Abstract
Resistant hypertension is highly prevalent, and is the form of arterial hypertension that is most difficult to treat. Many patients diagnosed with this disease do not have resistant hypertension, but rather have mismanaged primary hypertension. In many cases blood pressure can be controlled by directly addressing underlying causes such as primary aldosteronism, obstructive sleep apnoea, or excessive neurogenic stimulation. Clinicians should ensure that appropriate blood-pressure measurements are used to diagnose resistant hypertension, explore a variety of drug combinations, and battle clinical inertia. Patients should comply with medication schedules and dietary modifications. Correction of these factors will greatly diminish the prevalence of 'resistant' hypertension and avoid the consequences of a persistently elevated blood pressure in these patients.
Similar content being viewed by others
Introduction
Adequate control of blood pressure in patients with hypertension decreases the incidence of cardiovascular and cerebrovascular events.1 However, many patients are unresponsive to standard antihypertensive care. Resistant hypertension is a clinical problem faced by both primary-care clinicians and specialists, and is defined as a blood pressure (BP) that remains above the target despite the concurrent use of three or more antihypertensive agents of different classes, including one diuretic.2 Large blood volume, related to excessive dietary salt ingestion, frequently characterizes the absence of response to standard therapy.2 The prevalence of resistant hypertension is unknown, but seems to be increasing over time3 and is lower among patients being treated in general medical practice than in those being cared for at specialized clinics.4 Data from the Spanish Ambulatory Blood Pressure Monitoring (ABPM) Registry suggest that 12% of patients with hypertension who are treated and followed up in the primary-care setting have a resistant hypertension.5 Instead of genuinely resistant hypertension, about one-third of these patients are likely to have 'white coat' hypertension, where patients exhibit elevated BP only in a clinical setting. Many conditions are known to predispose patients to resistant hypertension, and contribute to the continued increase in its prevalence (Box 1). Resistant hypertension, especially for prolonged periods, is accompanied by a substantial increase in the overall risk of cardiovascular and renal events, owing to the common coexistence of other risk factors such as obesity (particularly abdominal obesity), left ventricular hypertrophy, reduced estimated glomerular filtration rate, and microalbuminuria.6 Although resistant hypertension is an extreme phenotype,2 few genetic tests are available. Furthermore, the most-relevant predisposing factor can be difficult to identify because of the multiple aetiologies of this condition.2
In this Perspectives article, we examine the main reasons for inadequate BP control and the development of resistant hypertension. We will demonstrate that adequate management of primary hypertension can prevent this condition from becoming 'resistant'.
Inadequate measurement of BP
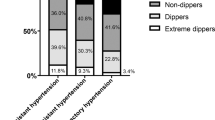
'White coat' hypertension is prevalent among patients diagnosed as having 'resistant' hypertension.2 Data from the Spanish ABPM Registry show that more than one-third of patients diagnosed with resistant hypertension have 'normal' ambulatory BP.5 In addition, up to 31% of patients taking three or more antihypertensive drugs who seem to have well-controlled BP when assessed in a clinical setting have at least one systolic or diastolic BP measurement >130 mmHg or >80 mmHg, respectively, in a 24 h period on ABPM.6 This phenomenon is known as 'masked' hypertension. To reduce the high rate of incorrect diagnosis, patients should perform frequent home BP measurements, and 24 h ABPM should be mandatory in patients with suspected resistant hypertension, helping to rule out the 'white coat' effect and to confirm the diagnosis of resistant hypertension.5
Clinical inertia
Clinical inertia is the failure to initiate or advance therapy for a patient who has not reached the evidence-based BP goal. This phenomenon is amplified by several multifactorial, interactive situations among patients, care providers, and health systems. The major responsibility for clinical inertia should be ascribed to the clinician. Lack of awareness of treatment guidelines (that, when used in team-based systems, can be effective in changing the process and outcomes of care), or reluctance to apply them (owing to lack of training or inexperience with antihypertensive medication), underestimation of cardiovascular risk, and overestimation of the effect of the treatment could all be detrimental to overall patient care.7
In an interesting retrospective study of >8,000 patients with hypertension and diabetes mellitus, Turchin et al. found an inverse relationship between the duration of time since the most-recent board certification of the patient's physician and the frequency of antihypertensive treatment intensification (an important measure of quality of care).8 Another retrospective cohort study in a Midwestern Veterans' Affairs administrative region has shown that intensification of treatment occurred in fewer than one-third of visits in which patients had elevated BP, regardless of whether the patient adherence to medication was good or poor.9
High-quality, continuous training is imperative. Training highlights the importance of treating patients to achieve a BP of <140/90 mmHg, and ensures that clinicians know when to refer patients to a hypertension specialist. Pragmatic, simple, and useful measures, such as keeping a hypertension registry, in which individual BP targets are fixed and recorded, and applying a programme of patient outreach and periodic recall, could be applied in a primary-care setting to reduce clinical inertia.
Poor compliance to medication
According to European10 and American11 guidelines, daily compliance and long-term adherence to therapy are the most-impotantobjectives in the treatment of patients with arterial hypertension. Patients might lack symptoms, poorly understand the disease, have difficulties in accessing medications, or, most importantly, might not adhere to their regimen of medications, all of which can lead to disease progression. Patients with hypertension or hyperlipidaemia tend to take less than half of their prescribed medications.12 These conditions can remain clinically silent for several years and, in the absence of symptoms, patients might feel that medications are not necessary. In addition, patients who lack insight into their illness and its consequences, or those who do not believe that treatment will positively impact their quality of life, are less likely to take their medications.12 Moreover, socioeconomic factors (low income, lack of education, language barriers, or lack of medical insurance) and characteristics of individual patients (depression, social isolation, or cognitive impairment) can place people at increased risk of reduced compliance and poor self-management.12
Improvements to the organization of the health system (ancillary support, and teams of allied health professionals such as nurses or physician assistants), and reinforcing communication strategies can help to improve the quality of care. The quality of interactions between patient and physician is critically important to the overall management of hypertension. Such interactions help to determine patient adherence to treatment recommendations, self care, satisfaction, and health outcomes.12 A meta-analysis of patients with hypertension showed improved patient compliance after simplification of dosing regimens.13 This strategy can be achieved, especially in patients with several comorbidities, by selecting long-acting drugs or drug combinations to reduce the number of pills taken on a daily basis.
Inadequate drug treatment
Pharmacological treatment of arterial hypertension is usually initiated with a combination of two antihypertensive drugs in an attempt to control BP within the first 3 months of therapy.14,15 Nevertheless, resistant hypertension develops in 2% of patients receiving such treatment.16 Early identification of these individuals makes controlling their condition easier. Some of these patients will have resistant hypertension, some merely require a different combination of drugs. Theoretically, if adequate combination therapy is used promptly to treat incident hypertension and numerous drug combinations are tried for patients who don't respond to the first drug combination, patients with resistant hypertension could be identified in less than a year.
A diuretic agent must be considered for every patient with hypertension who requires three or more drugs for BP control.1,2,17 Spironolactone has been shown to be particularly effective in controlling 'resistant' hypertension, probably because patients with this condition frequently have primary hyperaldosteronism (discussed below).18 By controlling aldosterone levels, spironolactone induces rapid reversal of left ventricular hypertrophy and intracardiac volume overload.19 The ASPIRANT trial,20 in which patients with resistant hypertension were specifically examined, documented a significant reduction in systolic BP among patients treated with spironolactone. Moreover, this trial demonstrated that spironolactone at the recommended dose (25–50 mg per day) has a more-pronounced diuretic effect than hydrochlorothiazide, thereby controlling BP (particularly systolic BP) more effectively. Primary aldosteronism should be excluded in patients with resistant hypertension, and the response to spironolactone in many patients suggests that this drug could be used early to treat patients who are unresponsive to three or four antihypertensive agents. For patients who cannot tolerate spironolactone, eplerenone also increases the potassium concentration in a dose-dependent manner (albeit with lower efficacy).21 Spironolactone is more frequently associated with adverse sexual effects: eplerenone shows a lower affinity for progesterone, androgen, and glucocorticoid receptors than spironolactone. The choice of agent should be made on a personalized basis. An alternative to prescribing spironolactone and eplerenone to patients with resistant hypertension is to add a calcium antagonist to a regimen including a renin–angiotensin system blocker, a diuretic, and a calcium-channel blocker; for example, long-acting diltiazem could be added to extended-release nifedipine. This therapeutic scheme has shown additive effects on BP values and has few adverse effects.22
Salt intake and dietary habits
Excessive sodium intake, commonly seen in modern societies, is a modifiable cause of resistant hypertension. Although the impact of a low-sodium diet on cardiovascular morbidity and mortality has been debated, many studies on which calls for the abandonment of low-sodium diet recommendations were based have now been shown to be flawed.23 Systolic and diastolic BP reductions of approximately 5.0 mmHg and 2.7 mmHg, respectively, can be obtained by simply reducing dietary sodium intake by 1.8 g.24 This approach also reduces the incidence of coronary heart disease, stroke, myocardial infarction, and all-cause mortality.25 A randomized trial, in which the effect of salt intake in patients with resistant hypertension was examined, showed a reduction in mean office systolic and diastolic BP of 22.7 mmHg and 9.1 mmHg, respectively, in patients following a low-salt diet.26 Patients should be educated on how to read food labels, and restaurants should provide information about the sodium content of their food. A low-salt diet could be enough to render patients with resistant hypertension responsive to drug treatment.
Resistant hypertension is highly prevalent among patients with obesity or type 2 diabetes.27 High fasting plasma glucose was found to be an independent predictor of the development of resistant hypertension in the ASCOT28 population. To date, however, the direct effect of excessive sugar or fat intake on the development of resistant hypertension has not been explored.
High alcohol intake (>2 units per day) is also related to a progressive increase in BP.29 Racial differences in sensitivity to the effects of alcohol between Asian and white populations should be considered, owing to a delayed oxidation of acetaldehyde by atypical aldehyde dehydrogenase in Asians.30 In future studies, the effects of a low-sodium diet should be tested in patients with resistant hypertension, severe obstructive sleep apnoea (OSA), and hyperaldosteronism.31 OSA and arterial hypertension share common risk factors and mechanisms, and excess salt intake can deteriorate both clinical conditions (Figure 1).
Underlying causes
Primary aldosteronism
Primary aldosteronism, a condition characterized by an excessive release of the hormone aldosterone by the adrenal cortex, can cause hypertension by increasing sodium and water retention and, therefore, must be excluded as part of the diagnosis of resistant hypertension. Primary aldosteronism occurs in 14–21% of patients with hypertension,32 and the symptoms are not specific, making diagnosis difficult. The most-common clinical scenarios in which aldosteronism should be considered include hypertension combined with spontaneous or unprovoked hypokalemia, or the development of severe or persistent hypokalemia despite treatment with low-to-moderate doses of potassium-wasting diuretics. However, approximately one-third to two-thirds of patients with primary aldosteronism are normokalemic.33 Patients frequently report fatigue, muscle weakness, cramps, headaches, and palpitations; polydipsia and polyuria can also coexist.34 In cases where primary aldosteronism is uncertain, the aldosterone:renin ratio should be quantified, bearing in mind that confounding effects can be produced by some antihypertensive drugs. In particular, atenolol can cause a falsely high aldosterone:renin ratio, and irbesartan can cause falsely low values. Amlodipine, doxazosin, and fosinopril can be used in patients while screening for primary aldosteronism.35
Obstructive sleep apnoea
OSA is common among patients with resistant hypertension,36 and this syndrome should be investigated in patients with poorly controlled hypertension who report snoring, witnessed apnoea, or frequent sleepiness during the day. Conversely, in patients with resistant hypertension, the symptoms of OSA are frequently minimized or atypical, and a polysomnographic examination is required to confirm the diagnosis. Aldosterone misregulation might contribute to both high BP and OSA: an intriguing hypothesis is that excess aldosterone, which is common in patients with OSA, might promote accumulation of fluid within the neck, thus increasing upper airway resistance.37 Therapy with continuous positive airway pressure has been shown to moderately lower BP values in small, short-term, randomized trials.38 Resistant hypertension and OSA share common risk factors. Alternatively, OSA may directly contribute to poor BP control through increased sympathetic tone, reduced baroreflex sensitivity, endothelial dysfunction, and impaired ion metabolism.39
Neurogenic hypertension
Ample evidence exists for the involvement of sympathetic nervous system activity in the development of primary hypertension.40 Reduced sensory neuron activity from the kidney to the central nervous system reduces the sympathetic activity to the heart, kidneys, and resistance vessels. The positive effects of renal sympathetic denervation on BP control in patients with hypertension uncontrolled with three or more drugs affirms the increased activity of the sympathetic nervous system as the main cause of resistance to medication.41 However, the effectiveness of drugs that block the sympathetic nervous system on BP control in patients unresponsive to antihypertensive therapy has not been examined.
Conclusions
Many patients initially diagnosed with hypertension are unresponsive to standard therapy owing to a series of extrinsic factors and underlying conditions. Some of these parameters, such as race, age, and sex, are immutable.42 Clinicians and patients need to work together to improve BP control. A correct and reliable evaluation of BP values in various settings (home, office, and ambulatory), fighting the clinical inertia that often characterizes daily practice, and encouraging patient compliance to medical therapy using a multifaceted approach can all improve clinical outcomes. Inadequate drug combinations and suboptimal dosing can lead to ineffective drug use. Managing clinical conditions that promote resistant hypertension, such as obesity and type 2 diabetes, whose prevalence is reaching epidemic proportions worldwide, is likely to require a global effort, with nutritional habits at the centre of health policy, and health workers and governments working together. Addressing these issues can facilitate better management of hypertension that is apparently unresponsive to treatment before classifying patients as having genuine 'resistant' hypertension. Once resistant hypertension has been correctly diagnosed, an accurate therapeutic strategy should include a strongly personalized treatment plan including lifestyle, dietetic, and pharmacological treatment, as well as careful follow-up.
References
Ruilope, L. M. Current challenges in the clinical management of hypertension. Nat. Rev. Cardiol. 9, 267–275 (2012).
Calhoun, D. A. et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 51, 1403–1419 (2008).
Egan, B. M., Zhao, Y., Axon, R. N., Brzezinski, W. A. & Ferdinand, K. C. Uncontrolled and apparent treatment resistant hypertension in the United States, 1998 to 2008. Circulation 124, 1046–1048 (2011).
Pimenta, E. & Calhoun, D. A. Resistant hypertension: incidence, prevalence, and prognosis. Circulation 125, 1594–1596 (2012).
de la Sierra, A. et al. Clinical features of 8,295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension 57, 898–902 (2011).
de la Sierra, A. et al. Clinical differences between resistant hypertensives and patients treated and controlled with three or less drugs. J. Hypertens. 30, 1211–1216 (2012).
Phillips, L. S. & Twombly J. G. It's time to overcome clinical inertia. Ann. Intern. Med. 148, 783–785 (2008).
Turchin, A., Shubina, M., Chodos, A. H., Einbinder, J. S. & Pendergrass, M. L. Effect of board certification on antihypertensive treatment intensification in patients with diabetes mellitus. Circulation 117, 623–628 (2008).
Heisler, M. et al. When more is not better: treatment intensification among hypertensive patients with poor medication adherence. Circulation 117, 2884–2892 (2008).
Mancia, G. et al. 2007 guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 25, 1105–1187 (2007).
Chobanian, A. V. et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Hypertension 42, 1206–1252 (2003).
Viswanathan, M. et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann. Intern. Med. 157, 785–795 (2012).
Schroeder, K., Fahey, T. & Ebrahim, S. How can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch. Intern. Med. 164, 722–732 (2004).
Basile, J. The importance of prompt blood pressure control. J. Clin. Hypertens. (Greenwich) 10 (Suppl. 1), 13–19 (2008).
Berlowitz, D. R. & Franklin, S. The clock is ticking: the case for achieving more rapid control of hypertension. J. Clin. Hypertens. (Greenwich) 12, 323–327 (2010).
Daugherty, S. L. et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation 125, 1635–1642 (2012).
Bobrie, G. et al. Sequential nephron blockade versus sequential renin–angiotensin system blockade in resistant hypertension: a prospective, randomized, open blinded endpoint study. J. Hypertens. 30, 1656–1664 (2012).
Acelajado, M. C. & Calhoun, D. A. Aldosteronism and resistant hypertension. Int. J. Hypertens. http://dx.doi.org/10.4061/2011/837817.
Gaddam, K. et al. Rapid reversal of left ventricular hypertrophy and intracardiac volume overload in patients with resistant hypertension and hyperaldosteronism: a prospective clinical study. Hypertension. 55, 1137–1142 (2010).
Václavík, J. et al. Addition of spironolactone in patients with resistant arterial hypertension (ASPIRANT): a randomized, double-blind, placebo-controlled trial. Hypertension 57, 1069–1075 (2011).
Calhoun, D. A. & White, W. B. Effectiveness of the selective aldosterone antagonist eplerenone in treating resistant hypertension. J. Am. Soc. Hypertens. 2, 462–468 (2008).
Gashti, C. N. & Bakris, G. L. The role of calcium antagonists in chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 13, 155–161 (2004).
Whelton, P. K. et al. Sodium, blood pressure, and cardiovascular disease: further evidence supporting the American Heart Association sodium reduction recommendations. Circulation 126, 2880–2889 (2012).
He, F. J. & MacGregor, G. A. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J. Hum. Hypertens. 16, 761–770 (2002).
Appel, L. J. et al. The importance of population-wide sodium reduction as a means to prevent cardiovascular disease and stroke: a call to action from the American Heart Association. Circulation 123, 1138–1143 (2011).
Pimenta, E. et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension 54, 475–481 (2009).
Sarafidis, P. A. Epidemiology of resistant hypertension. J. Clin. Hypertens. (Greenwich) 13, 523–528 (2011).
Gupta, A. K. et al. Baseline predictors of resistant hypertension in the Anglo-Scandinavian Cardiac Outcome Trial (ASCOT): a risk score to identify those at high-risk. J. Hypertens. 29, 2004–2013 (2011).
Yoshita, K. et al. Relationship of alcohol consumption to 7-year blood pressure change in Japanese men. J. Hypertens. 23, 1485–1490 (2005).
Li, D., Zhao, H. & Gelernter, J. Strong protective effect of the aldehyde dehydrogenase gene (ALDH2) 504lys (*2) allele against alcoholism and alcohol-induced medical diseases in Asians. Hum. Genet. 131, 725–737 (2012).
Pimenta, E. et al. Increased dietary sodium is related to severity of obstructive sleep apnea in patients with resistant hypertension and hyperaldosteronism. Chest http://dx.doi.org/10.1378/chest.12-0802.
Clark, D., Ahmed, M. I. & Calhoun, D. A. Resistant hypertension and aldosterone: an update. Can. J. Cardiol. 28, 318–325 (2012).
Mulatero, P. et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J. Clin. Endocrinol. Metab. 89, 1045–1050 (2004).
Funder, J. et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 9, 3266–3281 (2008).
Mulatero, P. et al. Drug effects on aldosterone/plasma renin activity in primary aldosteronism. Hypertension 40, 897–902 (2002).
Pedrosa, R. P. et al. Obstructive sleep apnea. The most common secondary cause of hypertension associated with resistant hypertension. Hypertension 58, 811–817 (2011).
Dudenbostel, T. & Calhoun, D. A. Resistant hypertension, obstructive sleep apnoea and aldosterone. J. Hum. Hypertens. 26, 281–287 (2012).
Lozano, L. et al. Continuous positive airway pressure treatment in sleep apnea patients with resistant hypertension: a randomized, controlled trial. J. Hypertens. 10, 2161–2168 (2010).
Kohler, M. & Stradling, J. R. Mechanisms of vascular damage in obstructive sleep apnea. Nat. Rev. Cardiol. 7, 677–685 (2010).
Parati, G. & Esler, M. The human sympathetic nervous system: its relevance in hypertension and heart failure. Eur. Heart J. 33, 1058–1066 (2012).
Ruilope, L. M. & Schmieder, R. Current status of renal denervation in resistant hypertension. J. Am. Soc. Hypertens. 6, 414–416 (2012).
Persell, S. D. Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension 57, 1076–1080 (2011).
Author information
Authors and Affiliations
Contributions
Both authors researched the data for the article, provided substantial contributions to discussions of its content, wrote the article, and undertook review and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Solini, A., Ruilope, L. How can resistant hypertension be identified and prevented?. Nat Rev Cardiol 10, 293–296 (2013). https://doi.org/10.1038/nrcardio.2013.23
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2013.23
This article is cited by
-
Sacubitril/valsartan in the treatment of arterial hypertension: an unaccomplished promise?
Hypertension Research (2017)
-
Difficult-to-Control or Resistant Hypertension?
Current Cardiovascular Risk Reports (2013)