Abstract
The impact of TP53 gene mutations in recurrent HPV-negative vulvar squamous cell carcinomas is unclear. TP53 gene mutations were analyzed in archival tissues of 24 primary squamous cell carcinoma and local vulvar recurrences arising in chronic inflammatory dermatoses by analyzing the full coding sequence of the TP53 gene and correlated with disease-free survival. After resection of the primary squamous cell carcinoma with clear margins 19/24 patients had one and 5/24 had multiple recurrences. The first recurrence occurred after median of 46 months (range 12–180 months). In all, 17/24 (71%) primary squamous cell carcinomas had TP53 gene mutations and recurred after median disease-free intervals of 33 months (range 12–180). 14/17 (88%) recurrent squamous cell carcinomas carried again TP53 gene mutations, five with identical and nine with different, more complex TP53 gene mutations. 7/24 (29%) patients with a p53 wild-type primary SCC had the first recurrence after median 65 months (range 14–144) featuring p53 wild-type in 3/7 (43%) and TP53 gene mutations in 4/7 (57%) recurrent squamous cell carcinomas. Disease-free intervals of > 5 years (60–180 months) were observed in 10/24 patients total (42%; equally divided among p53 wild-type (5/7; 71%) and TP53 gene mutated (5/17; 29%) squamous cell carcinomas). In summary, squamous cell carcinomas recurred in the residual vulvar dermatosis independent of TP53 gene mutational status of the primary squamous cell carcinoma. The majority of TP53 gene mutated cancers recurred with different TP53 gene mutations, some of them more complex, and patients with p53 wild type developed TP53 gene mutations in the recurrent squamous cell carcinomas, possibly indicating increased genetic instability in longstanding chronic inflammatory dermatoses. A change of TP53 gene mutational status after > 5 years suggests de novo oncogenic events/carcinogenesis. Longer disease-free intervals in patients with p53 wild-type primary squamous cell carcinoma suggest that TP53 gene mutational status may serve as a prognostic marker for disease-free intervals.
Similar content being viewed by others
Introduction
Invasive Human Papilloma Virus (HPV) -negative squamous cell carcinomas commonly arise in the back ground of chronic inflammatory disease lichen sclerosus and lichen planus [1,2,3]. They have a high recurrence rate despite complete excisions [4]. In contrast to HPV-induced squamous cell carcinomas HPV-negative invasive vulvar squamous cell carcinomas harbor a wide variety of random somatic TP53 gene mutations [5]. TP53 gene mutations represent a final common pathway in about 50% of cancers, and have been linked to poorer survival and shorter disease-free intervals when compared to HPV-induced squamous cell carcinomas in various organ systems including vulvar cancers [6,7,8,9,10,11,12]. The inferior outcome is attributed to chemo- and radio-resistance as the effects of radiation and many chemotherapeutic agents are mediated through the p53 pathway [13, 14]. Mainly due to the rarity of vulvar cancer and subsequent lack of randomized trials the most recent FIGO and ESGO guidelines do not recognize different oncogenic pathways, in particular presence/absence of TP53 gene mutations, as treatment relevant [15, 16]. To date, no data are available if and how TP53 gene mutational status of vulvar squamous cell carcinomas influences disease-free survival. It is unknown if the mutational status (wild-type or mutation) is maintained in recurrent invasive vulvar squamous cell carcinomas and if primary and recurrent squamous cell carcinomas carry identical TP53 gene mutations. Immunohistochemical staining allows identification of missense TP53 gene mutations via demonstration of nuclear accumulation of hyperstable mutant p53 protein. A negative staining result cannot reliably distinguish between TP53 gene mutations with frameshift or stop-gain mutations without p53 protein production or squamous cell carcinomas with p53 wild-type protein. We therefore investigated presence and type of TP53 gene mutations in primary and recurrent invasive vulvar squamous cell carcinomas by analyzing the entire coding region of the TP53 gene.
Materials and methods
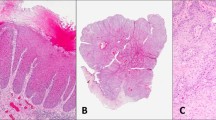
All primary and recurrent invasive vulvar squamous cell carcinomas included in this study were diagnosed at the Institute of Pathology at the Medical University Graz, Austria. The term “recurrence” in this paper refers to a new local vulvar cancer after complete resection of the primary squamous cell carcinomas with clear margins. The clinically widely used term “distant recurrence” reflects biologically a metastasis and correctly should be labelled as such, but they were not analyzed in this paper. All cancers were evaluated for etiology during routine surgical work-up and divided into (i) HPV-induced vulvar squamous cell carcinomas based on demonstration of HPV DNA along with concomitant p16ink4aoverexpression and (ii) squamous cell carcinomas arising independent of transforming HPV infections (no HPV-DNA and no p16ink4a overexpression), referred to as HPV-negative cancers in this paper. Tumor samples were taken from a central portion of the cancer.
HPV genotyping was performed on formalin fixed and paraffin embedded tumor tissue and is based on the principle of reverse hybridization and the SPF10 primer set which amplifies a 65-bp region in the L1 open reading frame of the HPV genome (INNO-LiPA HPV GENOTYPING EXTRA; Innogenetics Diagnostic, Heiden, Germany and CHIPRON GmbH, Berlin, Germany). Multiplex PCR and duplex hybridisation allows detection of DNA of 32 HPV-subtypes including HPV-high risk subtypes 16,18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59; HPV-low risk subtypes 6,11; and potentially carcinogenic HPV subtypes 26, 30, 34, 53, 66, 67, 68, 69, 70, 73, 82, 85, 97. DNA was extracted on a Maxwell, MDx Research System (Promega, Fitchburg, Wisconsin, USA).
Initially, we screened the previously published 24 patients [4] with recurrent squamous cell carcinomas arising in the background of mostly advanced untreated chronic inflammatory dermatoses and excluded eight patients with recurrences < 12 months (with the aim to avoid analysis of possibly missed precancerous lesions in the surrounding diseased skin rapidly evolving to invasive cancer), and one patient with non-invasive d-VIN. Sufficient DNA quality for TP53 gene mutational analysis was available for 13 of the remaining 15 patients. Since then we identified 11 more patients with at least one recurrent invasive SCC after ≥ 12 month disease-free intervals. In total we analyzed 24 patients with a lichen sclerosus or lichen planus-associated primary squamous cell carcinoma and their recurrent invasive squamous cell carcinoma. NGS libraries were prepared using the AmpliSeq library kit 2.0 (Thermo Fisher Scientific) and the Ion Ampliseq TP53 primer pool covering all exons of the TP53 gene. Sequencing was performed on an Ion Proton benchtop sequencer (Thermo Fisher Scientific) to a length of 200 base pairs. Initial data analysis was performed using the Ion Torrent Suite Software Plug-ins (Thermo Fisher Scientific, open source, GPL, https://github.com/iontorrent/). Briefly, this included base calling, alignment to the reference genome (HG19) using the TMAP mapper and variant calling by a modified diBayes approach taking into account the flow space information. Called variants were annotated using open source software ANNOVAR [17] and SnpEff [18]. All coding, non-synonymous mutations were further evaluated and visually inspected in IGV (http://www.broadinstitute.org/igv/) and variant calls resulting from technical read errors or sequence effects were excluded from the analysis. All annotations of TP53 mutations are based on reference transcript NM_000546. “Hot spot” mutations were defined as missense mutations that occur at an unusual high frequency (top 10% of the most commonly mutated amino acid positions in the TP53 gene according to the IARC TP53 database). Their effect of increased invasion/ migration, angiogenesis, dedifferentiation, anchorage-independent growth, rapid metastasis by interaction with other cellular proteins and regulation of cancer cell transcriptional programs is referred to as oncogenic gain-of-function (GOF). Conversely, mutations which lead to frameshift, stop-gain or otherwise abolished the function of the TP53 are referred to as loss-of-function (LOF) mutations. Paraffin blocks of primary and recurrent vulvar squamous cell carcinomas were evaluated for nuclear p53 expression with antibody clone DO-7 (DAKO, Denmark). Approval of the institutional ethics review board and research ethics committee for this study was obtained (Medical University Graz, Austria, EK20-255 ex 08/09).
Results
Overall characteristics
All 24 patients (median age 69 years, range 40–84 years) had a primary HPV-negative squamous cell carcinoma arising in the background of an untreated chronic lichenoid dermatosis. After resection of the 1° squamous cell carcinoma with clear margins, 19/24 patients had one and 5/24 patients had multiple recurrences. The first recurrence was resected after a median of 46 months (range 12–180 months; details see Table 1). The second recurrence occurred after a median of 22 months (range 12–46 months). In all, 3/24 patients had a third recurrences after a median of 29 months (range 12–46 months); 1/24 patient suffered five recurrences. Time intervals for second and further recurrences reflect time from last recurrence, not overall elapsed time. The local recurrences arose in skin/mucosa affected by residual chronic inflammatory diseases (lichen planus and lichen sclerosus). The spatial relationship between primary and recurrent squamous cell carcinoma was dependent on type of primary treatment and extent of surgery. In patients with primary radiation squamous cell carcinoma recurred close to the original site. In surgically treated patients site of recurrences and distance to the primary squamous cell carcinoma was determined by the amount of residual diseased skin/mucosa and differed between only 0.5–1 cm from the site of primary cancer or scar of resection and larger distances of several cm with recurrences on the other side of the vulva or in perineum after primary periclitoral squamous cell carcinoma.
In all, 17/24 (71%) primary squamous cell carcinomas harbored somatic TP53 gene mutations, while 7/24 (29%) primary squamous cell carcinomas had wild-type p53 protein. The median age at diagnosis of the primary squamous cell carcinomas was 70 years in the TP53 gene mutated cancer group und 68 years in the p53 wild-type cancer group.
Seventeen primary squamous cell carcinomas with somatic TP53 gene mutation
The primary squamous cell carcinoma of 17/24 (71%) patients (Table 2; pt.# 1-17; median age 70 years, range 40–83 years) harbored one (n = 14) or two (n = 3) somatic TP53 gene mutations. Missense TP53 gene mutations were identified in 12/17 squamous cell carcinomas and most occurred only once. GOF “hot spot” mutations were identified at codons R175H, R248Q, R273, R278A, R282, P278A; details see Table 2). In all, 5/17 squamous cell carcinomas harbored TP53 gene mutations with LOF (2 stop-gain, 3 frameshift). The first recurrence was diagnosed after a median of 33 months (range 12–180 months). Only 5/17 (29%) patients had disease-free intervals > 5 years, of whom three patients (3/17 = 18%; pt.# 5,11,15) showed a switch from TP53 gene mutation to wild-type p53 in the recurrence. Identical TP53 gene mutations in the first recurrent squamous cell carcinoma were observed in 5/17 (29%) of patients (pts.# 4,10,12, 14,17; 1x LOF Q317* stop-gain, and 4x missense mutation without GOF) after intervals of 1–3 years. The recurrence of 1/17 patients after 96 months revealed a new mutation in addition to the original TP53 gene mutation (pt. #8). In all, 8/17 (47%) recurrent squamous cell carcinoma showed again TP53 gene mutations, but different and typically more complex ones (e.g. more mutations than in the primary squamous cell carcinomas; missense mutations with GOF; LOF mutations; see Table 2).
Seven primary squamous cell carcinomas with p53 wild-type protein
A total of 7/24 (29%) primary squamous cell carcinomas (pt.# 18–24; median age 68 years, range 55–84 years) were devoid of TP53 gene mutations. The first recurrent squamous cell carcinoma was diagnosed after a median of 65 months (range 14–144 months). p53 wild-type status was maintained in the recurrences of 3/7 (43%) patients after 14, 20 and 69 months. The other 4/7 (57%) patients presented with TP53 gene mutations in the recurrent invasive squamous cell carcinoma after disease-free intervals between 60 and 144 months (see Table 3).
Type of TP53 gene mutations and immunohistochemical p53 staining
In analogy to the distribution of the most common hot spot mutations in human tumors in general, we identified mutations at codons R175H in 4 patients (1x primary squamous cell carcinoma, and 3x recurrent squamous cell carcinoma) and R273C in three patients (both primary and recurrent squamous cell carcinoma of one patient, 1x primary squamous cell carcinoma and 1x recurrence). In two patients each GOF (”hot spot”) TP53 gene mutations were detected at the following codons: R248Q (both primary and recurrent squamous cell carcinoma of one patient and 1x recurrent squamous cell carcinoma), R273H (1x primary squamous cell carcinoma and 1x recurrent squamous cell carcinoma), R248W and R282W (2x recurrent squamous cell carcinomas). The remaining hot spot mutations and gain or loss-of-function mutations occurred only once (see Tables 2 and 3).
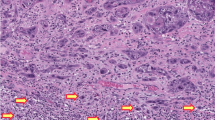
Strong nuclear staining of invasive tumor cells with antibody to p53 in immunohistochemical analysis was identified in 12/17 squamous cell carcinomas with missense TP53 gene mutations, while no staining was observed in the five squamous cell carcinomas with LOF-TP53 gene mutations. Squamous cell carcinomas with wild-type p53 were either negative or only individual nuclei of the cancer cells stained weakly positive.
Length of disease-free survival
The overall median length of disease-free interval until the first invasive recurrent squamous cell carcinoma of all patients was median 46 months (range 12-180 months), but intervals were 33 months within the TP53 gene mutated squamous cell carcinoma group and 65 months in the patient group with p53 wild-type squamous cell carcinomas. Disease-free intervals of > 5 years (60–180 months) were observed in 10/24 patients (42%; five patients each with a p53 wild-type primary squamous cell carcinomas (5/7 = 71%) and TP53 gene mutated squamous cell carcinomas (5/17 = 29%)). All but two of these recurrent squamous cell carcinomas after 5 years showed a change of mutational status. All patients with long intervals > 5 years had a surgically treated squamous cell carcinoma without regional lymph node metastases, or individual tumor cells and micro-metastases only. Extent of surgery, however, varied greatly from radical (hemi) vulvectomies to wide excisions owing to the recent trend towards conservative surgical treatment.
Discussion
In this first chronological documentation of the TP53 gene mutational status in recurrent HPV-negative vulvar cancers, we show that vulvar squamous cell carcinomas with and without TP53 gene mutations recur in the residual dermatosis, but that disease-free intervals differ greatly between patients with TP53 gene mutated primary squamous cell carcinomas (33 months) and patients with p53 wild-type squamous cell carcinomas (65 months). Long disease-free intervals > 5 years were observed in 42% of patients, and were over represented in patients with p53 wild-type primary squamous cell carcinomas (71%) when compared to TP53 gene mutated squamous cell carcinomas (29%). Interestingly, 80% recurrences after ≥ 5 years showed a change of mutational status which we interpret as de-novo carcinogenesis.
The majority of TP53 gene mutated cancers had a single TP53 gene mutation. The presence of multiple TP53 gene mutations suggests multiple independent genetic events within one squamous cell carcinoma, while identical TP53 gene mutations in primary and recurrent vulvar squamous cell carcinomas are indicative of clonal / genetic origin. The majority of TP53 gene mutated squamous cell carcinomas in our study, however, recurred with different, partly more complex TP53 gene mutations, i.e. LOF mutations and GOF (hot spot) missense TP53 gene mutations and/or multiple TP53 gene mutations were more common in recurrent squamous cell carcinomas. The distribution of GOF “hot spot” mutations in primary and recurrent vulvar squamous cell carcinomas was similar as in human tumors in general, with R175H and R273C being most common. It is also interesting that almost 60% of patients with p53 wild-type 1° squamous cell carcinoma had TP53 gene mutations in the recurrent squamous cell carcinomas. Our observations are in line with investigations of exons 2-11 of the TP53 gene of 11 HPV-negative precursor lesions differentiated vulvar intraepithelial neoplasia revealing different TP53 gene mutations in distinct areas within one clinical lesion of some but not all differentiated vulvar intraepithelial neoplasia as well as in associated invasive squamous cell carcinomas [19]. The increasing complexity and/ or new acquisition of TP53 gene mutations reflects an increased genetic fragility and instability in advanced untreated chronic inflammatory vulvar dermatoses rather than the initial carcinogenic event. This also has been suggested previously by detection of chromosome 17 aneusomy and polysomy in non-tumoral “normal “skin surrounding vulvar squamous cell carcinomas [20].
Nuclear accumulation of hyperstable mutant p53 protein as result of missense TP53 gene mutations can be demonstrated by immunohistochemical analysis with antibody to p53 as uniform nuclear staining/overexpression in tumor cells. Increased, but focal and discontinuous staining above the baseline level can occur in basal keratinocytes of hypertrophic vulvar lichenoid dermatosis after long duration of ischemia, repeated epithelial injury and regeneration, and chronic inflammation [21]. A chronic perpetuating inflammation/reactive T-lymphocytic proliferation to a yet unidentified antigen in lichen sclerosus, lichen planus and associated squamous cell carcinomas [22] may contribute to genomic instability [23, 24]. Treatment of inflammatory dermatoses aims at reduction of the inflammatory infiltrate [25, 26]. Reduction of disease activity / inflammatory infiltrate can be visualized by reduced p53 accumulation in the basal keratinocytes [27] and has a positive effect on cancer development [28].
Treatment of choice for vulvar cancer is surgical resection, but primary radiation or chemo-radiation is indicated in advanced stages [16]. As the cytoreductive effects of radiation and some chemotherapeutic regimens rely on an intact p53 pathway therapy resistance can be expected in TP53 gene mutated cancers [13, 29]. Therefore, analysis of TP53 gene mutations of vulvar squamous cell carcinoma may assist in planning individualized therapy. Pharmacological treatment of TP53 gene mutated cancers is still difficult, but research focuses on reactivating TP53 wild-type allele, and restoring or degrading mutant p53 [30,31,32]. The widely available synthetic lethal drug Paclitaxel for TP53 gene mutated cancers [33], however, has not been tested in vulvar squamous cell carcinomas. Interesting approaches include the inhibition of signaling pathways of glycolysis and lipid pathways, which are often upregulated as result of GOF TP53 gene mutation [34, 35].
In summary, despite the small numbers of patients in this retrospective study our results suggest that TP53 gene mutational status in primary and recurrent squamous cell carcinomas may serve as a prognostic marker predicting disease-free intervals. Although the clinical relevance is unclear at this point, TP53 gene mutational status may possibly assist in therapy planning and thus influence oncological outcome of HPV-negative squamous cell carcinomas.
References
Crum C, Herrington S, McCluggage WG, Regauer S, Wilkinson E. Tumours of the vulva. Epithelial tumours. In: Kurman RJ, Carcangiu ML, Herrington CS, Young RH, (eds). World Health Organisation, classification of tumours of the female genital tract. 4 edn. Lyon: IARC; 2014. p. 232–6.
Regauer S, Reich O, Eberz B. Vulvar cancers in women with vulvar lichen planus: a clinicopathological study. J Am Acad Dermatol. 2014;71:698–707.
de Sanjose S, Alemany L, Ordi J, et al. Worldwide human papillomavirus genotype attribution in over 2000 cases of intraepithelial and invasive lesions of the vulva. Eur J Cancer. 2013;49:3450–61.
Regauer S. Residual anogenital lichen sclerosus after cancer surgery has a high risk for recurrence: a clinicopathological study of 75 women. Gynecol Oncol. 2011;123:289–94.
Kashofer K, Regauer S. Analysis of full coding sequence of the TP53 gene in invasive vulvar cancers: implications for therapy. Gynecol Oncol. 2017;146:314–8.
Erber R, Conradt C, Homann N, et al. TP53 DNA contact mutations are selectively associated with allelic loss and have a strong clinical impact in head and neck cancer. Oncogene. 1998;16:1671–9.
Fakhry C, Westra WH, Li S, et al. Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst. 2008;100:261–9.
Lin BM, Wang H, D’Souza G, et al. Long-term prognosis and risk factors among patients with HPV-associated oropharyngeal squamous cell carcinoma. Cancer. 2013;119:3462–71.
Zhou G, Liu Z, Myers JN. TP53 mutations in head and neck squamous cell carcinoma and their impact on disease progression and treatment response. J Cell Biochem. 2016;117:2682–92.
Wakeham K, Kavanagh K, Cuschieri K, et al. HPV status and favourable outcome in vulvar squamous cancer. Int J Cancer. 2017;140:1134–46.
Rasmussen CL, Sand FL, Hoffmann Frederiksen M, Andersen KK, Kjær SK. Does HPV status influence survival after vulvar cancer? Int J Cancer. 2018;142:1158–65.
McAlpine JN, Leung SCY, Cheng A, et al. Human papillomavirus (HPV)-independent vulvar squamous cell carcinoma has a worse prognosis than HPV-associated disease: a retrospective cohort study. Histopathology. 2017;71:238–46.
Acedo P, Zawacka-Pankau J. p53 family members - important messengers in cell death signaling in photodynamic therapy of cancer? Photochem Photobiol Sci. 2015;14:1390–6.
He C, Li L, Guan X, Xiong L, Miao X. Mutant p53 gain of function and chemoresistance: the role of mutant p53 in response to clinical. Chemother Chemother. 2017;62:43–53.
Hacker NF, Eifel PJ, van der Velden J. Cancer of the vulva. Int J Gynaecol Obstet. 2015;131(Suppl 2):S76–83.
Oonk MHM, Planchamp F, Baldwin P, et al. European Society of Gynaecological Oncology guidelines for the management of patients with vulvar cancer. Int J Gynecol Cancer. 2017;27:832–7.
Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010;38:e164.
Cingolani P, Platts A, Wang le L, et al. A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strainw1118; iso-2; iso-3. Fly (Austin). 2012;6:80–92.
Pinto AP, Miron A, Yassin Y, et al. Differentiated vulvar intraepithelial neoplasia contains Tp53 mutations and is genetically linked to vulvar squamous cell carcinoma. Mod Pathol. 2010;23:404–12.
Carlson JA, Healy K, Tran TA, et al. Chromosome 17 aneusomy detected by fluorescence in situ hybridization in vulvar squamous cell carcinomas and synchronous vulvar skin. Am J Pathol. 2000;157:973–83.
Liegl B, Regauer S. p53 immunostaining in lichen sclerosus is related to ischaemic stress and is not a marker of differentiated vulvar intraepithelial neoplasia (d-VIN). Histopathology. 2006;48:268–74.
Regauer S, Reich O, Beham-Schmid C. Monoclonal gamma T-cell receptor rearrangement in vulvar lichen sclerosus and squamous cell carcinomas. Am J Pathol. 2002;160:1035–45.
Federico A, Morgillo F, Tuccillo C, Ciardiello F, Loguercio C. Chronic inflammation and oxidative stress in human carcinogenesis. Int J Cancer. 2007;121:2381–6.
Gonda TA, Tu S, Wang TC. Chronic inflammation, the tumor microenvironment and carcinogenesis. Cell Cycle. 2009;8:2005–13.
Neill SM, Tatnall FM, Cox NH. Guidelines for the management of lichen sclerosus. Br J Dermatol. 2002;147:640–9.
Kirtschig G, Becker K, Gunthert A, et al. Evidence-based (S3) guideline on (anogenital) Lichen sclerosus. J Eur Acad Dermatol Venereol. 2015;29:e1–43.
Nissi R, Kotila V, Knuuti E, Vare PO, Kauppila S. Altered p53 and Bcl-2 expression in keratinocytes of vulvar lichen sclerosus during pimecrolimus treatment. Br J Dermatol. 2009;161:958–60.
Lee A, Bradford J, Fischer G. Long-term management of adult vulvar Lichen Sclerosus: a prospective cohort study of 507 women. JAMA Dermatol. 2015;151:1061–7.
Bunz F, Hwang PM, Torrance C, et al. Disruption of p53 in human cancer cells alters the responses to therapeutic agents. J Clin Invest. 1999;104:263–9.
Wang Z, Sun Y. Targeting p53 for novel anticancer therapy. Transl Oncol. 2010;3:1–12.
Muller PA, Vousden KH. Mutant p53 in cancer: new functions and therapeutic opportunities. Cancer Cell. 2014;25:304–17.
Napoli M, Flores ER. The p53 family orchestrates the regulation of metabolism: physiological regulation and implications for cancer therapy. Br J Cancer. 2017; 116:149–51
Weinstein JN, Myers TG, O’Connor PM, et al. An information-intensive approach to the molecular pharmacology of cancer. Science. 1997;275:343–9.
Jeong YK, Kim MS, Lee JY, Kim EH, Ha H. Metformin radiosensitizes p53-deficient colorectal cancer cells through induction of G2/M arrest and inhibition of DNA repair proteins. PLoS One. 2015;10:e0143596.
Freed-Pastor W, Prives C. Targeting mutant p53 through the mevalonate pathway. Nat Cell Biol. 2016;18:1122–4.
Acknowledgements
Human Technology Interface Grant, County of Styria, GZ: ABT08-22-T-7/2013-23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Regauer, S., Kashofer, K. & Reich, O. Time series analysis of TP53 gene mutations in recurrent HPV-negative vulvar squamous cell carcinoma. Mod Pathol 32, 415–422 (2019). https://doi.org/10.1038/s41379-018-0141-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-018-0141-4