoacidosis or having ketonemia or ketonuria, uncontrolled hypertension, thyroid disorder, renal dysfunction [defined by estimated glomerular filtration rate (eGFR) <60 ml/min/m2], hepatic dysfunction (serum aspartate transaminase/alanine transaminase (AST/ALT) ratio more than 2.5 times upper limit of normal, and/or total serum bilirubin more than 2 times upper limit of normal), myopathies, receiving statins, fibrates, hormone replacement therapies or steroids, seropositive for human immunodeficiency virus, hepatitis C virus or hepatitis B virus infection, recent cardiovascular event (<6 months), history of malignancy, active infection and alcohol (>14 units/week or 112 gm pure alcohol for men, >7 units/week or 56 gm pure alcohol for women)18 or drug abuse were excluded from the study. An informed consent was obtained from every patient prior to inclusion in the study. Since this was a pilot study, with 90% power and two-sided 5% significance for standardised medium effect size of 0.5, a sample size of 30 patients was considered optimal for the study.
After screening, subjects were randomised to receive saroglitazar 4 mg and placebo in 1:1 distribution for 4 months. Life-style modification was insisted to all patients as per ADA recommendations19. Patients were advised to perform self-monitoring of blood glucose (SMBG) including a five-point glucose profile once a week. Compliance was ensured by weekly phone call by the investigator. Tablet glimeperide (1 to 2 mg) was used as a ‘rescue therapy’ in either group, when fasting plasma glucose (FPG) exceeded 130 mg/dl or post prandial plasma glucose (PPG) >180 mg/dl. Block randomization was done and random numbers were generated12 using Microsoft Excel. Randomization concealment was achieved by placing random number codes in sealed tamper- proof envelopes and blinding was not disclosed to either the trial participant or assessor (NJ). NJ enrolled participants and AB allocated them to intervention.
Study assessments
Five visits were planned, including first visit at baseline and then monthly till the completion of the study. Liver function tests, renal function tests, lipid profile and fasting and 2 hour post- prandial glucose were performed at each visit. At baseline and at the end of 4 months, anthropometry was performed and glycated haemoglobin (HbA1c), C -peptide and high sensitivity C-reactive protein (hsCRP) were measured. HbA1c was measured using automated high-performance liquid chromatography (HPLC)-based system using ion-exchange cartridge (D-10, Bio-Rad Laboratories, Inc., Hercules, CA, USA). C-peptide estimation was done at baseline and 4 months by electrochemiluminiscence immunoassay (ECLIA) (Elecsys 2010, Roche Diagnostics GmbH, Mannheim, Germany). Body composition was also measured by dual energy x-ray absorptiometry (Hologic Inc, USA) at baseline and 4 months.
Patients underwent hyperinsulinemic euglycemic clamp study at inclusion and at the end of 4 months as per DeFronzo’s clamp technique20. Subjects were requested to refrain from vigorous exercise prior to the procedure and were asked to report at 0630 h after an overnight fast of 10 hours. Clamp was started at FPG levels of 110 mg/dl. If patient’s plasma glucose was more than 140 mg/dl, low dose insulinization procedure was undertaken21. A priming insulin infusion was given for initial 10 minutes, followed by a constant infusion for the next 110 minutes at the rate of 40 mU/m2 to achieve plasma insulin concentration of 100 µU/ml. At the 4th minute, glucose infusion (25% dextrose) was started intravenously via infusion pump, with rate set at 2.0 mg/kg/min up to 10th min. subsequent infusion rate was adjusted depending on the arterialized plasma glucose values obtained every 5 minutes with aim of maintaining plasma glucose concentration at an average value of 90 mg/dl for next 110 min. The blood samples for glucose measurements were drawn into ethylene diamine tetra acetate (EDTA) tubes and the separated plasma was analyzed by the glucose oxidase method on a bedside glucose analyzer (GM9D, Analox instruments, London, UK). For insulin levels measurement, sample was collected every 20 min in heparinized tubes and plasma stored at −80 °C until analysis, which was done by ECLIA (Elecsys 2010, Roche Diagnostics, GmbH, Mannheim, Germany). Glucose disposal rate and insulin sensitivity (SI) were calculated over 40 to 120 min of the clamp. Mean steady state plasma glucose values, glucose infusion rates and insulin values were obtained during the study.
Glucose infusion rate = glucose disposal rate (M)
Insulin sensitivity index (SIclamp): = M/(G × ΔI) where M is glucose disposal rate and ΔI is the difference between fasting and steady-state plasma insulin concentrations22.
HOMA-IR = [fasting plasma insulin (μU/ml) × fasting plasma glucose (mmol/L)]/22.523,24
HOMA-β = 20 × fasting plasma insulin (μU/ml)/[fasting plasma glucose (mmol/L)−3.5]23
QUICKI = 1/[log(fasting insulin in μU/ml) + log(fasting glucose in mmol/L)]25.
End points
Primary end point was the change in insulin sensitivity (SIclamp) and glucose metabolism (M) by hyperinsulinemic-euglycemic clamp and HOMA-β at 4 months with saroglitazar as compared to placebo. Secondary end points included change in body weight, fasting plasma glucose, post-prandial plasma glucose, HbA1c, fasting lipid profile, insulin and C peptide levels.
Statistical analysis
Data obtained was analysed using Statistical Package of Social Sciences (SPSS) version 20. (Armonk, NY: IBM Corp). Results obtained were expressed as mean value ± 2 standard deviation (parametric data) or as median value and IQR (non-parametric data). Data was analysed using intention to treat26 analysis. Missing data was handled with last observation carried forward (LOCF). Student’s t-test (parametric data), Mann Whitney U test (non-parametric data) and Wilcoxon signed rank test (non-parametric data) were used for comparisons between saroglitazar and placebo groups. Correlation analysis was carried out using Pearson’s correlation and Spearman’s rho as appropriate. Analysis of covariance (ANCOVA) was used to study the effect of treatment on between group differences with treatment given (placebo or saroglitazar) as fixed factor, change in parameter as dependent variable and baseline value of the parameter being assessed as covariate.
Ethics approval and consent to participate
The study was performed according to the declaration of Helsinki and was approved by the Institutional Ethics Committee of Postgraduate Institute of Medical Education and Research, Chandigarh, India. Written informed consent was obtained from all the patients to participate in the study.
Results
Demographic characteristics
A total of 61 patients were screened from January, 2017 till June, 2018. Among them 30 had fulfilled the inclusion criteria and were recruited in the study (Fig. 1). Five patients were lost to follow up as they withdrew the consent (3 placebo, 2 saroglitazar), all within the first month of inclusion. The mean age of participants was 44 ± 9.5 years (27 men). The median duration of diabetes in saroglitazar group was 3 months (1–12 months) and in placebo group was 2 months (1–6 months). The mean weight, BMI, waist circumference and percentage body fat were comparable between the two groups (Table 1).The dose of glimepiride at the completion of the study was comparable in either group (2 mg).
Baseline metabolic parameters
Saroglitazar arm had significantly higher serum triglycerides (p = 0.019) and lower HDL-C levels (p = 0.026) as compared to the placebo arm (Table 1), whereas total cholesterol, low density lipoproteins (LDL-C) and apolipoprotein B were comparable in both the groups at baseline. The two groups had similar levels of hsCRP, fasting and post prandial plasma glucose, HbA1c, fasting plasma C-peptide and fasting plasma insulin. Hyperinsulinemic euglycemic clamp study revealed that the groups were similar with respect to glucose metabolism (M) and insulin sensitivity (SI clamp) as well as HOMA-IR, log HOMA, HOMA-β and 1/HOMA. (Table 2).
Study end points
Primary end points
After 4 months of the study period, saroglitazar improved glucose metabolism (M) (P = 0.025) and SIclamp(p = 0.011) significantly, as compared to the baseline levels (Fig. 2).Further, SI clamp improved to a greater extent in saroglitazar group as compared to placebo group {2.9 (1.33–6.64) to 6.1 (2.09–20.03) vs 2.3 (1.42–4.47) to 3.0 (2.1–3.8), p = 0.026, all values in [100 × (mg/kg) per μU/ml]}. The effect of saroglitazar on SIclamp at 4 months persisted despite controlling for baseline weight, TG, HDL-C and HbA1c (partial η 2 = 0.342, p = 0.002). However, change in SIclamp did not correlate with change in TG (r = −0.198, p = 0.479) and HbA1c levels (r = −0.415. p = 0.124). HOMA- β increased significantly (p = 0.01) in the saroglitazar group as compared to placebo and inversely correlated with change in fasting plasma glucose (r = 0.749, p = 0.001). However, change in HOMA-β did not significantly correlate with changes in TG (r = −0.098, p = 0.729) and HbA1c levels (r = −0.488, p = 0.065). Nonetheless, change in HOMA-β showed a trend towards significance with SIclamp (r = 0.503, p = 0.056).
Secondary end points
Patients in saroglitazar arm had a greater improvement in HbA1c (−1.34 ± 1 versus −0.5 ± 0.7 mg/dl, p = 0.019) and fasting plasma glucose (p = 0.019) as compared to placebo. Saroglitazar also resulted in higher fall in TG levels (p = 0.001) and the significant rise in HDL-C levels (p < 0.01) even after correcting for baseline inequalities (Fig. 2). Further, changes in fasting plasma insulin (p = 0.624), C-peptide (p = 0.234), body weight (p = 0.782),HOMA-IR (p = 0.081), log HOMA (p = 0.208), 1/HOMA (p = 0.302) and QUICKI (p = 0.232) were not significantly different between the two groups (Table 2).
Safety profile
No episodes of hypoglycemia, were noted during the clamp studies. No adverse effects including myalgias, peripheral edema, weight gain, hypoglycemia, transaminitis and renal dysfunction were noted in either group during the study period.
Discussion
This is the first study to evaluate the effects of saroglitazar, a dual PPAR-α/γ agonist, on insulin sensitivity by hyperinsulinemic euglycemic clamp in patients of T2DM with hypertriglyceridemia. Our study showed that saroglitazar treatment resulted in significant reduction in triglycerides, fasting plasma glucose and HbA1c along with increase in HDL-C levels. Further, a significant improvement in whole body insulin sensitivity was observed in the saroglitazar group as compared to placebo. This was accompanied with increase in HOMA-β and a change in HOMA-β showed a trend towards significance with improvement in insulin sensitivity. However, improvement in insulin sensitivity and β-cell function did not correlate either with decrease in HbA1c or with decline in triglycerides.
Insulin resistance is the key abnormality in the pathophysiology of T2DM accompanied with progressive decline in β-cell function, resulting in emergence of hyperglycemia27. Various modalities have been employed to estimate the insulin resistance including HOMA-IR,QUICKI and Matsuda index; however, the ‘gold standard’ remains the hyperinsulinemic-euglycemic clamp28. HOMA-IR measurement is useful in healthy and prediabetes individuals as well for epidemiological studies; however, with the emergence of hyperglycemia and failing β-cell function, its value may be limited. Similarly, QUICKI and Matsuda index are also contained in their usefulness with declining β-cell function29. Therefore, hyperinsulinemic-euglycemic clamp remains the procedure of choice to assess the whole body insulin sensitivity in patients with T2DM. Hence, we planned to use clamp studies for the assessment of insulin sensitivity in our study patients.
The strategies to target insulin resistance in patients with T2DM include life-style modification, metformin and thiazoledinediones30. The latter drug prototype include pioglitazone, which is a selective PPAR-γ agonist and improves insulin sensitivity by augmenting insulin signalling at insulin-target sites, and further by reducing lipotoxicity and proinflammatory adipocytokine, tumor necrosis factor-ά (TNF-ά), promote insulin action31.Lipotoxicity is one of the pivotal mechanism implicated in mediation of insulin resistance at insulin target sites as well as β-cell dysfunction. The key metabolites for inducing insulin resistance through lipotoxicity include non-esterified fatty acids and triglycerides. Impaired triglycerides metabolism in the liver and muscle in diabetes results in further production of various noxious metabolites such as fatty acyl conenzyme A, ceramides and diacylglycerol. Lipotoxicity may be attenuated with the use of PPAR-ά agonist, which by reducing triglycerides may attribute to improvement in insulin sensitivity32. Fenofibrate, a PPAR-ά agonist is widely used drug in the management of hypertriglyceridemia that effectively reduces serum triglycerides levels and modestly improves insulin sensitivity33. Saroglitazar, a predominant PPAR-α and moderate γ-agonist, is recently approved drug for the management of diabetic dyslipidemia and has been demonstrated to decrease triglycerides and improves HbA1c34; however, its effect on insulin sensitivity remains unexplored. In our study, saroglitazar significantly improved insulin sensitivity accompanied with significant decrease in HbA1c and TG levels, major attributes to reduction in gluco-lipotoxicity. Further, the effect on SIclamp persisted despite adjusting for weight, HbA1c, TG and HDL-C. However, change in insulin sensitivity in subjects receiving saroglitazar did not correlate significantly with changes in TG and HbA1c levels. Therefore, it is conceivable that beside reduction in gluco-lipotoxicity, it also exerts its additional moderate effect directly through PPAR-γ receptors that stimulates the transcription of several insulin-responsive genes, thereby, further contributing towards the improvement in insulin sensitivity. Alternatively, a small sample size and short duration of the study may have precluded its (saroglitazar) mediation of its beneficial effects through gluco-lipotoxicity alone.
Saroglitazar administration resulted in a significant reduction in FPG and HbA1c as compared to placebo. However, it was not accompanied with increase in fasting plasma insulin and C-peptide indicating that improvement in glycemic profile was possibly contributed by enhanced insulin sensitivity. Further, a significant decrease in FPG itself denotes improved hepatic insulin sensitivity as PPAR-α are predominantly expressed in liver, a major target site for saroglitazar. A significant change in HOMA-β was observed in the saroglitazar group which also showed a trend towards significance to SIclamp again indicating that improvement in β-cell function was a consequence of improved insulin sensitivity.
However, a modest direct effect of saroglitazar through PPAR-γ and α-agonist activity on β-cells cannot be excluded, as both these receptors are abundantly expressed on β-cells35. In addition, both the groups were well matched with respect to the median glimepiride dose, hence it seems plausible that the measured difference in HbA1c and FPG is likely ascribable to the effect of saroglitazar itself. While previous trials with saroglitazar36 and aleglitazar noted improvement in glycemic parameters, muraglitazar failed to cause a significant change in HbA1c26. This differential effect could be due to the variance in relative affinities of these drugs for PPAR-α and PPAR-γ receptors as well as differences in molecular weight and structure37,38.
In our study, both the groups had matched total cholesterol, LDL-C and apoB levels at baseline. However, baseline serum TG levels were higher and serum HDL-C levels were lower in patients receiving saroglitazar as compared to those randomized to placebo. The difference in baseline triglyceride existed despite randomization and blinding as the patients were not stratified as per triglyceride or HDL-C levels. Saroglitazar significantly lowered triglycerides and raised HDL-C levels as compared to placebo even after adjusting for the baseline differences. A similar effect on triglyceride and HDL-C levels with negligible effects on LDL-C levels has also been shown with muraglitazar26 and aleglitazar39, previously. We did not find lowering of LDL-C, apoB and total cholesterol unlike PRESSV, where significant lowering of above parameters were noted with saroglitazar. This discrepancy may be due to a relatively small sample size of our study whereby changes of smaller magnitude may not be easily apparent.
No significant effect of saroglitazar was noted on different anthropometric parameters, including body weight, BMI, waist circumference or body fat%., as measured by DEXA. Similar findings were also noted in PRESS V and PRESS VI36. Interestingly, studies with aleglitazar and muraglitazar had shown an increase in body weight along with an increase in fat mass26,39 inspite of similar study duration indicating that these may be a drug-specific effect rather than class action.
No adverse effects accountable to saroglitazar use were observed nor were any episodes of symptomatic hypoglycemia reported during the clamp study. The plasma glucose was analysed at 5 minutes interval during the clamp procedure to ensure the rapid correction of hypoglycemia, if noted. This is in accordance with the findings of PRESS V and PRESS VI trials wherein no serious adverse events were reported with saroglitazar36.
Our study has a number of strengths. As a pilot study, it was able to demonstrate a clinically and statistically significant improvement in insulin sensitivity as well as HbA1c. The groups were well matched with respect to most metabolic and laboratory parameters. Most patients (25/30, 83.3%) were able to complete the study with no adverse events. Our study had a few limitations. Owing to the invasive and time consuming nature of hyperinsulinemic euglycemic clamp, we recruited a small number of patients. Also, the absence of an active comparator limits the generalizability of the results. Further, we could not explore into mechanistic insights regarding improvement of insulin sensitivity with saroglitazar by estimating non-estified fatty acids and TNF-ά. Expectedly, our results will act as a harbinger for larger trials which can overcome these limitations.
Conclusion
We conclude that saroglitazar effectively reduces hypertriglyceridemia and improves insulin sensitivity along with β-cell function by reduction in gluco-lipotoxicity and possibly directly through PPAR-γ agonism in patients ofT2DM with hypertriglyceridemia.
Data availability
The datasets supporting the conclusions of this work are included in the article.On reasonable request, the content can be available from the corresponding author.
References
Ridker, P. M. et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 359, 2195–2207 (2008).
Musunuru, K. Atherogenic dyslipidemia: cardiovascular risk and dietary intervention. Lipids 45, 907–914 (2010).
Schofield, J. D., Liu, Y., Rao-Balakrishna, P., Malik, R. A. & Soran, H. Diabetes Dyslipidemia. Diabetes Ther 7, 203–219 (2016).
Shetty, S. R., Kumar, S., Mathur, R. P., Sharma, K. H. & Jaiswal, A. D. Observational study to evaluate the safety and efficacy of saroglitazar in Indian diabetic dyslipidemia patients. Indian heart journal 67, 23–26 (2015).
Boden, W. e. et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med 365, 2255–2267 (2011).
Landray, M. j. et al. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med 371, 203–212 (2014).
Sarwar, N. et al. Triglyceride-mediated pathways and coronary disease: collaborative analysis of 101 studies. Lancet 375, 1634–1639 (2010).
Austin, M. A., Hokanson, J. E. & Edwards, K. L. Hypertriglyceridemia as a cardiovascular risk factor. The American journal of cardiology 81, 7b–12b (1998).
Scherer, D. J. & Nicholls, S. J. Lowering triglycerides to modify cardiovascular risk: will icosapent deliver? Vasc Health Risk Manag 11, 203–209 (2015).
Sacks, F. M. et al. Association between plasma triglycerides and high-density lipoprotein cholesterol and microvascular kidney disease and retinopathy in type 2 diabetes mellitus: a global case-control study in 13 countries. Circulation 129, 999–1008 (2014).
Keech, A. et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet 366, 1849–1861 (2005).
Ginsberg, H. n. et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med 362, 1563–1574 (2010).
Henke, B. R. et al. N-(2-Benzoylphenyl)-L-tyrosine PPARgamma agonists. 1. Discovery of a novel series of potent antihyperglycemic and antihyperlipidemic agents. J Med Chem 41, 5020–5036 (1998).
Egerod, F. L. et al. Biomarkers for early effects of carcinogenic dual-acting PPAR agonists in rat urinary bladder urothelium in vivo. Biomarkers 10, 295–309 (2005).
Kendall, D. M. et al. Improvement of glycemic control, triglycerides, and HDL cholesterol levels with muraglitazar, a dual (alpha/gamma) peroxisome proliferator-activated receptor activator, in patients with type 2 diabetes inadequately controlled with metformin monotherapy: A double-blind, randomized, pioglitazone-comparative study. Diabetes Care 29, 1016–1023 (2006).
Ghosh, A., Sahana, P. K., Das, C., Mandal, A. & Sengupta, N. Comparison of Effectiveness and Safety of Add-on Therapy of Saroglitazar and Fenofibrate with Metformin in Indian Patients with Diabetic Dyslipidaemia. Journal of clinical and diagnostic research: JCDR 10, Fc01–04 (2016).
Anjana, R. M. et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia 54, 3022–3027 (2011).
Whitlock, E. P., Polen, M. R., Green, C. A., Orleans, T. & Klein, J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 140, 557–568 (2004).
Bantle, J. P. et al. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care 31(Suppl 1), S61–78 (2008).
DeFronzo, R. A., Tobin, J. D. & Andres, R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. The American journal of physiology 237, E214–223 (1979).
Hawkins, M. et al. Glycemic control determines hepatic and peripheral glucose effectiveness in type 2 diabetic subjects. Diabetes 51, 2179–2189 (2002).
Muniyappa, R., Madan, R. & Quon, M. J. Assessing Insulin Sensitivity and Resistance in Humans. https://www.ncbi.nlm.nih.gov/books/NBK278954 (2000).
Wallace, T. M., Levy, J. C. & Matthews, D. R. Use and abuse of HOMA modeling. Diabetes Care 27, 1487–1495 (2004).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
Katz, A. et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 85, 2402–2410 (2000).
Fernandez, M. et al. Metabolic effects of muraglitazar in type 2 diabetic subjects. Diabetes Obes Metab 13, 893–902 (2011).
Scheen, A. J. Pathophysiology of type 2 diabetes. Acta clinica Belgica 58, 335–341 (2003).
Monzillo, L. U. & Hamdy, O. Evaluation of insulin sensitivity in clinical practice and in research settings. Nutrition reviews 61, 397–412 (2003).
Thompson, D. S. et al. Limitations of fasting indices in the measurement of insulin sensitivity in Afro-Caribbean adults. BMC research notes 7, 98 (2014).
8. Pharmacologic Approaches to Glycemic Treatment. Standards of Medical Care in Diabetes-2018. Diabetes Care 41, S73–S85 (2018).
Gupta, P. et al. Efficacy and risk profile of anti-diabetic therapies: Conventional vs traditional drugs-A mechanistic revisit to understand their mode of action. Pharmacological research 113, 636–674 (2016).
Lalloyer, F. et al. Peroxisome proliferator-activated receptor alpha improves pancreatic adaptation to insulin resistance in obese mice and reduces lipotoxicity in human islets. Diabetes 55, 1605–1613 (2006).
Wysocki, J. et al. Effects of micronized fenofibrate on insulin resistance in patients with metabolic syndrome. International journal of clinical pharmacology and therapeutics 42, 212–217 (2004).
Chatterjee, S., Majumder, A. & Ray, S. Observational study of effects of Saroglitazar on glycaemic and lipid parameters on Indian patients with type 2 diabetes. Sci Rep 5, 7706 (2015).
Kim, H. I. & Ahn, Y. H. Role of peroxisome proliferator-activated receptor-gamma in the glucose-sensing apparatus of liver and beta-cells. Diabetes 53(Suppl 1), S60–65 (2004).
Pai, V. et al. A Multicenter, Prospective, Randomized, Double-blind Study to Evaluate the Safety and Efficacy of Saroglitazar 2 and 4 mg Compared to Pioglitazone 45 mg in Diabetic Dyslipidemia (PRESS V). Journal of diabetes science and technology 8, 132–141 (2014).
Wright, M. B., Bortolini, M., Tadayyon, M. & Bopst, M. Minireview: Challenges and opportunities in development of PPAR agonists. Mol Endocrinol 28, 1756–1768 (2014).
Salomone, S. Pleiotropic effects of glitazones: a double edge sword? Front Pharmacol 2, 14 (2011).
Stirban, A. O. et al. Aleglitazar, a dual peroxisome proliferator-activated receptor-alpha/gamma agonist, improves insulin sensitivity, glucose control and lipid levels in people with type 2 diabetes: findings from a randomized, double-blind trial. Diabetes Obes Metab 18, 711–715 (2016).
Acknowledgements
We would like to thank Zydus Cadila Healthcare for providing drug and placebo. We would also like to thank Dr Shipra Bhansali for her help in statistical analysis and editing the manuscript.
Author information
Authors and Affiliations
Contributions
Conceived and designed: A.B., N.J. Administrative support- A.B., A.R. Guidance for conducting the clamp and insulin secretion model: A.V.K., M.H. Patient’s recruitment-N.J., A.B., A.R. Collection and/or assembly of data- N.J., S.B., S.K. Data analysis and interpretation- N.J., A.S., A.B. Manuscript writing- N.J., A.B. All authors read and approved the final manuscript
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jain, N., Bhansali, S., Kurpad, A.V. et al. Effect of a Dual PPAR α/γ agonist on Insulin Sensitivity in Patients of Type 2 Diabetes with Hypertriglyceridemia- Randomized double-blind placebo-controlled trial. Sci Rep 9, 19017 (2019). https://doi.org/10.1038/s41598-019-55466-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-55466-3
This article is cited by
-
Flavonoid compound from Agrimonia pilosa Ledeb improves adipose insulin resistance by alleviating oxidative stress and inflammation
BMC Complementary Medicine and Therapies (2023)
-
Efficacy and Safety of Saroglitazar in Patients with Cardiometabolic Diseases: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Clinical Drug Investigation (2022)
-
Differential expression of gluconeogenic enzymes in early- and late-stage diabetes: the effect of Citrullus colocynthis (L.) Schrad. Seed extract on hyperglycemia and hyperlipidemia in Wistar-Albino rats model
Clinical Phytoscience (2021)
-
Emerging therapeutic approaches for the treatment of NAFLD and type 2 diabetes mellitus
Nature Reviews Endocrinology (2021)
-
Triglyceride is independently correlated with insulin resistance and islet beta cell function: a study in population with different glucose and lipid metabolism states
Lipids in Health and Disease (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.