Abstract
Clinical trials revealed significant antitumor activity for immune checkpoint inhibitors (ICI) in metastatic urothelial carcinoma (mUC). Due to their strict eligibility criteria, clinical trials include selected patient cohorts, and thus do not necessarily represent real-world population outcomes. In this multicentric, retrospective study, we investigated real-world data to assess the effectiveness of pembrolizumab and atezolizumab and to evaluate the prognostic value of routinely available clinicopathological and laboratory parameters. Clinical and follow-up data from mUC patients who received ICIs (01/2017-12/2021) were evaluated. Overall survival (OS), progression-free survival (PFS), objective response rate (ORR), disease control rate (DCR), and duration of response (DOR) were used as endpoints. Patients’ (n = 210, n = 76 atezolizumab and 134 pembrolizumab) median OS and PFS were 13.6 and 5.9 months, respectively. Impaired ECOG-PS, the presence of visceral, liver or bone metastases, and hemoglobin levels were independently associated with poor OS and DCR. Furthermore, Bellmunt risk factors and the enhanced Bellmunt-CRP score were shown to be prognostic for OS, PFS and DCR. In conclusion, ICIs are effective treatments for a broad range of mUC patients. Our results confirmed the prognostic value of numerous risk factors and showed that Bellmunt risk scores can further be improved when adding CRP to the model.
Similar content being viewed by others
Introduction
Platinum-based chemotherapy has been the standard treatment for patients with locally advanced or metastatic urothelial carcinoma (mUC) for over 3 decades. In the past few years, the therapeutic landscape of locally advanced or mUC has remarkably changed, as immune checkpoint inhibitors (ICI) targeting programmed cell death protein-1 (PD-1) or programmed cell death-ligand 1 (PD-L1) have been approved for the treatment of mUC1. Data from the two-cohort, single-arm, multicenter phase II IMvigor210 trial have led to accelerated approval of the first ICI, atezolizumab, a monoclonal antibody directed against PD-L1 at first in the platinum-refractory, and later also in the first-line setting2.
Subsequently, four other inhibitors have been approved (avelumab, durvalumab, nivolumab, pembrolizumab) in the cisplatin refractory setting3,4,5,6. The anti-PD-1 antibody, pembrolizumab proved to be superior in terms of overall response rate (ORR), complete response (CR), and partial response (PR) and showed overall survival (OS) benefit of 3 months compared to second-line chemotherapy in a multicenter, randomized, active-controlled phase III trial (KEYNOTE-045)6,7. Later pembrolizumab and atezolizumab had also been approved in the first-line setting8, however due to the early results of two clinical trials (KEYNOTE-361 and IMvigor130) the approval has been restricted to patients with high.
PD-L1 tissue expression9. The role of PD-L1 expression as a biomarker for the selection of patients who are more likely to benefit from ICI therapy remains controversial. It was shown to be associated with better response rates to second-line atezolizumab (9% vs. 26%; IMvigor 210 study) and to first-line pembrolizumab treatments (20% vs. 38%; KEYNOTE-052)2,8. According to this later results, a recent meta-analysis revealed a survival benefit for PD-L1–positive mUC patients receiving first-line ICI treatment compared to those receiving standard chemotherapy10. However, the negative predictive value of low PD-L1 expression should rather be considered as low, as pembrolizumab improved survival also in the PD-L1 low expression subgroup as shown in the KEYNOTE-045 study7. In addition, to ICI therapy, novel treatment options such as targeted anti-FGFR therapy or antibody–drug conjugates became available and providing further therapeutic options for mUC patients11.
The above-mentioned clinical ICI-trials have included strongly selected patient populations and have been conducted under standardized and strictly controlled conditions in order to minimize bias and potential confounders12. Since the populations enrolled in such studies may differ in many ways (age, comorbidities, generalized organ dysfunction) from those seen in everyday practice, study findings are not always generalizable to all patient populations13. Therefore, there is a need for real-world data to provide information on the efficacy of ICI treatment in the general population.
In this multicentric, retrospective study we examined real-world data in order (1) to assess the characteristics of ICI-treated urothelial cancer (UC) patients, (2) to examine the effectiveness of two widely used ICI agents (pembrolizumab and atezolizumab) comparing to respective randomized controlled trials (RCTs) and (3) to evaluate the prognostic value of routinely available clinicopathological and laboratory parameters.
Results
Patient characteristics
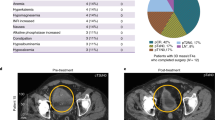
Data from 210 eligible patients were analyzed. A full description of patient characteristics for the whole cohort as well as for the first- and second-line treated patients are shown in Table 1. Seventy-six patients received atezolizumab and 134 patients received pembrolizumab. The median age at therapy initiation was 67.3 years (range: 28.9–87.2). Bellmunt risk calculation was possible for 184 patients14 (Table 1A).
Efficacy (tumor responses, PFS, OS)
Patients received a median of 6 (range: 1–80) treatment cycles and remained on therapy for a median of 4.3 months (range: 0–54.6). At the time of the data cutoff, 31 patients (14.8%) were still receiving ICI drugs. The median follow-up period after ICI initiation was 10.2 months. Among the 181 patients evaluable for tumor response, 13 had CR and 53 had PR. ORR for the whole cohort was 36.5%, while for the first-line 32.9% and for the second-line setting 38.9%. The median DOR was 11.8 months. Disease control was achieved in 112 patients.
The median PFS for the whole cohort and for the first-line and the second-line settings were 5.9 months (95% CI 3.9–7.8), 7.2 months (95% CI 4.2–10.3) and 4.4 months (95% CI 2.3–6.5), respectively. A total of 140 patients (66.7%) died during the follow-up period. The median OS was 13.6 months (95% CI 9.4–17.7) (Table 1B).
Factors associated with OS and PFS
In univariate Cox regression analyses, prior radical surgery, LN (lymph node) only metastases, high baseline hemoglobin and albumin as well as high eGFR values were significantly associated with improved OS. The presence of liver, visceral or bone metastases, worse ECOG-PS, presence of any Bellmunt risk factor (1 +) Bellmunt-CRP risk factor (1 +), and elevated NLR values were associated with shorter OS (Table 2).
In Cox regression analysis examining PFS age (> 68 years), LN only metastases, hemoglobin and albumin levels above the cutoff values were associated with improved PFS, while the presence of liver, visceral or bone metastases, ECOG-PS, Bellmunt and Bellmunt-CRP risk groups (1 +), and high NLR value were associated with worse PFS (Fig. 1A–D; Table 3). Univariate Cox regression analyses were also performed separately for first-, and second-line treatment groups. The detailed results are shown in Suppl. Tables 1 and 2.
Overall survival (OS) (left) and progression-free survival (PFS) (right) for patients grouped according to Bellmunt risk factors (A,B) and Bellmunt-CRP risk factors (C,D). Median OS for Bellmunt risk score groups (A) were as follows 26.9, 9.6, 6.3 and 2.6 months. Median PFS for Bellmunt risk score groups (B) were as follows 15.6, 3.6, 3.0 and 2.5 months. Median OS for Bellmunt-CRP risk score groups (C) were as follows 31.5, 14.1, 5.2, 3.9 months. Median PFS for Bellmunt-CRP risk score groups (D) were as follows 18.1, 5.6, 3.0 and 3.0 months.
Multivariate models included all the variables that showed significant associations with survival and were available for at least 85% of the cases. In multivariable analysis ECOG-PS, presence of visceral or bone metastases, and hemoglobin levels (> 10 g/dl) were found to be independent risk factors for OS. The presence of one or more Bellmunt risk factors proved to be an independent prognostic factor for shorter OS and PFS as well (Supplementary Table 3).
Factors associated with radiographic response or disease control
Information on therapy response during ICI treatment was available for a subset of patients (n = 181). Age at ICI initiation, ECOG-PS, presence of bone metastases, and Bellmunt risk factors as well as NLR and albumin levels showed significant associations with response and disease control (Table 3).
Discussion
The introduction of ICIs has significantly improved the treatment paradigm for mUC. Prospective clinical trials have shown that these agents can provide durable therapeutic effects and prolong survival, however, only in a rather small subgroup of patients2,6,7,8,15,16. Clinical trials include highly selected patient cohorts, which may not broadly represent real-world outcomes17. Therefore, real-world data received substantial attention in recent years, as it enables us to understand the practicality of medical interventions in a wider and more representative patient population18.
The multicentric nature of this study allowed the inclusion of a wide range of patients from the real clinical practice. Patient characteristics (age, sex, location of the primary tumor) of our cohort was comparable to those of the respective randomized clinical trials (KEYNOTE-045, KEYNOTE-052, IMvigor211 and IMvigor210), with only few exceptions (Table 4).
Interestingly, our real-life cohort included a lower rate of liver metastasis, which is an unexpected finding considering that investigators often tend to select more fit patients for inclusion in RCTs. A similar phenomenon was observed by Omland et al. when comparing a real-life cohort of Danish UC patients treated with pembrolizumab to cohorts from clinical trials19. The presence of liver metastasis is a well-known risk factor of OS. In line with our findings, a meta-analysis has reported a significant association between the presence of visceral or liver metastasis and worse OS in the pembrolizumab-treated UC patient cohort20. In addition, recent findings have shown that radical surgery of the primary tumor does not confer with OS benefits in patients with liver metastasis21. Due to the shorter life expectancy of these patients, they frequently do not receive any systematic treatment. This could serve as a plausible explanation for the underrepresentation of patients with liver metastasis in our real-life cohort. Another explanation might be that oncologists in real clinical practice may prefer chemotherapy for these patients or inclusion in clinical trials such as those involving antibody–drug conjugates, which were actively recruiting patients during the timeframe of this retrospective cohort study.
The ORRs observed in our study were similar to those reported in the RCTs, with exception of second-line atezolizumab treatment. In this setting, the ORR of the real-life cohort (41.7%) was more than 25% higher compared to the respective clinical trials (14.5% and 13.3% in the IMvigor210/cohort 2 and IMvigor211, respectively). Similarly, a real-life study by Tural et al. investigating an atezolizumab-treated UC population reported also a higher ORR rate (28.7%) for the second-line setting22.
The median OS time for our whole cohort was 13.6 months. When dividing the patients according to the applied drugs and settings; the worst OS could be observed in the first-line atezolizumab-treated patients’ group, although the case numbers in this subgroup are low. There was a relevant OS difference in the second-line atezolizumab-treated groups between the real-life (17.0 months) and RCT cohorts (7.9 and 11.1 months in the IMvigor210/cohort 2 and IMvigor211, respectively). According to this observation, also other real-life studies found a significantly longer survival for this subgroup comparing to the respective RCTs, suggesting an even higher benefit for this treatment setting in real-world conditions as observed in former clinical trials22,23,24.
In this study, impaired ECOG-PS, the presence of visceral, liver, or bone metastases, and baseline hemoglobin levels below 10 g/dl were found to be independent prognostic factors for OS. In addition, the presence of one or more Bellmunt risk factors proved to be an independent prognostic factor for shorter OS.
ECOG-PS is a validated prognostic parameter in oncology outpatient settings. It has previously been demonstrated as an independent prognostic factor for OS in patients with advanced UC who are treated with platinum-containing regimens14. In line with our present results, Yanagisawa et al. reported worse OS for UC patients with poor ECOG-PS despite pembrolizumab treatment20. In a retrospective cohort study, Khaki et al. investigated real-life patient data and reported shorter OS for patients with ECOG-PS ≥ 2, particularly in the first-line setting25. Similar results have been reported by Tural et al. in the second-line setting for a real-life cohort22.
The Bellmunt risk score is a further well-established prognostic factor in the second-line treatment setting UC6. While initially developed based on a chemotherapy cohort, its simplicity led to its utilization for risk stratification of ICI-treated patients. In order to enhance discrimination of the Bellmunt risk score in ICI-treated patients with UC, an enhanced version known as theBellmunt-CRP score has been recently established by Abuhelwa et al.26. In this study, we assessed the performance of the Bellmunt-CRP risk score for the first time on real-life data and could validate its improved ability to discriminate high-risk patients. However, this association was not found to be statistically significant in the first-line cohort.
Regarding hematological biomarkers, elevated pre-treatment levels of NLR and low albumin levels were found to be significantly associated with worse OS, PFS, and response to ICI therapy in various cancers27,28. Nassar et al. showed an association between high NLR and lack of clinical benefit to ICIs in UC patients29. The cause of the elevated ratio can be either higher neutrophil abundance or lower levels of lymphocytes. On one hand, neutrophil infiltration in cancer tissue can contribute to a pro-tumor microenvironment, as they are able to secrete immunosuppressive mediators and angiogenic factors (e.g. reactive oxygen species, vascular endothelial growth factor and matrix metalloproteinase 9), which can promote tumor growth and progression30. On the other hand, low levels of circulating lymphocytes may correlate with a decreased number of tumor-infiltrating lymphocytes and thus a reduced anti-tumor T-cell response31. The here presented results confirm that NLR is a suitable candidate for a cost-effective and widely accessible biomarker.
Our study has several limitations. First, the retrospective study design limits the availability of the collected data. In addition, detailed information about side effects is missing. Second, our cohort was heterogeneous regarding the line of therapy, and previous chemotherapy regimens. Third, real-life circumstances did not allow a strict timing of imaging analyses and there was no opportunity for a central evaluation of CT/MRI scans. Thus, treatment response was determined by the data collector, based on clinical reports, which may affect the interpretation of results. Fourth, PD-L1 immunohistostaining was available only for a limited number of patients with heterogeneous assay and evaluation methods, which did not allow us the performance of a statistically valid evaluation. Therefore, the therapy predictive value of tissue PD-L1 expression could not be assessed in this study.
In conclusion, in this multicentre study, we demonstrated that atezolizumab and pembrolizumab are effective treatment options for a broad range of mUC patients regardless of treatment line. Second-line atezolizumab provided higher response and OS rates compared to the respective RCTs. As the treatment landscape for mUC is continuously expanding, easily accessible markers like clinicopathological and laboratory parameters are essential for better therapeutic decision-making. Our results demonstrated the prognostic value of a series of risk factors such as ECOG-PS, liver, visceral, bone or LN only metastases, NLR, hemoglobin, albumin, eGFR levels and we were able to confirm that the prognostic value of Bellmunt risk scores can further be increase when adding CRP to the model. Based on these, our study contributes to the current body of evidence by reporting valuable real-life experiences and pointing out some important similarities and differences to the approval studies. These data will provide important input to larger meta-analyses and may contribute to clinical conclusions on high clinical evidence level. Finally, relevant real-world studies will help to place ICI therapy in the evolving treatment context of mUC.
Methods
Patients and data collection
Eligible patients for inclusion were adults (≥ 18 years) with a confirmed diagnosis of advanced or metastatic urothelial tract malignancy, who received at least one cycle of ICI therapy (pembrolizumab or atezolizumab) as first- or second-line treatment between 01/2017 and 12/2021. Patients with non-urothelial histology and those who were treated within clinical trials were excluded (Fig. 2). Patients’ data were obtained from medical records at 6 urooncology centers (Semmelweis University; National Institute of Oncology; University Hospital Duesseldorf; University of Duisburg-Essen; University of Szeged; Borsod-Abaúj-Zemplén County Hospital). Clinicopathological, laboratory, and outcome data were collected. Previously reported cutoff values were applied to the laboratory parameters. According to the original and the enhanced Bellmunt risk score 10 g/dl, 30 mg/l, and 5 were used as the cutoffs for hemoglobin, C-reactive protein (CRP), and neutrophil–lymphocyte-ratio (NLR), respectively14,26. In addition, the lower limit of the normal range was employed as the cutoff value for albumin (35 g/l), and the upper limit of the normal range as the cutoff for LDH (250 U/l). For estimated glomerular filtration rate (eGFR), we applied the 40 ml/min as the cut-off value. The follow-up cutoff was at 08/2022. The study conformed to the Declaration of Helsinki and the institutional ethics committee (Semmelweis Egyetem Regonális, Intézményi Tudományos és Kutatásetikai Bizottsága and Ethik Kommission Medizinische Fakultät der Universität Duisburg-Essen) approved the study protocol (SE RKEB 125/2019, 15–6400-BO, 2021–1548). Informed consent was obtained from all participants.
Outcomes
OS was the primary endpoint, while the secondary endpoints included progression-free survival (PFS), ORR, disease control rate (DCR), and duration of response (DOR). OS was defined as the period from ICI therapy initiation to the date of death, whereas PFS referred to the time from the first ICI treatment to the date of disease progression (radiographic or clinical) or death. Patients who did not die during the observation period were censored at the last follow-up. Responses were assessed using computed tomography (CT) scans according to institutional standard in patients with at least one follow-up scan during treatment. CT scans were evaluated by local radiologists at each center as part of the daily routine, following the Response Evaluation Criteria in Solid Tumors (RECIST) guideline version 1.1. Treatment response was determined by the data collector based on radiographic studies and clinic notes. ORR was defined as the percentage of patients who achieved a PR or CR to the treatment. DCR included patients with CR, PR, or stable disease (SD). Time-to-response referred to the duration from the first cycle until the first documented response. DOR was defined as the time from the first documented radiological response to disease progression or death.
Statistical analysis
Descriptive statistics included median and range for continuous variables and numbers and percentages for categorical variables. All time-to-event data (OS, PFS, DOR) are summarized using Kaplan–Meier estimates, and medians are reported with corresponding 95% confidence intervals (CI). The median and range of time-to-response are reported for patients with CR and PR. Cox proportional hazard models were used to assess differences in hazard ratios (HR) between groups according to the risk factors and stratified two-sided log-rank test was used to assess differences in OS. Chi-square test was used to determine the association between response (CR/PR) or disease control (CR/PR/SD) and different clinicopathological variables. A p-value of < 0.05 was considered significant. All statistical analyses were performed with SPSS version 27.0 (IBM, Armonk, N.Y., USA).
Data availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Stenehjem, D. D. et al. PD1/PDL1 inhibitors for the treatment of advanced urothelial bladder cancer. Onco Targets Ther. 11, 5973–5989 (2018).
Rosenberg, J. E. et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: A single-arm, multicentre, phase 2 trial. Lancet 387(10031), 1909–1920 (2016).
Apolo, A. B. et al. Avelumab, an anti-programmed death-ligand 1 antibody, in patients with refractory metastatic urothelial carcinoma: Results from a multicenter, phase Ib study. J. Clin. Oncol. 35(19), 2117–2124 (2017).
Powles, T. et al. Efficacy and safety of durvalumab in locally advanced or metastatic urothelial carcinoma: Updated results from a phase 1/2 open-label study. JAMA Oncol. 3(9), e172411 (2017).
Sharma, P. et al. Nivolumab in metastatic urothelial carcinoma after platinum therapy (CheckMate 275): A multicentre, single-arm, phase 2 trial. Lancet Oncol. 18(3), 312–322 (2017).
Bellmunt, J. et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N. Engl. J. Med. 376(11), 1015–1026 (2017).
Fradet, Y. et al. Randomized phase III KEYNOTE-045 trial of pembrolizumab versus paclitaxel, docetaxel, or vinflunine in recurrent advanced urothelial cancer: Results of >2 years of follow-up. Ann. Oncol. 30(6), 970–976 (2019).
Vuky, J. et al. Long-term outcomes in KEYNOTE-052: Phase II study investigating first-line pembrolizumab in cisplatin-ineligible patients with locally advanced or metastatic urothelial cancer. J. Clin. Oncol. 38(23), 2658–2666 (2020).
Teo, M. Y. & Rosenberg, J. E. EMA and FDA prune the checkpoint inhibitor treatment landscape. Nat. Rev. Urol. 15(10), 596–597 (2018).
Rizzo, A., Mollica, V. & Massari, F. Expression of programmed cell death ligand 1 as a predictive biomarker in metastatic urothelial carcinoma patients treated with first-line immune checkpoint inhibitors versus chemotherapy: A systematic review and meta-analysis. Eur. Urol. Focus 8(1), 152–159 (2022).
Mollica, V. et al. Current strategies and novel therapeutic approaches for metastatic urothelial carcinoma. Cancers (Basel) 12(6), 1449 (2020).
Katkade, V. B., Sanders, K. N. & Zou, K. H. Real world data: An opportunity to supplement existing evidence for the use of long-established medicines in health care decision making. J. Multidiscip. Healthc. 11, 295–304 (2018).
Sherman, R. E. et al. Real-world evidence—What is it and what can it tell us?. N. Engl. J. Med. 375(23), 2293–2297 (2016).
Bellmunt, J. et al. Prognostic factors in patients with advanced transitional cell carcinoma of the urothelial tract experiencing treatment failure with platinum-containing regimens. J. Clin. Oncol. 28(11), 1850–1855 (2010).
Powles, T. et al. Atezolizumab versus chemotherapy in patients with platinum-treated locally advanced or metastatic urothelial carcinoma (IMvigor211): A multicentre, open-label, phase 3 randomised controlled trial. Lancet 391(10122), 748–757 (2018).
Vander Velde, N. et al. Comparative effectiveness of non-cisplatin first-line therapies for metastatic urothelial carcinoma: Phase 2 IMvigor210 study versus US patients treated in the veterans health administration. Eur. Urol. Oncol. 2(1), 12–20 (2019).
Tan, Y. Y. et al. Comparing clinical trial population representativeness to real-world populations: An external validity analysis encompassing 43 895 trials and 5 685 738 individuals across 989 unique drugs and 286 conditions in England. Lancet Healthy Longev. 3(10), e674–e689 (2022).
Blonde, L. et al. Interpretation and impact of real-world clinical data for the practicing clinician. Adv. Ther. 35(11), 1763–1774 (2018).
Omland, L. H. et al. Real-world treatment patterns and overall survival in locally advanced and metastatic urothelial tract cancer patients treated with chemotherapy in Denmark in the preimmunotherapy era: A nationwide Population-based Study. Eur. Urol. Open Sci. 24, 1–8 (2021).
Yanagisawa, T. et al. Pretreatment clinical and hematologic prognostic factors of metastatic urothelial carcinoma treated with pembrolizumab: A systematic review and meta-analysis. Int. J. Clin. Oncol. 27(1), 59–71 (2022).
Dong, F. et al. Prognostic value of site-specific metastases and therapeutic roles of surgery for patients with metastatic bladder cancer: A population-based study. Cancer Manag. Res. 9, 611–626 (2017).
Tural, D. et al. Atezolizumab in patients with metastatic urothelial carcinoma who have progressed after first-line chemotherapy: Results of real-life experiences. Eur. Urol. Focus 7(5), 1061–1066 (2021).
Ruiz-Banobre, J. et al. Rethinking prognostic factors in locally advanced or metastatic urothelial carcinoma in the immune checkpoint blockade era: A multicenter retrospective study. ESMO Open 6(2), 100090 (2021).
Park, J. H. et al. Prognostic model in patients with metastatic urothelial carcinoma receiving immune checkpoint inhibitors after platinum failure. Curr. Probl. Cancer 46(3), 100848 (2022).
Khaki, A. R. et al. A new prognostic model in patients with advanced urothelial carcinoma treated with first-line immune checkpoint inhibitors. Eur. Urol. Oncol. 4(3), 464–472 (2021).
Abuhelwa, A. Y. et al. Enhanced bellmunt risk score for survival prediction in urothelial carcinoma treated with immunotherapy. Clin. Genitourin. Cancer 20(2), 132–138 (2022).
Jeyakumar, G. et al. Neutrophil lymphocyte ratio and duration of prior anti-angiogenic therapy as biomarkers in metastatic RCC receiving immune checkpoint inhibitor therapy. J. Immunother. Cancer 5(1), 82 (2017).
Park, W. & Lopes, G. Perspectives: Neutrophil-to-lymphocyte ratio as a potential biomarker in immune checkpoint inhibitor for non-small-cell lung cancer. Clin. Lung Cancer 20(3), 143–147 (2019).
Nassar, A. H. et al. A model combining clinical and genomic factors to predict response to PD-1/PD-L1 blockade in advanced urothelial carcinoma. Br. J. Cancer 122(4), 555–563 (2020).
Piccard, H., Muschel, R. J. & Opdenakker, G. On the dual roles and polarized phenotypes of neutrophils in tumor development and progression. Crit. Rev. Oncol. Hematol. 82(3), 296–309 (2012).
Restifo, N. P., Dudley, M. E. & Rosenberg, S. A. Adoptive immunotherapy for cancer: Harnessing the T cell response. Nat. Rev. Immunol. 12(4), 269–281 (2012).
Funding
Open access funding provided by Semmelweis University. T. S. was supported by a János Bolyai Research Scholarship of the Hungarian Academy of Sciences (BO/00451/20/5) and by the New National Excellence Program (ÚNKP-21-5-SE-3) and the K139059 grant of the Ministry for Innovation and Technology from the source of the National Research Development and Innovation Fund. T. F. was supported by the ÚNKP-22-3-1-SE-19 New National Excellence Program of the Ministry for Innovation and Technology from the source of the National Research, Development and Innovation Fund.
Author information
Authors and Affiliations
Contributions
M.V.: Conceptualization, Project administration, Data curation, Formal analysis, Writing—original draft. O.H.: Data curation, Writing—review & editing. O.M.: Data curation, Writing—review & editing. T.F.: Conceptualization, Methodology, Writing—review & editing. C.M.G.: Data curation, Writing—review & editing. G.N., U.K., V.G., B.H. and P.N.: Writing—review & editing. C.O.: Project administration, Writing—review & editing. A.M., A.F. and M.S.: Data curation, Writing—review & editing. T.S.: Conceptualization, Methodology, Supervision, Writing—original draft.
Corresponding author
Ethics declarations
Competing interests
Boris Hadaschik has had advisory roles for ABX, AAA/Novartis, Astellas, Astra-Zeneca, Bayer, Bristol Myers Squibb, Janssen R&D, Lightpoint Medical, Inc., and Pfizer; has received research funding from Astellas, Bristol Myers Squibb, AAA/Novartis, German Research Foundation, Janssen R&D, and Pfizer; and has received compensation for travel from Astellas, AstraZeneca, Bayer, and Janssen R&D. Günter Niegisch reports honoraria for lectures, symposia from Roche Pharma, MEDAC, Pfizer, BMS, AstraZeneca; and has had advisory roles for Roche Pharma, Sanofi, BMS, Merck Serono, Pfizer, MEDAC, Ipsen, Janssen; and reports support for travel expenses, congress fees from Roche Pharma, Pfizer, Merck, AstraZeneca. Viktor Grünwald has had advisory roles for Bristol-Myers Squibb, Pfizer, MSD Oncology, Merck HealthCare, Ipsen, Eisai, Debiopharm, PCI Biotech, Cureteq, Oncorena and has received compensation for travel from Pfizer, Ipsen, Merck HealthCare, and reports honoraria from Bristol-Myers Squibb, Pfizer, Ipsen, Eisai, MSD Oncology, Merck HealthCare, EUSAPharm, Apogepha, Ono Pharmaceutical. Ulrich Krafft has received research funding from Bristol Myers Sqibb, Novartis / AAA, and has received compensation for travel from Janssen Research funding, Bristol Myers Sqibb, Novartis/AAA. Camilla M. Grunewald has had advisory roles for Ferring. The remaining authors have no conflicts of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Váradi, M., Horváth, O., Módos, O. et al. Efficacy of immune checkpoint inhibitor therapy for advanced urothelial carcinoma in real-life clinical practice: results of a multicentric, retrospective study. Sci Rep 13, 17378 (2023). https://doi.org/10.1038/s41598-023-44103-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-44103-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.