Abstract
Gastroesophageal flap valve (GEFV) grading is a simple and reproducible parameter. There is limited information about the association between GEFV abnormality and novel parameters in patients with gastroesophageal reflux disease(GERD) symptoms by the Lyon Consensus. To investigate the value of GEFV grading in GERD, the clinical data of 320 patients with GERD symptoms who underwent endoscopy, 24-h multichannel intraluminal impedance-pH (MII-pH) monitoring, and high-resolution manometry (HRM) were retrospectively analyzed. The percentage of acid exposure time (AET%)(4.2 [1.5–7.4] vs. 1.3 [0.3–4.2], P < 0.001) and the proportion of abnormal esophagogastric junction (EGJ) morphology (71 [87.7%] vs. 172 [72.0%], P = 0.011) were significantly higher, while the mean nocturnal baseline impedance (MNBI) (2068.3 [1658.4–2432.4] vs. 2228.5 [1794.8–2705.3]Ω, P = 0.012) and post-reflux swallow-induced peristaltic wave index (PSPWI) (19.7 [13.9–29.0] vs. 33.3 [25.0–44.0]%, P < 0.001) were significantly lower in the abnormal GEFV group compared with the normal GEFV group. AET% and EGJ morphology showed positive correlations with GEFV grade, while PSPWI and MNBI showed negative correlations. Patients with an abnormal GEFV had a significantly greater risk of conclusive evidence of GERD compared to those with a normal GEFV (OR 3.035, 95% CI 1.758–5.240, P < 0.001). Further, when identifying patients with conclusive evidence of GERD, abnormal GEFV had a specificity of 80.4% (95% CI 75.3–85.5%). GEFV grading might be regarded as supportive evidence for GERD diagnosis.
Similar content being viewed by others
Introduction
Gastroesophageal reflux disease (GERD) is a common clinical condition. Although it is a benign disease, longstanding GERD can lead to Barrett's esophagus (BE), a premalignant condition1. Hence, accurate and timely diagnosis of GERD is important. The Lyon Consensus was developed to aid the diagnosis of GERD based on 24-h multichannel intraluminal impedance-pH (MII-pH), upper gastrointestinal endoscopy, and high-resolution manometry (HRM). Accordingly, the evidence for GERD is classified as follows: conclusive evidence for pathologic reflux, borderline or inconclusive evidence, adjunctive or supportive evidence, and evidence against pathological reflux2.
MII-pH monitoring is used increasingly often for diagnosing GERD. The mean nocturnal baseline impedance (MNBI) and post-reflux swallow-induced peristaltic wave index (PSPWI) are two novel parameters detected on MII-pH and regarded as supportive parameters for detecting GERD2. The MNBI reflects the reflux-induced impairment of mucosal integrity3,4. On the other hand, the PSPWI highlights the integrity of primary peristalsis initiated by reflux4.
The esophagogastric junction (EGJ) is important for the prevention of GERD5. The gastroesophageal flap valve (GEFV) serves as the anti-reflux barrier and is easily visualized with a retroflexed endoscope with an excellent inter-observer agreement6. Previous studies have found that GEFV grade is positively associated with acid reflux and could reflect EGJ morphology7.
However, the GEFV is not included in the Lyon Consensus, and studies on the potential associations between GEFV grading and GERD classification by the Lyon Consensus, mucosal integrity, esophageal peristaltic function, and EGJ are limited. In the present study, we aimed to assess the correlations between GEFV grading and the classification of GERD by the Lyon Consensus and to explore the relationship of GEFV grading with the MNBI and PSPWI, EGJ morphology, EGJ tone, and esophageal body motility.
Methods
Patient selection
A retrospective chart review of adult patients with GERD symptoms (heartburn and/or regurgitation) who underwent endoscopy, HRM, and 24-h MII-pH at Beijing Tong Ren Hospital from August 2015 to January 2020 was conducted. The exclusion criteria were: inadequate or incomplete studies; pregnancy; previous thoracic, esophageal or gastric surgery; the presence of infectious, eosinophilic esophagitis or scleroderma; achalasia cardia, and EGJ outflow obstruction and major esophageal motility disorders such as absent contractility. The Medical Ethics Committee of Beijing Tong Ren Hospital approved the study (Approved Document Number: trxhzcfa01). All patients had signed informed consent for the endoscopy, MII-pH, HRM, and use of data for research purposes. And all methods were carried out in accordance with relevant guidelines and regulations.
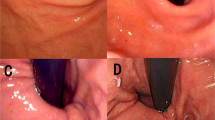
Endoscopic examination
All patients underwent upper gastrointestinal (GI) endoscopy using a GIF-260 upper GI endoscope (Olympus, Hamburg, Germany) under intravenous anesthesia or topical anesthesia. Esophagitis was diagnosed and graded by the Los Angeles classification8. Barrett’s esophagus (BE) was diagnosed by confirmation of intestinal metaplasia by pathology. Each GEFV was graded using Hill's classification from grade I to IV as described previously6. A GEFV that remained tightly snug to the endoscope was categorized as grade I. A GEFV that opened and closed with respiration was considered grade II. A GEFV that failed to remain snug to the endoscope was rated as grade III. If a wide-open diaphragmatic hiatus was observed by endoscopy, the GEFV was categorized as grade IV6. All endoscopists in the department had attended a previous training workshop on GEFV evaluation and were encouraged to assess GEFV grading during endoscopic examination. All endoscopic procedures in our study were performed by one experienced endoscopist (Z.H.G.) who had experience performing upper gastrointestinal endoscopy with at least 5000 procedures over the last 5 years, and GEFV grading was determined during endoscopic examination. To ensure consistency of GEFV grading, all the clear photographs of GEFV of enrolled patients were reviewed again by the other author (Y.T.Z.), who was blind to the patient information. If disagreement occurred, a senior endoscopist (C.Z.) would participate in making the final decision.
Esophageal HRM
All patients were instructed to stop proton pump inhibitors, prokinetic antagonists, and H2 receptors at least 2 weeks before esophageal HRM and reflux monitoring. HRM was performed after an overnight fast using a 36-channel trans-nasal solid-state catheter system with circumferential sensors 1 cm apart (Medical Measurement Systems Inc. [MMS], Williston, VT, USA). Esophageal motility was assessed by using 5 mL of ambient temperature water at 30-s intervals for at least 10 water swallows as previously described9. The Chicago Classification version 3.0 (CCv3.0) criteria were used to evaluate each HRM study (EGJ morphology, EGJ tone, and esophageal body contractility and motility)10. The EGJ morphology was determined by the relation between the lower esophageal sphincter (LES) and crural diaphragm (CD). EGJ-contractile integral (EGJ-CI), expiratory EGJ pressure (EGJP-exp), and inspiratory EGJ pressure (EGJP-insp) were calculated as previously described10,11. Esophageal body motility was classified as follows: normal peristalsis, ineffective esophageal motility (IEM), and fragmented peristalsis10.
MII-pH recording
Immediately after HRM, the pH-impedance catheter (eight impedance rings and one pH ring, Ref. No 261A; Given Imaging, Los Angeles, CA, USA) was placed. Data from the pH-impedance monitor were downloaded and analyzed using the MMS database software. All data were initially identified by the software and subsequently verified and calculated by two of the authors (Z.H.G. and Y.H.W.) for accuracy. The total number of reflux events and the total acid exposure time (AET) were recorded. Also, symptom index (SI) and symptom association probability (SAP) were determined. SI ≥ 50% or SAP ≥ 95% was considered as positive, while SAP < 95% and SI < 50% was labeled as negative12. Additionally, PSPWI and MNBI were determined as described previously13,14.
Group definitions
Patients were classified into three groups according to the Lyon Consensus as follows: (1) conclusive evidence for GERD (conclusive GERD): presence of erosive esophagitis (EE) LA grades C or D, long-segment BE or peptic strictures or AET > 6%; (2) inconclusive or borderline evidence for GERD (inconclusive or borderline GERD): LA grades A or B esophagitis, AET between 4 and 6%, or reflux episodes 40–80. In this group, adjunctive evidence included low MNBI, low PSPWI, reflux episodes > 80, and reflux-symptom association. (3) evidence against pathologic reflux (against GERD): normal endoscopic findings as well as AET < 4% and reflux episodes < 40 on pH-impedance monitoring when patients are off PPIs2. Among these patients, those with normal endoscopic findings, normal AET, negative SAP, and SI in the setting of esophageal symptoms were labeled to have FH, and those with normal endoscopic findings, normal AET, but positive SAP or SI were considered to have RH based on Rome IV criteria15.
Patients were grouped according to GEFV grading as follows: normal GEFV (grades I and II) and abnormal GEFV (grades III and IV)6.
Statistical analysis
The SPSS version 23.0 (SPSS Inc., Chicago, IL, USA) and Prism software version 6.0 (GraphPad Software Inc., San Diego, CA, USA) were used for analysis. Continuous data were expressed as mean ± standard deviation (SD) and compared using either one-way analysis of variance (ANOVA) among the four groups or t-test between two groups if the data were normally distributed. Continuous data with a skewed distribution were reported as median (interquartile range [IQR]) and compared using either Kruskal–Wallis H test among four groups or Mann–Whitney U test between two groups. Qualitative data were reported as numbers (percentages), and the chi-squared test was used to compare them. Spearman's correlation analysis was used to determine the association between MII-pH parameters and GEFV grade, and the association between HRM parameters and GEFV grade. Inter-observer agreement of GEFV grading was evaluated using weighted kappa statistics with linear weights. Logistic regression analysis was used to assess whether sedation was a risk fator for abnormal GEFV, and whether abnormal GEFV was a risk factor for conclusive evidence of GERD. And diagnostic values (accuracy, sensitivity, specificity, and predictive values) of abnormal GEFV to identify patients with conclusive evidence of GERD were calculated. A value of P < 0.05 was considered to be statistically significant.
Results
Patient characteristics and distribution of GEFV grades among patients with conclusive evidence of GERD, inconclusive or borderline evidence of GERD, and evidence against GERD
A total of 320 Chinese patients who satisfied the selection criteria were included. Of these, 80 (25.0%) patients were classified into the conclusive evidence group, 174 (54.4%) patients into the inconclusive or borderline evidence group, and 66 (20.6%) patients into the evidence against pathologic reflux group. Among patients with evidence against pathologic reflux, 19 (28.8%) patients had RH, and 47 (71.2%) patients had FH (Table 1 and Fig. 1). The proportions of male patients and mean body mass index (BMI) were significantly higher in patients with conclusive evidence of GERD than in patients with inconclusive or borderline evidence of GERD and in patients with evidence against pathological reflux (39 [48.8%] vs. 56 [31.5%] and vs. 14 [21.2%]; 24.7 ± 3.4 vs. 23.4 ± 3.7 and vs. 23.3 ± 4.0, respectively; all P < 0.05) (Table 1). The median ages of the three groups were similar.
The weighted kappa coefficient for GEFV grading was 0.921 (95% CI 0.892–0.951) between the two investigators. The upper GI endoscopy was performed in 67 patients under intravenous anesthesia and 253 patients under topical anesthesia. Among the 320 patients, 24 patients had undergone twice EGD examination under intravenous anesthesia and topical anesthesia respectively within 2 years, which were performed by the same endoscopist. Among the 24 patients, the GEFV grading of 2 patients was not consistent between intravenous anesthesia and topical anesthesia (one patient with GEFV I under intravenous anesthesia but with GEFV II under topical anesthesia; the other patient with GEFV II under intravenous anesthesia but with GEFV I under topical anesthesia). The concordance rate of GEFV grading was 91.7% between intravenous anesthesia and topical anesthesia. And sedation was not a risk factor for abnormal GEFV (OR 0.582, 95% CI 0.294–1.152, P = 0.120).
As shown in Table 1, abnormal GEFV (GEFV III + IV) was found in 42.5% of the patients with conclusive evidence of GERD, and among 25.3% of all study patients. The proportion of abnormal GEFV was significantly higher in the conclusive evidence of GERD group than in the inconclusive or borderline evidence of GERD group and in the evidence against GERD group (34 [42.5%] vs. 43 [24.7%] vs. 4 [6.1%]; both P < 0.05). In addition, patients with inconclusive or borderline evidence of GERD had a significantly higher proportion of abnormal GEFV than patients with evidence against GERD (43 [24.7%] vs. 4 [6.1%]; P < 0.05).
Baseline characteristics of different GEFV grades and comparison of demographic findings between abnormal GEFV and normal GEFV groups
As shown in Table 2, the proportion of males increased gradually from GEFV I to GEFV IV (20 [21.3%], 50 [34.5%], 17 [42.5%] and 22 [53.7%], respectively) and it was significantly higher in the abnormal GEFV group than in the normal GEFV group (39 [48.1%] vs. 70 [29.3%], P = 0.002). The median age of the abnormal GEFV group was significantly higher than that of the normal GEFV group (63.0 [51.5–71.5] vs. 60.0 [51.0–66.0], P = 0.031). Also, age showed a positive correlation with GEFV grade (r = 0.178, P = 0.001). The mean BMI was similar between the normal GEFV and abnormal GEFV groups, and it showed no correlation with GEFV grade (r = 0.097, P = 0.084).
Comparison of MII-pH parameters between abnormal GEFV and normal GEFV groups
As shown in Table 2, the abnormal GEFV group had a significantly higher total AET%, upright AET%, and recumbent AET% than the normal GEFV group (4.2 [1.5–7.4] vs. 1.3 [0.3–4.2], 4.9 [1.3–9.4] vs. 1.5 [0.4–5.0], and 1.6 [0.1–5.7] vs. 0.2 [0–1.4], respectively; all P < 0.001). Moreover, MNBI and PSPWI were significantly lower in the abnormal GEFV group than in the normal GEFV group (2068.3 [1658.4–2432.4] Ω vs. 2228.5 [1794.8–2705.3] Ω, P = 0.012; 19.7 [13.9–29.0] % vs. 33.3 [25.0–44.0] %, P < 0.001, respectively). Reflux events and bolus exposures were similar between the abnormal GEFV and normal GEFV groups.
Comparison of HRM findings between abnormal GEFV and normal GEFV groups
The proportion of Type I EGJ morphology gradually decreased from GEFV I to GEFV IV (31 [33.0%] vs. 36 [24.8%] vs. 7 [17.5%] vs. 3 [7.3%], respectively), and it was significantly higher in the normal GEFV group than in the abnormal GEFV group (67 [28.0%] vs. 10 [12.3%], P = 0.011). However, the values for EGJ-CI, EGJP-insp, EGJP-exp, and the proportion of normal esophageal motility were similar between the abnormal GEFV and normal GEFV groups.
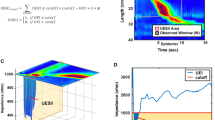
Correlation of GEFV grade with MII-pH and HRM findings
GEFV grade was positively correlated with total AET%, recumbent AET%, and upright AET% (r = 0.318, r = 0.323, and r = 0.303, respectively; all P < 0.001). PSPWI had a negative correlation with GEFV grade (r = − 0.478, p < 0.001). GEFV grade had a weak correlation with MNBI and EGJ morphology (r = − 0.134, P = 0.017; r = 0.172, P = 0.002; respectively) (Fig. 2). There were no significant differences in EGJ-CI, EGJP-insp and EGJP-exp among the different GEFV grades (Fig. 3).
Diagnostic value of abnormal GEFV for conclusive evidence of GERD
Patients with an abnormal GEFV had a significantly greater risk of conclusive evidence of GERD compared to patients with a normal GEFV (OR 3.035, 95% CI 1.758–5.240, P < 0.001) in patients with GERD symptoms. Further, when identifying patients with conclusive evidence of GERD in patients with GERD symptoms, abnormal GEFV had an accuracy of 70.9% (95% CI 66.0–75.8%), sensitivity of 42.5% (95% CI 31.7–53.3%), specificity of 80.4% (95% CI 75.3–85.5%), positive predictive value of 42.0% (95% CI 31.2–52.8%), and negative predictive value of 80.8% (95% CI 75.9–85.7%), respectively.
Discussion
Because of the heterogeneity, there is no simple definition and classification of GERD. Instead, there are many proposed diagnostic classifications for GERD. In one of the most accepted classifications, patients with GERD symptoms are categorized as having an EE or non-erosive reflux disease (NERD)15. The Lyon Consensus was published to classify GERD based on endoscopy, biopsy, ambulatory reflux monitoring, and HRM findings. Moreover, novel parameters such as MNBI and PSPWI were also included2. However, GEFV grading has not yet been included in the Lyon Consensus. Also, there has been no study on the relationship between GEFV grade and the Lyon Consensus classification.
In the present study, we evaluated the association between GEFV grade and patients with GERD symptoms as classified by the Lyon Consensus. An abnormal GEFV was present in 25.3% of all patients with GERD symptoms in our study, which was in line with previous studies showing that the proportion of abnormal GEFV in patients with GERD symptoms ranged from 25.0 to 36.2%7,16,17,18. And the proportion of abnormal GEFV was 42.5% in patients with conclusive evidence of GERD, consistent with previous papers reporting that the percentage of abnormal GEFV in GERD patients was from 34.9 to 52.6%7,16. Further, we demonstrated that an abnormal GEFV was a significant risk factor for conclusive evidence of GERD in patients with GERD symptoms. The specificity of abnormal GEFV for conclusive evidence of GERD was good (80.4%). And a recent meta-analysis showed that the pooled specificity of an abnormal GEFV for the diagnosis of EE in patients with symptomatic GERD was 75.7%19. However, the present study and the previous meta anylysis19 showed that the sensitivity of abnormal GEFV for GERD was low, resulting from the heterogeneity of GERD pathophysiology, which included not only EGJ barrier function but also mucosal integrity, esophageal peristalsis, etc. Our study firstly used abnormal GEFV to detect conclusive evidence of GERD in patients with GERD symptoms as classified by the Lyon Consensus, which proposed stricter criteria for GERD diagnosis to avoid inappropriate use of PPIs.
The Lyon Consensus not only proposed stricter criteria for GERD diagnosis but also included novel metrics on MII-pH and HRM2. Therefore, we further explored the association between GEFV grading and these traditional and novel parameters. In the present study, AET% showed a significant positive correlation with GEFV grade, which was consistent with the findings of previous studies7,17. Kim et al. found that the incidence of distal gastroesophageal reflux was significantly higher in subjects with an abnormal GEFV17. Xie et al. also found that the AET% was lower in patients with GEFV grade I7. In addition, previous studies have shown that GEFV III/IV grades were associated with a higher prevalence of EE and BE17,18,20. The reason could be that the GEFV is a part of the anti-reflux barrier and higher grades of GEFV indicate anatomical disturbance in the EGJ, which increases the risk of reflux7.
The MNBI and the PSPWI were regarded as supportive evidence for the diagnosis of GERD in the Lyon Consensus2. The MNBI reflects the esophageal mucosal integrity, the link to reflux symptoms, alterations in tight junctions, and intercellular space21,22. The PSPW suggests whether primary peristalsis is initiated in the esophagus on stimulation by reflux and evaluates the esophageal chemical clearance14,23. These two parameters have been found to increase the diagnostic yield of MII/pH for GERD, even if the patients are on PPI therapy24,25,26. In addition, abnormal PSPWI and MNBI have been shown to be associated with a satisfactory response to medical treatment for GERD27. Ribolsi et al. showed that pathological AET, absent contractility on HRM, and the presence of type 2 or 3 EGJ significantly correlated with pathological MNBI values3. To the best of our knowledge, there has been no study on the relationship between GEFV grade and MNBI/PSPWI. The current study showed that MNBI and PSPWI were significantly lower in the abnormal GEFV group, and these parameters had significant negative correlations with GEFV grades (from I to IV). Therefore, we believe that abnormal GEFV reflects a poor anti-reflux barrier, which leads to a higher reflux burden and results in a lower MNBI and PSPWI. These results indicate that the GEFV and its grade can serve as supportive evidence for the diagnosis of GERD.
The EGJ plays a crucial role as an anti-reflux barrier. EGJ morphology, which is determined by the spatial separation between CD and LES, is an important determinant of the EGJ barrier function28. EGJ-CI is a novel parameter reflecting a contraction of the EGJ at rest and has shown to be decreased in GERD patients compared with those with functional heartburn11. Xie et al. suggested that the GEFV grade could reflect EGJ morphology on HRM and that EGJ type III correlated with GEFV grade IV, but the GEFV grades had no impact on the EGJ-CI, EGJP-exp, and EGJP-insp. The authors believed that the reason might be that the GEFV was not the only structure contributing to EGJ contractility7. Our study also showed that the type I EGJ morphology was more common in patients with a normal GEFV than in those with an abnormal GEFV. However, the values for EGJ-CI, EGJP-insp, and EGJP-exp were similar between the abnormal GEFV and normal GEFV groups. In addition, GEFV grade had no impact on esophageal body motility.
In the current study, the abnormal GEFV group had a significantly higher proportion of males, consistent with a previous study showing that the male gender was a significant risk factor for abnormal GEFV29. Among patients with GERD symptoms, those in the abnormal GEFV group were significantly older, which was in line with a previous study showing that among patients with laryngopharyngeal reflux, those with an abnormal GEFV were significantly older than those with a normal GEFV30.
The present study showed that inter-observer agreement of GEFV grading was 92.1%, which was consistent with previous studies demonstrating that the rate of agreement of GEFV grading ranged from 80.0 to 92.4%30,31,32. And disagreement was never more than one grade and usually occurred in the classification between GEFV I and II or between GEFV III and IV31. In addition, to our knowledge, there has been no study to evaluate if sedation has effects on GEFV abnormality. In the present study, the concordance rate of GEFV grading was excellent between intravenous anesthesia and topical anesthesia in 24 patients, who had undergone twice EGD examination under intravenous anesthesia and topical anesthesia respectively within 2 years. In addition, the present study showed that sedation was not a risk factor for abnormal GEFV. These findings indicated that sedation might not affect GEFV abnormality. However, further prospective and multi-center studies are needed on this issue.
Of note, due to the heterogeneity of GERD pathophysiology, GEFV grading could not replace but aid MII-pH monitoring, which is considered to be the gold standard for the identification of reflux events2. However, 24 h MII-pH has not been widely available in the clinic due to time consuming, inconvenience and discomfort, and the cost burden2. Our study showed that abnormal GEFV was a significant risk factor for conclusive evidence of GERD. In addition, GEFV grading as a simple and reproducible classification during routine endoscopy was associated with reflux burden and could be a good reflection of EGJ morphology. Moreover, to our knowledge, the present study firstly demonstrated that GEFV grading was correlated with MNBI and PSPWI, which were two novel impedance-detected parameters included in the Lyon Consensus, reflecting mucosal integrity and esophageal peristalsis respectively2. Therefore, GEFV grading might be referred to as supportive evidence of GERD in patients with typical GERD symptoms.
This study has several strengths. First, the number of patients was relatively large, with over 300 patients being evaluated. Second, all patients received endoscopy, 24-h MII-pH monitoring, and HRM. Third, this study was the first to show the association between GEFV grade and the classification of GERD by Lyon Consensus, and the association of GEFV with the MNBI and PSPWI, two novel metrics on MII-pH. However, this study has some limitations. It was a single-center retrospective study, which may be associated with selection bias. In addition, some patients underwent endoscopy after PPI therapy. Thus, there is a possibility of misclassification of the esophagitis on endoscopy.
In summary, an abnormal GEFV was a significant risk factor for conclusive evidence of GERD in patients with GERD symptoms, and patients with an abnormal GEFV had a higher reflux burden, lower MNBI, and lower PSPWI. We recommend that GEFV grading should be determined during endoscopy and can be regarded as supportive evidence for the diagnosis of GERD.
Data availability
The datasets analyzed during the current study are available from the corresponding authors on reasonable request.
References
Dent, J. Barrett’s esophagus: A historical perspective, an update on core practicalities and predictions on future evolutions of management. J. Gastroenterol. Hepatol. 26(Suppl 1), 11–30. https://doi.org/10.1111/j.1440-1746.2010.06535.x (2011).
Gyawali, C. P. et al. Modern diagnosis of GERD: The Lyon Consensus. Gut 67, 1351–1362. https://doi.org/10.1136/gutjnl-2017-314722 (2018).
Ribolsi, M. et al. Correlation between reflux burden, peristaltic function, and mucosal integrity in GERD patients. Neurogastroenterol. Motil. 32, e13752. https://doi.org/10.1111/nmo.13752 (2020).
Frazzoni, M. et al. Impairment of chemical clearance and mucosal integrity distinguishes hypersensitive esophagus from functional heartburn. J. Gastroenterol. 52, 444–451. https://doi.org/10.1007/s00535-016-1226-9 (2016).
Savarino, E. et al. Expert consensus document: Advances in the physiological assessment and diagnosis of GERD. Nat. Rev. Gastroenterol. Hepatol. 14, 665–676. https://doi.org/10.1038/nrgastro.2017.130 (2017).
Hill, L. D. et al. The gastroesophageal flap valve: In vitro and in vivo observations. Gastrointest. Endosc. 44, 541–547. https://doi.org/10.1016/s0016-5107(96)70006-8 (1996).
Xie, C. et al. Gastroesophageal flap valve reflected EGJ morphology and correlated to acid reflux. BMC Gastroenterol. 17, 118. https://doi.org/10.1186/s12876-017-0693-7 (2017).
Lundell, L. R. et al. Endoscopic assessment of oesophagitis: Clinical and functional correlates and further validation of the Los Angeles classification. Gut 45, 172–180. https://doi.org/10.1136/gut.45.2.172 (1999).
Savarino, E. et al. Practice guidelines on the use of esophageal manometry—A GISMAD-SIGE-AIGO medical position statement. Dig. Liver Dis. 48, 1124–1135. https://doi.org/10.1016/j.dld.2016.06.021 (2016).
Kahrilas, P. J. et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol. Motil. 27, 160–174. https://doi.org/10.1111/nmo.12477 (2015).
Nicodème, F., Pipa-Muniz, M., Khanna, K., Kahrilas, P. J. & Pandolfino, J. E. Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-Contractile Integral: Normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol. Motil. 26, 353–360. https://doi.org/10.1111/nmo.12267 (2014).
Bredenoord, A. J., Weusten, B. L. & Smout, A. J. Symptom association analysis in ambulatory gastro-oesophageal reflux monitoring. Gut 54, 1810–1817. https://doi.org/10.1136/gut.2005.072629 (2005).
Patel, A., Wang, D., Sainani, N., Sayuk, G. S. & Gyawali, C. P. Distal mean nocturnal baseline impedance on pH-impedance monitoring predicts reflux burden and symptomatic outcome in gastro-oesophageal reflux disease. Aliment Pharmacol. Ther. 44, 890–898. https://doi.org/10.1111/apt.13777 (2016).
Frazzoni, M. et al. Esophageal chemical clearance is impaired in gastro-esophageal reflux disease–a 24-h impedance-pH monitoring assessment. Neurogastroenterol. Motil. 25, 399–406. https://doi.org/10.1111/nmo.12080 (2013).
Aziz, Q. et al. Functional esophageal disorders. Gastroenterology https://doi.org/10.1053/j.gastro.2016.02.012 (2016).
Quach, D. T., Nguyen, T. T. & Hiyama, T. Abnormal gastroesophageal flap valve is associated with high gastresophageal reflux disease questionnaire score and the severity of gastroesophageal reflux disease in vietnamese patients with upper gastrointestinal symptoms. J. Neurogastroenterol. Motil. 24, 226–232. https://doi.org/10.5056/jnm17088 (2018).
Kim, G. H. et al. Gastroesophageal flap valve is associated with gastroesophageal and gastropharyngeal reflux. J. Gastroenterol. 41, 654–661. https://doi.org/10.1007/s00535-006-1819-9 (2006).
Chang, K. C. et al. Impacts of endoscopic gastroesophageal flap valve grading on pediatric gastroesophageal reflux disease. PLoS ONE 9, e107954. https://doi.org/10.1371/journal.pone.0107954 (2014).
Osman, A., Albashir, M. M., Nandipati, K., Walters, R. W. & Chandra, S. Esophagogastric junction morphology on hill’s classification predicts gastroesophageal reflux with good accuracy and consistency. Dig. Dis. Sci. https://doi.org/10.1007/s10620-020-06146-0 (2020).
Contractor, Q. Q., Akhtar, S. S. & Contractor, T. Q. Endoscopic esophagitis and gastroesophageal flap valve. J. Clin. Gastroenterol. 28, 233–237. https://doi.org/10.1097/00004836-199904000-00009 (1999).
Kandulski, A. et al. Esophageal intraluminal baseline impedance differentiates gastroesophageal reflux disease from functional heartburn. Clin. Gastroenterol. Hepatol. 13, 1075–1081. https://doi.org/10.1016/j.cgh.2014.11.033 (2015).
Zhong, C. et al. Esophageal intraluminal baseline impedance is associated with severity of acid reflux and epithelial structural abnormalities in patients with gastroesophageal reflux disease. J. Gastroenterol. 48, 601–610. https://doi.org/10.1007/s00535-012-0689-6 (2013).
Martinucci, I. et al. Esophageal baseline impedance levels in patients with pathophysiological characteristics of functional heartburn. Neurogastroenterol. Motil. 26, 546–555. https://doi.org/10.1111/nmo.12299 (2014).
Frazzoni, M. et al. Analyses of the post-reflux swallow-induced peristaltic wave index and nocturnal baseline impedance parameters increase the diagnostic yield of impedance-ph monitoring of patients with reflux disease. Clin. Gastroenterol. Hepatol. 14, 40–46. https://doi.org/10.1016/j.cgh.2015.06.026 (2016).
Frazzoni, M. et al. Lack of improvement of impaired chemical clearance characterizes PPI-refractory reflux-related heartburn. Am. J. Gastroenterol. 113, 670–676. https://doi.org/10.1038/s41395-018-0044-5 (2018).
Frazzoni, M. et al. The added diagnostic value of postreflux swallow-induced peristaltic wave index and nocturnal baseline impedance in refractory reflux disease studied with on-therapy impedance-pH monitoring. Neurogastroenterol. Motil. https://doi.org/10.1111/nmo.12947 (2017).
Frazzoni, L. et al. Postreflux swallow-induced peristaltic wave index and nocturnal baseline impedance can link PPI-responsive heartburn to reflux better than acid exposure time. Neurogastroenterol. Motil. https://doi.org/10.1111/nmo.13116 (2017).
Bredenoord, A. J., Weusten, B. L., Timmer, R. & Smout, A. J. Intermittent spatial separation of diaphragm and lower esophageal sphincter favors acidic and weakly acidic reflux. Gastroenterology 130, 334–340. https://doi.org/10.1053/j.gastro.2005.10.053 (2006).
Ko, S. H., Baeg, M. K., Jung, H. S., Kim, P. & Choi, M. G. Russian Caucasians have a higher risk of erosive reflux disease compared with East Asians: A direct endoscopic comparison. Neurogastroenterol. Motil. https://doi.org/10.1111/nmo.13002 (2017).
Wu, W. et al. Reflux finding score is associated with gastroesophageal flap valve status in patients with laryngopharyngeal reflux disease: A retrospective study. Sci. Rep. 9, 15744. https://doi.org/10.1038/s41598-019-52349-5 (2019).
Hill, L. D. & Kozarek, R. A. The gastroesophageal flap valve. J. Clin. Gastroenterol. 28, 194–197. https://doi.org/10.1097/00004836-199904000-00002 (1999).
Fujiwara, Y. et al. Association between gastroesophageal flap valve, reflux esophagitis, Barrett’s epithelium, and atrophic gastritis assessed by endoscopy in Japanese patients. J. Gastroenterol. 38, 533–539. https://doi.org/10.1007/s00535-002-1100-9 (2003).
Funding
This study was supported by the Digestive Medical Coordinated Development Center of Beijing Hospitals Authority (XXT09).
Author information
Authors and Affiliations
Contributions
Z.H.G. and Y.H.W. performed the data collection, analyzed the data, and wrote the manuscript, and both are to be considered as first authors. C.Z. and Y.T.Z. designed the study and provided financial support for this work, and both are to be considered as the corresponding authors. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guo, Z., Wu, Y., Zhan, Y. et al. Correlation between gastroesophageal flap valve abnormality and novel parameters in patients with gastroesophageal reflux disease symptoms by the lyon consensus. Sci Rep 11, 15076 (2021). https://doi.org/10.1038/s41598-021-94149-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-94149-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.