Abstract
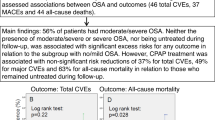
Refractory hypertension (RfH) is defined as a lack of blood pressure control despite the administration of at least 5 anti-hypertensive drugs. The factors associated with its natural history are unknown. This study aimed to evaluate both the incidence of RfH in an cohort of patients with resistant hypertension (RH) and the factors involved in that progression. This was an observational prospective multicenter study (24 centers) with 172 patients with confirmed RH (24-h ABPM) who underwent a further 24 h ABPM study at the end of the follow-up. Prospective information was obtained from all patients in their corresponding Hypertension Units via a standard clinical protocol, and they all underwent a sleep study. Thirty patients were diagnosed with RfH (17.4%) after a mean follow-up of 57 months, despite the prescription of a greater number of long-acting thiazide-like diuretics and mineralocorticoid receptor antagonists. The factors associated with progression to RfH were: a longer period since the diagnosis of RH (OR: 1.06, 95% CI: 1.01–1.1, p = 0.007); the HbA1c concentration (OR: 1.42, 95% CI: 1.42–1.8; p = 0.005); the initial heart rate (OR: 1.05, 95% CI: 1.01–1.09, p = 0.004); and poor adherence to continuous positive airway pressure (CPAP) in cases of obstructive sleep apnea (OR: 3.36, 95% CI: 1.47–7.7, p = 0.004). In conclusion, a considerable percentage of patients evolved from the RH to the RfH phenotype despite changes in their treatment. Some easily measurable variables, such as heart rate, the time since the diagnosis, the HbA1c level, and the presence of untreated obstructive sleep apnea (or poor adherence to CPAP) have been demonstrated to be prognostic factors in the progression to RfH.
Similar content being viewed by others
Introduction
In recent years, there has been a trend toward classifying patients with certain diseases (e.g., cardiovascular diseases) into various subgroups with similar clinical pictures or prognoses to offer them a more personalized treatment. These more homogeneous groups of patients are known as “clinical phenotypes” [1]. Ideally, each of these phenotypes should be associated with a specific endotype, which would support the phenotype’s existence as a consequence of the activation of specific pathophysiological processes [2]. One of the intrinsic characteristics of a clinical phenotype is its capacity to appear alongside several others in a single patient or to change over time as a result of various endogenous or exogenous factors, such as changes in treatment or the emergence of comorbidities [1].
Arterial hypertension is a highly prevalent disease, but it is also very heterogeneous in its characteristics, capacity to be controlled and associations with comorbidities [3]. In this respect, some authors have defended the existence of different clinical phenotypes in hypertensive patients associated with race [4], obesity [5], and the contrast between the blood pressure readings obtained in the office and in an ambulatory context (known as white coat hypertension). In the case of the latter group of patients, for example, the readings can change over time and evolve toward a more constant level [6]. Regarding difficulties in handling hypertension, a clinical phenotype was defined several years ago –hypertension resistant to treatment (RH) – and its diagnosis and management have been established in specific guidelines [7]. Some studies have maintained that this phenotype of RH patients presents a corresponding endotype that confirms its existence, such as the predominant role of the activation of the renin-angiotensin-aldosterone axis and associated fluid retention [8] or functional microvascular damage and inflammation [9] (RH patients present a higher cardiovascular risk than those with nonresistant hypertension [10,11,12,13,14,15]).
In recent years, some authors have defended the existence of a new phenotype of undeniable clinical interest: hypertension refractory to treatment (RfH). This type of hypertension remains uncontrolled despite the ingestion of a minimum of five anti-hypertensive drugs at full doses and with good adherence, of which two are ideally a long-acting thiazide-like diuretic and an antagonist of the mineralocorticoid receptors [16]. There is very little literature on this phenomenon, and so it is still not known whether it is just a more serious manifestation of the RH spectrum or whether it has sufficient weight to be considered a well-differentiated phenotype. The latter hypothesis is supported by the distinctive pathophysiology underlying RfH, as some authors have postulated that the origin of the refractoriness to treatment could be more closely related to the impossibility of controlling sympathetic hyperactivity than to fluid retention (the mechanism most associated with RH) [17, 18]. The real prevalence of RfH is unknown, but it has been estimated that it affects 2–10% of RH patients and less than 1% of hypertensive patients receiving treatment, although the figures vary greatly according to the definition of RfH adopted as a reference (particularly regarding the diagnostic requirement of treatment with a long-acting thiazide-like diuretic and aldosterone antagonist) [16].
Our working hypothesis is based on the fact that a percentage of patients initially evaluated as having an RH phenotype could, over time, evolve to have the RfH phenotype. The characterization of these patients, as well as the risk factors associated with this phenotypic change, would unquestionably be of clinical interest, particularly if these risk factors are potentially preventable or treatable. The main objective of the present study was, therefore, to evaluate, in a cohort of patients initially diagnosed with RH and followed over time, both the incidence of RfH (new diagnoses) and the clinical factors associated with its eventual diagnosis.
Methods
Study design
This was an observational and prospective multicenter study (24 centers) that was a post hoc analysis of the HIPARCO randomized clinical trial [18].
The HIPARCO study and the patients included
Throughout 2012–2013, 266 consecutive patients with a diagnosis of RH were recruited from 24 specialist units in Spain. Patients were included if they had primary RH. All the major causes of RH, including primary aldosteronism, renal artery stenosis, and renal insufficiency (creatinine concentration higher than 1.5 mg/dL), were ruled out in each Hypertension Clinical Unit that participated in the study. Furthermore, patients with poor adherence to antihypertensive treatment, long-term treatment with oral corticosteroids or nonsteroidal anti-inflammatory drugs, or an alcohol intake of more than 100 g per day were excluded. Moreover, good adherence to the antihypertensive treatment was verified during the study by means of the Haynes-Sackett test, which is designed to assess self-reported adherence. Patients were also asked to bring the empty blister packs of their anti-hypertensive pills to check the number of tablets missed per month. All patients underwent a new 24-h ambulatory study to monitor their blood pressure (24-h ABPM) and thus confirm the diagnosis. A substantial number of variables were assessed in all patients, resulting in an excellent baseline characterization [18]. Patients who had their RH confirmed underwent a sleep study (cardio-respiratory polygraphy). Those who also presented moderate-to-severe obstructive sleep apnea (OSA), defined by an apnea-hypopnea index (AHI) ≥ 15 events/hour in the sleep study, were randomized to receive continuous positive airway pressure (CPAP) or not (HIPARCO randomized clinical trial). The objective of the HIPARCO study was to evaluate the effect of CPAP treatment over three months on patients’ blood pressure readings. The characteristics of this study have been published elsewhere [18]. The present study included not only the patients randomized in the HIPARCO study but also those with confirmed RH who were not randomized because they presented an AHI < 15 events/hour. In short, the study included 266 consecutive patients with RH confirmed by 24-h ABPM (with or without apnea). The study adhered to the STROBE guidelines. All patients gave their signed informed consent, and the study was approved by the ethics committees of all participating hospitals. This study conforms to the principles outlined in the Declaration of Helsinki.
Follow-up
All the patients included in the study after confirmation of their RH were followed from their initial characterization (2012–2013) until December 2017. During this follow-up (after the completion of the three months of the HIPARCO randomized clinical study), a pragmatic methodology was introduced to give physicians the freedom, from then on, to prescribe their patients all the diagnostic or therapeutic interventions needed for follow-up and control in the specialist hypertension and sleep units from which they had been referred, following the prevailing guidelines. The physician responsible for each patient was thus able to modify the anti-hypertensive treatment, prescribe or withdraw the CPAP treatment, or take other additional measures during the follow-up.
To obtain an exhaustive record of all the patients’ variables over the course of the follow-up, a standard protocol was used to register clinical and evolutionary data, new cardiovascular events, changes in treatment (particularly in anti-hypertensive drugs), clinical data on OSA and its treatment, and the patient’s vital status during the follow-up and at the end of the study. Upon completion of the follow-up, the centers were asked to perform an additional 24-h ABPM, using the same methodology as in the initial study, although they were allowed to reuse the data from the patient’s most recently completed 24-h ABPM study if less than a year had passed from when it was performed to the endpoint established for the study (December 2017). The starting point for a patient’s follow-up was established as the date of the 24-h ABPM that initially confirmed the diagnosis of RH (2012–2013), while the endpoint of the follow-up was the date of the last 24-h ABPM, whenever available (December 2017). All patients for whom information about the 24 h ABPM was unavailable at the end of the follow-up were excluded from the study. Similarly, those patients who already fulfilled at the onset the criteria for the definition of RfH established via a 24-ABPM were also excluded (treatment with 5 or more antihypertensive drugs and uncontrolled hypertension).
24-h ambulatory blood pressure monitoring (ABPM)
The summarized values from each patient’s 24-h ABPM reports (both at the outset and at the end of the follow-up) were used in the data analysis. ABPM was performed using a Spacelabs 90207 automated noninvasive oscillometric device (Spacelabs Healthcare, Redmond, WA), which was programmed to register BP at 20-min intervals throughout the 24-h period. Data related to the average 24-h, daytime, and nighttime systolic blood pressure (SBP) and diastolic blood pressure (DBP) values were recorded. Some indices of sympathetic tone, such as resting heart rate and variability of BP (as calculated from their coefficient of variation), were explored. The sleeping and waking periods were determined by instructing the patients to record the approximate times when they fell asleep and woke up.
Valid registries had to fulfill a series of pre-established criteria, including ≥80% successful systolic and diastolic BP recordings during the daytime and nighttime periods, 24-h duration, and ≥1 BP measurement per hour [19, 20]. The 24-h ABPM criteria used to define RH in the present study were a blood pressure that remained above the target (i.e., average SBP ≥ 130 mm Hg, average DBP ≥ 80 mm Hg, or both), in spite of the concurrent use of at least three antihypertensive medication agents prescribed at doses that would provide the optimal benefit, with one of those being, ideally, a diuretic (if no contraindication existed), or a blood pressure that remained below the target with the use of more than three antihypertensive drugs (four or more). In contrast, the criteria used to define RfH were a BP that remained uncontrolled (i.e., average SBP ≥ 130 mm Hg, average DBP ≥ 80 mm Hg, or both) despite the concurrent use of five or more antihypertensive drugs.
Statistical analysis
Continuous variables are expressed as the means (SD), while categorical variables are reported as absolute numbers and percentages. The normality of the distributions of variables was tested using the Kolmogorov-Smirnov test. The baseline values of the patients with RH and RfH were compared by means of a t-test or Mann–Whitney U test, depending on the distributions of the quantitative variables. The χ2 test was used to compare dichotomous or qualitative variables. A Cox multivariate analysis was used to evaluate the variables independently associated with the progression from RH at the start of the study to RfH at the end of the follow-up. The variables introduced into the model were those that were demonstrated to be significantly different (p < 0.1) in the comparative study of the two groups (RH and RfH) and those that the researchers considered clinically significant (initial readings of SBD). The appropriate 95% CIs were also calculated. A two-sided p value less than 0.05 was considered significant. Data management and statistical analyses were performed using SPSS predictive analytics software (IBM), version 21.
Results
Of the 266 initial patients, 229 satisfied the criteria for RH (n = 187) or RfH (n = 42) on the first 24-h ABPM at the start of the study. Of those 187 patients with RH, 172 underwent an additional 24-h ABPM at the end of the follow-up (Fig. 1). After a median follow-up of 57 (interquartile interval: 42–72) months, 30 patients who initially satisfied the criteria for RH (17.4%) went on to satisfy those for RfH at the end of the follow-up.
Table 1 shows the baseline characteristics of the patients, divided into those who ended up presenting RfH and those who did not (RH). Patients who progressed to RfH presented the following clinical characteristics: more years since the diagnosis of their RH; a greater number of cardiovascular risk factors, especially a higher initial mean value of HbA1c and a higher percentage of antecedents of dyslipidemia; and a nonsignificant trend to present higher initial readings of 24-h SDB on the 24 h-ABPM; a greater variability between the readings; and a higher mean 24-h baseline heart rate. Finally, regarding OSA, a higher percentage of patients with OSA (IAH ≥ 5 events/hr) who progressed to an RfH phenotype presented intolerance (use of less than 4 h/night on average) or lack of use of CPAP.
During follow-up, no significant changes were observed between the body mass index (BMI) in either the group that progressed to RfH (32.8 [4.5] vs 33.2 [4.6]; p = 0.19) or the group that did not (34.1 [5.1] vs 34.2 [5.2]; p = 0.88).
Table 2 shows the antihypertensive drugs prescribed to the patients at the start of the study. The patients who progressed to RfH also increased the number of antihypertensive drugs they were taking to a greater extent, although this increase only proved statistically significant with respect to thiazide/thiazide-like diuretics and inhibitors of aldosterone receptors (p < 0.05).
Table 3 shows the Cox multivariate analysis, in which it can be seen that the four variables significantly associated with a higher probability of progression to RfH were a greater number of years since the diagnosis of RH, a higher level of HbA1c, a higher mean 24-h heart rate on the initial 24-h ABPM, and the use of CPAP for less than 4 hours per day or a decision not to prescribe CPAP in the case of a previous diagnosis of OSA (IAH ≥ 5). In the end, the variables of variability in blood pressure readings, the presence of dyslipidemia, 24-h SBP and mean 24-h SDP did not enter the model, although dyslipidemia lay on the borderline of statistical significance. The results did not change when patients with antecedents of heart failure (n = 5; 2.2%) or development of this disease during follow-up (n = 6; 2.6%) were excluded from the analysis.
Discussion
According to our results, 17.4% of the patients with RH under treatment at the start of the study evolved toward an RfH clinical phenotype after 5 years of follow-up. The factors associated with this evolution were a greater number of years since the diagnosis of RH at the start of the follow-up, a higher level of baseline HbA1c, a higher mean 24-h heart rate on the initial 24-h ABPM and the use of less than 4 h of CPAP, in the case of it being required due to a prior diagnosis of OSA, or a decision not to treat a patient with OSA with CPAP.
In recent years, there has been a particular interest in characterizing the subgroup of RH patients who seem to present a higher cardiovascular risk, i.e., patients with RfH. However, very few studies have been devoted to this subject to date. In one previous study [21], our working group demonstrated that the prevalence of OSA was extraordinarily high in RfH patients (even higher than in RH patients), and it has been hypothesized that the heightened participation of the activation of the sympathetic system in its genesis could be one of the causes, as it has been proven that OSA is a trigger of hypertension via the activation of the very same pathophysiological route. It has also been shown that CPAP can attenuate this sympathetic hyperactivity and thus bring down blood pressure, as has also been demonstrated in another recently published study [22]. These findings could explain the results of the present study regarding the relationship observed between a lack of adherence to CPAP (less than 4 hours per night on average) or a failure to prescribe this treatment for patients with OSA and a greater probability of progression to RfH, independent of other variables, including changes in the antihypertensive treatment and the changes observed in the BMI.
The hypothesis regarding the participation of the sympathetic pathophysiological route in the genesis of RfH (as opposed to RH) is further endorsed by the fact that those patients with a higher initial mean 24-h heart rate also presented a greater probability of progressing over time to an RfH phenotype. Data derived from previous studies have also shown that patients with RfH presented a higher baseline heart rate than those with RH, both in the office and on 24-h ABPM [17], although there has been no assessment so far of the possible prognostic value of this variable over the course of a follow-up period with respect to the eventual presentation of the RfH phenotype in subjects initially diagnosed with RH. Although heart rate is very variable and susceptible to influence from many factors not analyzed in the present study and the administration of antihypertensive drugs such as beta-blockers (although no significant differences were observed between the compared groups with regard to the use of beta-blockers), it is also the case that a higher heart rate at the start of the study in those patients who later went on to present RfH may indicate that they already presented the pathophysiological profile of RfH, as yet undiagnosed, or that they initially failed to satisfy all the conditions for the manifestation of RfH (but would go on to receive additional medication during the follow-up). The latter situation would be supported by another variable that was also associated with a greater probability of ending up with the refractory phenotype: a greater number of years since the initial diagnosis of RH. Our results with respect to the evolution period for hypertension concur with those published by other authors [23].
Another variable characteristic of the subjects who ended up developing RfH was worse control of diabetes, as reflected in a higher mean level of HbA1c (7 ± 1.8 in patients with RfH vs 6.1 ± 0.95 in patients with RH). Other studies that have used similar criteria to define RfH have reported a higher degree of comorbidity in RfH patients than in RH patients and, more specifically, a higher prevalence of diabetes associated with RfH [23, 24]. Diabetes, as a factor that contributes to increased sympathetic activation [25], could further the development of a hypertensive phenotype in which this pathophysiological mechanism could play a dominant role, as seems to be the case with RfH.
There is a clear relationship between the severity of arterial hypertension and the degree of sympathetic activation [26]. The subjects with RH who ended up expressing an RfH phenotype presented a higher initial SBP (borderline statistical significance). This could mean that these subjects already had a greater degree of sympathetic activity and that some of them may truly have been suffering from RfH that had not yet manifested or had not been diagnosed, due to a lack of the follow-up time that would bring with it an increase in the number of prescribed anti-hypertensive drugs.
The main strength of our study is that it is the first in the literature to evaluate the factors associated with the eventual progression of RH to RfH with a large and well-characterized series of patients followed for a median of 5 years. Furthermore, all patients were diagnosed and followed via 24-h ABPM to confirm the diagnosis of RH and RfH and avoid confounders such as the white-coat effect, which is very common in RH patients [15, 27].
Our study does, however, also have a number of limitations. First, we have shown that poor adherence to CPAP treatment was associated with a progression from RH to RfH over time in our series, but this does not necessarily indicate a cause-effect relationship. Second, we are not using the most commonly accepted definition of RfH because, since its first description by Acelajado et al [28]., the definition has evolved, and at the time when the original HIPARCO study was performed, the strictest definition had still not been established [29]. Third, we do not know whether, in the course of the follow-up, the patients encountered any circumstances not covered by the data collection protocols that could have contributed to their progression to RfH (changes in diet or salt consumption, changes in adherence to antihypertensive treatment, unrecorded ingestion of drugs that could destabilize their blood pressure readings, unreported or unrecognized comorbidities, etc.). No intermediate 24-h ABPA studies were performed over the course of the 5 years of follow-up. Fourth, our study does not enable us to elucidate any causal relationship that could explain the evolution from RH to RfH, rather merely listing the clinical factors associated with this phenomenon. It is therefore impossible to know whether the progression to RfH was merely the natural evolution of RH patients or whether they had undiagnosed RfH from the start. Finally, at the start of the study, the definition of RfH used as a reference did not necessarily include the ingestion of thiazide-like diuretics or aldosterone inhibitors (although there was a trend toward a greater use of these drugs over time).
In conclusion, in our series, we observed that a considerable percentage of patients with RH evolved over time to have the more severe RfH phenotype and that the variables independently associated with this change were: a longer period since the diagnosis of RH; a higher concentration of HbA1c; a higher mean heart rate on the initial 24-h ABPM, and a lack of adherence to or prescription of CPAP in those patients with OSA. These results could be of interest to health professionals who manage such patients, as they could contribute to an earlier identification of those patients susceptible to progressing to RfH (through anticipatory measures such as close monitoring of diabetes, a sleep study for all patients, and CPAP treatment whenever necessary), over and above any required changes in lifestyle or medication.
References
Han MK, Agusti A, Calverley PM, Celli BR, Criner G, Curtis JL, et al. Chronic obstructive pulmonary disease phenotypes. The future of COPD. Am J Respir Crit Care Med. 2010;182:598–604.
Agusti A, Celli B, Faner R. What does endotyping mean for treatment in chronic obstructive pulmonary disease? Lancet. 2017;390:980–7.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the management of arterial hypertension. J Hypertens. 2018;2018(36):2284–309.
Spence JD, Rayner BL. Hypertension in Blacks: individualized therapy based on renin/aldosterone phenotyping. Hypertension. 2018;72:263–9.
Mirzababaei A, Mozaffari H, Shab-Bidar S, Milajerdi A, Djafarian K Risk of hypertension among different metabolic phenotypes: a systematic review and meta-analysis of prospective cohort studies. J Hum Hypertens. 2018. https://doi.org/10.1038/s41371-018-0146-y.
Mancia G, Bombelli M, Facchetti R, Madotto F, Quarti-Trevano F, Polo Friz H, et al. Long-term risk of sustained hypertension in white-coat or masked hypertension. Hypertension. 2009;54:226–32.
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation and treatment: a scientific statement from the American Heart Association professional education committee of the council for high blood pressure research. Hypertension. 2008;51:1403–19.
Gaddam K, Nishizaka M, Pratt-Ubunama M, Pimenta E, Aban I, Oparil S, et al. Resistant hypertension characterized by increased aldosterone levels and persistent intravascular volume expansion. Arch Intern Med. 2008;168:1159–64.
Junqueira CLC, Magalhães MEC, Brandão AA, Ferreira E, FZGA Cyrino, Maranhão PA, et al. Microcirculation and biomarkers in patients with resistant or mild-to-moderate hypertension: a cross-sectional study. Hypertens Res. 2018;41:515–23.
Kumbhani DJ, Steg PG, Cannon CP, Eagle KA, Smith SC Jr, Crowley K, et al. Resistant hypertension: a frequent and ominous finding among hypertensive patients with atherothrombosis; REACH Registry Investigators. Eur Heart J. 2013;34:1204–14.
Pierdomenico SD, Lapenna D, Bucci A, Di Tommaso R, Di Mascio R, Manente BM, et al. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens. 2005;18:1422–8.
Sim JJ, Bhandari SK, Shi J, Reynolds K, Calhoun DA, Kalantar-Zadeh K, et al. Comparative risk of renal, cardiovascular, and mortality outcomes in controlled, uncontrolled resistant, and non-resistant hypertension. Kidney Int. 2015;88:622–32.
Persell SD. Epidemiology/population studies prevalence of resistant hypertension in the United States, 2003–2008. Hypertension. 2011;57:1076–80.
Egan BM, Zaho Y, Axon RN, Brezinsky WA, Ferdinand KC. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988–2008. Circulation. 2011;124:1046–58.
de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P, et al. Clinical features of 8295 patients with resistant hypertension clasified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011;57:898–902.
Dudenbostel T, Siddiqui M, Oparil S, Calhoun DA. Refractory hypertension: a novel phenotype of antihypertensive treatment failure. Hypertension. 2016;67:1085–92.
Dudenbostel T, Acelajado MC, Pisoni R, Li P, Oparil S, Calhoun DA. Refractory hypertension: evidence of heightened sympathetic activity as a cause of antihypertensive treatment failure. Hypertension. 2015;66:126–33.
Martínez-García MA, Capote F, Campos-Rodríguez F, Lloberes P, Díaz de Atauri MJ, Somoza M, et al. Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension. The HIPARCO randomized clinical trial. J Am Med Assoc. 2013;310:2407–15.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
Martínez-García MA, Navarro-Soriano C, Torres G, Barbé F, Caballero-Eraso C, Lloberes P, et al. Beyond resistant hypertension. Relationship between refractory hypertension and obstructive sleep apnea. Hypertension. 2018;72:618–24.
Navarro-Soriano C, Martinez-Garcia MA, Torres G, Barbé F, Caballero C, Lloberes P, et al. Effect of continuous positive airway pressure in patients with true refractory hypertension and sleep apnea. A post-hoc intention-to-treat analysis of the HIPARCO randomized clinical trial. J Hypertens. 2019. https://doi.org/10.1097/HJH.0000000000002053.
Armario P, Calhoun DA, Oliveras A, Blanch P, Vinyoles E, Banega JR, et al. Prevalence and clinical characteristics of refractory hypertension. J Am Heart Assoc. 2017;6:e007365. https://doi.org/10.1161/JAHA.117.007365
Calhoun DA, Booth JN III, Oparil S, Irvin MR, Shimbo D, Lackland DT, et al. Refractory hypertension: determination of prevalence, risk factors, and comorbidities in a large, population-based cohort. Hypertension . 2014;63:451–8.
Huggett RJ, Scott EM, Gilbey SG, Stoker JB, Mackintosh AF, Mary DA. Impact of type 2 diabetes mellitus on sympathetic neural mechanisms in hypertension. Circulation. 2003;108:3097–101.
Mancia G, Grassi G. The autonomic nervous system and hypertension. Circ Res. 2014;23(114):1804–14.
Persu A, O´Brien E, Verdecchia P. Use of ambulatory Blood pressure measurement in the definition of resistant hypertension. A review of the evidence. Hypertens Res. 2014;37:967–72.
Acelajado MC, Pisoni R, Dudenbostel T, Dell’Italia LJ, Cartmill F, Zhang B, et al. Refractory hypertension: definition, prevalence, and patient characteristics. J Clin Hypertens. 2012;14:7–12.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. ACC /AHA /AAPA /ABC /ACPM /AGS /APhA /ASH /ASPC /NMA /PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension . 2018;71(6):e13–e115.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All authors had access to the data and a role in writing the manuscript.
Rights and permissions
About this article
Cite this article
Navarro-Soriano, C., Martínez-García, MA., Torres, G. et al. Factors associated with the changes from a resistant to a refractory phenotype in hypertensive patients: a Pragmatic Longitudinal Study. Hypertens Res 42, 1708–1715 (2019). https://doi.org/10.1038/s41440-019-0285-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0285-8
Keywords
This article is cited by
-
CPAP Treatment in Resistant Hypertension
Current Sleep Medicine Reports (2024)
-
Refractory hypertension and obstructive sleep apnea: a novel relationship
Sleep and Breathing (2023)
-
Refractory Hypertension: a Narrative Systematic Review with Emphasis on Prognosis
Current Hypertension Reports (2022)
-
Obstructive Sleep Apnea and Arterial Hypertension: Implications of Treatment Adherence
Current Hypertension Reports (2020)