Key Points
-
Despite several advances, the pathogenesis of systemic autoinflammatory diseases (SAIDs) is only partially understood, and how mutations in causative genes lead to increased IL-1β secretion is unclear in many of these conditions
-
Circulating monocytes from patients with SAIDs are in a state of stress, possibly owing to the presence of mutated proteins
-
Levels of damage-associated molecular patterns (DAMPs) are increased in patients with SAIDs, and these concur with cytokines to generate amplifying loops that sustain inflammation
-
We propose that stress lowers the threshold for activation of immune cells in SAIDs, promoting oxidative stress with consequent loss of control of proinflammatory and anti-inflammatory cytokine production
-
Individual resistance to stress can explain the variable severity of the clinical manifestations in patients with SAIDs sharing the same mutation, and suggests that stress pathways could be a therapeutic target in these diseases
Abstract
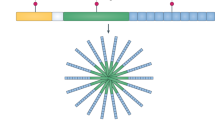
Inflammation is initiated by innate immune cell activation after contact with pathogens or tissue injury. An increasing number of observations have suggested that cellular stress, in the absence of infection or evident damage, can also induce inflammation. Thus, inflammation can be triggered by exogenous pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs)—so-called classic inflammation—or by endogenous stress resulting from tissue or cellular dysfunction. External triggers and cellular stress activate the same molecular pathways, possibly explaining why classic and stress-induced inflammation have similar clinical manifestations. In some systemic autoinflammatory diseases (SAIDs), inflammatory cells exhibit reduction–oxidation (redox) distress, having high levels of reactive oxygen species (ROS), which promote proinflammatory cytokine production and contribute to the subversion of mechanisms that self-limit inflammation. Thus, SAIDs can be viewed as a paradigm of stress-related inflammation, being characterized by recurrent flares or chronic inflammation (with no recognizable external triggers) and by a failure to downmodulate this inflammation. Here, we review SAID pathophysiology, focusing on the major cytokines and DAMPs, and on the key roles of redox distress. New therapeutic opportunities to tackle SAIDs by blocking stress-induced pathways and control the response to stress in patients are also discussed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
French FMF Consortium. A candidate gene for familial Mediterranean fever. Nat. Genet. 17, 25–31 (1997).
McDermott, M. F. et al. Germline mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes. Cell 97, 133–144 (1999).
Martinon, F. & Aksentijevich, I. New players driving inflammation in monogenic autoinflammatory diseases. Nat. Rev. Rheumatol. 11, 11–20 (2015).
Gattorno, M. & Martini, A. Beyond the NLRP3 inflammasome: autoinflammatory diseases reach adolescence. Arthritis Rheum. 65, 1137–1147 (2013).
Rubartelli, A. Redox control of NLRP3 inflammasome activation in health and disease. J. Leukoc. Biol. 92, 951–958 (2012).
Rubartelli, A. Autoinflammatory diseases. Immunol. Lett. 16, 226–230 (2014).
Bulua, A. C. et al. Mitochondrial reactive oxygen species promote production of proinflammatory cytokines and are elevated in TNFR1-associated periodic syndrome (TRAPS). J. Exp. Med. 208, 519–533 (2011).
Omenetti, A. et al. Increased NLRP3-dependent interleukin 1β secretion in patients with familial Mediterranean fever: correlation with MEFV genotype. Ann. Rheum. Dis. 73, 462–469 (2014).
van der Burgh, R. et al. Defects in mitochondrial clearance predispose human monocytes to interleukin-1β hypersecretion. J. Biol. Chem. 289, 5000–5012 (2014).
Frosch, M. et al. The myeloid-related proteins 8 and 14 complex, a novel ligand of toll-like receptor 4, and interleukin-1β form a positive feedback mechanism in systemic-onset juvenile idiopathic arthritis. Arthritis Rheum. 60, 883–891 (2009).
Hotamisligil, G. S. Inflammation and metabolic disorders. Nature 444, 860–867 (2006).
Dinarello, C. A. Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood 117, 3720–3732 (2011).
Carta, S., Lavieri, R. & Rubartelli, A. Different members of the IL-1 family come out in different ways: DAMPs vs. cytokines? Front. Immunol. 4, 1–9 (2013).
Arend, W. P., Malyak, M., Guthridge, C. J. & Gabay, C. Interleukin-1 receptor antagonist: role in biology. Annu. Rev. Immunol. 16, 27–55 (1998).
Dinarello, C. A. The role of the interleukin-1-receptor antagonist in blocking inflammation mediated by interleukin-1. N. Engl. J. Med. 343, 732–734 (2000).
Varga, G. et al. Glucocorticoids induce an activated, anti-inflammatory monocyte subset in mice that resembles myeloid-derived suppressor cells. J. Leukoc. Biol. 84, 644–650 (2008).
Varga, G. et al. Immune suppression via glucocorticoid-stimulated monocytes: a novel mechanism to cope with inflammation. J. Immunol. 193, 1090–1099 (2014).
Goldbach-Mansky, R. et al. Neonatal-onset multisystem inflammatory disease responsive to interleukin-1β inhibition. N. Engl. J. Med. 355, 581–592 (2006).
Gattorno, M. et al. Pattern of interleukin-1β secretion in response to lipopolysaccharide and ATP before and after interleukin-1 blockade in patients with CIAS1 mutations. Arthritis Rheum. 56, 3138–3148 (2007).
Lachmann, H. J. et al. Use of canakinumab in the cryopyrin-associated periodic syndrome. N. Engl. J. Med. 360, 2416–2425 (2009).
Hoffman, H. M. et al. Efficacy and safety of rilonacept (interleukin-1 trap) in patients with cryopyrin-associated periodic syndromes: results from two sequential placebo-controlled studies. Arthritis Rheum. 58, 2443–2452 (2008).
Aksentijevich, I. et al. An autoinflammatory disease with deficiency of the interleukin-1-receptor antagonist. N. Engl. J. Med. 360, 2426–2437 (2009).
Carta, S. et al. Deficient production of IL-1 receptor antagonist and IL-6 coupled to oxidative stress in cryopyrin-associated periodic syndrome monocytes. Ann. Rheum. Dis. 71, 1577–1581 (2012).
Rubartelli, A., Cozzolino, F., Talio, M. & Sitia, R. A novel secretory pathway for interleukin-1β, a protein lacking a signal sequence. EMBO J. 9, 1503–1510 (1990).
Agostini, L. et al. NALP3 forms an IL-1β-processing inflammasome with increased activity in Muckle-Wells autoinflammatory disorder. Immunity 20, 319–325 (2004).
Dinarello, C. et al. IL-1 family nomenclature. Nat. Immunol. 11, 973 (2010).
Marrakchi, S. et al. Interleukin-36-receptor antagonist deficiency and generalized pustular psoriasis. N. Engl. J. Med. 365, 620–628 (2011).
Tassi, S. et al. Altered redox state of monocytes from cryopyrin-associated periodic syndromes causes accelerated IL-1β secretion. Proc. Natl Acad. Sci. USA 107, 9789–9794 (2010).
Canna, S. W. et al. An activating NLRC4 inflammasome mutation causes autoinflammation with recurrent macrophage activation syndrome. Nat. Genet. 46, 1140–1146 (2014).
Romberg, N. et al. Mutation of NLRC4 causes a syndrome of enterocolitis and autoinflammation. Nat. Genet. 46, 1135–1139 (2014).
Carta, S. et al. Cell stress increases ATP release in NLRP3 inflammasome-mediated autoinflammatory diseases resulting in cytokine imbalance. Proc. Natl Acad. Sci. USA 112, 2835–2840 (2015).
Chen, C. J. et al. Identification of a key pathway required for the sterile inflammatory response triggered by dying cells. Nat. Med. 13, 851–856 (2007).
Eigenbrod, T., Park, J. H., Harder, J., Iwakura, Y. & Núñez, G. Cutting edge: critical role for mesothelial cells in necrosis-induced inflammation through the recognition of IL-1α released from dying cells. J. Immunol. 181, 8194–8198 (2008).
Mandinova, A. et al. S100A13 mediates the copper-dependent stress-induced release of IL-1α from both human U937 and murine NIH 3T3 cells. J. Cell Sci. 116, 2687–2696 (2003).
Keller, M., Rüegg, A., Werner, S. & Beer, H. D. Active caspase-1 is a regulator of unconventional protein secretion. Cell 132, 818–831 (2008).
Gross, O. et al. Inflammasome activators induce interleukin-1α secretion via distinct pathways with differential requirement for the protease function of caspase-1. Immunity 36, 388–400 (2012).
Rubartelli, A. & Lotze, M. T. Inside, outside, upside down: damage-associated molecular-pattern molecules (DAMPs) and redox. Trends Immunol. 28, 429–436 (2007).
Matzinger, P. Tolerance, danger, and the extended family. Annu. Rev. Immunol. 12, 991–1045 (1994).
Bianchi, M. E. HMGB1 loves company. J. Leukoc. Biol. 86, 573–576 (2009).
Mellins, E. D. Macaubas, C. & Grom, A. A. Pathogenesis of systemic juvenile idiopathic arthritis: some answers, more questions. Nat. Rev. Rheumatol. 7, 416–426 (2011).
Kessel, C., Holzinger, D. & Foell, D. Phagocyte-derived S100 proteins in autoinflammation: putative role in pathogenesis and usefulness as biomarkers. Clin. Immunol. 147, 229–241 (2013).
Li, G., Tang, D. & Lotze M. T. Ménage à trois in stress: DAMPs, redox and autophagy. Semin. Cancer Biol. 23, 380–390 (2013).
Ghavami, S. et al. S100A8/A9 induces autophagy and apoptosis via ROS-mediated cross-talk between mitochondria and lysosomes that involves BNIP3. Cell Res. 20, 314–331 (2010).
Hewinson, J., Moore, S. F. Glover, C. Watts, A. G. & MacKenzie, A. B. A key role for redox signaling in rapid P2X7 receptor-induced IL-1β processing in human monocytes. J. Immunol. 180, 8410–8420 (2008).
Cruz, C. M. et al. ATP activates a reactive oxygen species-dependent oxidative stress response and secretion of proinflammatory cytokines in macrophages. J. Biol. Chem. 282, 2871–2879 (2007).
Wang, H. et al. HMG-1 as a late mediator of endotoxin lethality in mice. Science 285, 248–251 (1999).
Scaffidi, P., Misteli, T. & Bianchi, M. E. Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature 418, 191–195 (2002).
Foell, D., Wittkowski, H., Vogl, T. & Roth, J. S100 proteins expressed in phagocytes: a novel group of damage-associated molecular pattern molecules. J. Leukoc. Biol. 81, 28–37 (2007).
Bours, M. J., Swennen, E. L., Di Virgilio, F., Cronstein, B. N. & Dagnelie, P. C. Adenosine 5′-triphosphate and adenosine as endogenous signaling molecules in immunity and inflammation. Pharmacol. Ther. 112, 358–404 (2006).
Harris, H. E., Andersson, U. & Pisetsky, D. S. HMGB1: a multifunctional alarmin driving autoimmune and inflammatory disease. Nat. Rev. Rheumatol. 8, 195–202 (2012).
Gardella S. et al. The nuclear protein HMGB1 is secreted by monocytes via a non-classical, vesicle-mediated secretory pathway. EMBO Rep. 3, 995–1001 (2002).
Tang, D. et al. Hydrogen peroxide stimulates macrophages and monocytes to actively release HMGB1. J. Leuk. Biol. 81, 741–747 (2007).
Yang, H. et al. Programmed necrosis induced by asbestos in human mesothelial cells causes high-mobility group box 1 protein release and resultant inflammation. Proc. Natl Acad. Sci. USA 107, 12611–12616 (2010).
Apetoh, L. Toll-like receptor 4-dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nat. Med. 13, 1050–1059 (2007).
Thorburn, J. et al. Autophagy regulates selective HMGB1 release in tumor cells that are destined to die. Cell Death Differ. 16, 175–183 (2009).
Hori, O. et al. The receptor for advanced glycation end products (RAGE) is a cellular binding site for amphoterin. Mediation of neurite outgrowth and co-expression of rage and amphoterin in the developing nervous system. J. Biol. Chem. 270, 25752–25761 (1995).
Park, J. S. et al. High mobility group box 1 protein interacts with multiple Toll-like receptors. Am. J. Physiol. Cell Physiol. 290, C917–C924 (2006).
Yang, H. et al. A critical cysteine is required for HMGB1 binding to Toll-like receptor 4 and activation of macrophage cytokine release. Proc. Natl Acad. Sci. USA 107, 11942–11947 (2010).
Yang, H. et al. Redox modification of cysteine residues regulates the cytokine activity of high mobility group box-1 (HMGB1). Mol. Med. 18, 250–259 (2012).
Schiraldi, M. et al. HMGB1 promotes recruitment of inflammatory cells to damaged tissues by forming a complex with CXCL12 and signaling via CXCR4. J. Exp. Med. 209, 551–563 (2012).
Venereau, E. et al. Mutually exclusive redox forms of HMGB1 promote cell recruitment or proinflammatory cytokine release. J. Exp. Med. 209, 1519–1528 (2012).
Park, H. S. et al. Cutting edge: direct interaction of TLR4 with NAD(P)H oxidase 4 isozyme is essential for lipopolysaccharide-induced production of reactive oxygen species and activation of NF-κB. J. Immunol. 173, 3589–3593 (2004).
Taniguchi, N. et al. High mobility group box chromosomal protein 1 plays a role in the pathogenesis of rheumatoid arthritis as a novel cytokine. Arthritis Rheum. 48, 971–981 (2003).
Kokkola, R. et al. Successful treatment of collagen-induced arthritis in mice and rats by targeting extracellular high mobility group box chromosomal protein 1 activity. Arthritis Rheum. 48, 2052–2058 (2003).
Hamada, T. et al. Extracellular high mobility group box chromosomal protein 1 is a coupling factor for hypoxia and inflammation in arthritis. Arthritis Rheum. 58, 2675–2685 (2008).
Lundbäck, P. et al. Characterization of the inflammatory properties of actively released HMGB1 in juvenile idiopathic arthritis. Antioxid. Redox Signal. http://dx.doi.org/10.1089/ars.2014.6039.
De Benedetti, F. et al. Randomized trial of tocilizumab in systemic juvenile idiopathic arthritis. N. Engl. J. Med. 367, 2385–2395 (2012).
Willingham, S. B. et al. Microbial pathogen-induced necrotic cell death mediated by the inflammasome components CIAS1/cryopyrin/NLRP3 and ASC. Cell Host Microbe 2, 147–159 (2007).
Nacken, W., Roth, J., Sorg, C. & Kerkhoff, C. S100A9/S100A8: myeloid representatives of the S100 protein family as prominent players in innate immunity. Microsc. Res. Tech. 60, 569–580 (2003).
Niki, I., Yokokura, H., Sudo, T., Kato, M. & Hidaka, H. Ca2+ signaling and intracellular Ca2+ binding proteins. J. Biochem. 120, 685–698 (1996).
Steinbakk, M. et al. Antimicrobial actions of calcium binding leucocyte L1 protein, calprotectin. Lancet 336, 763–765 (1990).
Vogl, T. et al. S100A12 is expressed exclusively by granulocytes and acts independently from MRP8 and MRP14. J. Biol. Chem. 274, 25291–25296 (1999).
Vogl, T. et al. Mrp8 and Mrp14 are endogenous activators of Toll-like receptor 4, promoting lethal, endotoxin-induced shock. Nat. Med. 13, 1042–9 (2007).
Foell, D. et al. Proinflammatory S100A12 can activate human monocytes via Toll-like receptor 4. Am. J. Respir. Crit. Care Med. 187, 1324–1334 (2013).
Rammes, A. et al. Myeloid-related protein (MRP) 8 and MRP14, calcium-binding proteins of the S100 family, are secreted by activated monocytes via a novel, tubulin-dependent pathway. J. Biol. Chem. 272, 9496–9502 (1997).
Wittkowski, H. et al. S100A12 is a novel molecular marker differentiating systemic-onset juvenile idiopathic arthritis from other causes of fever of unknown origin. Arthritis Rheum. 58, 3924–3931 (2008).
Kallinich, T., Wittkowski, H., Keitzer, R., Roth, J. & Foell, D. Neutrophil-derived S100A12 as novel biomarker of inflammation in familial Mediterranean fever. Ann. Rheum. Dis. 69, 677–682 (2010).
Foell, D. et al. Monitoring neutrophil activation in juvenile rheumatoid arthritis by S100A12 serum concentration. Arthritis Rheum. 50, 1286–1295 (2004).
Lin, Y. T., Wang, C. T., Gershwin, M. E. & Chiang, B. L. The pathogenesis of oligoarticular/polyarticular vs systemic juvenile idiopathic arthritis. Autoimmun. Rev. 10, 482–489 (2011).
Wittkowski, H. et al. MRP8 and MRP14, phagocyte-specific danger signals, are sensitive biomarkers of disease activity in cryopyrin-associated periodic syndromes. Ann. Rheum. Dis. 70, 2075–2081 (2011).
Giuliani, F., Grieve, A. & Rabouille C. Unconventional secretion: a stress on GRASP. Curr. Opin. Cell. Biol. 23, 498–504 (2011).
Holzinger, D. The Toll-like receptor 4 agonist MRP8/14 protein complex is a sensitive indicator for disease activity and predicts relapses in systemic-onset juvenile idiopathic arthritis. Ann. Rheum. Dis. 71, 974–980 (2012).
Kolly, L. et al. Periodic fever, aphthous stomatitis pharyngitis, cervical adenitis syndrome is linked to dysregulated monocyte IL-1β production. J. Allergy Clin. Immunol. 131, 1635–1643 2013).
Gombault, A., Baron, L. & Couillin, I. ATP release and purinergic signaling in NLRP3 inflammasome activation. Front. Immunol. 3, 414 (2013).
Lazarowski, E. R., Boucher, R. C. & Harden, T. K. Mechanisms of release of nucleotides and integration of their action as P2X- and P2Y-receptor activating molecules. Mol. Pharmacol. 64, 785–795 (2003).
Praetorius, H. A. & Leipziger, J. ATP release from non-excitable cells. Purinergic Signal. 5, 433–446 (2009).
Lavieri, R. et al. TLR costimulation causes oxidative stress with unbalance of proinflammatory and anti-inflammatory cytokine production. J. Immunol. 192, 5373–5381 (2014).
Iyer, S. S. et al. Necrotic cells trigger a sterile inflammatory response through the Nlrp3 inflammasome. Proc. Natl Acad. Sci. USA 106, 20388–20393 (2009).
Antonioli, L., Pacher, P., Vizi, E. S. & Haskó, G. CD39 and CD73 in immunity and inflammation. Trends Mol. Med. 19, 355–367 (2013).
Piccini, A. et al. ATP is released by monocytes stimulated with pathogen-sensing receptor ligands and induces IL-1β and IL-18 secretion in an autocrine way. Proc. Natl Acad. Sci. USA 105, 8067–8072 (2008).
Cannon, W. B. “Physiological regulation of normal states: some tentative postulates concerning biological homeostatics” in Jubilee Volume for Charles Richet 91–93 (Paris: Les Éditions Médicales, 1926).
Rubartelli, A. & Sitia, R. Stress as an intercellular signal: the emergence of stress-associated molecular patterns (SAMP). Antioxid. Redox. Signal. 11, 2621–2629 (2009).
Pal, R. et al. Src-dependent impairment of autophagy by oxidative stress in a mouse model of Duchenne muscular dystrophy. Nat. Commun. 5, 4425 (2014).
Luciani, A. et al. Defective CFTR induces aggresome formation and lung inflammation in cystic fibrosis through ROS-mediated autophagy inhibition. Nat. Cell Biol. 12, 863–875 (2010).
Tassi, S. et al. Pathogen-induced interleukin-1β processing and secretion is regulated by a biphasic redox response. J. Immunol. 183, 1456–1462 (2009).
Gloire, G., Legrand-Poels, S. & Piette, J. NF-κB activation by reactive oxygen species: fifteen years later. Biochem. Pharmacol. 72, 1493–1505 (2006).
Martinon, F. Signaling by ROS drives inflammasome activation. Eur. J. Immunol. 40, 616–619 (2010).
Zhou, R., Yazdi, A. S., Menu, P. & Tschopp, J. A role for mitochondria in NLRP3 inflammasome activation. Nature 469, 221–225 (2011).
Harijith, A., Ebenezer, D. L. & Natarajan, V. Reactive oxygen species at the crossroads of inflammasome and inflammation. Front. Physiol. 5, 352 (2014).
Meissner, F., Molawi, K. & Zychlinsky, A. Superoxide dismutase 1 regulates caspase-1 and endotoxic shock. Nat. Immunol. 9, 866–872 (2008).
Zhao, C., Gillette, D. D., Li, X, Zhang, Z. & Wen, H. Nuclear factor E2-related factor-2 (Nrf2) is required for NLRP3 and AIM2 inflammasome activation. J. Biol. Chem. 289, 17020–17029 (2014).
Borghini, S. et al. Clinical presentation and pathogenesis of cold-induced autoinflammatory disease in a family with recurrence of an NLRP12 mutation. Arthritis Rheum. 63, 830–839 (2011).
Sundqvist, M. et al. Increased intracellular oxygen radical production in neutrophils during febrile episodes of periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis syndrome. Arthritis Rheum. 65, 2971–2983 (2013).
Simon, A. et al. Concerted action of wild-type and mutant TNF receptors enhances inflammation in TNF receptor 1-associated periodic fever syndrome. Proc. Natl Acad. Sci. USA 107, 9801–9806 (2010).
Silva, J. M., Wong, A., Carelli, V. & Cortopassi, G. A. Inhibition of mitochondrial function induces an integrated stress response in oligodendroglia. Neurobiol. Dis. 34, 357–365 (2009).
Grant, C. M. Regulation of translation by hydrogen peroxide. Antioxid. Redox Signal. 15, 191–203 (2011).
Rice, G. I. et al. Gain-of-function mutations in IFIH1 cause a spectrum of human disease phenotypes associated with upregulated type I interferon signaling. Nat. Genet. 46, 503–509 (2014).
Crow, Y. J. Type I interferonopathies: mendelian type I interferon up-regulation. Curr. Opin. Immunol. 32, 7–12 (2015).
Ahn, J. & Barber, G. N. Self-DNA, STING-dependent signaling and the origins of autoinflammatory disease. Curr. Opin. Immunol. 31, 121–126 (2014).
Liu, Y. et al. Mutations in proteasome subunit β type 8 cause neutrophilic dermatosis with lipodystrophy and elevated temperature with evidence of genetic and phenotypic heterogeneity. Arthritis Rheum. 64, 895–907 (2012).
Liu, Y. et al. Activated STING in a vascular and pulmonary syndrome. N. Engl. J. Med. 371, 507–518 (2014).
Bennett, L. Interferon and granulopoiesis signatures in systemic lupus erythematosus blood. J. Exp. Med. 197, 711–723 (2003).
Savva, A. & Roger, T. Targeting toll-like receptors: promising therapeutic strategies for the management of sepsis-associated pathology and infectious diseases. Front. Immunol. 4, 387 (2013).
Cauwels, A., Rogge, E., Vandendriessche, B., Shiva, S. & Brouckaert, P. Extracellular ATP drives systemic inflammation, tissue damage and mortality. Cell. Death Dis. 5, e1102 (2014).
Mehta, N. et al. Purinergic receptor P2X7: a novel target for anti-inflammatory therapy. Bioorg. Med. Chem. 22, 54–88 (2014).
Ramprasath, T. & Selvam, G. S. Potential impact of genetic variants in Nrf2 regulated antioxidant genes and risk prediction of diabetes and associated cardiac complications. Curr. Med. Chem. 20, 4680–4693 (2013).
Medzhitov, R., Schneider, D. S. & Soares, M. P. Disease tolerance as a defense strategy. Science 335, 936–941 (2012).
Carta, S. et al. The rate of interleukin-1β secretion in different myeloid cells varies with the extent of redox response to Toll-like receptor triggering. J. Biol. Chem. 286, 27069–27080 (2011).
Janssens, S., Pulendran, B. & Lambrecht, B. N. Emerging functions of the unfolded protein response in immunity. Nat. Immunol. 15, 910–919 (2014).
Adolph, T. E. et al. Paneth cells as a site of origin for intestinal inflammation. Nature 503, 272–276 (2013).
Hotamisligil, G. S. Endoplasmic reticulum stress and the inflammatory basis of metabolic disease. Cell 140, 900–917 (2010).
Osorio, F., Lambrecht, B. & Janssens, S. The UPR and lung disease. Semin. Immunopathol. 35, 293–306 (2013).
Martinon, F., Chen, X., Lee, A.-H. & Glimcher, L. H. TLR activation of the transcription factor XBP1 regulates innate immune responses in macrophages. Nat. Immunol. 11, 411–418 (2010).
Savic, S. et al. TLR dependent XBP-1 activation induces an autocrine loop in rheumatoid arthritis synoviocytes. J. Autoimmun. 50, 59–66 (2014).
Qiu, Q. et al. Toll-like receptor-mediated IRE1α activation as a therapeutic target for inflammatory arthritis. EMBO J. 32, 2477–2490 (2013).
Rubartelli, A., Gattorno, M., Netea, M. G. & Dinarello, C. A. Interplay between redox status and inflammasome activation. Trends Immunol. 32, 559–66 (2011).
D'Antonio, M. et al. Resetting translational homeostasis restores myelination in Charcot-Marie-Tooth disease type 1B mice. J. Exp. Med. 210, 821–838 (2013).
Ayala-Peña, S. Role of oxidative DNA damage in mitochondrial dysfunction and Huntington's disease pathogenesis. Free Radic. Biol. Med. 62, 102–110 (2013).
Lei, Y. et al. Redox regulation of inflammation: old elements, a new story. Med. Res. Rev. 35, 306–340 (2015).
Bachetti, T. et al. Autophagy contributes to inflammation in patients with TNFR-associated periodic syndrome (TRAPS). Ann. Rheum. Dis. 72, 1044–1052 (2013).
Palmblad, K. et al. High systemic levels of the cytokine-inducing HMGB1 isoform secreted in severe macrophage activation syndrome. Mol. Med. 20, 538–547 (2014).
Andersson, U. & Tracey, K. J. HMGB1 is a therapeutic target for sterile inflammation and infection. Annu. Rev. Immunol. 29, 139–162 (2011).
Steinckwich, N., Schenten, V., Melchior, C., Bréchard, S. & Tschirhart, E. J. An essential role of STIM1, Orai1, and S100A8-A9 proteins for Ca2+ signaling and FcγR-mediated phagosomal oxidative activity. J. Immunol. 186, 2182–2191 (2011).
Foell, D., Wittkowski, H. & Roth, J. Mechanisms of disease: a “DAMP” view of inflammatory arthritis. Nat. Clin. Pract. Rheumatol. 3, 382–390 (2007).
Ferrari, D. et al. The P2X7 receptor: a key player in IL-1 processing and release. J. Immunol. 176, 3877–3883 (2006).
Acknowledgements
The authors' work is supported in part by the Italian Ministry of Health (M.G., A.R.), by Telethon, Italy (grant n. GGP14144; M.G., A.R.) and by Associazione Italiana per la Ricerca sul Cancro (grant n. IG15434; A.R.).
Author information
Authors and Affiliations
Contributions
G.V. and A.R. reviewed and edited the manuscript before submission. All authors researched data for the article, made substantial contributions to discussion of content and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
M.G. has received lecture fees and institutional unrestricted grants from SoBi and Novartis; D.F. has received lecture fees from Chugai, Novartis, Pfizer, Roche and SoBi; A.R. has received lecture fees from SoBi and Novartis; G.V. declares no competing interests.
Rights and permissions
About this article
Cite this article
Varga, G., Gattorno, M., Foell, D. et al. Redox distress and genetic defects conspire in systemic autoinflammatory diseases. Nat Rev Rheumatol 11, 670–680 (2015). https://doi.org/10.1038/nrrheum.2015.105
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrrheum.2015.105
This article is cited by
-
Hydrogen peroxide release by bacteria suppresses inflammasome-dependent innate immunity
Nature Communications (2019)
-
Imaging findings of sterile pyogenic arthritis, pyoderma gangrenosum and acne (PAPA) syndrome: differential diagnosis and review of the literature
Pediatric Radiology (2019)
-
Anti-inflammatory monocytes—interplay of innate and adaptive immunity
Molecular and Cellular Pediatrics (2018)
-
Oxidation of Atg3 and Atg7 mediates inhibition of autophagy
Nature Communications (2018)
-
Basal autophagy prevents autoactivation or enhancement of inflammatory signals by targeting monomeric MyD88
Scientific Reports (2017)