Abstract
Objective
To describe a series of paediatric orbital lymphoma patients in a single tertiary referral centre.
Methods
A retrospective case-note search in the Oxford Eye Hospital of all patients under the age of 18 years with orbital lymphoma between 2010 and 2020. Demographic and clinical data were obtained, and a literature review was conducted.
Results
Five patients were identified with orbital lymphoma, mean age 48.2 ± 36 months (1–109 months), three were males. Clinical presentation included: ptosis, proptosis, lethargy, visual loss, and strabismus. Two patients had bilateral orbital disease and one patient was diagnosed within the first month of life. The tissue diagnosis revealed four cases of Burkitt’s lymphoma and one case of T- lymphoblastic lymphoma. Central nervous system (CNS) sampling was also positive in the four cases of Burkitt’s lymphoma. All patients were treated systemically for the lymphoma with chemotherapy. Complete remission was achieved in all cases post chemotherapy. Follow-up of 36.4 ± 18.9 months (10–61 months).
Conclusion
This is the largest published case series of paediatric orbital lymphoma. We described a patient diagnosed within the first month of life and we believe this to have developed intra-uterine. In this series, patients were younger, had more bilateral disease and had better outcome than previously described. This rare condition should be considered in any child with an orbital mass, at any age. When managed appropriately, good outcomes can be achieved.
Similar content being viewed by others
Introduction
Lymphoma is a malignant neoplasm of lymphocytes which is most commonly seen within the lymph nodes and the spleen [1]. Non-Hodgkins Lymphoma (NHL) is the most common orbital malignancy in adults and accounts for around 10% of extra-nodal lymphoma and for 1% of all lymphomas [2, 3]. Orbital lymphoma can arise from the conjunctiva, eyelid, lacrimal gland and sac and orbit including the extra-ocular muscles [4, 5], and have a varied presentation including eyelid swelling, ptosis, proptosis, diplopia and more [6].
Paediatric orbital lymphoma, however, is rare and described previously in only 15 case reports, with only one case series of three patients published to date. We present a case series of paediatric biopsy-proven orbital lymphoma seen at a single institution.
Methods
A retrospective case-note search was conducted for all patients under the age of 18 years of age, with a biopsy proven orbital lymphoma treated in the Oxford Eye Hospital between 2010 and 2020. Data was collected from patient notes and included demographic data, clinical presentation, radiological findings, histopathology, medical and surgical management, follow-up course and clinical outcomes. A literature review was also performed for all cases of paediatric orbital lymphoma of all sub-types and is summarized. Due to the nature of a retrospective review and the lack of identifiable features, ethical approval was not necessary and not obtained.
Results
Five paediatric patients were diagnosed with orbital lymphoma in our institution between the years 2010–2020. The main demographic and clinical data is summarized in Table 1.
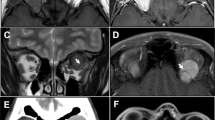
Case 1: A 62-month-old male patient with parental complaints of decreased visual acuity. Examination revealed visual acuity of 1.0 LogMAR in conjunction with a left convergent squint and bilateral 6th nerve palsy. MRI revealed an enhancing lesion involving the central sphenoid and posterior ethmoid sinuses, with erosion of the orbital apices, anterior cranial fossa, pituitary fossa and left cavernous sinus. This resulted in compression of the intracranial section of the optic nerves (Fig. 1(1)). A tissue diagnosis of high grade Burkitt’s lymphoma (Fig. 1(2)) with CNS involvement was made and treatment with chemotherapy was initiated. The patient underwent bilateral optic nerve decompression at the time of the biopsy and was given glasses and occlusion therapy to prevent amblyopia. At 34 months follow-up there was a residual 6th nerve palsy bilaterally. The visual acuity improved to 0.1 LogMAR.
1 Coronal and sagittal MRI sections of patient 1 showing enhancing lesion in the central sphenoid sinus and posterior ethmoid sinus with erosion of the orbital apices, anterior cranial fossa, pituitary fossa and left cavernous sinus. Compression of optic nerves (intracranial component) is noted bilaterally. 2 Histology from patient 2 shows fragments of sino-nasal mucosa and bone extensively infiltrated by rather monotonous, cellular dense sheets of medium-sized lymphoid cells with brisk mitotic activity. Marked tumour cell apoptosis is seen with scattered macrophages (arrows) to engulf the cellular debris. H&E stain (original magnification: A x10; B, C and E x100; D x20; F x300). The neoplastic cells are immunopositive for CD20 (G; original magnification x100) and CD79a (H; original magnification x100). The proliferation (MIB-1) index is high at ~95% (I; original magnification x100).
Case 2: A 33-month-old male patient, with parental complaints of lethargy and headaches. Examination revealed a left esotropia, proptosis and left sided visual acuity of nil perception of light (NPL). MRI outlined skull base disease centred on the left sphenoid bone with intracranial extension and multiple bilateral renal deposits. A tissue diagnosis of Burkitt’s lymphoma was made with CNS involvement. The patient was treated with chemotherapy and squint surgery to repair the esotropia. At 61 months of follow-up there was complete remission for the last 48 months though the visual acuity on the left remained NPL.
Case 3: A 109-month-old female patient with a right scapular mass. MRI showed multiple bony lesions with involvement of the right orbital floor. (Fig. 2(1)) Examination revealed a right orbital floor mass with full ocular motility and visual acuity of 0.7 LogMAR. A biopsy confirmed T-cell lymphoma without CNS involvement. She was treated with chemotherapy and was given refractive correction for the right eye. After 54 months of follow-up there was complete remission of the tumour with a visual acuity of 0.1 LogMAR.
1 Coronal MRI section with gadolinium showing a soft tissue mass centred on the right anterior lateral maxillary bone. This extends from the marrow through into the malar soft tissues, the submucosal plane of the sinus, the extraconal space of the orbit and to a lesser extent the infratemporal fossa, without destruction of the cortical bone. 2 Coronal and transverse MRI sections showing a large mass lesion of the central skull base. The lesion appears to be centred on the body of the sphenoid bone. Anteriorly, the lesion extends into the posterior ethmoid air cells and up to the posterosuperior aspect of the nasal septum. The tumour extends into the orbital apex on the left where it comes into contact with the medial aspect of the medial rectus muscle and causes some crowding at the orbital apex. The tumour extends into the left pterygopalatine fissure and inferior orbital fissure.
Case 4: A 36-month-old male patient presented with a left ptosis and a squint. Examination confirmed left-sided visual acuity of perception of light (PL), an upper eyelid ptosis with 3rd and 6th cranial nerve palsies. MRI confirmed a large mass centred on the body of the sphenoid bone with extensive central skull base involvement and extension into left cavernous sinus, orbital apex, pterygopalatine fissure with extradural extension to both the anterior and middle cranial fossae. (Fig. 2 (2)) Tissue diagnosis confirmed Burkitt’s lymphoma with CNS involvement. The patient was managed with chemotherapy resulting with a vision of 1.0 LogMAR, normal ocular movements and marked reduction in tumour size after a 23-month follow-up.
Case 5: A 1 month-old female presented with bilateral proptosis, more on the left and a visible mass on the lateral aspect of the left orbit with a further mass seen in the right temporoparietal region. The visual acuity could not be assessed due to her age. There was a left-sided lagophthalmos. MRI showed extensive infiltration on the lateral aspect of the left orbit with bone destruction and soft tissue extension to the left side of the face. There was also right orbital mass and right parietal involvement with intracranial (extradural) involvement. (Fig. 3) Bone marrow was also involved. Tissue sampling confirmed Burkitt’s lymphoma. The child was managed with chemotherapy and lubricants for the left lagophthalmos and exposure keratopathy. After six months of treatment no proptosis or orbital disease. By 10 months there was a marked reduction in size of the second mass involving the temporo-parietal on MRI.
Coronal and transverse MRI sections showing the presence of an intraorbital mass lesion on the left with mild proptosis and a small extra orbital component. No bony changes. There is evidence of an extensive aggressive disease process involving bone marrow, extracranial soft tissue particularly within both orbits where there is now bilateral marked proptosis; and intracranially. The disease process, severally destroyed bones as the lateral wall of the left orbit, and the right parietal bone and others show evidence of “lytic/destructive” changes within them.
Literature review
Eighteen cases of paediatric orbital lymphoma are previously described in the medical literature and summarized in Table 2 [1, 5,6,7,8,9,10,11,12,13,14,15,16,17,18,19]. Gupta et al. published three cases [7] and the remaining publications are single case reports. The overall mean reported age was 73.3 ± 18.3 months (18–156), 12 were males (67%) and 11 had primary disease (61%). Five patients (28%) had T-cell lymphoma, 6 patients (33%) had Burkitt lymphoma, and 7 patients (39%) had other non-Hodgkin’s lymphoma. Unilateral disease was diagnosed in 89% of cases. One patient received palliative treatment and all other patients were managed with chemotherapy. Seven patients received adjuvant radiotherapy (39%). Mean follow-up was 24.9 ± 35.7 months (1–156). In two patients the disease was controlled, five patients died, and ten patients had complete remission. Three patients had a relapse during the follow-up period, but all were successfully treated and reached full remission of the disease.
Discussion
We present, to our knowledge, the largest case series of orbital lymphoma in the paediatric population. This series further describes a patient diagnosed within the first month of life. Due to the extensive nature of the disease on presentation we believe the lymphoma developed intra-uterine; This is the youngest patient described in the literature to date with orbital lymphoma.
In this series, compared with what was previously described in the literature, patients were younger by 25 months and more likely to present with bilateral disease (40% vs. 11% respectively). Given the young presentation (mean: 4 years), symptoms such as blurred vision or double vision may be under-reported in the paediatric population. In our series, three patients were diagnosed with orbital lymphoma under 36 months of age; they all presented with clear signs of ptosis or proptosis, which are easily identifiable signs. The two patients who were diagnosed after the age of three had more subtle clinical signs such as a convergence squint and a small palpable orbital mass, making a formal diagnosis more difficult; This may present a diagnosis bias due to a later presentation in older children.
Our literature review reports similar findings; with all patients under three years of age presenting with proptosis, globe displacement or a clear ophthalmoplegia.
In our cohort there was a higher prevalence of males (60%), a finding also seen in the literature review (67%). This finding reflects similar published data seen in systemic paediatric lymphoma [20], but differs from orbital lymphoma in the adult population; with a published male to female ratio of 52:48, which changes depending on the subtype of orbital lymphoma [21].
The signs in paediatric orbital lymphoma patients may resemble those seen in adults and include ptosis, proptosis, limited motility and strabismus, orbital mass or eyelid swelling, changes in visual acuity or lagophthalmos [21]. The unique finding in the paediatric population are signs that are not “classic” for orbital mass lesions such as convergent squint and esotropia, as seen in our cohort. Although most of the patients will have at least one of the more “classic” signs, some may present without it.
To our knowledge, this is the first documented case of an orbital lymphoma in a child under one month of age. In this patient, the proptosis and masses were seen as early as four days post-partum when prominence of one eye was reported by the parents. We speculate that this developed during pregnancy, given the advanced, multifocal disease seen at presentation involving both orbits, brain and bone marrow. There are no other reports of confirmed intra-uterine lymphoma, although Marcotte et al. who reviewed lymphoma in children aged from birth until the age of five, found a 2-fold risk in certain pregnancies including: feto-pelvic disproportion, and a previous pre-term birth. Non-Hodgkin Lymphoma (NHL) which is the most common lymphoma in the orbit was linked to premature rupture of membranes [20]. Triebwasser et al. showed a correlation between high birth weight and paediatric Hodgkin Lymphoma (HL) presenting between the ages of 0 and five years [22]. We have no data about peri-natal history or birth weight in the cases we describe. Burkitt’s lymphoma was the most common diagnosis in the literature (33%) and in our cohort (80%), although T-cell lymphoma, quite a rare orbital lymphoma was seen in 28% of the cases. Burkitt’s lymphoma is a rapidly progressing tumour found mostly in the paediatric population and accounts for 40% of childhood NHL [5, 6]. Of the three sub-types of Burkitt lymphoma, the endemic form is the most common one to affect the orbits and is commonly associated with the Epstein-Barr virus This is found in Sub-Saharan Africa [5].
T-cell lymphoblastic lymphoma is a rare cause of orbital involvement [23]. Primary orbital T Cell Lymphoma is even less common.
In our cohort, four of the five patients received local ophthalmic and/or orbital treatment alongside their chemotherapy. One patient had received lubrication for exposure keratopathy, two patients had refractive management with spectacles and one underwent squint surgery for residual strabismus. One patient underwent optic nerve decompression due to decreased visual function. Local ocular management is not well reported in the literature. The treatment of corneal exposure, dry eye, strabismus and refraction error is particularly relevant in the paediatric population due to the high risk of amblyopia. In cases of orbital involvement surgical decompression may be considered to preserve visual function and improve visual prognosis.
The systemic treatment of orbital lymphoma consists of chemotherapy and/or radiotherapy directed at the orbit lesion, although in lymphoma this is rarely indicated. Chemotherapy regimens differ depending on the tumour subtypes and paradigms have developed over time. Most treatments include a combination of steroids, cyclophosphamide, vincristine, methotrexate and anthracycline.
The outcome in our series was better than previously described in terms of overall mortality (0% vs. 27.7% mortality rate) despite a marginally longer follow-up period (26 vs. 25 months). This may relate to a more effective and modern treatment protocols compared to those previously reported. The concept of a multidisciplinary approach is considered mandatory in today’s practice and should include an oncologist, an oculoplastic surgeon and a paediatric ophthalmologist.
In the literature review we came across a population-based analysis of paediatric orbital lymphoma from the US [24]. This was an epidemiology study without any references to individual patients, and thus, it was not included in our study. It showed an incidence of 0.12 to 1000000 children, with a non-significant tendency towards males (similar to our findings and those of our literature review) and people of black ethnicity. The median age was 13 which is much older than the mean age in our cohort or the literature review. Lymphoma was diagnosed mainly in the conjunctiva (49%) and orbit (36%). Despite Burkitt’s lymphoma being the most prevalent subtype in our cohort and the literature review, it was seen in only 5.5% of this study and the most prevalent was extranodal marginal zone lymphoma (45.5%).
Conclusion
This series highlights a rare condition that should be considered in any child with an orbital mass, at any age. Other, progressive signs and symptoms may warrant imaging if the clinician does not have an adequate explanation for the progression of symptoms. Paediatric orbital lymphoma is much better treated nowadays with a low mortality rate of 21.7%. No mortality cases were seen in our recent cohort which, hopefully, reflect the improved treatment modalities and the usefulness of a multi-disciplinary approach which is increasingly utilized in modern medicine.
Summary
What was known before
-
Only about 20% present with bilateral disease.
-
Signs and symptoms resemble those of adults.
-
Complete remission is mostly achieved.
What this study adds
-
Orbital lymphoma can develop intra-uterine.
-
Up to 40% bilateral disease.
-
Burkitt’s lymphoma is the most prevalent in the orbit.
Data availability
All data in this manuscript is available in the John Radcliffe records under the laws of confidentiality.
References
Amit S, Purwar N, Agarwal A, Kanchan S. Primary orbital non-Hodgkin’s lymphoma. BMJ Case Rep. 2012. https://doi.org/10.1136/bcr-2012-006847
Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972;29:252–60. https://doi.org/10.1002/1097-0142(197201)29:1<252::AID-CNCR2820290138>3.0.CO;2-#
Fitzpatrick PJ, Macko S. Lymphoreticular tumors of the orbit. Int J Radiat Oncol Biol Phys. 1984;10:333–40. https://doi.org/10.1016/0360-3016(84)90051-8
Nutting CM, Jenkins CD, Norton AJ, Cree I, Rose GE, Plowman PN. Primary orbital lymphoma. Hematol J. 2002;3:14–16. https://doi.org/10.1038/sj.thj.6200142
Bouali S, Said IB, Yedeas MD, Abderrahmen K, Maatar N, Boubaker A, et al. Primary sporadic Burkitt lymphoma of the orbit, clinical characteristics, management, and outcomes: a case study. Child’s Nerv Syst. 2016;32:437–40. https://doi.org/10.1007/s00381-016-3018-1
Grasso D, Borreggine C, Ladogana S, De Santis R, Delle Noci N, Grilli G, et al. Sporadic Burkitt’s lymphoma/acute B-cell leukaemia presenting with progressive proptosis and orbital mass in a child. Neuroradiol J. 2016;29:231–5. https://doi.org/10.1177/1971400916639964
Gupta R, Yadav JS, Yadav S, Wadood A. Orbital involvement in nonendemic burkitts lymphoma. Orbit. 2012;31:441–5. https://doi.org/10.3109/01676830.2012.711886
Kiratli H, Uzun S, Varan A, Akyüz C, Orhan D. Management of anaplastic lymphoma kinase positive orbito-conjunctival inflammatory myofibroblastic tumor with crizotinib. J AAPOS. 2016;20:260–3. https://doi.org/10.1016/j.jaapos.2016.01.009
Hung IJ, Kuo TT, Sun CF. Subcutaneous panniculitic T-cell lymphoma developing in a child with idiopathic myelofibrosis. J Pediatr Hematol Oncol. 2020;21:38–41. http://www.ncbi.nlm.nih.gov/pubmed/10029810
Hassan AS, Elner VM. Orbital peripheral T-cell lymphoma in a child. Ophthal Plast Reconstr Surg. 2005;21:385–7. https://doi.org/10.1097/01.iop.0000176264.30697.02
Leidenix MJ, Mamalis N, Olson RJ, McLeish WM, Anderson RL. Primary T-cell Immunoblastic Lymphoma of the Orbit in a Pediatric Patient. Ophthalmology. 1993;100:998–1002. https://doi.org/10.1016/S0161-6420(13)31527-9
Alkatan HM, Alrashed SH, Al-Rikabi AC, Al-Faky YH. Orbital T-cell lymphoma in youngest recorded patient - Early diagnosis, management, and successful outcome: A case report and review of the literature. J Med Case Rep. 2018;12:139. https://doi.org/10.1186/s13256-018-1630-2
Alford MA, Nerad JA, Conlan RM, Comito M, Giller RH. Precursor B-cell lymphoblastic lymphoma presenting as an orbital mass. Orbit. 1999;18:17–24. https://doi.org/10.1076/orbi.18.1.17.2723
Pomeranz HD, McEvoy LT, Lueder GT. Orbital tumor in a child with posttransplantation lymphoproliferative disorder. Arch Ophthalmol. 1996;114:1422–3. https://doi.org/10.1001/archopht.1996.01100140622023
Edelstein C, Shields JA, Shields CL, De Potter P, Eagle J, Hagstrom N. Non-african burkitt lymphoma presenting with oral thrush and an orbital mass in a child. Am J Ophthalmol. 1997;124:859–61. https://doi.org/10.1016/S0002-9394(14)71714-3
King AJ, Fahy GT, Brown L. Null cell lymphoblastic lymphoma of the orbit [7]. Eye. 2000;14:665–7. https://doi.org/10.1038/eye.2000.165
Chou YC, Shih IH, Yang CP, Kuo TT, Hong HS. Concurrent mycosis fungoides and precursor B cell lymphoblastic lymphoma in a 6-year-old child. Pediatr Dermatol. 2005;22:23–5. https://doi.org/10.1111/j.1525-1470.2005.22105.x
Faridpooya K, Mulder MMS, Merks JHM, De Smet M, Pals ST, Saeed P. Precursor B lymphoblastic lymphoma of the orbit in a child: An unusual presentation of a non-Hodgkin lymphoma. Orbit. 2006;25:153–7. https://doi.org/10.1080/01676830600575501
Bhat SK, Shrestha SP, Barthakur R, Natarajan M. Atypical presentation and diagnostic pitfalls: A case of rapidly progressive bilateral proptosis in a child aged 18 months. Indian J Ophthalmol. 2008;56:68–70. https://doi.org/10.4103/0301-4738.37602
Marcotte EL, Ritz B, Cockburn M, Clarke CA, Heck JE. Birth characteristics and risk of lymphoma in young children. Cancer Epidemiol. 2014;38:48–55. https://doi.org/10.1016/j.canep.2013.11.005
Olsen TG, Heegaard S. Orbital lymphoma. Surv Ophthalmol. 2019;64:45–66. https://doi.org/10.1016/j.survophthal.2018.08.002
Triebwasser C, Wang R, DeWan AT, Metayer C, Morimoto L, Wiemels JL, et al. Birth weight and risk of pediatric Hodgkin lymphoma: Findings from a population-based record linkage study in California. Eur J Cancer. 2016;69:19–27. https://doi.org/10.1016/j.ejca.2016.09.016
Coupland SE, Krause L, Delecluse HJ, Anagnostopoulos I, Foss HD, Hummel M, et al. Lymphoproliferative lesions of the ocular adnexa: Analysis of 112 cases. Ophthalmology. 1998;105:1430–41. https://doi.org/10.1016/S0161-6420(98)98024-1
Moustafa GA, Topham AK, Aronow ME, Vavvas DG. Paediatric ocular adnexal lymphoma: a population-based analysis. BMJ Open Ophth. 2020;5:000483. https://doi.org/10.1136/bmjophth-2020-000483
Acknowledgements
We are grateful to Dr. Debora Pehl (Oxford University Hospitals NHS Foundation Trust) who reviewed the biopsy, made the diagnosis and provided the images.
Author information
Authors and Affiliations
Contributions
All authors contributed in data collection and participated in the writing of the manuscript and review process
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keren, S., Lapira, M., McCallum, E. et al. Paediatric orbital lymphoma; a case series and review of the literature. Eye 37, 1002–1008 (2023). https://doi.org/10.1038/s41433-022-02266-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02266-1
This article is cited by
-
Ocular oncology demystified
Eye (2023)