Abstract
Epidemiological and clinical data of patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron variant (BA.2) admitted to three designated hospitals in Quanzhou City, Fujian Province, China, were collected and analyzed. Overall, 2,541 patients infected with BA.2, comprising 1,060 asymptomatic, 1,287 mild, and 194 moderate infections, were enrolled. The percentage of moderate infections was higher in patients aged ≥ 60 years than in those aged < 18 years and 18–59 years. The median hospitalization duration was 17 days. Among the 2,541 patients, 43.52% had a clear history of close contact. The vaccination rate was 87.92%, and the percentage of asymptomatic infections was higher in vaccinated than in unvaccinated patients. Moreover, patients with underlying diseases, including hypertension and diabetes mellitus, had more moderate infections than those without underlying diseases. The three most common clinical manifestations were fever, dry cough, and sore throat. The albumin-to-globulin (A/G) ratio and lymphocyte count decreased in cases with mild and moderate infections, while procalcitonin, erythrocyte sedimentation rate, interleukin-6, D-dimer, and C4 levels increased. Advanced age, non-vaccination, and underlying comorbid diseases were high-risk factors for disease progression in patients. However, dynamic monitoring of blood routine parameters, A/G ratio, and inflammatory indicators facilitated the prediction of disease progression.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is highly contagious and can easily create modes of avoidance to evade immune system attacks. It continuously mutates and evolves, producing mutant strains, such as Alpha (B.1.1.7), Beta (B.1.351), Gamma (P.1), Delta (B.1.617.2), and Omicron (B.1.1.529), with varying transmissibility, pathogenicity, and immune escape ability1. The World Health Organization received the first report of an infection with the SARS-CoV-2 Omicron variant in South Africa on November 24, 2021, and upgraded its classification to concern variants on November 26 of the same year2. Omicron variants have since spread rapidly to many countries and regions worldwide and are now the dominant strains, threatening human health and life. The mutants have high transmissibility with a shorter generation time and incubation period, as well as a stronger ability to evade the immune system. The effectiveness of the coronavirus disease 2019 (COVID-19) vaccines in preventing infection, illness, hospitalization, and death diminishes over time, with mutations in the spike (S) protein and resulting mutants posing new challenges to the development and application of these vaccines, as well as to prevention and control of the COVID-19 pandemic3. COVID-19 vaccines may cause side effects in some individuals, including rare abnormal blood clotting and heart inflammation4. COVID-19 can affect the entire range of infected individuals, in whom multiple organs and systems may be involved and affected, including but not limited to the respiratory system, cardiovascular system, nervous system, gastrointestinal system, and musculoskeletal system. The “post-acute sequelae of SARS-CoV-2 infection (PASC)” is highly heterogeneous, with unclear etiology and different pathogenesis, which requires further clarification5.
To our knowledge, there are few reports about real-world studies on COVID-19 in China, especially in the southeast coastal areas. Existing reports have included a few COVID-19 cases and evaluation indicators, which cannot comprehensively and objectively describe the clinical characteristics of the population under the state of natural COVID-19. In March 2022, a sudden outbreak of COVID-19 occurred in Quanzhou City, Fujian Province, China. Nucleic acid testing of clinical samples by the Quanzhou Center for Disease Control and Prevention (CDC) showed that the strain was a SARS-CoV-2 Omicron sublineage (BA.2). After comparing it with the current SARS-CoV-2 sequence database in China, the Chinese CDC confirmed that the mutant strain was newly discovered in China at that time. The newly emerged recombinant coronavirus variant may have the characteristics of high transmissibility of SARS-CoV-2, which may have a catastrophic impact. Therefore, there is an urgent need to develop broad-spectrum vaccines and therapeutics that are effective against beta-coronavirus in order to prevent possible future outbreaks of SARS-CoV-26. Few retrospective clinical studies on the SARS-CoV-2 Omicron variant have been reported in China. Therefore, this study analyzed the epidemiological and clinical features of BA.2 infections that caused the current epidemic outbreak in Quanzhou, aiming to provide a scientific basis for clinical diagnosis and treatment of the disease and accurate prognostic prediction.
Methods
Ethics declarations
Informed consent was obtained from all patients and/or their legal guardians. This study was approved by the Ethics Committee of the First Hospital of Quanzhou, Affiliated with Fujian Medical University (Quan Yi Lun 2023; approval number: K004). The study was conducted in accordance with the relevant guidelines and regulations of the Chinese Health Commission on the prevention and control of COVID-19.
Source of cases
This study enrolled patients who had either asymptomatic infections or confirmed symptomatic infections of Omicron variant strain BA.2 and were admitted between March 13, 2022, and April 14, 2022, at the Chengdong Branch and Infectious Diseases Branch of Fujian Medical University Affiliated First Quanzhou Hospital, as well as the Quanzhou "Huoweishan" Cabin Hospital. Patients suspected of recovering from COVID-19 but re-tested positive for SARS-CoV-2, with previous infection of the novel coronavirus, originating from regions other than Quanzhou, and with significant missing information on medical records were excluded from this study.
Diagnostic criteria
Patients with an epidemiological history and clinical manifestation of novel coronavirus infections along with serological or pathogenic evidence were defined as having a confirmed diagnosis of COVID-19 according to the COVID-19 Diagnosis and Treatment Protocol (Trial Version 9)7 issued by the Office of the National Health Care Commission and Office of the State Administration of Traditional Chinese Medicine. According to clinical manifestations and auxiliary examinations, confirmed cases were classified as mild, moderate, severe, and critical. Asymptomatic infections were defined as testing positive for the novel coronavirus and having no associated clinical manifestations according to the Prevention and Control Plan for Novel Coronavirus Disease (Version 8) issued by the Integrated Group of the State Council for Joint Prevention and Control of Novel Coronavirus Disease Epidemic8.
Data collection
Information on demographic characteristics, such as sex, age, body mass index, underlying disease, and vaccination status for COVID-19, as well as disease classification and clinical manifestations, was obtained. Auxiliary examinations, including routine tests for blood parameters, inflammatory markers, humoral immunity, T-lymphocyte subsets (absolute counts), coagulation, complete biochemical parameters, and COVID-19 antibodies; quantitative reverse-transcription polymerase chain reaction (RT-qPCR) cycle threshold (CT) for nucleic acid testing; pulmonary imaging (except in pregnant women); and post-treatment testing, were performed within 48 h of admission. Moreover, each case was evaluated as to whether Western or traditional Chinese medical treatments were to apply. The efficacy was evaluated by recording the time interval from testing positive to testing negative for SARS-CoV-2. Strict regulations of database management were implemented to ensure data security and confidentiality.
Statistical methods
All statistical analyses were performed using SPSS 23.0 (IBM Corp., Armonk, NY, USA). Measurement data were analyzed using the Kruskal–Wallis rank-sum or Mann–Whitney U tests and expressed as medians (25th and 75th percentiles). Count data were subjected to the χ2 or Fisher’s exact test and expressed as percentages. Differences with a P-value of < 0.05 were considered statistically significant.
Results
Epidemiological, demographic, and clinical features
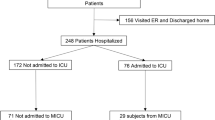
A total of 2,541 patients infected with SARS-CoV-2 Omicron sublineage (BA.2) were enrolled in this study, of whom 1,060 (41.72%) were asymptomatic, and 1,481 (58.28%) had a confirmed diagnosis of COVID-19. Of the confirmed cases, 1,287 (86.90%) were mild and 194 (13.10%) were moderate, but there were no severe or critical cases. Of the 2,541 patients, 1,106 (43.52%), 901 (35.47%), and 34 (21.01%) had a confirmed, uncertain, and no history of contact, respectively. Regarding the number of infected patients (whether asymptomatic or confirmed cases), most patients were from Fengze District (46.80% and 55.15%), followed by Jinjiang City, Licheng District, Shishi City, Luojiang District, Nan’an City, Hui’an County, Dehua County, and Quangang District. Meanwhile, no confirmed cases were reported in Yongchun County, and no Omicron variant infections were reported in Anxi County (Fig. 1). The percentages of patients who received the one, two, and three doses of the COVID-19 vaccine were 5.16%, 41.95%, and 40.82%, respectively, while that of unvaccinated patients was 10.19%. The percentage of asymptomatic infections was higher while the percentage of mild infections was lower in vaccinated than in unvaccinated patients (42.75% vs. 36.29%, χ2 = 3.97, P = 0.046; and 49.69% vs. 56.76%, χ2 = 4.64, P = 0.031; respectively). However, there was no significant difference in the percentage of moderate infections (7.56% vs. 6.95%, P = 0.72) between the vaccinated and unvaccinated groups, with no association of the between-group difference or similarity with the number of doses of the COVID-19 vaccine.
Distribution of patients with coronavirus disease 2019 (COVID-19) across Quanzhou City. (AB) Fengze District had the highest number of asymptomatic (A) and confirmed cases (B), followed by Jinjiang City, Licheng District, Shishi City, Luojiang District, Nan'an City, Hui'an County, Dehua County, and Quangang District. The map in Fig. 1 was generated using MS Paint. Version number: Windows 10 Home Chinese Version 21H2.URL link: https://www.microsoft.com/zh-cn/software-download/windows10.
As shown in Table 1, there were 1,218 male patients (47.93%), of whom 51.04% (541) were asymptomatic, which was higher than those with moderate infections (41.75%, n = 81). The age of the patients ranged from 1 to 97 years, with a median of 35 (24–48) years. Moreover, the infected patients were mainly aged between 18 and 59 years (76.34%). Patients aged < 18 years (15.03%) mainly had mild infections (57.33%), which was relatively higher than those aged 18–59 and > 60 years. The percentages of asymptomatic (49.32%) and moderate infections (10.96%) were higher in patients aged ≥ 60 years (8.62%) than in those belonging to the other two age groups (< 18 and 18–39). The median hospitalization duration was 17 (14–20) days, with the longest being 19 days for moderate infections, 17 days for mild infections, and 16 days for asymptomatic infections. A total of 275 patients (10.82%) had at least one underlying comorbid disease, with a high percentage of cases of hypertension (151 cases for 5.94%) and diabetes mellitus (81 cases for 3.12%), followed by coronary heart disease, malignancy, chronic liver disease, thyroid disease, connective tissue disease, and respiratory disease. The percentage of moderate infections was higher in patients with underlying comorbid disease than in those without (12.00% vs. 7.12%, χ2 = 8.26, P = 0.004). The most common clinical manifestations in confirmed cases were fever (27.47%), followed by dry cough (25.19%), sore throat (15.31%), fatigue (12.20%), expectoration (10.82%), myalgia (10.74%), stuffy and runny nose (4.80%), anosmia and ageusia (2.99%), diarrhea (2.56%), shortness of breath (1.02%), conjunctivitis (0.31%), as well as nausea and vomiting (0.19%) (Fig. 1).
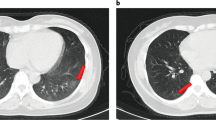
Results of auxiliary examinations within 48 h of admission
Abnormal alanine transaminase (ALT) levels and hypo-albuminemia were observed in 190 (7.48%) and 312 (12.28%) patients, respectively (Table 2). The lymphocyte count and albumin-to-globulin ratio (A/G) were higher in asymptomatic cases than in mild and moderate cases (all P < 0.01), while asymptomatic cases had lower levels of C-reactive protein (CRP), complement C4, interleukin-6 (IL-6), prothrombin, globulin (GLB), and D-dimer than mild and moderate cases (all P < 0.05). White blood cell, neutrophil, and platelet counts; total bilirubin (TBIL), ALT, and gamma-glutamyl transferase (GGT) levels; as well as CD3+ and CD4+ T-cell counts were higher in asymptomatic cases than in mild cases (all P < 0.01). Meanwhile, asymptomatic cases had a lower international normalized ratio than mild cases (P < 0.001), as well as a lower erythrocyte sedimentation rate (ESR) and immunoglobulin levels than moderate cases (all P < 0.01). Blood urea nitrogen levels were higher in asymptomatic cases, and albumin (ALB) levels were higher in mild cases than in moderate cases (both P < 0.05). The common imaging findings of moderate cases were patchy opacities (61.34%) and ground-glass opacities (53.09%), followed by strip cord shadow (39.18%) and nodular shadow (14.95%).
Main treatment options
All patients received traditional Chinese medicine treatment. In addition, 33 (1.29%), 54 (2.13%), and 12 (0.47%) patients received conventional nasal cannula oxygenation, oral antibiotic therapy (e.g., moxifloxacin and cefdinir) due to the consideration of bacterial co-infections, and antiviral therapy with oseltamivir phosphate, respectively.
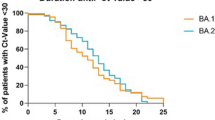
Risk factors for delayed discharge or release from quarantine
To explore the risk factors for delayed discharge or release from quarantine, patients with incomplete laboratory results were excluded from the analysis. Subsequently, using the median length of hospital stay of 17 days as the threshold, patients were divided into the control (< 17 days, n = 1210) and observation (≥ 17 days, n = 1331) groups. Crude logistic regression analysis showed that sex, disease classification, as well as lymphocyte and platelet counts, were related to delays in discharge or release from quarantine. Multivariable logistic regression analysis showed that only the disease classification and lymphocyte count were risk factors for delayed discharge or release from quarantine (Table 3).
Discussion
This retrospective clinical study involved patients infected with the community-transmitted SARS-CoV-2 Omicron BA.2 in China. Our results show that patients with SARS-CoV-2 Omicron BA.2 infection in Quanzhou were associated with lower median age, mild clinical presentation, shorter hospital stays, no severe cases and deaths, higher coverage of COVID-19 vaccine, and better prognosis compared with those infected with the original strain (Fig. 2). Despite the relatively low virulence of the Omicron variant, unvaccinated older adults, especially those with underlying comorbid diseases, were at high risk of suffering from both severe infection and death9. The predominance of asymptomatic infections in the vaccinated patients in this study and that of mild infections in the unvaccinated patients suggest that COVID-19 vaccination is protective against the Omicron variant, and the protective effect is independent of the number of vaccination doses.
Existing studies have suggested that women are less susceptible to SARS-CoV-2 due to the protective effects of the X chromosome and sex hormones10, with a lower risk of death in women infected with SARS-CoV-2 than in men (hazard ratio 1.59, 95% confidence interval: 1.53–1.65)11. In contrast, this study shows that the percentage of infected men was lower than that of infected women (47.93% vs. 52.07%). Moreover, the percentage of men with moderate infections was significantly lower than that of men with asymptomatic infections, suggesting that women are more susceptible to the Omicron variant BA.2 and more likely to have moderate infections. Unlike those infected with the original SARS-CoV-2 strain, the median age of patients infected with the Omicron variant was relatively low, with a downward shift in the age of infection12,13,14. Although patients aged ≥ 60 accounted for only 8.62% of the enrolled population, a higher percentage of them were with moderate infections than those aged < 18 and 18–59 years, suggesting that older age is still an important factor influencing disease progression. Another independent risk factor for disease progression is underlying comorbid disease15 rather than various mutations in the Omicron sublineage BA.2.216. The role of underlying diseases in the progression of Omicron infections was further highlighted by the fact that 10.82% of the patients in our study had comorbidities, and the percentage of moderate infections was higher in this sub-population than in the rest of the patients without pre-existing conditions.
In this study, 41.72% of the patients infected with Omicron BA.2 were asymptomatic, and the clinical manifestations of confirmed cases were relatively mild. The most common symptoms of confirmed cases were fever, dry cough, sore throat, fatigue, and muscle aches. Meanwhile, anosmia and ageusia, conjunctivitis, nausea, and vomiting were relatively rare, consistent with the results reported in a South Korea-based study17. The relatively high percentage of asymptomatic infections poses a great challenge to effective prevention and control of the pandemic. Furthermore, nucleic acid testing and COVID-19 antigen detection remain important tools to help in dynamic monitoring of the pandemic and prompt identification of infected persons18. Although asymptomatic and mild infections do not lead to changes in pulmonary imaging, the imaging parameter plays an irreplaceable role in clinical diagnosis and staging. Similar to the original SARS-CoV-2 strain, infections with the Omicron variant can also damage the lungs. In our study, damage manifested as patchy and ground-glass opacities in computed tomography images, with most lesions distributed in the peripheral zone and the subpleural areas. The difference was that pulmonary lesions in patients infected with the Omicron variant were significantly smaller or nodular, consistent with that reported in an Italian study19. The main reason for this difference is that the Omicron variant has a reduced binding capacity to the TMPRSS2 protein, significantly reducing the amount of virus entering the lung cells20,21.
Moreover, laboratory tests play an integral role in monitoring the severity of the disease and its treatment. Current studies have shown that decreased lymphocyte and increased neutrophil counts are significantly and positively associated with mortality22. Although there were no fatalities in this study, it is apparent that lymphocyte count was significantly reduced in moderate and mild infections compared with that in asymptomatic infections, which is consistent with the results of a previous Chinese study23. Inflammatory indicators of infection, such as procalcitonin (PCT), ESR, IL-6, and D-dimer levels, are effective predictors of mortality in inpatients in intensive care units24. In this study, the PCT, ESR, IL-6, and D-dimer levels were progressively elevated during asymptomatic, mild, and moderate infections. In particular, the IL-6 level was significantly elevated, with 7.48% of infected patients having an IL-6 level of > 1,000 mg/L and 2.32% of infected patients surpassing the upper limit (> 5,000 mg/L). Meanwhile, the CRP level, ESR, and leukocyte count were not simultaneously elevated to a high level. This observation ruled out the possibility of bacterial infections and suggested that over-activation of the IL-6 signaling pathway by the Omicron variants may be involved. However, the specific mechanism needs further investigation. These results suggest that dynamic monitoring of routine blood parameters, especially lymphocyte count and inflammatory indicators of infection, is useful in predicting the severity of the disease.
A previous study showed that the incidence of liver dysfunction in patients with COVID-19 was approximately 14–53%25, which was significantly higher than that observed in this study (7.48%). Our results can potentially be attributed to milder infections and the Omicron variant. Although levels of ALB, GLB, ALT, GGT, and TBIL in most infected patients were within normal ranges, approximately 12.28% of these patients still developed hypo-albuminemia, a condition that can be used as a marker to assess the severity of injury to the endothelial cells of the pulmonary capillary in infected patients26. Low ALB levels and high GLB levels in moderate infections led to a further decrease in the A/G ratio, and thus monitoring the A/G ratio helps determine the prognosis of the disease. Serum ferritin and lactate dehydrogenase are considered predictors of disease severity and progression in SARS-CoV-2-infected patients27; however, neither was associated with disease severity in Omicron variant-infected patients in this study. Moreover, this study did not observe acute kidney injury induced by the interaction of SARS-CoV-2 nucleoproteins with Smad3 signaling molecules28.
Several studies have demonstrated the presence of complement system activation in patients with COVID-19, as evidenced by a decrease in both complement C3 and complement C4 levels, as well as a significant correlation between the decrease in disease severity and high mortality29,30. Complement C4 level dropped in only 2.94% of infected patients in this study but was progressively elevated in asymptomatic, mild, and moderate infections, suggesting that the increase in complement C4 level is associated with disease severity in Omicron variant-infected patients. Further, high complement C3 level is an independent risk factor for delayed hospital discharge in patients infected with the original SARS-CoV-2 strain13.
This study has some limitations. First, all investigated infections originated only from the Quanzhou area, and there were no severe cases; hence, the epidemiological and clinical features did not comprehensively cover all SARS-CoV-2 Omicron infections. Second, the incubation period, CT of RT-qPCR for nucleic acid testing, and duration of symptoms of infected patients were not investigated. Third, the effect of the traditional Chinese medicine decoction on disease outcomes was not clarified. Although traditional Chinese medicine can play a role in adjuvant therapy, it is not the main therapy. Traditional Chinese medicine has certain advantages in relieving symptoms, improving immunity, and promoting rehabilitation, which has been involved in the treatment of patients with COVID-19 enrolled in this research institute. In this study, all patients with COVID-19 were treated with traditional Chinese medicine decoction as Yiqi Jiedu prescription, and clarifying its effect was impossible without comparison to other treatments or controls.
Despite these limitations, this was a rare real-world study of a large number of COVID-19 community infections in coastal areas of China. The number of infected patients included was large, and all infected patients were hospitalized. The observation and judgment of the condition of infected people were supported by medical staff with professional knowledge. This is a comprehensive and objective study with a detailed description of the demography, clinical manifestations, imaging features of the lung, and clinical outcomes of infected patients, which would have a certain clinical reference value.
In conclusion, this study revealed that patients infected with the SARS-CoV-2 Omicron variant in Quanzhou had a high rate of novel coronavirus vaccination, mild clinical manifestations, short hospitalization duration, and good prognosis, with no severe and death-related cases. This study reveals, to a certain extent, the basic characteristics and prognostic outcomes of Omicron BA.2 infections. Our findings would provide a reference for the prognostic prediction and medical resource allocation regarding Omicron BA.2 infections.
Data availability
All relevant information is provided in this current manuscript. If required, the data presented in this work can be shared by e-mail. If you need the data, please contact Xueping Yu.
References
WHO. Tracking SARS-CoV-2 Variants[EB/OL]. https://www.who.int/, (2021–12–06).
Pal, R. & Yadav, U. Resurgence of COVID-19 in India: time for introspection. Postgrad. Med. J. 98, e86–e87 (2022).
Luo, W. R. et al. Novel coronavirus mutations: Vaccine development and challenges. Microb. Pathog. 173, 105828 (2022).
Lamprinou, M., Sachinidis, A., Stamoula, E., Vavilis, T. & Papazisis, G. COVID-19 vaccines adverse events: potential molecular mechanisms. Immunol. Res. 71, 356–372 (2023).
Thaweethai, T. et al. Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA. 329, 1934–1946 (2023).
Callaway, E. The next generation of coronavirus vaccines: a graphical guide. Nature. 614, 22–25 (2023).
National Health Commission of China. COVID-19 diagnosis and treatment protocol (trial version 9). Int. J. Epidemiol. Infect. Dis. 49, 73–80 (2022).
Notice on the Publication of COVID-19 Prevention and Control (Eighth edition). Gazette of the National Health Commission of People's Republic of China 2021:4–60.
Cheung, P. H., Chan, C. P. & Jin, D. Y. Lessons learned from the fifth wave of COVID-19 in Hong Kong in early 2022. Emerg. Microbes Infect. 11, 1072–1078 (2022).
Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395, 507–513 (2020).
Williamson, E. J. et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 584, 430–436 (2020).
Maslo, C. et al. Characteristics and outcomes of hospitalized patients in South Africa During the COVID-19 omicron wave compared with previous waves. JAMA. 327, 583–584 (2022).
Lin, P. et al. Delayed discharge is associated with higher complement C3 levels and a longer nucleic acid-negative conversion time in patients with COVID-19. Sci. Rep. 11, 1233 (2021).
Wang, S. et al. Analysis of clinical characteristics and virus strains variation of patients infected with SARS-CoV-2 in Jiangsu Province-A retrospective study. Front. Public Health. 9, 791600 (2021).
Liu, X. Q. et al. Clinical characteristics and related risk factors of disease severity in 101 COVID-19 patients hospitalized in Wuhan. China. Acta Pharmacol. Sin. 43, 64–75 (2022).
Zhang, X., Zhang, W. & Chen, S. Shanghai’s life-saving efforts against the current omicron wave of the COVID-19 pandemic. Lancet. 399, 2011–2012 (2022).
Kim, M. K. et al. Clinical characteristics of 40 patients infected with the SARS-CoV-2 omicron variant in Korea. J. Korean Med. Sci. 37, e31 (2022).
Peeling, R. W., Heymann, D. L., Teo, Y. Y. & Garcia, P. J. Diagnostics for COVID-19: Moving from pandemic response to control. Lancet. 399, 757–768 (2022).
Okoye, C. et al. Computed tomography findings and prognosis in older COVID-19 patients. BMC Geriatr. 22, 166 (2022).
Yu, Y. Q. et al. SMYD2 inhibition downregulates TMPRSS2 and decreases SARS-CoV-2 infection in human intestinal and airway epithelial cells. Cells. 11, 1262 (2022).
Meng, B. et al. Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts infectivity and fusogenicity. Nature. 603, 706–714 (2022).
Cai, J. et al. The neutrophil-to-lymphocyte ratio determines clinical efficacy of corticosteroid therapy in patients with COVID-19. Cell Metab. 33, 258-269.e3 (2021).
Chen, W. et al. A retrospective study of the epidemiologic and clinical characteristics of COVID-19 among hospitalized patients in Quanzhou. China. Infect. Microbes Dis. 3, 32–40 (2021).
Milenkovic, M. et al. D-dimer, CRP, PCT, and IL-6 levels at admission to ICU can predict in-hospital mortality in patients with COVID-19 pneumonia. Oxid. Med. Cell. Longev. 2022, 8997709 (2022).
Zhang, C., Shi, L. & Wang, F. S. Liver injury in COVID-19: Management and challenges. Lancet. Gastroenterol. Hepatol. 5, 428–430 (2020).
Wu, M. A. et al. Hypoalbuminemia in COVID-19: assessing the hypothesis for underlying pulmonary capillary leakage. J. Intern. Med. 289, 861–872 (2021).
Chen, A. T. C., Coura-Filho, G. B. & Rehder, M. H. H. Clinical characteristics of Covid-19 in China. N. Engl. J. Med. 382, 1860 (2020).
Wang, W. et al. SARS-CoV-2 N protein induces acute kidney injury via Smad3-dependent G1 cell cycle arrest mechanism. Adv. Sci. Weinh. 9, e2103248 (2022).
Zinellu, A. & Mangoni, A. A. Serum complement C3 and C4 and COVID-19 severity and mortality: A systematic review and meta-analysis with meta-regression. Front. Immunol. 12, 696085 (2021).
Fang, S., Wang, H., Lu, L., Jia, Y. & Xia, Z. Decreased complement C3 levels are associated with poor prognosis in patients with COVID-19: A retrospective cohort study. Int. Immunopharmacol. 89, 107070 (2020).
Acknowledgements
This study was supported by the Major Health Research Project of Fujian Province (2021ZD01001), the Scientific and Technological Development Project of the Central Government shall guide local (2021L3018), the Young and middle-aged Talents Training Project of Fujian Provincial Health Commission (2020GGA076), and the Natural Science Foundation of Fujian Province (2023J01239).
Author information
Authors and Affiliations
Contributions
H.T.Z., Z.Y.W., Y.J.Z., M.H.Z., Z.J.S., Y.J.Z., and X.P.Y. conceived and designed the study; W.H.C., H.Y.H., and X.Y.Y. reviewed the literature; Y.X.Z., J.F.X., and K.C.Z. assessed the P.C.R. screening results; J.M.Z., Z.J.S., and X.B.Z. managed the datasets. H.T.Z., Z.Y.W., Y.J.Z., and M.H.Z. performed the statistical analysis; H.T.Z., Z.Y.W., Y.J.Z., M.H.Z., Z.J.S., Y.J.Z., and X.P.Y. wrote the original draft. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, H., Weng, Z., Zheng, Y. et al. Epidemiological and clinical features of SARS-CoV-2 Omicron variant infection in Quanzhou, Fujian province: a retrospective study. Sci Rep 13, 22152 (2023). https://doi.org/10.1038/s41598-023-49098-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-49098-x
This article is cited by
-
Deciphering the omicron variant: integrated omics analysis reveals critical biomarkers and pathophysiological pathways
Journal of Translational Medicine (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.