Abstract
Background/Objectives:
To analyse the approach to diagnose gastroesophageal reflux (GER) and the qualification criteria for anti-reflux (AR) procedures in Polish children fed via gastrostomy between 2000 and 2010.
Subjects/Methods:
An electronic questionnaire containing questions on the demographic and clinical data of patients with gastrostomies was distributed to six Polish centres of nutritional therapy. The portion pertaining to GER included data on clinical exponents, diagnostic procedures (pH-metry, pH-impedance, scintigraphy and upper gastrointestinal (GI) series) and AR.
Results:
In total, 348 children (M199/F149; age at gastrostomy 5.78±5.49 years) were included. Data on the diagnosis of GER and the AR criteria were available for 343 and 336 subjects, respectively. Percutaneous endoscopic gastrostomy was performed in 258/348 patients (74.1%), while surgery was performed in 80/348 patients (23%). The data from 10/348 (2.9%) cases were unavailable. At least one of the tests for GER was conducted in 177/343 (51.6%) of patients: pH-metry in 74/343 (21.6%), pH-impedance in 17/343 (5.0%), scintigraphy in 60/343 (17.5%) and upper GI series in 102/343 (29.7%). GER was reported in 114/343 cases (33.2%), and fundoplication was performed in 87 children (76.3% of patients with GER). The highest congruence between a positive test result and the decision to perform fundoplication was documented in cases of scintigraphy and upper GI series (P=0.00000 and P=0.00191, respectively). A significant increase in the prevalence of simultaneous gastrostomy and AR was observed over the decade analysed (r=0.8, P=0.009). This study revealed a centre-specific attitude towards the diagnosis of GER and the assessment of qualifications for fundoplication in Polish gastrostomy-fed children.
Conclusions:
The unified diagnostic algorithm of GER and the universal qualification criteria for AR procedures need to be defined for gastrostomy-fed children.
Similar content being viewed by others
Introduction
Gastrostomy is currently a widely applied method for providing nutritional support to children with disorders that make obtaining adequate nutrition impossible via physiological routes.1, 2, 3
The interplay between the construction of nutritional gastrostomy and gastroesophageal reflux (GER) is still controversial. The preference of some centres to simultaneously perform gastrostomy and fundoplication is based on the idea that gastrostomy enhances GER, particularly in patients with chronic impairments of the central nervous system (CNS). Such an approach was proposed and named a ‘protective anti-reflux operation’ by Jolley et al.,4 who utilised oesophageal pH-monitoring to determine the need for combined anti-reflux (AR) and gastrostomy procedures in neurologically disabled children. However, further studies have not provided reliable data to support the predictive value of pH-metry for the AR surgery decision-making process and outcome. Similarly, no other single diagnostic test (for example, pH-impedance, barium studies, gastrointestinal (GI) scintigraphy, endoscopy or ultrasound examination) has provided reliable data anticipating a post-gastrostomy evolution of GER that will require AR surgery.5, 6 Moreover, the results of recently published surveys have indicated that the percentage of patients with isolated gastrostomy who require further AR surgeries is low, further emphasising current consensus statements (NSPGHAN/ESPGHAN).7, 8, 9, 10, 11, 12 The aim of this study was to analyse the methods used in the diagnosis of GER, as well as the qualification criteria for fundoplication in Polish children subjected to enteral nutrition via gastrostomy over the period of 2000–2010. The study, conducted under the auspices of the Polish Society of Pediatric Gastroenterology, Hepatology and Nutrition, included Polish hospital-based centres that dealt with the nutritional therapy of children during the decade analysed. To the best of our knowledge, this study is the first critical, multicentre, nationwide analysis of the ‘real-life approach’ to the qualification of AR procedures for children fed via gastrostomy. The only similar, previously published study dealt with the trends and inter-centre differences in the performance of AR procedures in a generally American population under 18 years of age.13
Materials and methods
The study involved six Polish centres of nutritional therapy: two from Warsaw, and one each from Gdansk, Katowice, Lodz and Toruń. The protocol of the study was approved by the Bioethical Committee of The Children’s Memorial Health Institute in Warsaw.
We developed an electronic questionnaire containing questions on the demographic and clinical data of patients. The portion of the questionnaire pertaining to the diagnosis of GER included questions about the clinical signs and diagnostic procedures of pH-metry, pH-impedance, scintigraphy and upper GI series (Supplementary Table 1).
Within the examined period, we analysed the prevalence of AR surgery, along with its selection criteria and the relationship between the mode of the decision-making process and the centre where the children were treated.
Statistical analysis
Correlations were assessed using the Pearson correlation coefficient. The Chi-square test was used for nominal data. P-values lower than 0.05 were considered as statistically significant.
Results
A total of 348 children (M/F: 199/149; mean age at gastrostomy insertion 5.78±5.49 years; median: 3.93 (25–75%: 0.99–9.59)) were included in the study. Data on the diagnosis of GER were available for 343 participants, and the data regarding the AR procedure were available for 336 cases. In 285 cases (81.9%), the feeding disorders resulted from CNS impairments of various origins (Supplementary Table 2). Percutaneous endoscopic gastrostomy (PEG) was performed in 258 children (74.1%), and surgical gastrostomy was performed in 80 patients (23%). Information on the method of gastrostomy insertion was unavailable in 10 cases (2.9%). The mean age of the patients at the first gastrostomy placement increased during the successive years of the decade analysed (r=0.13, P=0.0199; Supplementary Figure 1). The number of gastrostomies performed within the 10-year period is shown in Figure 1.
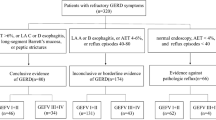
Different combinations of the diagnostic modalities for GER were used as shown in the Venn diagram (Figure 2). At least one of the tests was conducted in 177/343 patients (51.6%). pH-metry was performed in 74 children (21.6%), pH-impedance in 17 (5.0%), scintigraphy in 60 (17.5%) and upper GI series in 102 (29.7%). In 166 children (48.4%), the assessment was based solely on the analysis of clinical signs. Overall, the diagnosis of GER was reported in 114/343 children (33.2%).
Fundoplication was performed in 87 patients (including 81 neurological children), corresponding to 25.9% of the patients with available documentation of the AR procedure and to 76.3% of the children diagnosed with GER. In 72 cases (21.4%), the decision to perform AR was based on the positive results of test(s) for GER, and in 13 (3.9%), solely on the presence of the clinical signs of reflux. Two children (0.6%) were subjected to fundoplication in the absence of clinical symptoms and without any prior test(s) for GER. The numbers of fundoplications and established cases of GER during the analysed period are presented in Figures 3 and 4.
A significant increase in the prevalence of simultaneous gastrostomy and fundoplication was observed in the 10-year period covered by this study (r=0.8, P=0.009; Figure 5).
Among the diagnostic modalities of GER, the highest congruence between the positive result of the test and the decision to perform fundoplication was documented in the cases of scintigraphy and upper GI series (P=0.00000 and P=0.00191, respectively). For the remaining diagnostic tests, pH-metry (P=0.48350) and pH-impedance (P=0.49015), the congruence proved to be insignificant. The frequency distribution of the utilisation of various diagnostic tests and fundoplication in participating centres is presented in Table 1.
The comparison of nutritional status (percentile of body weight) before and 12 months following gastrostomy revealed a significant improvement in this parameter in the entire group of patients (P=0.0001) and in AR and non-AR children as well (P=0.008 and P=0.001, respectively; Supplementary Figures 2 and 3).
Discussion
Feeding via gastrostomy is a method of nutritional support used in patients with various conditions; however, the chronic impairment of the CNS and neuromuscular disorders constitutes the most frequent indications for its implementation in pediatrics.3, 10, 11, 12, 14 Corresponding to 20–72% of cases, patients with neurological abnormalities predominate in all available registries of home enteral nutrition (HEN), as well as in large multicentre studies.15, 16, 17
We observed a similar structure related to the indications for gastrostomy formation in the present study, which was based on the retrospective data from questionnaire surveys based on the children with gastrostomies treated between 2000 and 2010 in the participating hospital-based centres. After a reimbursement for HEN was introduced in Poland by the National Health Fund (in 2008 for pediatric patients), the number of children fed via gastrostomy increased significantly, with the prevalence of HEN amounting to 13.75 per 1 million inhabitants.18 Our analysis included patients whose medical data were made available by the collaborating teams; therefore, there was a risk of omitting some individuals treated at the newly funded nutritional outpatient clinics, which were established after 2008. Nevertheless, the number of children included in our study was relatively large (348 participants), making this group representative of the Central European population. Additionally, the analysis of the collected data provided information on ‘real-life’ clinical practices with regard to the diagnosis of GER and the qualifications for AR surgery in children enrolled to receive enteral nutrition via gastrostomy.
The gastrostomy was placed endoscopically in most participating children (74%), and the mean age of participants at qualification was 5.78±5.49 years, increasing slightly during the studied decade. PEG is considered as a safe and widely preferred pediatric procedure.12, 19 A retrospective multicentre analysis of HEN in children was published recently by an Italian group.16 The mean age of this cohort (4 centres, 14 years of follow-up) was 2 years. Gastrostomy/gastrojejunostomy was performed in 41% of children, although the method of constructing the gastrostomy was not mentioned. Ponsky et al.20 published the results of a retrospective analysis covering a similar period (2000–2008; 884 patients from two surgical centres in United States). In this study, the mean age of the children at qualification for gastrostomy was also markedly lower (2.9 years) than in our series. Of note is the relatively frequent use of the laparoscopic approach in the placement of the gastrostomy; the laparoscopic and endoscopic approaches were used at roughly equal frequencies (∼40% each). A comparison of our findings with those published by the Italian group and American centre showed that, despite the increasing availability of the procedure, the qualification of children with CNS impairment for gastrostomy is still postponed in our country, the number of patients is underestimated, and the laparoscopic method is practically not in use. In contrast, the results of recently published studies suggest that the laparoscopic approach can constitute a safe alternative to PEG, particularly in younger children.21 A trend towards the implementation of gastrostomy in older children was observed in our study; this, in our opinion, reflects the growing availability of the medical procedure and the catch-up phenomenon, which is demonstrated by the young patients instead of older patients requiring nutritional support.
The association among dysphasia, GER and pulmonary aspiration and, consequently, the attitude towards the decision to perform AR procedures in children with chronic CNS impairments requiring gastrostomy have recently stimulated debate in the literature.3, 11, 12, 20
The analysis of the results of our survey on the diagnostic criteria of GER and the qualification criteria for fundoplication revealed high variability in this matter. Among the diagnostic methods included in our analysis, clinical symptoms constituted the only diagnostic/exclusion criterion for GER in 48% of the patients, while more than a half of the patients (52%) had at least one diagnostic test for GER. Radiological evaluation was used the most frequently (30% of the patients) and was often performed together with scintigraphy or pH-metry (Figure 3). In the study by Cuenca et al.,22 the upper GI series was conducted in 71% of children who qualified for gastrostomy and AR. The results of radiology were abnormal in 37% of the participants; the most frequently diagnosed pathologies included GER (80%) and anatomical abnormalities (6%). The authors emphasized that, in most of the children, the diagnosis of GER could be established on the basis of presented clinical signs and the results of tests that detect GER with a high probability (pH-metry and evaluation of gastric emptying). It is of note that the NSPGHAN/ESPGHAN guidelines on the clinical practice of pediatric gastroesophageal reflux (2009) strictly views the upper GI series as a useful diagnostic tool for detecting structural abnormalities in the esophagus and other parts of GI tract; however, the routine performance of upper GI series is not recommended for the diagnosis of GERD. The shortcomings of barium contrast studies (besides radiation exposure, which should be always considered in chronically ill children) include the risk of omitting or over-interpreting reflux episodes during this short-term procedure. These shortcomings result in low and non-reproducible sensitivity (29–86%) and specificity (21–83%) for the upper GI series, as estimated by the pH-monitoring and pH-impedance monitoring.6, 23, 24, 25 pH metry was the second most frequently used diagnostic test for GER in our study (22% of patients from various centres). Additionally, pH-impedance was tested for in 5% of the patients. pH metry is still the principal method for the diagnosis of acidic GER, and pH-impedance is considered as a golden standard in the detection of reflux, irrespective of its physicochemical properties.6, 26, 27 Nevertheless, prospective studies did not confirm the enhancement of reflux following the formation of isolated gastrostomy.28, 29 In contrast, an improvement in the nutritional status of patients with CNS impairment, including those with pH-metrically confirmed GER, was documented to facilitate gastric emptying and reduce the frequency of reflux episodes.30 Therefore, the predictive value of the tests identifying the intra-oesophageal presence of gastric reflux during the qualification for the AR procedures is low. For our patients, scintigraphy was used in combination with upper GI series or pH-metry or as an isolated diagnostic test. This method not only enables the identification of reflux but can also detect pulmonary aspiration.31 Thus, it is a potentially valuable method for identifying patients who may require AR surgery. However, its application is limited by its relatively low availability (only two centres involved in our study had the capability), the lack of unified protocols of examination, and the necessity of sedation in non-complying patients. Furthermore, there is a lack of prospective studies documenting the long-term effects in patients who qualified for gastrostomy and AR on the basis of scintigraphy.
GER was detected in 33% of the children participating in our study. According to the literature, the prevalence of GER in neurological patients ranges from 15 to 78%, depending on the source and methods.3, 6, 32, 33 In a previously published study conducted by the co-authors of this paper, the prevalence of GER in children with CNS injuries, as determined on the basis of pH-impedance before PEG, was 29%.29
The results of our survey point to an association between the selection of diagnostic tests and the treatment centre (Table 1). While scintigraphy and pH-impedance were performed in single centres, pH-metry was used in all participating centres and performed for 21% of all patients. Noticeably, despite its wide availability, pH-metry was not recommended for every patient; depending on the centre, it was performed in 3.5%–64.5% of the children. Similar centre-specific tendencies were documented through the analysis of the frequency distributions of AR procedures in various regions.
In 76% of patients with established GER, fundoplication was performed. On the basis of our data, we were unable to directly determine the predictive values of the various diagnostic tests used in the qualification for fundoplication. Analysing the congruence of the positive results of a given test and the decision to perform the AR procedure, we revealed that AR was most frequently performed in children with ‘reflux’ results from scintigraphy and upper GI series. Moreover, there were isolated cases in which fundoplication was performed despite the absence of GER, the lack of confirmation from any clinical tests and the presence of symptoms. This suggests that CNS impairment was regarded as the sole indication for the AR procedure.
Both the number of gastrostomies and the frequency of AR procedures performed in the group of children analysed here increased during subsequent years (Figures 1, 3 and 4). Moreover, we observed a significant increase in the frequency of combined procedures, while the percentage of delayed fundoplications remained at a relatively stable level (Figure 5). The increase in the number of combined procedures and the high percentage of children subjected to the AR procedures overall in our cohort undoubtedly require clarification, as these trends do not follow the recently recommended models of care or data reported by other authors.6, 20, 34 Ponsky et al.20 revealed that the percentage of children with primary isolated gastrostomy requiring further fundoplication did not exceed 10%. In the group of children analysed by Viswanath et al.,34 17% had indications for the AR procedure during the follow-up; the morbidity rate was higher in children subjected to simultaneous PEG and fundoplication.
On the basis of systematic review, Noble et al.35 identified only eight pediatric studies analysing the prevalence of GER before and after gastrostomy. The authors concluded that their findings did not support a causative relationship between gastrostomy and an increase in the GER exponents. Moreover, it was shown that children subjected to a combined gastrostomy and AR procedure did not show improved scores in terms of their nutritional parameters compared to patients with isolated gastrostomies.11 Our analysis revealed a significant improvement in body weight after 12 months of gastrostomy feeding in the whole examined cohort; no significant differences were found between the AR and non-AR groups.
There are no data comparing the outcomes of AR procedures and the pharmacological treatment in children with GERD. A meta-analysis of the results for adults did not favour any of the approaches and indicated that as many as 70% of patients undergoing operations may still require anti-secretory treatments, even 7 years after the AR procedure.36, 37 At the same time, the higher complication rate reported in neurologically impaired children who have undergone Nissen fundoplication and the lack of control of respiratory symptoms in nearly 1/3 of patients should be considered.38
It is not possible to directly compare the results of our nationwide analysis on the gastrostomy-GER-AR approach with the findings of other authors. Data from European HEN registries, as well as the results of a recently published multicentre study of children with cerebral palsy from six European countries, do not contain any details on the prevalence of GER and AR procedures in patients with gastrostomy.15, 16, 17 Likewise, this issue was not addressed in the previously mentioned study dealing with HEN in Italian children.16
Various possible drawbacks exist to the interpretation of our findings. First, the lower availability of HEN must be considered. Compared with the availability of HEN in developed countries, lower availability of HEN results in the referrals of children with more profound malnutrition and complications to highly specialised centres, and this is reflected in more aggressive treatment. The higher mean age of the patients included in our study constitutes an argument supporting this hypothesis. Second, the indications for AR procedures could be exaggerated due to the high predictive values ascribed to diagnostic tests or routine qualifications for fundoplication in the cases of children with certain conditions.
Interesting findings were reported by Goldin et al.,13 who analysed the number of AR procedures performed in the general pediatric population of the United States between 2001 and 2006. The data obtained from electronic databases contained the records of 13 691 AR procedures, 23 527 gastrostomies, 41 441 appendectomies and 14 895 pyloromyotomies performed in patients under 18 years of age between 2001 and 2006. Thirty-nine AR procedures were performed in children with CNS abnormalities, while 33% of AR cases were diagnosed with aspiratory pneumonia, 44% of which were subjected to laparoscopic procedures. The authors of this study revealed a marked decrease in the number of AR procedures in both their absolute number and their value relative to other types of pediatric surgeries. During the period analysed here, the prevalence of AR in American children was approximately fourfold lower than the frequency of gastrostomies. In some hospitals, the prevalence of AR procedures was 40 times lower than the prevalence of other procedures, while other centres performed a 10-fold higher number of fundoplications relative to other comparable procedures.
The number of patients included in our study may correspond to only one centre represented in the above-mentioned report. However, it should be noted that we analysed the data of a selected group of patients requiring gastrostomy (82% neurological children), while Goldin et al.13 studied the prevalence of this procedure in the general population, of which the neurological indications constitute ∼40%. Furthermore, there is a risk of underestimating our data due to the lack of a centralised system for registering medical procedures. Nevertheless, this analysis of our series indicates a lower prevalence of gastrostomies and AR procedures in general, as well as a change in their proportions in the course of long-term observations. The differences in the number of AR procedures performed in various American hospitals suggest that the centre-specific approach documented in our material may be a universal phenomenon that should not be ascribed to the specific character of Polish health-care system. Rather, this circumstance is the result of various centres specialising in different procedures.
In conclusion, our study revealed that the fraction of ‘neurological’ indications for AR procedures in the group of Polish gastrostomy-fed children is higher than those in other European countries and the United States. GER can be detected through various diagnostic tests and is performed in various combinations and under different clinical conditions. Most likely, this represents an unnecessary burden for the patient and increases the cost of diagnosis. The prevalence of GER in our cohort is similar to those in the other European populations, while the constantly increasing percentage of children qualifying for simultaneous gastrostomy and fundoplication in our study is higher than that in the other countries. Thus, a comprehensive analysis of the qualification criteria used in all participating centres is necessary. Additionally, our study revealed a centre-specific attitude towards the diagnosis of GER and the qualifications for the AR procedure among Polish gastrostomy-fed children. In our opinion, this attitude results from the lack of unified recommendations that can be adapted to local conditions related to this matter. We believe that this conclusion has practical significance, particularly for nutritional teams in countries that continue to implement nutritional therapy procedures, as it indicates the necessity of more precisely defining the standards.
References
Sleigh G, Brocklehurst P . Gastrostomy feeding in cerebral palsy: a systematic review. Arch Dis Child 2004; 89: 534–539.
Lochs H, Allison SP, Meier R, Pirlich M, Kondrup J, Schneider S et al. Introductory to the ESPEN Guidelines on Enteral Nutrition: Terminology, definitions and general topics. Clin Nutr 2006; 25: 180–186.
Fortunato JE, Troy AL, Cuffari C, Davis JE, Loza MJ, Oliva-Hemker M et al. Outcome after percutaneous endoscopic gastrostomy in children and young adults. J Pediatr Gastroenterol Nutr 2010; 50: 390–393.
Jolley S, Smith E, Tunell W . Protective antireflux operation with feeding gastrostomy. Experience with children. Ann Surg 1985; 201: 736–740.
Rosen R, Levine P, Lewis J, Mitchell P, Nurko S . Reflux events detected by pH-MII do not determine fundoplication outcome. J Pediatr Gastroenterol Nutr 2010; 50: 251–255.
Vandenplas Y, Rudolph CD, Di Lorenzo C, Hassall E, Liptak G, Mazur L et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr 2009; 49: 498–547.
Isch J, Rescorla F, Scherer L, West K, Grosfeld J . The development of gastroesophageal reflux after percutaneous endoscopic gastrostomy. J Pediatr Surg 1997; 32: 321–322.
Wilson G, van der Zee D, Bax N . Endoscopic gastrostomy placement in the child with gastroesophageal reflux: is concomitant antireflux surgery indicated. J Pediatr Surg 2006; 41: 1441–1445.
Puntis JW, Thwaites R, Abel G, Stringe MD . Children with neurological disorders do not always need fundoplication concomitant with percutaneous endoscopic gastrostomy. Dev Med Child Neurol 2000; 42: 97–99.
Loser C, Aschl G, Hebuterne X, Mathus-Vliegen EM, Muscaritoli M, Niv Y et al. ESPEN guidelines on artificial enteral nutrition--percutaneous endoscopic gastrostomy (PEG). Clin Nutr 2005; 24: 848–861.
Marchand V, Motil KJ, Nutrition Nco. Nutrition support for neurologically impaired children: a clinical report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr 2006; 43: 123–135.
Braegger C, Decsi T, Dias JA, Hartman C, Kolacek S, Koletzko B et al. Practical approach to paediatric enteral nutrition: a comment by the ESPGHAN committee on nutrition. J Pediatr Gastroenterol Nutr 2010; 51: 110–122.
Goldin AB, Garrison M, Christakis D . Variations between hospitals in antireflux procedures in children. Arch Pediatr Adolesc Med 2009; 163: 658–663.
Brant CQ, Stanich P, Ferrari AP Jr . Improvement of children's nutritional status after enteral feeding by PEG: an interim report. Gastrointest Endosc 1999; 50: 183–188.
Frias L, Puiggros C, Calanas A, Cuerda C, Garcia-Luna PP, Camarero E et al. Home enteral nutrition in Spain: NADYA registry in 2010. Nutr Hosp 2012; 27: 266–269.
Diamanti A, Di Ciommo VM, Tentolini A, Lezo A, Spagnuolo MI, Campanozzi A et al. Home enteral nutrition in children: a 14-year multicenter survey. Eur J Clin Nutr 2013; 67: 53–57.
Dahlseng MO, Andersen GL, DAGA M, Arnaud C, Balu R, De la Cruz J et al. Gastrostomy tube feeding of children with cerebral palsy: variation across six European countries. Dev Med Child Neurol 2012; 54: 938–944.
Szlagatys-Sidorkiewicz A, Popinska K, Toporowska-Kowalska E, Borkowska A, Sibilska M, Gebora-Kowalska B et al. Home enteral nutrition in children--2010 nationwide survey of the Polish Society for Clinical Nutrition of Children. Eur J Pediatr 2012; 171: 719–723.
Minar P, Garland J, Martinez A, Werlin S . Safety of percutaneous endoscopic gastrostomy in medically complicated infants. J Pediatr Gastroenterol Nutr 2011; 53: 293–295.
Ponsky TA, Gasior AC, Parry J, Sharp SW, Boulanger S, Parry R et al. Need for subsequent fundoplication after gastrostomy based on patient characteristics. J Surg Res 2013; 179: 1–4.
Wragg RC, Salminen H, Pachl M, Singh M, Lander A, Jester I et al. Gastrostomy insertion in the 21st century: PEG or laparoscopic? Report from a large single-centre series. Pediatr Surg Int 2012; 28: 443–448.
Cuenca AG, Reddy SV, Dickie B, Kays DW, Islam S . The usefulness of the upper gastrointestinal series in the pediatric patient before anti-reflux procedure or gastrostomy tube placement. J Surg Res 2011; 170: 247–252.
Siebert J, Byrne W, Euler A, Latture T, Leach M, Campbell M . Gastrooesophageal reflux- the acid test: scintigraphy or pH probe? Am J Roentgenol 1983; 140: 1087–1090.
Thompson J, Koehler R, Richter J . Detection of gastroesophageal reflux: value of barium studies compared with 24-hr pH monitoring. Am J Roentgenol 1994; 162: 621–626.
Macharia E . Comparison of upper gastrointestinal contrast studies and pH-impedance tests for diagnosis of childhood gastro-oesophageal reflux. Pediatr Radiol 2012; 42: 946–951.
Bredenoord AJ, Tutuian R, Smout AJ, Castell DO . Technology review: Esophageal impedance monitoring. Am J Gastroenterol 2007; 102: 187–194.
Wenzl TG, Benninga MA, Loots CM, Salvatore S, Vandenplas Y, Group EE-PW. Indications, methodology, and interpretation of combined esophageal impedance-pH monitoring in children: ESPGHAN EURO-PIG standard protocol. J Pediatr Gastroenterol Nutr 2012; 55: 230–234.
Razeghi S, Lang T, Behrens R . Influence of percutaneous endoscopic gastrostomy on gastroesophageal reflux: a prospective study in 68 children. J Pediatr Gastroenterol Nutr 2002; 35: 27–30.
Toporowska-Kowalska E, Gebora-Kowalska B, Jablonski J, Fendler W, Wasowska-Krolikowska K . Influence of percutaneous endoscopic gastrostomy on gastro-oesophageal reflux evaluated by multiple intraluminal impedance in children with neurological impairment. Dev Med Child Neurol 2011; 53: 938–943.
Wakamatsu H, Nagamachi S, Nishii R, Higaki K, Kawai K, Kamimura K et al. Effect of percutaneous endoscopic gastrostomy on gastrointestinal motility: evaluation by gastric-emptying scintigraphy. Nucl Med Commun 2008; 6: 562–567.
Ravelli AM, Panarotto MB, Verdoni L, Consolati V, Bolognini S . Pulmonary aspiration shown by scintigraphy in gastroesophageal reflux-related respiratory disease. Chest 2006; 130: 1520–1526.
Sullivan PB . Gastrostomy and the disabled child. Dev Med Child Neurol 1992; 34: 552–555.
Sondheimer JM, Morris BA . Gastroesophageal reflux among severely retarded children. J Pediatr 1979; 94: 710–714.
Viswanath N, Wong D, Channappa D, Kukkady A, Brown S, Samarakkody U . Is prophylactic fundoplication necessary in neurologically impaired children? Eur J Pediatr Surg 2010; 20: 226–229.
Noble LJ, Dalzell AM, El-Matary W . The relationship between percutaneous endoscopic gastrostomy and gastro-oesophageal reflux disease in children: a systematic review. Surg Endosc 2012; 26: 2504–2512.
Spechler SJ, Lee E, Ahnen D, Goyal RK, Hirano I, Ramirez F et al. Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease: follow-up of a randomized controlled trial. JAMA 2001; 285: 2331–2338.
Vernon-Roberts A, Sullivan P . Fundoplication versus post-operative medication for gastroesophageal reflux in children with neurological impairment undergoing gastrostomy. Cochrane Database Syst Rev 2007; 24: CD006151.
Wong KK, Liu XL . Perioperative and late outcomes of laparoscopic fundoplication for neurologically impaired children with gastro-esophageal reflux disease. Chin Med J (Engl) 2012; 125: 3905–3908.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Toporowska-Kowalska, E., Gębora-Kowalska, B., Fendler, W. et al. Diagnosis of gastroesophageal reflux and anti-reflux procedures among polish children with gastrostomies: a 10-year nationwide analysis. Eur J Clin Nutr 67, 1169–1174 (2013). https://doi.org/10.1038/ejcn.2013.164
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2013.164
Keywords
This article is cited by
-
Fundoplication with gastrostomy vs gastrostomy alone: a systematic review and meta-analysis of outcomes and complications
Pediatric Surgery International (2017)
-
Percutaneous endoscopic gastrostomy (PEG) does not worsen vomiting in children
Pediatric Surgery International (2015)