Abstract
Background/Aims
A prospective study identified three patients between 2004 and 2010 with mesectodermal leiomyoma. The study was conducted to analyse the presence or absence of sex steroid hormone receptors in mesectodermal leiomyomas.
Methods
The clinical features were collated. All three patients had operative procedures to either remove or sample the mesectodermal leiomyomas. The tissue was fixed in formalin and exposed to conventional histological processing. Immunohistochemistry using antibodies to androgen (AR), oestrogen (ER), and progesterone (PR) receptors was performed, followed by stain scoring to assess for expression status.
Results
All three cases were confirmed by histology to be examples of mesectodermal leiomyomas. All three expressed sex steroid hormone receptors. One case expressed both PR and AR, one case PR only and another case AR only. None of the cases expressed ER receptors.
Conclusion
All three cases displayed some sex steroid hormone receptor expression. This is supportive evidence that sex steroid hormones may have a role in the pathogenesis of this tumour and suggest that it may be amenable to hormonal manipulation therapy, in a manner similar to conventional uterine leiomyomas.
Similar content being viewed by others
Introduction
Intraocular leiomyomas are rare benign smooth-muscle tumours of the uveal tract.1, 2, 3 In contrast to ocular melanoma, patients with leiomyoma are on average younger and more commonly female.2 This raises the possibility of hormonal influence on these tumours,2 and the potential for hormone manipulation therapy. Surgical excision is currently the only available treatment option. We present three consecutive prospective cases of mesectodermal leiomyoma, all of which were immunohistochemically positive for steroid hormone receptors.
Methods
All studies were conducted in accordance with the Declaration of Helsinki. All patients with a histopathological diagnosis of intraocular leiomyoma were prospectively included in the study. Specimens were fixed in standard 10% buffered formalin, processed to paraffin wax, and sections were cut and stained with haematoxylin and eosin. All cases were exposed to immunohistochemistry, with antibodies to smooth-muscle actin and desmin (both 1 : 75 dilution; Dako UK Ltd, Ely, UK), Melan A (1 : 20 dilution; Leica Biosystems, Newcastle, UK), progesterone receptor (PR, 1 : 50 dilution; Vector Labs, Peterborough, UK), oestrogen (ER) receptor, and androgen (AR) receptor (both 1 : 50 dilution; Leica Biosystems). The degree of hormonal receptor positivity was assessed using the scoring system of Leitao et al.4 Briefly, a 0–3 scale was used to score the slides (score 0: no staining; score 1: 5% of the cells staining or diffuse staining difficult to separate from background; score 2: 6–50% of the cells staining; and score 3: greater than 50% of the cells staining). The scoring was done by one observer (HSM). A result was classed as negative for score 0–1 and positive for score 2–3.4
Case reports
Case 1
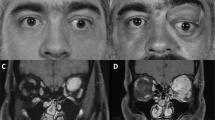
A 60-year-old post-menopausal woman presented with 2 years of intermittent blurring of the right eye. A lesion which was clinically suspicious of a peripheral inferotemporal ciliochoroidal malignant melanoma of the right eye was detected, and she underwent an enucleation (Figures 1a and b).
(a) Fundus photograph showing the dome-shaped lesion emanating from the ciliary body in case 1, with the apex showing features suspicious of a collar-stud. (b) The B-scan ultrasound of the lesion for case 1. (c) The B-scan ultrasound showing a mass in the supraciliary space for case 2. (d) Post-biopsy B-scan ultrasound of case 2, showing the reduction in size of the lesion.
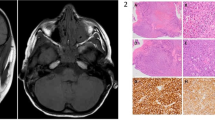
Macroscopy showed a white-to-cream ovoid mass, 10 mm in maximum diameter, in the supraciliary space (Figure 2a black arrow). Microscopically, it showed intersecting eosinophilic spindle cells, with para-nuclear vacuoles (Figure 2b). It was positive for smooth-muscle actin (Figure 2c) and desmin (Figure 2d), and negative for Melan A (not shown). The features were of benign mesectodermal leiomyoma. Transmission electron microscopy showed cytoplasmic filaments with fusiform densities, confirming a smooth-muscle phenotype (Figure 2e). Steroid hormone receptor immunohistochemical staining revealed nuclear positivity for progesterone (Figure 2f) and AR receptors (Figure 2g). ER receptors were not expressed (not shown).
(a) Macroscopic intraocular appearance of mesectodermal leiomyoma during histopathology macroscopic documentation in case 1. Note how the solid white lesion lies between the sclera and the elevated choroid (brown pigmented layer over lesion). (b) Haematoxylin- and eosin-stained section of case 1, showing spindle cells with para-nuclear vacuoles (black arrow). (c) Smooth-muscle actin immunopositivity of case 1 (brown is positive). (d) Desmin immunopositivity of case 1. (e) Transmission electron microscopy of case 1 showing focal cytoplasmic actin densities (arrow). (f) Nuclei expressing progesterone receptor (brown immunopositivity) in case 1. (g) Nuclei expressing androgen receptor (brown immunopositivity) in case 1. (h) Nuclei expressing progesterone receptor (brown immunopositivity) in case 2. (i) Nuclei expressing androgen receptor (brown immunopositivity) in case 3.
Case 2
A 66-year-old post-menopausal woman was referred for routine cataract surgery. She had an incidental finding of a temporal ciliary body lesion in the left eye, well circumscribed on B-scan ultrasound assessment, and its location in the supraciliary region raised the possibility of intraocular leiomyoma (Figure 1c). She underwent open flap biopsy (Figure 1d). Histopathology and immunohistochemistry showed a mesectodermal leiomyoma, with positivity for progesterone receptor (Figure 2h), but negative for both AR and ER receptors (not shown).
The residual lesion has not increased in size and she is doing well following phacoemulsification surgery.
Case 3
A 55-year-old man, initially referral as a glaucoma suspect, was found to have an abnormal amelanotic right temporal iris root. The differential diagnosis was of amelanotic melanoma or leiomyoma. Right eye iridocyclectomy was performed, and the histology and immunohistochemistry were those of mesectodermal leiomyoma with positivity for AR receptor (Figure 2i), but negative for both progesterone and ER receptor (not shown).
The clinical, histopathological, and follow-up data are summarised in Table 1.
Discussion
All our cases of mesectodermal leiomyoma were positive for sex steroid hormone receptors (except ER receptor), potentially implicating hormonal manipulation therapy to shrink large symptomatic leiomyomas medically and avoiding surgery.
In the second case presented, with residual intraocular tumour, we approached the local gynaecology team for advice on potential systemic hormone antagonist use. The view was that there was no role for hormonal manipulation because she was post-menopausal, and therefore endogenous hormone levels were already diminished. We have not challenged this as the patient is currently completely asymptomatic from her residual intraocular leiomyoma.
It is interesting to note that the male patient mesectodermal leiomyoma expressed AR receptor only, whereas those cases from the two female patients expressed progesterone receptors. This may reflect slightly different hormonal pathogenesis profiles in the two sexes, although uterine leiomyomas are known to express AR receptor.4 It is interesting to note that not all the tumour cells in the three cases expressed progesterone or AR receptors. This heterogeneity may reflect the fact that mesectodermal leiomyomas are of neural crest origin, whereas uterine leiomyomas are of mesenchymal origin.

References
Blodi FC . Leiomyoma of the ciliary body. Am J Ophthalmol 1950; 33: 939–942.
Shields JA, Shields CL, Eagle RC, De Potter P . Observations on seven cases of intraocular leiomyoma. The 1993 Byron Demorest Lecture. Arch Ophthalmol 1994; 112: 521–528.
Jakobiec FA, Font RL, Tso MO, Zimmerman LE . Mesectodermal leiomyoma of the ciliary body: a tumour of presumed neural crest origin. Cancer 1977; 39: 2102–2113.
Leitao MM, Soslow RA, Nonaka D, Olshen AB, Aghajanian C, Sabbatini P et al. Tissue microarray immunohistochemical expression of estrogen, progesterone, and androgen receptors in uterine leiomyomata and leiomyosarcoma. Cancer 2004; 101 (6): 1455–1462.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author Contributions
Dr Hibba Quhill is the main author of the paper. Dr HS Mudhar collated data and wrote the histopathology component. Professor Rennie and Paul Rundle edited the paper and contributed intellectual input.
Rights and permissions
About this article
Cite this article
Quhill, H., Rennie, I., Rundle, P. et al. Three cases of intraocular mesectodermal leiomyoma expressing progesterone and androgen receptors. Eye 27, 669–672 (2013). https://doi.org/10.1038/eye.2013.37
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.37