Abstract
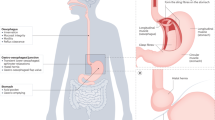
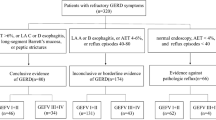
Gastro-oesophageal reflux disease (GERD) is a common disorder in adults and children. The global prevalence of GERD is high and increasing. Non-erosive reflux disease is the most common phenotype of GERD. Heartburn and regurgitation are considered classic symptoms but GERD may present with various atypical and extra-oesophageal manifestations. The pathophysiology of GERD is multifactorial and different mechanisms may result in GERD symptoms, including gastric composition and motility, anti-reflux barrier, refluxate characteristics, clearance mechanisms, mucosal integrity and symptom perception. In clinical practice, the diagnosis of GERD is commonly established on the basis of response to anti-reflux treatment; however, a more accurate diagnosis requires testing that includes upper gastrointestinal tract endoscopy and reflux monitoring. New techniques and new reflux testing parameters help to better phenotype the condition. In children, the diagnosis of GERD is primarily based on history and physical examination and treatment vary with age. Treatment in adults includes a combination of lifestyle modifications with pharmacological, endoscopic or surgical intervention. In refractory GERD, optimization of proton-pump inhibitor treatment should be attempted before a series of diagnostic tests to assess the patient’s phenotype.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Vakil, N., van Zanten, S. V., Kahrilas, P., Dent, J. & Jones, R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am. J. Gastroenterol. 101, 1900–1920 (2006).
Shibli, F., Skeans, J., Yamasaki, T. & Fass, R. Nocturnal gastroesophageal reflux disease (GERD) and sleep: an important relationship that is commonly overlooked. J. Clin. Gastroenterol. 54, 663–674 (2020).
Vaezi, M. F. Chronic cough and gastroesophageal reflux disease: how do we establish a causal link? Chest 143, 587–589 (2013).
Naik, R. D. & Vaezi, M. F. Extra-esophageal gastroesophageal reflux disease and asthma: understanding this interplay. Expert Rev. Gastroenterol. Hepatol. 9, 969–982 (2015).
Fass, R. & Achem, S. R. Noncardiac chest pain: epidemiology, natural course and pathogenesis. J. Neurogastroenterol. Motil. 17, 110–123 (2011).
Mönnikes, H. et al. Evaluation of GERD symptoms during therapy. Part II. Psychometric evaluation and validation of the new questionnaire ReQuest in erosive GERD. Digestion 75, 41–47 (2007).
Heading, R. C. et al. Discrepancies between upper GI symptoms described by those who have them and their identification by conventional medical terminology: a survey of sufferers in four countries. Eur. J. Gastroenterol. Hepatol. 28, 455–462 (2016).
Wiklund, I., Carlsson, J. & Vakil, N. Gastroesophageal reflux symptoms and well-being in a random sample of the general population of a Swedish community. Am. J. Gastroenterol. 101, 18–28 (2006).
Aro, P. et al. Quality of life in a general adult population with gastroesophageal reflux symptoms and/or esophagitis. A report from the Kalixanda study. Gastroenterology 124, A168 (2003).
Shaw, M., Adlis, S. & Beebe, T. When does heartburn become a disease. Gastroenterology 114, G1166 (1998).
Fass, R. & Ofman, J. J. Gastroesophageal reflux disease–should we adopt a new conceptual framework? Am. J. Gastroenterol. 97, 1901–1909 (2002). The first paper that challenged the concept that GERD is a spectrum of disease but rather composed of three unique phenotypes.
Modlin, I. M. et al. Non-erosive reflux disease–defining the entity and delineating the management. Digestion 78, 1–5 (2008).
Modlin, I. M. et al. Diagnosis and management of non-erosive reflux disease–the Vevey NERD Consensus Group. Digestion 80, 74–88 (2009).
Yamasaki, T. & Fass, R. Reflux hypersensitivity: a new functional esophageal disorder. J. Neurogastroenterol. Motil. 23, 495–503 (2017).
Lundell, L. R. et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 45, 172–180 (1999).
Gyawali, C. P. et al. Modern diagnosis of GERD: the lyon consensus. Gut 67, 1351–1362 (2018).
Sharma, P. et al. The development and validation of an endoscopic grading system for Barrett’s esophagus: the Prague C & M criteria. Gastroenterology 131, 1392–1399 (2006).
Fass, R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J. Clin. Gastroenterol. 41, 131–137 (2007).
Hershcovici, T., Jha, L. K. & Fass, R. Comparison of distribution of intraesophageal pH during nighttime recumbency among patients with gastroesophageal reflux disease. J. Clin. Gastroenterol. 46, 562–566 (2012).
Dickman, R. et al. Comparisons of the distribution of oesophageal acid exposure throughout the sleep period among the different gastro-oesophageal reflux disease groups. Aliment. Pharmacol. Ther. 26, 41–48 (2007).
Schey, R. et al. Comparison of the different characteristics of sensed reflux events among different heartburn groups. J. Clin. Gastroenterol. 43, 699–704 (2009).
Shah, A., Shibli, F., Kitayama, Y. & Fass, R. The natural course of gastroesophageal reflux disease: a critical appraisal of the literature. J. Clin. Gastroenterol. 55, 12–20 (2021).
Smout, A. Endoscopy-negative acid reflux disease. Alimentary Pharmacol. Therapeut. 11, 81–85 (1997).
Venables, T. et al. Omeprazole 10 milligrams once daily, omeprazole 20 milligrams once daily, or ranitidine 150 milligrams twice daily, evaluated as initial therapy for the relief of symptoms of gastro-oesophageal reflux disease in general practice. Scand. J. Gastroenterol. 32, 965–973 (1997).
Yi, C.-H., Hu, C.-T. & Chen, C.-L. Sleep dysfunction in patients with GERD: erosive versus nonerosive reflux disease. Am. J. Med. Sci. 334, 168–170 (2007).
Carlsson, R. et al. Gastro-oesophageal reflux disease in primary care: an international study of different treatment strategies with omeprazole. International GORD Study Group. Eur. J. Gastroenterol. Hepatol. 10, 119–124 (1998).
Eusebi, L. H. et al. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut 67, 430–440 (2018). One of the most updated reviews of the global prevalence of GERD.
El-Serag, H. B., Sweet, S., Winchester, C. C. & Dent, J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 63, 871–880 (2014).
Kotzan, J., Wade, W. & Yu, H. H. Assessing NSAID prescription use as a predisposing factor for gastroesophageal reflux disease in a Medicaid population. Pharm. Res. 18, 1367–1372 (2001).
Ruigómez, A. et al. Natural history of gastro-oesophageal reflux disease diagnosed in general practice. Aliment. Pharmacol. Ther. 20, 751–760 (2004).
El-Serag, H. B. et al. Gastroesophageal reflux among different racial groups in the United States. Gastroenterology 126, 1692–1699 (2004).
Boeckxstaens, G., El-Serag, H. B., Smout, A. J. & Kahrilas, P. J. Symptomatic reflux disease: the present, the past and the future. Gut 63, 1185–1193 (2014).
Shiota, S., Singh, S., Anshasi, A. & El-Serag, H. B. Prevalence of Barrett’s esophagus in asian countries: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 13, 1907–1918 (2015).
Lembo, A., Zaman, M., Jones, M. & Talley, N. J. Influence of genetics on irritable bowel syndrome, gastro-oesophageal reflux and dyspepsia: a twin study. Aliment. Pharmacol. Ther. 25, 1343–1350 (2007).
El-Serag, H. B., Satia, J. A. & Rabeneck, L. Dietary intake and the risk of gastro-oesophageal reflux disease: a cross sectional study in volunteers. Gut 54, 11–17 (2005).
Murphy, D. W. & Castell, D. O. Chocolate and heartburn: evidence of increased esophageal acid exposure after chocolate ingestion. Am. J. Gastroenterol. 83, 633–636 (1988).
Nocon, M., Labenz, J. & Willich, S. N. Lifestyle factors and symptoms of gastro-oesophageal reflux – a population-based study. Aliment. Pharmacol. Ther. 23, 169–174 (2006).
Zheng, Z., Nordenstedt, H., Pedersen, N. L., Lagergren, J. & Ye, W. Lifestyle factors and risk for symptomatic gastroesophageal reflux in monozygotic twins. Gastroenterology 132, 87–95 (2007).
Johnson, T., Gerson, L., Hershcovici, T., Stave, C. & Fass, R. Systematic review: the effects of carbonated beverages on gastro-oesophageal reflux disease. Aliment. Pharmacol. Ther. 31, 607–614 (2010).
Piesman, M., Hwang, I., Maydonovitch, C. & Wong, R. K. Nocturnal reflux episodes following the administration of a standardized meal. Does timing matter? Am. J. Gastroenterol. 102, 2128–2134 (2007).
DiSilvestro, R. A., Verbruggen, M. A. & Offutt, E. J. Anti-heartburn effects of a fenugreek fiber product. Phytother. Res. 25, 88–91 (2011).
Kubo, A., Corley, D. A., Jensen, C. D. & Kaur, R. Dietary factors and the risks of oesophageal adenocarcinoma and Barrett’s oesophagus. Nutr. Res. Rev. 23, 230–246 (2010).
Nilsson, M., Johnsen, R., Ye, W., Hveem, K. & Lagergren, J. Lifestyle related risk factors in the aetiology of gastro-oesophageal reflux. Gut 53, 1730–1735 (2004).
Singh, S. et al. Central adiposity is associated with increased risk of esophageal inflammation, metaplasia, and adenocarcinoma: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 11, 1399–1412 (2013).
El-Serag, H. Role of obesity in GORD-related disorders. Gut 57, 281–284 (2008).
El-Serag, H. B. et al. Visceral abdominal obesity measured by CT scan is associated with an increased risk of Barrett’s oesophagus: a case-control study. Gut 63, 220–229 (2014).
Liska, D. et al. Interethnic differences in muscle, liver and abdominal fat partitioning in obese adolescents. PLoS ONE 2, e569 (2007).
Yaghoobi, M., Farrokhyar, F., Yuan, Y. & Hunt, R. H. Is there an increased risk of GERD after Helicobacter pylori eradication?: a meta-analysis. Am. J. Gastroenterol. 105, 1007–1013 (2010). quiz 1006, 1014.
Zhao, Y. et al. The effect of helicobacter pylori eradication in patients with gastroesophageal reflux disease: a meta-analysis of randomized controlled studies. Dig. Dis. 38, 261–268 (2020).
Fischbach, L. A. et al. The association between Barrett’s esophagus and Helicobacter pylori infection: a meta-analysis. Helicobacter 17, 163–175 (2012).
Islami, F. & Kamangar, F. Helicobacter pylori and esophageal cancer risk: a meta-analysis. Cancer Prev. Res. 1, 329–338 (2008).
El-Serag, H. B. et al. Corpus gastritis is protective against reflux oesophagitis. Gut 45, 181–185 (1999).
Fischbach, L. A. et al. Association between Helicobacter pylori and Barrett’s esophagus: a case-control study. Am. J. Gastroenterol. 109, 357–368 (2014).
Havemann, B. D., Henderson, C. A. & El-Serag, H. B. The association between gastro-oesophageal reflux disease and asthma: a systematic review. Gut 56, 1654–1664 (2007).
Hershcovici, T. et al. Systematic review: the relationship between interstitial lung diseases and gastro-oesophageal reflux disease. Aliment. Pharmacol. Ther. 34, 1295–1305 (2011).
Ruhl, C. E., Sonnenberg, A. & Everhart, J. E. Hospitalization with respiratory disease following hiatal hernia and reflux esophagitis in a prospective, population-based study. Ann. Epidemiol. 11, 477–483 (2001).
Chitkara, D. K. et al. Incidence of presentation of common functional gastrointestinal disorders in children from birth to 5 years: a cohort study. Clin. Gastroenterol. Hepatol. 5, 186–191 (2007).
Nelson, S. P., Chen, E. H., Syniar, G. M. & Christoffel, K. K. Prevalence of symptoms of gastroesophageal reflux during infancy. A pediatric practice-based survey. Pediatric Practice Research Group. Arch. Pediatr. Adolesc. Med. 151, 569–572 (1997).
Rosen, R. et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 66, 516–554 (2018).
Orenstein, S. R., Shalaby, T. M. & Cohn, J. F. Reflux symptoms in 100 normal infants: diagnostic validity of the infant gastroesophageal reflux questionnaire. Clin. Pediatr. 35, 607–614 (1996).
Ruigómez, A., Lundborg, P., Johansson, S., Wallander, M. A. & García Rodríguez, L. A. Follow-up of a cohort of children and adolescents with gastro-esophageal reflux disease who were free of reflux esophagitis at initial diagnosis. Scand. J. Gastroenterol. 45, 814–821 (2010).
El-Serag, H. B., Gilger, M., Carter, J., Genta, R. M. & Rabeneck, L. Childhood GERD is a risk factor for GERD in adolescents and young adults. Am. J. Gastroenterol. 99, 806–812 (2004).
Hirschowitz, B. I. A critical analysis, with appropriate controls, of gastric acid and pepsin secretion in clinical esophagitis. Gastroenterology 101, 1149–1158 (1991).
Fletcher, J., Wirz, A., Young, J., Vallance, R. & McColl, K. E. Unbuffered highly acidic gastric juice exists at the gastroesophageal junction after a meal. Gastroenterology 121, 775–783 (2001).
McColl, K. E., Clarke, A. & Seenan, J. Acid pocket, hiatus hernia and acid reflux. Gut 59, 430–431 (2010).
Pandolfino, J. E. et al. Acidity surrounding the squamocolumnar junction in GERD patients: “acid pocket” versus “acid film”. Am. J. Gastroenterol. 102, 2633–2641 (2007).
Clarke, A. T. et al. Severe reflux disease is associated with an enlarged unbuffered proximal gastric acid pocket. Gut 57, 292–297 (2008).
Beaumont, H., Bennink, R. J., de Jong, J. & Boeckxstaens, G. E. The position of the acid pocket as a major risk factor for acidic reflux in healthy subjects and patients with GORD. Gut 59, 441–451 (2010).
Stacher, G. et al. Gastric emptying: a contributory factor in gastro-oesophageal reflux activity? Gut 47, 661–666 (2000).
Penagini, R. et al. Motor function of the proximal stomach and visceral perception in gastro-oesophageal reflux disease. Gut 42, 251–257 (1998).
Zerbib, F. et al. Proximal gastric tone in gastro-oesophageal reflux disease. Eur. J. Gastroenterol. Hepatol. 11, 511–515 (1999).
Dodds, W. J. et al. Mechanisms of gastroesophageal reflux in patients with reflux esophagitis. N. Engl. J. Med. 307, 1547–1552 (1982).
Mittal, R. K., Holloway, R. H., Penagini, R., Blackshaw, L. A. & Dent, J. Transient lower esophageal sphincter relaxation. Gastroenterology 109, 601–610 (1995).
Babaei, A., Bhargava, V., Korsapati, H., Zheng, W. H. & Mittal, R. K. A unique longitudinal muscle contraction pattern associated with transient lower esophageal sphincter relaxation. Gastroenterology 134, 1322–1331 (2008).
Mittal, R. K. & McCallum, R. W. Characteristics and frequency of transient relaxations of the lower esophageal sphincter in patients with reflux esophagitis. Gastroenterology 95, 593–599 (1988).
Sifrim, D. & Holloway, R. Transient lower esophageal sphincter relaxations: how many or how harmful? Am. J. Gastroenterol. 96, 2529–2532 (2001).
Dent, J., Holloway, R. H., Toouli, J. & Dodds, W. J. Mechanisms of lower oesophageal sphincter incompetence in patients with symptomatic gastrooesophageal reflux. Gut 29, 1020–1028 (1988).
Schoeman, M. N., Tippett, M. D., Akkermans, L. M., Dent, J. & Holloway, R. H. Mechanisms of gastroesophageal reflux in ambulant healthy human subjects. Gastroenterology 108, 83–91 (1995).
Penagini, R., Schoeman, M. N., Dent, J., Tippett, M. D. & Holloway, R. H. Motor events underlying gastro-oesophageal reflux in ambulant patients with reflux oesophagitis. Neurogastroenterol. Motil. 8, 131–141 (1996).
Holloway, R. H. & Dent, J. Pathophysiology of gastroesophageal reflux. Lower esophageal sphincter dysfunction in gastroesophageal reflux disease. Gastroenterol. Clin. North Am. 19, 517–535 (1990).
van Herwaarden, M. A., Samsom, M. & Smout, A. J. Excess gastroesophageal reflux in patients with hiatus hernia is caused by mechanisms other than transient LES relaxations. Gastroenterology 119, 1439–1446 (2000).
Kahrilas, P. J., Lin, S., Chen, J. & Manka, M. The effect of hiatus hernia on gastro-oesophageal junction pressure. Gut 44, 476–482 (1999).
Mittal, R. K. & Balaban, D. H. The esophagogastric junction. N. Engl. J. Med. 336, 924–932 (1997).
Sloan, S. & Kahrilas, P. J. Impairment of esophageal emptying with hiatal hernia. Gastroenterology 100, 596–605 (1991).
DeMeester, T. R. et al. Technique, indications, and clinical use of 24 hour esophageal pH monitoring. J. Thorac. Cardiovascular Surg. 79, 656–670 (1980).
Frazzoni, M., De Micheli, E. & Savarino, V. Different patterns of oesophageal acid exposure distinguish complicated reflux disease from either erosive reflux oesophagitis or non-erosive reflux disease. Aliment. Pharmacol. Ther. 18, 1091–1098 (2003).
Bredenoord, A. J., Hemmink, G. J. & Smout, A. J. Relationship between gastro-oesophageal reflux pattern and severity of mucosal damage. Neurogastroenterol. Motil. 21, 807–812 (2009).
Bredenoord, A. J., Weusten, B. L., Curvers, W. L., Timmer, R. & Smout, A. J. Determinants of perception of heartburn and regurgitation. Gut 55, 313–318 (2006).
Savarino, E. et al. Gastro-oesophageal reflux and gastric aspiration in idiopathic pulmonary fibrosis patients. Eur. Respir. J. 42, 1322–1331 (2013).
Sifrim, D. et al. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut 54, 449–454 (2005).
Blondeau, K. et al. Nocturnal weakly acidic reflux promotes aspiration of bile acids in lung transplant recipients. J. Heart Lung Transplant. 28, 141–148 (2009).
Pauwels, A. et al. Gastric emptying and different types of reflux in adult patients with cystic fibrosis. Aliment. Pharmacol. Ther. 34, 799–807 (2011).
Smith, J. A. et al. Acoustic cough-reflux associations in chronic cough: potential triggers and mechanisms. Gastroenterology 139, 754–762 (2010).
Herregods, T. V. K. et al. Determinants of reflux-induced chronic cough. Gut 66, 2057–2062 (2017).
Wenzl, T. G. et al. Association of apnea and nonacid gastroesophageal reflux in infants: Investigations with the intraluminal impedance technique. Pediatr. Pulmonol. 31, 144–149 (2001).
Rosen, R. et al. Higher rate of bronchoalveolar lavage culture positivity in children with nonacid reflux and respiratory disorders. J. Pediatr. 159, 504–506 (2011).
Skopnik, H. et al. Gastroesophageal reflux in infants: evaluation of a new intraluminal impedance technique. J. Pediatr. Gastroenterol. Nutr. 23, 591–598 (1996).
López-Alonso, M. et al. Twenty-four-hour esophageal impedance-pH monitoring in healthy preterm neonates: rate and characteristics of acid, weakly acidic, and weakly alkaline gastroesophageal reflux. Pediatrics 118, e299–e308 (2006).
Vaezi, M. F. & Richter, J. E. Synergism of acid and duodenogastroesophageal reflux in complicated Barrett’s esophagus. Surgery 117, 699–704 (1995).
Pace, F., Sangaletti, O., Pallotta, S., Molteni, P. & Porro, G. B. Biliary reflux and non-acid reflux are two distinct phenomena: a comparison between 24-hour multichannel intraesophageal impedance and bilirubin monitoring. Scand. J. Gastroenterol. 42, 1031–1039 (2007).
Vaezi, M. F. & Richter, J. E. Role of acid and duodenogastroesophageal reflux in gastroesophageal reflux disease. Gastroenterology 111, 1192–1199 (1996).
Siddiqui, A., Rodriguez-Stanley, S., Zubaidi, S. & Miner, P. B. Jr. Esophageal visceral sensitivity to bile salts in patients with functional heartburn and in healthy control subjects. Dig. Dis. Sci. 50, 81–85 (2005).
Farré, R. et al. Short exposure of oesophageal mucosa to bile acids, both in acidic and weakly acidic conditions, can impair mucosal integrity and provoke dilated intercellular spaces. Gut 57, 1366–1374 (2008).
Tack, J., Koek, G., Demedts, I., Sifrim, D. & Janssens, J. Gastroesophageal reflux disease poorly responsive to single-dose proton pump inhibitors in patients without Barrett’s esophagus: acid reflux, bile reflux, or both? Am. J. Gastroenterol. 99, 981–988 (2004).
Gasiorowska, A. et al. Comparison of the degree of duodenogastroesophageal reflux and acid reflux between patients who failed to respond and those who were successfully treated with a proton pump inhibitor once daily. Am. J. Gastroenterol. 104, 2005–2013 (2009).
de Bortoli, N. et al. Bile reflux in patients with nerd is associated with more severe heartburn and lower values of mean nocturnal baseline impedance and chemical clearance. Neurogastroenterol. Motil. 32, e13919 (2020).
Emerenziani, S. et al. Presence of gas in the refluxate enhances reflux perception in non-erosive patients with physiological acid exposure of the oesophagus. Gut 57, 443–447 (2008).
Bredenoord, A. J., Weusten, B. L., Sifrim, D., Timmer, R. & Smout, A. J. Aerophagia, gastric, and supragastric belching: a study using intraluminal electrical impedance monitoring. Gut 53, 1561–1565 (2004).
Hemmink, G. J., Bredenoord, A. J., Weusten, B. L., Timmer, R. & Smout, A. J. Supragastric belching in patients with reflux symptoms. Am. J. Gastroenterol. 104, 1992–1997 (2009).
Koukias, N., Woodland, P., Yazaki, E. & Sifrim, D. Supragastric belching: prevalence and association with gastroesophageal reflux disease and esophageal hypomotility. J. Neurogastroenterol. Motil. 21, 398–403 (2015).
Sifrim, D., Silny,, J., Holloway, R. H. & Janssens, J. J. Patterns of gas and liquid reflux during transient lower oesophageal sphincter relaxation: a study using intraluminal electrical impedance. Gut 44, 47–54 (1999).
Cicala, M. et al. Intra-oesophageal distribution and perception of acid reflux in patients with non-erosive gastro-oesophageal reflux disease. Aliment. Pharmacol. Ther. 18, 605–613 (2003).
Weusten, B. L., Akkermans, L. M., vanBerge-Henegouwen, G. P. & Smout, A. J. Symptom perception in gastroesophageal reflux disease is dependent on spatiotemporal reflux characteristics. Gastroenterology 108, 1739–1744 (1995).
Zerbib, F., Duriez, A., Roman, S., Capdepont, M. & Mion, F. Determinants of gastro-oesophageal reflux perception in patients with persistent symptoms despite proton pump inhibitors. Gut 57, 156–160 (2008).
Rohof, W. O., Bennink, R. J., de Jonge, H. & Boeckxstaens, G. E. Increased proximal reflux in a hypersensitive esophagus might explain symptoms resistant to proton pump inhibitors in patients with gastroesophageal reflux disease. Clin. Gastroenterol. Hepatol. 12, 1647–1655 (2014).
Tipnis, N. A., Rhee, P. L. & Mittal, R. K. Distension during gastroesophageal reflux: effects of acid inhibition and correlation with symptoms. Am. J. Physiol. Gastrointest. Liver Physiol. 293, G469–G474 (2007).
Helm, J. F. et al. Effect of esophageal emptying and saliva on clearance of acid from the esophagus. N. Engl. J. Med. 310, 284–288 (1984).
Richter, J. E. et al. Relationship of radionuclide liquid bolus transport and esophageal manometry. J. Lab. Clin. Med. 109, 217–224 (1987).
Ribolsi, M., Balestrieri, P., Emerenziani, S., Guarino, M. P. & Cicala, M. Weak peristalsis with large breaks is associated with higher acid exposure and delayed reflux clearance in the supine position in GERD patients. Am. J. Gastroenterol. 109, 46–51 (2014).
Roman, S., Lin, Z., Kwiatek, M. A., Pandolfino, J. E. & Kahrilas, P. J. Weak peristalsis in esophageal pressure topography: classification and association with Dysphagia. Am. J. Gastroenterol. 106, 349–356 (2011).
Kahrilas, P. J. et al. Esophageal peristaltic dysfunction in peptic esophagitis. Gastroenterology 91, 897–904 (1986).
Katzka, D. A. Motility abnormalities in gastroesophageal reflux disease. Gastroenterol. Clin. North. Am. 28, 905–915 (1999).
Ang, D., Blondeau, K., Sifrim, D. & Tack, J. The spectrum of motor function abnormalities in gastroesophageal reflux disease and Barrett’s esophagus. Digestion 79, 158–168 (2009).
Schoeman, M. N. & Holloway, R. H. Integrity and characteristics of secondary oesophageal peristalsis in patients with gastro-oesophageal reflux disease. Gut 36, 499–504 (1995).
Mittal, R. K., Lange, R. C. & McCallum, R. W. Identification and mechanism of delayed esophageal acid clearance in subjects with hiatus hernia. Gastroenterology 92, 130–135 (1987).
Shay, S. S., Johnson, L. F. & Richter, J. E. Acid rereflux: a review, emphasizing detection by impedance, manometry, and scintigraphy, and the impact on acid clearing pathophysiology as well as interpreting the pH record. Dig. Dis. Sci. 48, 1–9 (2003).
Dantas, R. O., Oliveira, R. B., Aprile, L. R., Hara, S. H. & Sifrim, D. A. Saliva transport to the distal esophagus. Scand. J. Gastroenterol. 40, 1010–1016 (2005).
Korsten, M. A. et al. Chronic xerostomia increases esophageal acid exposure and is associated with esophageal injury. Am. J. Med. 90, 701–706 (1991).
Chang, C. S., Liao, C. H., Muo, C. H. & Kao, C. H. Increased risk of concurrent gastroesophageal reflux disease among patients with Sjögren’s syndrome: a nationwide population-based study. Eur. J. Intern. Med. 31, 73–78 (2016).
Orr, W. C., Chen, C. L. & Sloan, S. The role of age and salivation in acid clearance in symptomatic patients with gastro-oesophageal reflux disease. Aliment. Pharmacol. Ther. 15, 1385–1388 (2001).
Frazzoni, M. et al. Lack of improvement of impaired chemical clearance characterizes PPI-refractory reflux-related heartburn. Am. J. Gastroenterol. 113, 670–676 (2018).
Frazzoni, L. et al. Postreflux swallow-induced peristaltic wave index and nocturnal baseline impedance can link PPI-responsive heartburn to reflux better than acid exposure time.Neurogastroenterol. Motil. https://doi.org/10.1111/nmo.13116 (2017).
Tobey, N. A., Carson, J. L., Alkiek, R. A. & Orlando, R. C. Dilated intercellular spaces: a morphological feature of acid reflux–damaged human esophageal epithelium. Gastroenterology 111, 1200–1205 (1996).
Souza, R. F. et al. Gastroesophageal reflux might cause esophagitis through a cytokine-mediated mechanism rather than caustic acid injury. Gastroenterology 137, 1776–1784 (2009). The first study to propose that EE is the result of cytokine-mediated inflammation rather than direct mucosal caustic acid injury.
Dunbar, K. B. et al. Association of acute gastroesophageal reflux disease with esophageal histologic changes. JAMA 315, 2104–2112 (2016).
Souza, R. F., Bayeh, L., Spechler, S. J., Tambar, U. K. & Bruick, R. K. A new paradigm for GERD pathogenesis. Not acid injury, but cytokine-mediated inflammation driven by HIF-2α: a potential role for targeting HIF-2α to prevent and treat reflux esophagitis. Curr. Opin. Pharmacol. 37, 93–99 (2017).
Ustaoglu, A. et al. Mucosal pathogenesis in gastro-esophageal reflux disease. Neurogastroenterol. Motil. 32, e14022 (2020).
Bytzer, P., van Zanten, S. V., Mattsson, H. & Wernersson, B. Partial symptom-response to proton pump inhibitors in patients with non-erosive reflux disease or reflux oesophagitis - a post hoc analysis of 5796 patients. Aliment. Pharmacol. Ther. 36, 635–643 (2012).
Calabrese, C. et al. Reversibility of GERD ultrastructural alterations and relief of symptoms after omeprazole treatment. Am. J. Gastroenterol. 100, 537–542 (2005).
Woodland, P., Al-Zinaty, M., Yazaki, E. & Sifrim, D. In vivo evaluation of acid-induced changes in oesophageal mucosa integrity and sensitivity in non-erosive reflux disease. Gut 62, 1256–1261 (2013).
Kessing, B. F. et al. Esophageal acid exposure decreases intraluminal baseline impedance levels. Am. J. Gastroenterol. 106, 2093–2097 (2011).
Wiener, G. J., Richter, J. E., Copper, J. B., Wu, W. C. & Castell, D. O. The symptom index: a clinically important parameter of ambulatory 24-hour esophageal pH monitoring. Am. J. Gastroenterol. 83, 358–361 (1988).
Knowles, C. H. & Aziz, Q. Visceral hypersensitivity in non-erosive reflux disease. Gut 57, 674–683 (2008).
Kollarik, M., Ru, F. & Brozmanova, M. Vagal afferent nerves with the properties of nociceptors. Auton. Neurosci. 153, 12–20 (2010).
Shi, G., Bruley des Varannes, S., Scarpignato, C., Le Rhun, M. & Galmiche, J. P. Reflux related symptoms in patients with normal oesophageal exposure to acid. Gut 37, 457–464 (1995).
Reeh, P. W. & Kress, M. Molecular physiology of proton transduction in nociceptors. Curr. Opin. Pharmacol. 1, 45–51 (2001).
Holzer, P. Acid-sensitive ion channels in gastrointestinal function. Curr. Opin. Pharmacol. 3, 618–625 (2003).
Caterina, M. J. & Julius, D. The vanilloid receptor: a molecular gateway to the pain pathway. Annu. Rev. Neurosci. 24, 487–517 (2001).
Burnstock, G. & Wood, J. N. Purinergic receptors: their role in nociception and primary afferent neurotransmission. Curr. Opin. Neurobiol. 6, 526–532 (1996).
Knowles, C. H. & Aziz, Q. Basic and clinical aspects of gastrointestinal pain. Pain 141, 191–209 (2009).
Kirkup, A. J., Brunsden, A. M. & Grundy, D. Receptors and transmission in the brain-gut axis: potential for novel therapies. I. Receptors on visceral afferents. Am. J. Physiol. Gastrointest. Liver Physiol. 280, G787–G794 (2001).
Sarkar, S. et al. Patients with chest pain and occult gastroesophageal reflux demonstrate visceral pain hypersensitivity which may be partially responsive to acid suppression. Am. J. Gastroenterol. 99, 1998–2006 (2004).
Sarkar, S., Aziz, Q., Woolf, C. J., Hobson, A. R. & Thompson, D. G. Contribution of central sensitisation to the development of non-cardiac chest pain. Lancet 356, 1154–1159 (2000).
Woodland, P. et al. Distinct afferent innervation patterns within the human proximal and distal esophageal mucosa. Am. J. Physiol. Gastrointest. Liver Physiol. 308, G525–G531 (2015).
Nikaki, K. et al. Esophageal mucosal innervation in functional heartburn: closer to healthy asymptomatic subjects than to non-erosive reflux disease patients. Neurogastroenterol. Motil. 31, e13667 (2019).
Woodland, P. et al. Superficial esophageal mucosal afferent nerves may contribute to reflux hypersensitivity in nonerosive reflux disease. Gastroenterology 153, 1230–1239 (2017). A study demonstrating that esophageal hypersensitivity in patients with NERD is the result of sensory afferents that are uniquely situated close to the mucosa.
Sifrim, D. & Zerbib, F. Diagnosis and management of patients with reflux symptoms refractory to proton pump inhibitors. Gut 61, 1340–1354 (2012).
Fass, R. et al. The effect of auditory stress on perception of intraesophageal acid in patients with gastroesophageal reflux disease. Gastroenterology 134, 696–705 (2008).
Kessing, B. F., Bredenoord, A. J., Saleh, C. M. & Smout, A. J. Effects of anxiety and depression in patients with gastroesophageal reflux disease. Clin. Gastroenterol. Hepatol. 13, 1089–1095.e1 (2015).
Schey, R. et al. Sleep deprivation is hyperalgesic in patients with gastroesophageal reflux disease. Gastroenterology 133, 1787–1795 (2007).
Farré, R. et al. Critical role of stress in increased oesophageal mucosa permeability and dilated intercellular spaces. Gut 56, 1191–1197 (2007).
Guadagnoli, L. et al. Esophageal hypervigilance is prevalent across gastroesophageal reflux disease presentations.Neurogastroenterol. Motil. https://doi.org/10.1111/nmo.14081 (2021).
de Bortoli, N. et al. Gastroesophageal reflux disease, functional dyspepsia and irritable bowel syndrome: common overlapping gastrointestinal disorders. Ann. Gastroenterol. 31, 639–648 (2018).
Omari, T. I. et al. Mechanisms of gastroesophageal reflux in healthy premature infants. J. Pediatr. 133, 650–654 (1998).
Omari, T. I. et al. Mechanisms of gastro-oesophageal reflux in preterm and term infants with reflux disease. Gut 51, 475–479 (2002).
Krishnan, U. et al. ESPGHAN-NASPGHAN guidelines for the evaluation and treatment of gastrointestinal and nutritional complications in children with esophageal atresia-tracheoesophageal fistula. J. Pediatr. Gastroenterol. Nutr. 63, 550–570 (2016).
Arcos-Machancoses, J. V. et al. A systematic review with meta-analysis of the prevalence of gastroesophageal reflux in congenital diaphragmatic hernia pediatric survivors. Dis. Esophagus 31, dox158 (2018).
Catalano, P., Di Pace, M. R., Caruso, A. M., Casuccio, A. & De Grazia, E. Gastroesophageal reflux in young children treated for esophageal atresia: evaluation with pH-multichannel intraluminal impedance. J. Pediatr. Gastroenterol. Nutr. 52, 686–690 (2011).
Pedersen, R. N. et al. Esophageal atresia: gastroesophageal functional follow-up in 5-15 year old children. J. Pediatr. Surg. 48, 2487–2495 (2013).
Moayyedi, P., Talley, N. J., Fennerty, M. B. & Vakil, N. Can the clinical history distinguish between organic and functional dyspepsia? JAMA 295, 1566–1576 (2006).
Klauser, A. G., Schindlbeck, N. E. & Müller-Lissner, S. A. Symptoms in gastro-oesophageal reflux disease. Lancet 335, 205–208 (1990).
Moayyedi, P. & Axon, A. T. The usefulness of the likelihood ratio in the diagnosis of dyspepsia and gastroesophageal reflux disease. Am. J. Gastroenterol. 94, 3122–3125 (1999).
Katz, P. O., Gerson, L. B. & Vela, M. F. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am. J. Gastroenterol. 108, 308–328 (2013). The American College of Gastroenterology guidelines for the diagnosis and treatment of GERD.
Muthusamy, V. R. et al. The role of endoscopy in the management of GERD. Gastrointest. Endosc. 81, 1305–1310 (2015).
Johnsson, F., Joelsson, B., Gudmundsson, K. & Greiff, L. Symptoms and endoscopic findings in the diagnosis of gastroesophageal reflux disease. Scand. J. Gastroenterol. 22, 714–718 (1987).
Kahrilas, P. J., Shaheen, N. J. & Vaezi, M. F. American Gastroenterological Association Institute technical review on the management of gastroesophageal reflux disease. Gastroenterology 135, 1392–1413.e1-5 (2008).
Sifrim, D., Castell, D., Dent, J. & Kahrilas, P. J. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut 53, 1024–1031 (2004).
Bredenoord, A. J., Weusten, B. L., Timmer, R., Conchillo, J. M. & Smout, A. J. Addition of esophageal impedance monitoring to pH monitoring increases the yield of symptom association analysis in patients off PPI therapy. Am. J. Gastroenterol. 101, 453–459 (2006).
Savarino, E. et al. The added value of impedance-pH monitoring to Rome III criteria in distinguishing functional heartburn from non-erosive reflux disease. Dig. Liver Dis. 43, 542–547 (2011).
Frazzoni, M. et al. Impedance-pH monitoring for diagnosis of reflux disease: new perspectives. Dig. Dis. Sci. 62, 1881–1889 (2017).
Johnston, B. T., Troshinsky, M. B., Castell, J. A. & Castell, D. O. Comparison of barium radiology with esophageal pH monitoring in the diagnosis of gastroesophageal reflux disease. Am. J. Gastroenterol. 91, 1181–1185 (1996).
Saleh, C. M., Smout, A. J. & Bredenoord, A. J. The diagnosis of gastro-esophageal reflux disease cannot be made with barium esophagograms. Neurogastroenterol. Motil. 27, 195–200 (2015).
Saritas Yuksel, E. et al. Use of direct, endoscopic-guided measurements of mucosal impedance in diagnosis of gastroesophageal reflux disease. Clin. Gastroenterol. Hepatol. 10, 1110–1116 (2012).
Katzka, D. A. et al. Endoscopic mucosal impedance measurements correlate with eosinophilia and dilation of intercellular spaces in patients with eosinophilic esophagitis. Clin. Gastroenterol. Hepatol. 13, 1242–1248.e1 (2015).
Ates, F. et al. Mucosal impedance discriminates GERD from non-GERD conditions. Gastroenterology 148, 334–343 (2015). Mucosal impedance, a new technique for spot assessment of oesophageal mucosal integrity, enables an immediate diagnosis of GERD.
Potluri, S. et al. Comparison of a salivary/sputum pepsin assay with 24-hour esophageal pH monitoring for detection of gastric reflux into the proximal esophagus, oropharynx, and lung. Dig. Dis. Sci. 48, 1813–1817 (2003).
Saritas Yuksel, E. et al. Rapid salivary pepsin test: blinded assessment of test performance in gastroesophageal reflux disease. Laryngoscope 122, 1312–1316 (2012).
Hayat, J. O. et al. Objective detection of esophagopharyngeal reflux in patients with hoarseness and endoscopic signs of laryngeal inflammation. J. Clin. Gastroenterol. 48, 318–327 (2014).
Spyridoulias, A., Lillie, S., Vyas, A. & Fowler, S. J. Detecting laryngopharyngeal reflux in patients with upper airways symptoms: Symptoms, signs or salivary pepsin? Respir. Med. 109, 963–969 (2015).
Sereg-Bahar, M., Jerin, A., Jansa, R., Stabuc, B. & Hocevar-Boltezar, I. Pepsin and bile acids in saliva in patients with laryngopharyngeal reflux - a prospective comparative study. Clin. Otolaryngol. 40, 234–239 (2015).
Kim, T. H., Lee, K. J., Yeo, M., Kim, D. K. & Cho, S. W. Pepsin detection in the sputum/saliva for the diagnosis of gastroesophageal reflux disease in patients with clinically suspected atypical gastroesophageal reflux disease symptoms. Digestion 77, 201–206 (2008).
Ocak, E., Kubat, G. & Yorulmaz, İ. Immunoserologic pepsin detection in the saliva as a non-invasive rapid diagnostic test for laryngopharyngeal reflux. Balk. Med. J. 32, 46–50 (2015).
Yadlapati, R. et al. Abilities of oropharyngeal ph tests and salivary pepsin analysis to discriminate between asymptomatic volunteers and subjects with symptoms of laryngeal irritation. Clin. Gastroenterol. Hepatol. 14, 535–542.e2 (2016).
Lynch, C. R. et al. Effect of acid-suppressive therapy on narrow band imaging findings in gastroesophageal reflux disease: a pilot study. Dis. Esophagus 26, 124–129 (2013).
Arul, P., Vinoth, B., Alexander, T., Phansalkar, M. & Padhi, S. Correlation of narrow band imaging endoscopy and histopathology in the diagnosis of nonerosive reflux disease. Saudi J. Gastroenterol. 21, 330–336 (2015).
Tseng, P. H. et al. Performance of narrow band imaging and magnification endoscopy in the prediction of therapeutic response in patients with gastroesophageal reflux disease. J. Clin. Gastroenterol. 45, 501–506 (2011).
Orenstein, S. R. et al. The spectrum of pediatric eosinophilic esophagitis beyond infancy: a clinical series of 30 children. Am. J. Gastroenterol. 95, 1422–1430 (2000).
Rosen, R. et al. The utility of endoscopy and multichannel intraluminal impedance testing in children with cough and wheezing. Pediatr. Pulmonol. 49, 1090–1096 (2014).
Rosen, R., Lord, C. & Nurko, S. The sensitivity of multichannel intraluminal impedance and the pH probe in the evaluation of gastroesophageal reflux in children. Clin. Gastroenterol. Hepatol. 4, 167–172 (2006).
Jadcherla, S. R. et al. Impact of feeding strategies on the frequency and clearance of acid and nonacid gastroesophageal reflux events in dysphagic neonates. J. Parenter. Enter. Nutr. 36, 449–455 (2012).
Mahoney, L. B., Nurko, S. & Rosen, R. The prevalence of rome IV nonerosive esophageal phenotypes in children. J. Pediatr. 189, 86–91 (2017).
Metheny, N. A. et al. Tracheobronchial aspiration of gastric contents in critically ill tube-fed patients: frequency, outcomes, and risk factors. Crit. care Med. 34, 1007–1015 (2006).
Farhath, S. et al. Pepsin, a reliable marker of gastric aspiration, is frequently detected in tracheal aspirates from premature ventilated neonates: relationship with feeding and methylxanthine therapy. J. Pediatr. Gastroenterol. Nutr. 43, 336–341 (2006).
Rosen, R., Johnston, N., Hart, K., Khatwa, U. & Nurko, S. The presence of pepsin in the lung and its relationship to pathologic gastro-esophageal reflux. Neurogastroenterol. Motil. 24, 129–133 (2012).
Dy, F., Amirault, J., Mitchell, P. D. & Rosen, R. Salivary pepsin lacks sensitivity as a diagnostic tool to evaluate extraesophageal reflux disease. J. Pediatr. 177, 53–58 (2016).
Rosen, R., Fritz, J., Nurko, A., Simon, D. & Nurko, S. Lipid-laden macrophage index is not an indicator of gastroesophageal reflux-related respiratory disease in children. Pediatrics 121, e879–e884 (2008).
Rosen, R., Rodriguez, L. & Nurko, S. Pediatric rumination subtypes: a study using high-resolution esophageal manometry with impedance. Neurogastroenterol. Motil. https://doi.org/10.1111/nmo.12998 (2017).
Singendonk, M. M. J. et al. Objectively diagnosing rumination syndrome in children using esophageal pH-impedance and manometry.Neurogastroenterol. Motil. https://doi.org/10.1111/nmo.12996 (2017).
Kurin, M. & Fass, R. Management of gastroesophageal reflux disease in the elderly patient. Drugs Aging 36, 1073–1081 (2019).
Poh, C. H., Navarro-Rodriguez, T. & Fass, R. Review: treatment of gastroesophageal reflux disease in the elderly. Am. J. Med. 123, 496–501 (2010).
Yadlapati, R. et al. Management options for patients with GERD and persistent symptoms on proton pump inhibitors: recommendations from an expert panel. Am. J. Gastroenterol. 113, 980–986 (2018).
Kaltenbach, T., Crockett, S. & Gerson, L. B. Are lifestyle measures effective in patients with gastroesophageal reflux disease? An evidence-based approach. Arch. Intern. Med. 166, 965–971 (2006).
Jacobson, B. C., Somers, S. C., Fuchs, C. S., Kelly, C. P. & Camargo, C. A. Jr. Body-mass index and symptoms of gastroesophageal reflux in women. N. Engl. J. Med. 354, 2340–2348 (2006).
Singh, M. et al. Weight loss can lead to resolution of gastroesophageal reflux disease symptoms: a prospective intervention trial. Obesity 21, 284–290 (2013).
Kahrilas, P. J., Fennerty, M. B. & Joelsson, B. High- versus standard-dose ranitidine for control of heartburn in poorly responsive acid reflux disease: a prospective, controlled trial. Am. J. Gastroenterol. 94, 92–97 (1999).
Allen, L. et al. Increased oesophageal acid exposure at the beginning of the recumbent period is primarily a recumbent-awake phenomenon. Aliment. Pharmacol. Ther. 32, 787–794 (2010).
Peghini, P. L., Katz, P. O. & Castell, D. O. Ranitidine controls nocturnal gastric acid breakthrough on omeprazole: a controlled study in normal subjects. Gastroenterology 115, 1335–1339 (1998).
Hershcovici, T. & Fass, R. Pharmacological management of GERD: where does it stand now? Trends Pharmacol. Sci. 32, 258–264 (2011).
Weberg, R. & Berstad, A. Symptomatic effect of a low-dose antacid regimen in reflux oesophagitis. Scand. J. Gastroenterol. 24, 401–406 (1989).
Grove, O. et al. Ranitidine and high-dose antacid in reflux oesophagitis. A randomized, placebo-controlled trial. Scand. J. Gastroenterol. 20, 457–461 (1985).
Leiman, D. A. et al. Alginate therapy is effective treatment for GERD symptoms: a systematic review and meta-analysis. Dis. Esophagus 30, 1–9 (2017).
De Ruigh, A., Roman, S., Chen, J., Pandolfino, J. E. & Kahrilas, P. J. Gaviscon Double Action Liquid (antacid & alginate) is more effective than antacid in controlling post-prandial oesophageal acid exposure in GERD patients: a double-blind crossover study. Aliment. Pharmacol. Ther. 40, 531–537 (2014).
Müller, M., Labenz, G., Borkenstein, D. P. & Labenz, J. Alginate on demand as add-on for patients with gastro-oesophageal reflux disease and insufficient PPI effect. Dtsch. Med. Wochenschr. 144, e30–e35 (2019).
Rees, W. D. Mechanisms of gastroduodenal protection by sucralfate. Am. J. Med. 91, 58S–63S (1991).
Simon, B., Ravelli, G. P. & Goffin, H. Sucralfate gel versus placebo in patients with non-erosive gastro-oesophageal reflux disease. Aliment. Pharmacol. Ther. 10, 441–446 (1996).
Wolfe, M. M. & Sachs, G. Acid suppression: optimizing therapy for gastroduodenal ulcer healing, gastroesophageal reflux disease, and stress-related erosive syndrome. Gastroenterology 118, S9–S31 (2000).
Chiba, N., De Gara, C. J., Wilkinson, J. M. & Hunt, R. H. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis. Gastroenterology 112, 1798–1810 (1997).
van Pinxteren, B., Sigterman, K. E., Bonis, P., Lau, J. & Numans, M. E. Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux disease-like symptoms and endoscopy negative reflux disease. Cochrane Database Syst. Rev. 2013, CD002095 (2010).
Donnellan, C., Sharma, N., Preston, C. & Moayyedi, P. Medical treatments for the maintenance therapy of reflux oesophagitis and endoscopic negative reflux disease. Cochrane Database Syst. Rev. 2, CD003245 (2005).
Pappa, K. A. et al. Low-dose ranitidine for the relief of heartburn. Aliment. Pharmacol. Ther. 13, 459–465 (1999).
Pappa, K. A. et al. A double-blind, placebo-controlled study of the efficacy and safety of non-prescription ranitidine 75 mg in the prevention of meal-induced heartburn. Aliment. Pharmacol. Ther. 13, 467–473 (1999).
Horn, J. The proton-pump inhibitors: similarities and differences. Clin. Ther. 22, 266–280 (2000).
Howden, C. W. Appropriate acid suppression in the treatment of acid-related conditions. Pharmacol. Ther. 63, 123–134 (1994).
Vela, M. F. et al. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology 120, 1599–1606 (2001).
Gyawali, C. P. & Fass, R. Management of gastroesophageal reflux disease. Gastroenterology 154, 302–318 (2018). An updated review on diagnosis and management of GERD with emphasis on refractory GERD.
Gralnek, I. M., Dulai, G. S., Fennerty, M. B. & Spiegel, B. M. Esomeprazole versus other proton pump inhibitors in erosive esophagitis: a meta-analysis of randomized clinical trials. Clin. Gastroenterol. Hepatol. 4, 1452–1458 (2006).
Hershcovici, T. & Fass, R. Nonerosive reflux disease (NERD) - an update. J. Neurogastroenterol. Motil. 16, 8–21 (2010).
Dean, B. B., Gano, A. D. Jr., Knight, K., Ofman, J. J. & Fass, R. Effectiveness of proton pump inhibitors in nonerosive reflux disease. Clin. Gastroenterol. Hepatol. 2, 656–664 (2004).
Corley, D. A. Safety and complications of long-term proton pump inhibitor therapy: getting closer to the truth. Gastroenterology 157, 604–607 (2019).
Moayyedi, P. et al. Safety of proton pump inhibitors based on a large, multi-year, randomized trial of patients receiving rivaroxaban or aspirin. Gastroenterology 157, 682–691.e2 (2019). The first prospective trial that assessed the safety of PPIs given to patients over a period of 3 years.
Freedberg, D. E., Kim, L. S. & Yang, Y. X. The risks and benefits of long-term use of proton pump inhibitors: expert review and best practice advice from the American Gastroenterological Association. Gastroenterology 152, 706–715 (2017).
Abdallah, J., George, N., Yamasaki, T., Ganocy, S. & Fass, R. Most patients with gastroesophageal reflux disease who failed proton pump inhibitor therapy also have functional esophageal disorders. Clin. Gastroenterol. Hepatol. 17, 1073–1080.e1 (2019).
Inatomi, N., Matsukawa, J., Sakurai, Y. & Otake, K. Potassium-competitive acid blockers: advanced therapeutic option for acid-related diseases. Pharmacol. Ther. 168, 12–22 (2016).
Scarpignato, C. & Hunt, R. H. The potential role of potassium-competitive acid blockers in the treatment of gastroesophageal reflux disease. Curr. Opin. Gastroenterol. 35, 344–355 (2019).
Beil, W., Hackbarth, I. & Sewing, K. F. Mechanism of gastric antisecretory effect of SCH 28080. Br. J. Pharmacol. 88, 19–23 (1986).
Andersson, K. & Carlsson, E. Potassium-competitive acid blockade: a new therapeutic strategy in acid-related diseases. Pharmacol. Ther. 108, 294–307 (2005).
Xiao, Y. et al. Phase III, randomised, double-blind, multicentre study to evaluate the efficacy and safety of vonoprazan compared with lansoprazole in Asian patients with erosive oesophagitis. Gut 69, 224–230 (2020).
Ashida, K. et al. Randomised clinical trial: a dose-ranging study of vonoprazan, a novel potassium-competitive acid blocker, vs. lansoprazole for the treatment of erosive oesophagitis. Aliment. Pharmacol. Ther. 42, 685–695 (2015).
Ashida, K. et al. Randomised clinical trial: vonoprazan, a novel potassium-competitive acid blocker, vs. lansoprazole for the healing of erosive oesophagitis. Aliment. Pharmacol. Ther. 43, 240–251 (2016).
Ashida, K. et al. Maintenance for healed erosive esophagitis: Phase III comparison of vonoprazan with lansoprazole. World J. Gastroenterol. 24, 1550–1561 (2018).
Kinoshita, Y. et al. Evaluation of the efficacy and safety of vonoprazan in patients with nonerosive gastroesophageal reflux disease: a phase III, randomized, double-blind, placebo-controlled, multicenter study. Curr. Ther. Res. Clin. Exp. 81-82, 1–7 (2016).
Ren, L.-H. et al. Addition of prokinetics to PPI therapy in gastroesophageal reflux disease: a meta-analysis. World J. Gastroenterol. 20, 2412–2419 (2014).
Shibli, F., Kitayama, Y. & Fass, R. Novel therapies for gastroesophageal reflux disease: beyond proton pump inhibitors. Curr. Gastroenterol. Rep. 22, 16 (2020).
Zhang, Q., Lehmann, A., Rigda, R., Dent, J. & Holloway, R. H. Control of transient lower oesophageal sphincter relaxations and reflux by the GABA(B) agonist baclofen in patients with gastro-oesophageal reflux disease. Gut 50, 19–24 (2002).
Araki, H. et al. Combination of proton pump inhibitor and rebamipide, a free radical scavenger, promotes artificial ulcer healing after endoscopic submucosal dissection with dissection size >40mm. J. Clin. Biochem. Nutr. 51, 185–188 (2012).
Savarino, V., Pace, F. & Scarpignato, C. Randomised clinical trial: mucosal protection combined with acid suppression in the treatment of non-erosive reflux disease - efficacy of Esoxx, a hyaluronic acid-chondroitin sulphate based bioadhesive formulation. Aliment. Pharmacol. Ther. 45, 631–642 (2017).
Fass, R. Endoscopic approaches for the treatment of gastroesophageal reflux disease. Gastroenterol. Hepatol. 15, 555–557 (2019).
Maradey-Romero, C., Kale, H. & Fass, R. Nonmedical therapeutic strategies for nonerosive reflux disease. J. Clin. Gastroenterol. 48, 584–589 (2014).
Fass, R., Cahn, F., Scotti, D. J. & Gregory, D. A. Systematic review and meta-analysis of controlled and prospective cohort efficacy studies of endoscopic radiofrequency for treatment of gastroesophageal reflux disease. Surg. Endosc. 31, 4865–4882 (2017).
Sandhu, D. S. & Fass, R. Current trends in the management of gastroesophageal reflux disease. Gut Liver 12, 7–16 (2018).
Testoni, P. A. et al. Transoral incisionless fundoplication with an ultrasonic surgical endostapler for the treatment of gastroesophageal reflux disease: 12-month outcomes. Endoscopy 52, 469–473 (2020).
Lipka, S., Kumar, A. & Richter, J. E. No evidence for efficacy of radiofrequency ablation for treatment of gastroesophageal reflux disease: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 13, 1058–1067.e1 (2015).
Richter, J. E., Kumar, A., Lipka, S., Miladinovic, B. & Velanovich, V. Efficacy of laparoscopic nissen fundoplication vs transoral incisionless fundoplication or proton pump inhibitors in patients with gastroesophageal reflux disease: a systematic review and network meta-analysis. Gastroenterology 154, 1298–1308.e7 (2018). This meta-analysis demonstrates the limited value of endoscopic procedures for GERD, especially in addressing objective clinical endpoints.
Testoni, P. A., Mazzoleni, G. & Testoni, S. G. Transoral incisionless fundoplication for gastro-esophageal reflux disease: Techniques and outcomes. World J. Gastrointest. Pharmacol. Ther. 7, 179–189 (2016).
Witteman, B. P. et al. Randomized controlled trial of transoral incisionless fundoplication vs. proton pump inhibitors for treatment of gastroesophageal reflux disease. Am. J. Gastroenterol. 110, 531–542 (2015).
Zerbib, F. et al. Randomised clinical trial: oesophageal radiofrequency energy delivery versus sham for PPI-refractory heartburn. Aliment. Pharmacol. Ther. 52, 637–645 (2020).
Khan, F., Maradey-Romero, C., Ganocy, S., Frazier, R. & Fass, R. Utilisation of surgical fundoplication for patients with gastro-oesophageal reflux disease in the USA has declined rapidly between 2009 and 2013. Aliment. Pharmacol. Ther. 43, 1124–1131 (2016).
Wang, Y. R., Dempsey, D. T. & Richter, J. E. Trends and perioperative outcomes of inpatient antireflux surgery in the United States, 1993-2006. Dis. Esophagus 24, 215–223 (2011).
Finks, J. F., Wei, Y. & Birkmeyer, J. D. The rise and fall of antireflux surgery in the United States. Surg. Endosc. 20, 1698–1701 (2006).
Morgenthal, C. B., Lin, E., Shane, M. D., Hunter, J. G. & Smith, C. D. Who will fail laparoscopic Nissen fundoplication? Preoperative prediction of long-term outcomes. Surg. Endosc. 21, 1978–1984 (2007).
Frantzides, C. T., Carlson, M. A., Madan, A. K., Stewart, E. T. & Smith, C. Selective use of esophageal manometry and 24-Hour pH monitoring before laparoscopic fundoplication. J. Am. Coll. Surg. 197, 358–363 (2003).
Yang, H. et al. Esophageal manometry and clinical outcome after laparoscopic Nissen fundoplication. J. Gastrointest. Surg. 11, 1126–1133 (2007).
Kahrilas, P. J. Surgical therapy for reflux disease. JAMA 285, 2376–2378 (2001).
Peters, M. J. et al. Meta-analysis of randomized clinical trials comparing open and laparoscopic anti-reflux surgery. Am. J. Gastroenterol. 104, 1548–1561 (2009).
Varin, O., Velstra, B., De Sutter, S. & Ceelen, W. Total vs partial fundoplication in the treatment of gastroesophageal reflux disease: a meta-analysis. Arch. Surg. 144, 273–278 (2009).
Broeders, J. A. et al. Laparoscopic anterior versus posterior fundoplication for gastroesophageal reflux disease: systematic review and meta-analysis of randomized clinical trials. Ann. Surg. 254, 39–47 (2011).
Memon, M. A. et al. Laparoscopic anterior versus posterior fundoplication for gastro-esophageal reflux disease: a meta-analysis and systematic review. World J. Surg. 39, 981–996 (2015).
Lord, R. V. et al. Hiatal hernia, lower esophageal sphincter incompetence, and effectiveness of Nissen fundoplication in the spectrum of gastroesophageal reflux disease. J. Gastrointest. Surg. 13, 602–610 (2009).
Broeders, J. A. et al. Long-term outcome of Nissen fundoplication in non-erosive and erosive gastro-oesophageal reflux disease. Br. J. Surg. 97, 845–852 (2010).
Lundell, L. et al. Continued (5-year) followup of a randomized clinical study comparing antireflux surgery and omeprazole in gastroesophageal reflux disease. J. Am. Coll. Surg. 192, 172–179 (2001).
Galmiche, J. P. et al. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA 305, 1969–1977 (2011).
Garg, S. K. & Gurusamy, K. S. Laparoscopic fundoplication surgery versus medical management for gastro-oesophageal reflux disease (GORD) in adults.Cochrane Database Syst. Rev. 11, CD003243 (2015).
Spechler, S. J. et al. Randomized trial of medical versus surgical treatment for refractory heartburn. N. Engl. J. Med. 381, 1513–1523 (2019). This study demonstrates the value of surgical fundoplication compared with medical therapy in patients with true refractory GERD.
Richter, J. E. Gastroesophageal reflux disease treatment: side effects and complications of fundoplication. Clin. Gastroenterol. Hepatol. 11, 465–471 (2013).
Bonavina, L. et al. Magnetic augmentation of the lower esophageal sphincter: results of a feasibility clinical trial. J. Gastrointest. Surg. 12, 2133–2140 (2008).
Fass, R. Alternative therapeutic approaches to chronic proton pump inhibitor treatment. Clin. Gastroenterol. Hepatol. 10, 338–345 (2012); quiz e339–e340.
Lipham, J. C. et al. The LINX® reflux management system: confirmed safety and efficacy now at 4 years. Surg. Endosc. 26, 2944–2949 (2012).
Ganz, R. A. et al. Esophageal sphincter device for gastroesophageal reflux disease. N. Engl. J. Med. 368, 719–727 (2013).
Guidozzi, N., Wiggins, T., Ahmed, A. R., Hanna, G. B. & Markar, S. R. Laparoscopic magnetic sphincter augmentation versus fundoplication for gastroesophageal reflux disease: systematic review and pooled analysis. Dis. Esophagus 32, doz031 (2019).
Bell, R. et al. Magnetic sphincter augmentation superior to proton pump inhibitors for regurgitation in a 1-year randomized trial. Clin. Gastroenterol. Hepatol. 18, 1736–1743.e2 (2020).
Madalosso, C. A. et al. The impact of gastric bypass on gastroesophageal reflux disease in morbidly obese patients. Ann. Surg. 263, 110–116 (2016).
Kim, M. et al. Minimally invasive Roux-en-Y gastric bypass for fundoplication failure offers excellent gastroesophageal reflux control. Am. Surg. 80, 696–703 (2014).
Varela, J. E., Hinojosa, M. W. & Nguyen, N. T. Laparoscopic fundoplication compared with laparoscopic gastric bypass in morbidly obese patients with gastroesophageal reflux disease. Surg. Obes. Relat. Dis. 5, 139–143 (2009).
Chao, H. C. & Vandenplas, Y. Effect of cereal-thickened formula and upright positioning on regurgitation, gastric emptying, and weight gain in infants with regurgitation. Nutrition 23, 23–28 (2007).
Jung, W. J. et al. The efficacy of the upright position on gastro-esophageal reflux and reflux-related respiratory symptoms in infants with chronic respiratory symptoms. Allergy Asthma Immunol. Res. 4, 17–23 (2012).
Chao, H. C. & Vandenplas, Y. Comparison of the effect of a cornstarch thickened formula and strengthened regular formula on regurgitation, gastric emptying and weight gain in infantile regurgitation. Dis. Esophagus 20, 155–160 (2007).
Wenzl, T. G. et al. Effects of thickened feeding on gastroesophageal reflux in infants: a placebo-controlled crossover study using intraluminal impedance. Pediatrics 111, e355–e359 (2003).
Hron, B. et al. Health outcomes and quality of life indices of children receiving blenderized feeds via enteral tube. J. Pediatr. 211, 139–145.e1 (2019).
Vandenplas, Y. & De Greef, E. Extensive protein hydrolysate formula effectively reduces regurgitation in infants with positive and negative challenge tests for cow’s milk allergy. Acta Paediatr. 103, e243–e250 (2014).
Tolia, V., Gilger, M. A., Barker, P. N. & Illueca, M. Healing of erosive esophagitis and improvement of symptoms of gastroesophageal reflux disease after esomeprazole treatment in children 12 to 36 months old. J. Pediatr. Gastroenterol. Nutr. 51, 593–598 (2010).
Karjoo, M. & Kane, R. Omeprazole treatment of children with peptic esophagitis refractory to ranitidine therapy. Arch. Pediatr. Adolesc. Med. 149, 267–271 (1995).
Cucchiara, S. et al. Omeprazole and high dose ranitidine in the treatment of refractory reflux oesophagitis. Arch. Dis. Child. 69, 655–659 (1993).
Orenstein, S. R., Hassall, E., Furmaga-Jablonska, W., Atkinson, S. & Raanan, M. Multicenter, double-blind, randomized, placebo-controlled trial assessing the efficacy and safety of proton pump inhibitor lansoprazole in infants with symptoms of gastroesophageal reflux disease. J. Pediatr. 154, 514–520.e4 (2009).
Moore, D. J. et al. Double-blind placebo-controlled trial of omeprazole in irritable infants with gastroesophageal reflux. J. Pediatr. 143, 219–223 (2003).
Slaughter, J. L., Stenger, M. R., Reagan, P. B. & Jadcherla, S. R. Neonatal histamine-2 receptor antagonist and proton pump inhibitor treatment at United States Children’s hospitals. J. Pediatr. 174, 63–70 (2016).
Blank, M. L. & Parkin, L. National study of off-label proton pump inhibitor use among New Zealand infants in the first year of life (2005-2012). J. Pediatr. Gastroenterol. Nutr. 65, 179–184 (2017).
Nelson, S. P. et al. Pediatric gastroesophageal reflux disease and acid-related conditions: trends in incidence of diagnosis and acid suppression therapy. J. Med. Econ. 12, 348–355 (2009).
Tolia, V. et al. Multicenter, randomized, double-blind study comparing 10, 20 and 40 mg pantoprazole in children (5-11 years) with symptomatic gastroesophageal reflux disease. J. Pediatr. Gastroenterol. Nutr. 42, 384–391 (2006).
Gold, B. D. et al. Safety and symptom improvement with esomeprazole in adolescents with gastroesophageal reflux disease. J. Pediatr. Gastroenterol. Nutr. 45, 520–529 (2007).
Holbrook, J. T. et al. Lansoprazole for children with poorly controlled asthma: a randomized controlled trial. JAMA 307, 373–381 (2012).
Cucchiara, S. et al. Cimetidine treatment of reflux esophagitis in children: an Italian multicentric study. J. Pediatr. Gastroenterol. Nutr. 8, 150–156 (1989).
Simeone, D., Caria, M. C., Miele, E. & Staiano, A. Treatment of childhood peptic esophagitis: a double-blind placebo-controlled trial of nizatidine. J. Pediatr. Gastroenterol. Nutr. 25, 51–55 (1997).
Rosen, R. et al. 16S community profiling identifies proton pump inhibitor related differences in gastric, lung, and oropharyngeal microflora. J. Pediatr. 166, 917–923 (2015).
Rosen, R. et al. Changes in gastric and lung microflora with acid suppression: acid suppression and bacterial growth. JAMA Pediatr. 168, 932–937 (2014).
Gupta, R. W. et al. Histamine-2 receptor blockers alter the fecal microbiota in premature infants. J. Pediatr. Gastroenterol. Nutr. 56, 397–400 (2013).
Canani, R. B. et al. Therapy with gastric acidity inhibitors increases the risk of acute gastroenteritis and community-acquired pneumonia in children. Pediatrics 117, e817–e820 (2006).
Turco, R. et al. Proton pump inhibitors as a risk factor for paediatric Clostridium difficile infection. Aliment. Pharmacol. Ther. 31, 754–759 (2010).
Lima, J. J. et al. Association of CYP2C19 polymorphisms and lansoprazole-associated respiratory adverse effects in children. J. Pediatr. 163, 686–691 (2013).
Dehlink, E., Yen, E., Leichtner, A. M., Hait, E. J. & Fiebiger, E. First evidence of a possible association between gastric acid suppression during pregnancy and childhood asthma: a population-based register study. Clin. Exp. Allergy 39, 246–253 (2009).
Mitre, E. et al. Association between use of acid-suppressive medications and antibiotics during infancy and allergic diseases in early childhood. JAMA Pediatr. 172, e180315 (2018).
Malchodi, L., Wagner, K., Susi, A., Gorman, G. & Hisle-Gorman, E. Early acid suppression therapy exposure and fracture in young children. Pediatrics 144, e20182625 (2019).
Ng, P. C. Use of oral erythromycin for the treatment of gastrointestinal dysmotility in preterm infants. Neonatology 95, 97–104 (2009).
Ng, S. C., Gomez, J. M., Rajadurai, V. S., Saw, S. M. & Quak, S. H. Establishing enteral feeding in preterm infants with feeding intolerance: a randomized controlled study of low-dose erythromycin. J. Pediatr. Gastroenterol. Nutr. 37, 554–558 (2003).
Kessing, B. F. et al. Prucalopride decreases esophageal acid exposure and accelerates gastric emptying in healthy subjects. Neurogastroenterol. Motil. 26, 1079–1086 (2014).
Ariagno, R. L., Kikkert, M. A., Mirmiran, M., Conrad, C. & Baldwin, R. B. Cisapride decreases gastroesophageal reflux in preterm infants. Pediatrics 107, E58 (2001).
Cohen, R. C., O’Loughlin, E. V., Davidson, G. P., Moore, D. J. & Lawrence, D. M. Cisapride in the control of symptoms in infants with gastroesophageal reflux: A randomized, double-blind, placebo-controlled trial. J. Pediatr. 134, 287–292 (1999).
Lee, S. L., Shabatian, H., Hsu, J. W., Applebaum, H. & Haigh, P. I. Hospital admissions for respiratory symptoms and failure to thrive before and after Nissen fundoplication. J. Pediatr. Surg. 43, 59–63 (2008).
Barnhart, D. C. et al. Effectiveness of fundoplication at the time of gastrostomy in infants with neurological impairment. JAMA Pediatr. 167, 911–918 (2013).
Srivastava, R. et al. Reflux related hospital admissions after fundoplication in children with neurological impairment: retrospective cohort study. BMJ 339, b4411 (2009).
Goldin, A. B., Sawin, R., Seidel, K. D. & Flum, D. R. Do antireflux operations decrease the rate of reflux-related hospitalizations in children? Pediatrics 118, 2326–2333 (2006).
Rosen, R., Hart, K. & Warlaumont, M. Incidence of gastroesophageal reflux during transpyloric feeds. J. Pediatr. Gastroenterol. Nutr. 52, 532–535 (2011).
Srivastava, R. et al. Impact of fundoplication versus gastrojejunal feeding tubes on mortality and in preventing aspiration pneumonia in young children with neurologic impairment who have gastroesophageal reflux disease. Pediatrics 123, 338–345 (2009).
Wiklund, I. Quality of life in patients with gastroesophageal reflux disease. Am. J. Gastroenterol. 96, S46–S53 (2001).
Revicki, D. A., Wood, M., Maton, P. N. & Sorensen, S. The impact of gastroesophageal reflux disease on health-related quality of life. Am. J. Med. 104, 252–258 (1998).
Stewart, A. L., Hays, R. D. & Ware, J. E. Jr. The MOS short-form general health survey. Reliability and validity in a patient population. Med. Care 26, 724–735 (1988).
Gralnek, I. M., Hays, R. D., Kilbourne, A., Naliboff, B. & Mayer, E. A. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology 119, 654–660 (2000).
Sjöland, H. et al. Improvement in quality of life and exercise capacity after coronary bypass surgery. Arch. Intern. Med. 156, 265–271 (1996).
Kulig, M. et al. Quality of life in relation to symptoms in patients with gastro-oesophageal reflux disease–an analysis based on the ProGERD initiative. Aliment. Pharmacol. Ther. 18, 767–776 (2003).
Becher, A. & El-Serag, H. Systematic review: the association between symptomatic response to proton pump inhibitors and health-related quality of life in patients with gastro-oesophageal reflux disease. Aliment. Pharmacol. Ther. 34, 618–627 (2011).
Tack, J., Becher, A., Mulligan, C. & Johnson, D. A. Systematic review: the burden of disruptive gastro-oesophageal reflux disease on health-related quality of life. Aliment. Pharmacol. Ther. 35, 1257–1266 (2012).
Castelijns, P. S. S., Ponten, J. E. H., Vd Poll, M. C. G., Bouvy, N. D. & Smulders, J. F. Quality of life after Nissen fundoplication in patients with gastroesophageal reflux disease: Comparison between long- and short-term follow-up. J. Minim. Access. Surg. 14, 213–220 (2018).
Pilli, S., Jiwane, A. & Krishnan, U. Quality of life in children who have undergone fundoplication surgery for the treatment of gastroesophageal reflux disease: a review of literature. Dis. Esophagus 30, 1–5 (2017).
Kahrilas, P. J. et al. Impact of regurgitation on health-related quality of life in gastro-oesophageal reflux disease before and after short-term potent acid suppression therapy. Gut 63, 720–726 (2014).
Fujiwara, Y., Arakawa, T. & Fass, R. Gastroesophageal reflux disease and sleep disturbances. J. Gastroenterol. 47, 760–769 (2012).
Calleja, J. L., Bixquert, M. & Maldonado, J. Impact of nocturnal heartburn on quality of life, sleep, and productivity: the SINERGE study. Dig. Dis. Sci. 52, 2858–2865 (2007).
Bruley des Varannes, S. et al. Cost and burden of gastroesophageal reflux disease among patients with persistent symptoms despite proton pump inhibitor therapy: an observational study in France. BMC Gastroenterol. 13, 39 (2013).
Bruley des Varannes, S. et al. Gastroesophageal reflux disease: impact on work productivity and daily-life activities of daytime workers. A French cross-sectional study. Dig. Liver Dis. 45, 200–206 (2013).
Wahlqvist, P. et al. Relationship between symptom load of gastro-oesophageal reflux disease and health-related quality of life, work productivity, resource utilization and concomitant diseases: survey of a US cohort. Aliment. Pharmacol. Ther. 27, 960–970 (2008).
Author information
Authors and Affiliations
Contributions
Introduction (R.F.); Epidemiology (H.E.-S. and R.R.); Mechanisms/pathophysiology (D.S. and R.R.); Diagnosis, screening and prevention (M.F.V. and R.R.); Management (R.F. and R.R.); Quality of life (G.E.B.); Outlook (R.F., D.S., M.F.V. and R.R.); Overview of the Primer (R.F.).
Corresponding author
Ethics declarations
Competing interests
R.F. receives adviser/speaker/consultant honoraria from Takeda, Daewoong, Medtronic, Phathom Pharmaceuticals, Neurogastrx, GERDCare, AstraZeneca, Eisai Pharmaceuticals and Johnson & Johnson. M.F.V. receives adviser/speaker/consultant honoraria from Ironwood, Phathom Pharmaceuticals and Diversatek; research funding for M.F.V. is provided by Diversatek. Research funding for D.S. is provided by Reckitt Benckiser, Jinshan Technology and Alfa Sigma. R.R., H.E.-S. and G.E.B. declare no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks S. Bhatia, S. Bor, L. Lundell, E. Savarino and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
FDA requests removal of all ranitidine products (Zantac) from the market: https://www.fda.gov/news-events/press-announcements/fda-requests-removal-all-ranitidine-products-zantac-market
Glossary
- Hiatal hernia
-
The sliding of the upper part of the stomach into the chest through the diaphragmatic hiatus.
- Transient LES relaxations
-
(TLESRs). The sudden relaxation of the lower oesophageal sphincter (LES) that is not preceded by a swallow; a normal gastric venting mechanism that is the most common cause of gastro-oesophageal reflux.
- Bilitec
-
A 24-hour intra-luminal catheter that records the frequency and duration of bile exposure in the oesophagus by using bilirubin as a surrogate marker for bile (currently not available for clinical use).
- Pharyngeal pumping
-
A rhythmic contraction (pumping) of the pharynx in response to the presence of a food bolus.
- Sjögren syndrome
-
An autoimmune inflammatory disorder characterized by xerophthalmia (dry eyes) and xerostomia (dry mouth).
- Angle of His
-
The acute angle created between the cardia at the entrance to the stomach and the oesophagus.
- Gastroparesis
-
A neuromuscular disorder of the stomach that is characterized by delayed solid food emptying in the absence of mechanical obstruction.
- Eosinophilic oesophagitis
-
A chronic immune-antigen-mediated oesophageal disorder, characterized by symptoms related to oesophageal dysfunction and, histologically, by eosinophil-predominant inflammation.
- Pill-induced injury
-
Oesophageal injury due to direct damage to the oesophageal mucosa by a pill.
- pH–impedance monitoring
-
Detection of both acid and non-acid gastro-oesophageal reflux episodes with multichannel intra-oesophageal catheter by measuring intra-luminal changes in pH and impedance.
- Rumination syndrome
-
An effortless regurgitation of undigested or partially digested food from the stomach into the mouth, followed by either re-chewing and re-swallowing or spitting of the regurgitate.
- Breakthrough symptoms
-
Symptoms that occur while the patient is on medical therapy.
- Tachyphylaxis
-
Diminishing biological response to a given drug when it is administered continually.
Rights and permissions
About this article
Cite this article
Fass, R., Boeckxstaens, G.E., El-Serag, H. et al. Gastro-oesophageal reflux disease. Nat Rev Dis Primers 7, 55 (2021). https://doi.org/10.1038/s41572-021-00287-w
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-021-00287-w
This article is cited by
-
Gastroesophageal reflux disease and the risk of respiratory diseases: a Mendelian randomization study
Journal of Translational Medicine (2024)
-
Therapy of Upper Gastrointestinal Symptoms: Experience with a Medical Device Made of Natural Substances
Current Treatment Options in Gastroenterology (2024)
-
Exploration of the causal effects of leukocyte telomere length and four gastrointestinal diseases: a two-sample bidirectional Mendelian randomization study
BMC Gastroenterology (2023)
-
Different dosages of vonoprazan for gastroesophageal reflux disease: study protocol for a pragmatic, crossover-cluster, randomized controlled trial with patient preference arms
Trials (2023)
-
Burden of gastroesophageal reflux disease in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of disease study 2019
BMC Public Health (2023)