Abstract
The risk of pancreatic cancer is increased in both Snus (the Swedish variant of oral smokeless tobacco) users and, to a greater extent, in cigarette smokers. Concurrent chronic pancreatitis further increases the risk in cigarette smokers. Little is known about the mechanism by which cigarette smoke or Snus increase the risk of pancreatic cancer in individuals with chronic pancreatitis. This study examined the carcinogenic effects of an aqueous extract of cigarette smoke (tobacco smoke, TS) or Snus in an Elastase-IL-1β transgenic mouse model of chronic pancreatitis. Both transgenic and wild-type (WT) mice were fed diluted TS water or Snus-containing diet for up to 15 months, and monitored for phenotypic and molecular changes in the pancreas. Both TS- and Snus-treated Elastase-IL-1β mice, but not WT mice, developed significant pancreatic ductal epithelial flattening and severe glandular atrophy compared with untreated transgenic mice. Ductal epithelial cells displayed a high proliferative index, minimal apoptosis, and induction of COX-2 in the setting of chronic inflammation. Up-regulation of TNF-α correlated with the onset of severe glandular atrophy. In comparison with Snus-treated mice, TS-Elastase-IL-1β mice had an earlier onset and a greater extent of phenotypic changes, which were associated with up-regulation of TNF-α and increased expression of IL-6, TGF-β, and SDF-1. Collectively, these findings provide new insights into the mechanism by which tobacco products are likely to promote carcinogenesis in the setting of chronic pancreatitis.
Similar content being viewed by others
Main
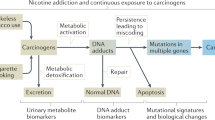
Cigarette smoking is a well-documented risk factor for pancreatic cancer.1, 2, 3 It increases the risk approximately threefold, and contributes to almost 30% of all cases.4, 5 An increasing body of evidence6, 7, 8, 9 suggests that use of oral smokeless tobacco also increases the risk of pancreatic cancer. The risk of pancreatic cancer was increased approximately twofold in people who used Snus, also known as Swedish moist oral snuff, compared with those who never used any tobacco products.7 Although the mechanisms underlying tobacco use and development of pancreatic cancer are not fully understood, many tobacco-derived chemicals, such as nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) and its metabolite 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL), are carcinogens. These carcinogens have been detected in human pancreatic juice at significantly higher concentration in smokers than in nonsmokers.10 NNK and its metabolites can also be found in the urine of Snus users.11, 12 Metabolites of NNK form DNA adducts and induce K-Ras mutations,13, 14, 15 which are believed to be critical in the initiation of pancreatic cancer. NNK is also known to activate COX-2 and β-adrenergic signaling pathways, which are important in carcinogenesis.16 The carcinogenicity of NNK or NNAL has been shown in animal models of pancreatic cancer.17, 18 Snus accelerated the development of gastric cancer in Helicobacter pylori-infected gastrin transgenic mice,19 providing additional evidence of Snus being carcinogenic in vivo.
Interestingly, there is epidemiological evidence that cigarette smoking may also be a risk factor for acute and chronic pancreatitis.20, 21, 22, 23, 24, 25, 26, 27, 28 The association between cigarette smoking and pancreatitis seemed to be both dose and duration dependent. The link between cigarette smoking and pancreatitis is also supported by the results of animal studies.29, 30, 31 For instance, exposure to high-dose cigarette smoke caused pancreatic inflammation including fibrosis and scarring of acini. Many chronic pancreatitis-associated genes, such as IL-1β and TGF-β, were found to be overexpressed.31
In addition, cigarette smoking was found to predispose to pancreatic cancer in a dose-dependent manner, especially in the setting of hereditary chronic pancreatitis.32 Although both chronic pancreatitis and tobacco consumption are independent risk factors for pancreatic cancer, little is known about potential interactions between the two. In this study, we have investigated the following hypotheses: cigarette smoke and Snus are carcinogenic in the pancreas; cigarette smoke is more carcinogenic than Snus; cigarette smoke or Snus cause inflammation in the pancreas and synergize with chronic pancreatitis in the development of pancreatic cancer. The effects of aqueous extracts of cigarette smoke (tobacco smoke, TS) or Snus on the pancreas gland were examined in Elastase-IL-1β mice, a transgenic model of chronic pancreatitis.33 These mice were established by overexpressing IL-1β, a proinflammatory cytokine, with a pancreas-specific promoter, the rat elastase promoter. The mice develop chronic pancreatitis at an early age that closely mimics that found in human beings.33 However, no preneoplastic or neoplastic lesions occur after >24 months of observation, suggesting that chronic pancreatitis per se may not be sufficient to induce pancreatic cancer in this model. The effects of TS water or Snus-containing diet were evaluated in Elastase-IL-1β and wild-type (WT) mice for up to 15 months. Our results suggest that tobacco is potentially carcinogenic to the pancreas in the setting of chronic inflammation.
MATERIALS AND METHODS
Generation of Elastase-IL-1β Mice
All animal procedures were performed according to the protocol (AC-AAAA9881) approved by the Institutional Animal Use and Care Committee of Columbia University. Elastase-IL-1β mice of line 12333 were mated with C57B/6 WT mice. Offspring were genotyped by PCR assays from tail DNA at 3–4 weeks of age as described earlier.33
Preparation of Aqueous Extract of Cigarette Smoke
Cigarettes (2R4F, Kentucky Tobacco Research Institute) were smoked in a Borgwaldt piston-controlled apparatus (Model RG-1, Hamburg, Germany) using a modification of the Federal Trade Commission standard protocol. The protocol variables were duration, 2 seconds/puff; frequency, 4 puffs per minute; and volume, 35 ml per puff. Cigarettes were smoked one at a time in the apparatus and the smoke drawn under sterile conditions into pre-measured amounts of sterile PBS (pH 7.4). The smoke in PBS represented whole trapped mainstream smoke. Quantification of smoke content was expressed in puffs/ml of PBS with one cigarette yielding about 20 puffs drawn into a 1 ml of volume. The final concentration of the aqueous extract of cigarette smoke was 40 puffs/ml.
Tobacco Treatment
There were eight groups of mice, 20–30 mice in each group, included in the study (Table 1). There were equal numbers of male and female mice within groups. At age of 5–8 weeks, mice were started on tobacco (TS or Snus) treatment or control diet (SDS diet, Special Diet Service, Witham, Essex, UK) or control water (PBS diluted by 1:100 in the regular drinking water). For TS-treated groups, the aqueous extract of cigarette smoke (40 puffs/ml) was diluted 1:100 in the regular drinking water. For Snus-treated groups, mice were fed with a Snus-containing diet similar to that reported earlier.19 In brief, Snus with the brand name General, one of the most popular brands in Sweden and Norway, was purchased over the counter. The Snus was mixed with powdered rodent SDS diet in 5, 7, or 9% (wt/wt), respectively, using an ordinary food processor, and then pelleted (Research Diets Inc., New Brunswick, NJ, USA). Mice were started with 5% Snus-containing diet, gradually advanced to 7% in 6 weeks, then 9% in another 6 weeks, and maintained on 9% for the rest of the study period.
Measurement of Urine Cotinine and Trans-3′-hydroxycotinine (3′-HC)
Urine samples from individual mice in each group were collected at different times. Concentrations of cotinine and 3′-HC in urine were determined using liquid chromatography-tandem mass spectrometry with a method similar to that published earlier.34 (Clinical Pharmacology Laboratory, University of California, San Francisco). In brief, deuterium-labeled cotinine and 3′-HC were used as the internal standards. The mass spectrometer was operated in the positive ion mode using the atmospheric pressure chemical ionization. Quantitation was achieved using selected reaction monitoring of the transitions m/z 177 to m/z 80 for cotinine and m/z 193 to m/z 80 for 3′-HC, and the transitions m/z 186 to m/z 84 and m/z 202 to m/z 84 for the respective internal standards. Calibration curves were constructed from peak area ratios of the analyte to its internal standard using linear regression. Standard curves were linear over the concentration range studied, 1–500 ng/ml. Between-run precision (percent coefficient of variation) of cotinine ranged from 2.7 to 6.1% and of 3′-HC ranged from 2.8 to 5.8%. Between-run accuracy (percent of expected values) of cotinine ranged from 89 to 104% and of 3′-HC ranged from 87 to 103% for concentrations ranging from 5 to 200 ng/ml. The limit of quantitation was 1 ng/ml for both cotinine and 3′-HC.
Blood and Tissue Sample Preparation
Four to seven mice were sacrificed at the designated time points, that is 4–6, 7–9, 10–12, and 13–15 months of treatment. Blood samples were collected by cardiac puncture, and serum was collected after centrifugation and stored at −80°C. Tissue samples from various organs (including pancreas, oral mucosa, lungs, bladder, stomach, colon, and kidneys) were dissected and collected. Tissues for histopathological observation were fixed for 24 h in 10% neutral buffered formalin, and processed and embedded in paraffin according to standard protocol. Thin sections (4 μm) were cut for H&E staining and for immunohistochemical staining. Tissues for mRNA assays were frozen immediately in liquid nitrogen. For RNA preparation, frozen samples were homogenized in Trizol reagent (Invitrogen, Carlsbad, CA, USA). RNA was extracted according to manufacturer's instructions (Qiagen, Valencia, CA, USA).
Histologic Scoring
H&E-stained sections were analyzed and chronic pancreatitis lesions were graded using a modified version of scores described earlier by Demols et al35 taking into account of the extent of inflammation, glandular atrophy, tubular complexes, and fibrosis. Scoring of glandular atrophy was modified by assigning a score of 4 to remarkably severe glandular atrophy, which involved >75% of acini.
Immunohistochemical Staining
Slides were de-paraffinized in xylene and endogenous peroxidase was blocked by incubation with 3% hydrogen peroxide in methanol when immunohistochemical staining was performed using the peroxidase reaction. Alternatively, slides were incubated with 20% acetic acid in methanol for 2 min, if the staining was to be revealed using the alkaline phosphatase reaction. Slides were rinsed and heated in 10 mM citrate buffer pH 6 in a boiling water bath for 20 min. Slides were rinsed in PBS Tween 0.05% and blocked for 30 min with 2% bovine serum albumin (Sigma-Aldrich, St Louis, MO, USA) in PBS. Primary antibodies and biotinylated secondary antibodies (Jackson Immunoresearch, West Grove, PA, USA) were diluted in 2% bovine serum albumin in PBS and incubated for 1 h each at the room temperature. Subsequently, slides were incubated with the alkaline phosphatase- or peroxidase-conjugated streptavidin (Dako North America, Carpinteria, CA, USA) and staining was revealed using the VectorRed substrate (Vector Laboratories, Burlingame, CA, USA, SK 5100) for the alkaline phosphatase, or 3, 3′-diaminobenzidine (Sigma-Aldrich) plus hydrogen peroxide for the peroxidase. Finally, slides were counterstained with hematoxylin and mounted. Primary antibodies included Ki67 (ABGENT, San Diego, #ab15580, 1/200), COX-2 (Cayman Chemical, Aachen, Germany, #160126, 1/200), α-smooth muscle actin (Dako North America, Inc., M0851, 1/200), desmin (Lab Vision, Fremont, CA, USA, #RB-9014, 1/200), and CD3e (Biosciences, San Jose, CA, USA, #553058, 1/200). When primary antibody was from the mouse, ARK kit (Dako North America, #K3954) was used according to the manufacturer's instructions.
Apoptosis quantification was performed using the TUNEL assay (Klenow Frageltm DNA fragmentation kit, Calbiochem, San Diego, CA, USA) according to the manufacturer's instructions.
Quantitative and Semi-quantitative RT–PCR
Reverse transcription of mRNA was performed on RNA from three to five mice in each group using the Superscript First-Strand Synthesis System III (Invitrogen, #18080-051) according to the manufacturer's instructions, and semi-quantitative PCR reactions were performed using a PCR Core kit (Roche). The resulting PCR products were analyzed by agarose gel electrophoresis. Quantitative real-time PCR was performed with a three-step method using an ABI 7300 system and QuantiTect SYBR Green PCR (Qiagen). The PCR conditions were as follows: 95°C for 3 min, followed by 40 cycles of 95°C for 15 s, 55°C for 30 s, and 72°C for 15 s. The sequences of primers are listed in Supplementary Table 1.
Measurement of Serum IL-6 Levels
The levels of mouse IL-6 in the serum of control and tobacco-treated mice were measured using an ELISA kit (BD Company, San Diego, CA, USA). Absorbance was measured at 450 nm by a Multiscan MC reader, and the samples were analyzed by the DELTA SOFT II software (BioMetallics, Inc., Princeton, NJ, USA).
Statistical Analysis
The χ2 test was used to compare the incidences of ductal epithelial flattening and severe acinar atrophy between Snus- and TS-treated groups. A P-value<0.05 was considered statistically significant.
In quantitative real-time RT–PCR and ELISA assays, the data was presented as mean±s.d. The t-test was used for statistical analysis. A P-value<0.05 was considered statistically significant.
RESULTS
Tobacco Treatment and Intake
To investigate whether chronic inflammation could increase the sensitivity of the pancreas to carcinogenic effects of tobacco, Elastase-IL-1β mice of line 123, which show moderate expression of human IL-1β,33 and WT mice were fed diluted TS water or Snus-containing diet for up to 15 months. Mice tolerated these tobacco products well without significant adverse effects, such as skin sensitivity, loss of hair, or weight loss. Throughout the study period, there were no significant differences in body weights between tobacco-treated and control groups of Elastase-IL-1β or WT mice.
As shown in Table 1, tobacco consumption was assessed by measuring levels of urinary cotinine and its metabolite, 3′-HC, biomarkers of nicotine exposure. In control PBS- and SDS-Elastase-IL-1β or WT mice, levels of urine cotinine and 3′-HC were minimal or below the limit of quantitation (BLQ) to 3.75±0.6 ng/ml and BLQ to 1.1 to BLQ to 3.3 ng/ml, respectively. In TS-treated mice, concentrations of urine cotinine and 3′-HC (93.5±24.5 to 145.2±13.0 ng/ml and 1102.6±44.9 to 1946.0±366.4 ng/ml) were >60 and 600 times, respectively, higher than those of control mice. The highest concentrations of urinary cotinine and 3′-HC were found in Snus-treated mice; levels were >70- and 200-fold higher, respectively, than those of TS-treated mice. There was either no significant or a very slight difference in levels of urinary cotinine and 3′-HC between tobacco-treated Elastase-IL-1β and WT mice.
TS- or Snus-Induced Significant Flattening of Pancreatic Ductal Epithelium in Elastase-IL-1β Mice
As described earlier,33 Elastase-IL-1β mice developed chronic pancreatitis at an early age. By 4 months of age, all mice developed severe chronic pancreatitis manifested by chronic inflammation, acinar atrophy, tubular complexes, and fibrosis. In comparison with cuboidal-shaped ductal cells in WT mice (Figure 1a), the epithelial cells in the pancreatic ducts of Elastase-IL-1β mice were columnar or slightly elongated cubic (Figure 1b). After 4 months of TS treatment, the ductal epithelium of the pancreas was significantly flattened in Elastase-IL-1β mice (Figure 1c). Nucleus-to-cytoplasm ratios of these cells were much higher than those of control transgenic mice. These epithelial changes were detected in 73% (16/22) of TS-treated Elastase-IL-1β mice. These changes were found in the main pancreatic ducts and >40% of segmental ducts. Similar changes in the ductal epithelium were found in Snus-treated Elastase-IL-1β mice. After 4–5 months of Snus treatment, ductal epithelial cells were flattened in a few main pancreatic ducts compared with age-matched control Elastase-IL-1β mice. Changes also occurred in the segmental ducts. These epithelial changes were present in 52% (15/29) of Snus-treated mice, statistically similar to that of TS-treated Elastase-IL-1β mice (P>0.05). By Ki67 immunohistochemical staining, these flattened ductal epithelial cells displayed a significantly higher proliferative index compared with those of age-matched control Elastase-IL-1β mice (Figure 1d). In contrast, TUNEL assays for apoptosis revealed little to no staining in the ductal epithelial cells (data not shown). Intra-epithelial infiltration of neutrophils was found in some of these ducts in both tobacco-treated and control Elastase-IL-1β mice (Figure 1c). There was no significant difference in intra-epithelial neutrophil infiltration between these groups. In 24% (7/29) of Snus-treated Elastase-IL-1β mice, inspissated mucus was found primarily in main ducts that seemed to be dilated. Epithelial cells of affected ducts were generally flattened, and based on Ki67 staining they were found to have a similarly high proliferative index compared with those of flattened epithelial cells in the ducts that had no mucus plugs. In contrast, in tobacco-treated WT mice, the morphology of the epithelial cells in both segmental and main pancreatic ducts seemed normal. Ki67 staining and TUNEL assays were both negative.
Ductal epithelium of the pancreas. (a) Normal pancreatic duct in control WT mouse of 5 months old. (b) Pancreatic duct in control Elastase-IL-1β mice of 5 months old. (c) Flattening of ductal epithelium in Elastase-IL-1β mice treated with TS for 4 months, intra-epithelial infiltration of inflammatory cells were shown by arrows, and one polymorphonuclear neutrophil was shown in the insert. (d) High proliferation index of epithelial cells of pancreatic ducts in Elastase-IL-1β mice treated with Snus for 8 months (Ki67 immunohistochemical staining).
TS- or Snus-Accelerated Pancreatic Acinar Cell Injury in Elastase-IL-1β Mice
As described earlier,33 Elastase-IL-1β mice developed pancreatic glandular atrophy, primarily manifested as loss of acinar cells and fatty replacement (Figure 2a). The majority of mice (>90%) showed moderate to marked acinar atrophy (50–75%) after 4 months. In TS-treated Elastase-IL-1β mice, as early as 4 months of treatment, diffuse glandular atrophy was remarkably more severe than that of control Elastase-IL-1β mice, with >75% loss of acini (Figure 2b). Atrophy of acini was seen in all parts of the pancreas gland evenly, namely head, body, and tail. Concomitant replacement by fat, almost always extensive, was also noted (Figure 2b). These changes became persistent and occurred in 64% (14/22) of TS-treated Elastase-IL-1β mice. Glandular atrophy also occurred in Snus-treated Elastase-IL-1β mice, but was less severe and occurred after longer treatment. Loss of acini and fatty replacement occurred in 35% (10/29) of Snus-treated Elastase-IL-1β mice compared with 64% of TS-treated Elastase-IL-1β mice (P<0.05). In tobacco-treated WT mice, morphological changes were not observed after treatment with TS or Snus for up to 15 months.
(a) Chronic pancreatitis, including glandular atrophy, tubular complexes, and fibrosis, in control Elastase-IL-1β mice of 5 months old; tubular complexes are highlighted in the insert (arrows). (b) Severe glandular atrophy in Elastase-IL-1β mice treated with TS for 4 months, minimal acini were seen, and the pancreas showed extensive fatty replacement and some fibrosis. (c) Immunohistochemical staining of CD3e of the pancreas of Elastase-IL-1β mice treated with Snus for 8 months. T lymphocytes were positively stained. (d) Immunohistochemical staining for COX-2 in the pancreas of Elastase-IL-1β mice treated with Snus for 8 months; arrows indicate ductal epithelial cells showing positive staining for COX-2.
TS or Snus Did Not Worsen Fibrosis and Tubular Complexes in Tobacco-Treated Elastase-IL-1β
The inflammatory infiltrate was found to be a mixed population of T lymphocytes that were predominant, B lymphocytes, granulocytes, and macrophages.33 Similar to that of control Elastase-IL-1β mice, in tobacco-treated Elastase-IL-1β mice, the majority of inflammatory cells were T lymphocytes, suggesting the chronic nature of inflammation (Figure 2c). There were no significant differences between tobacco-treated and control Elastase-IL-1β mice, with regard to the scores of tubular complexes and fibrosis. By immunohistochemical staining for desmin, the numbers of activated fibroblasts in pancreatic stroma of tobacco-treated Elastase-IL-1β mice were similar to those of control transgenic mice (data not shown). The numbers of activated stellate cells detected by immunohistochemical staining for α-smooth muscle actin were also similar between tobacco-treated and control transgenic mice (data not shown).
Many other organs, such as oral mucosa, lungs, bladder, stomach, colon, and kidneys, were examined in tobacco-treated Elastase-IL-1β and WT mice. Overall, there were no detectable changes in these tissues in comparison with those of their corresponding control mice.
TS- or Snus-Activated Cancer-Initiating Signaling Pathways in the Pancreas
Consistent with reports earlier,33 the expression of COX-2 was found to be slightly increased in control Elastase-IL-1β mice compared with that of WT mice by semi-quantitative RT–PCR (Figure 3a) and real-time PCR (data not shown). As the COX-2 pathway is a known target of tobacco derivatives, such as NNK,16 we also examined the expression of COX-2 in tobacco-treated mice. In comparison with control transgenic mice, the expression of COX-2 was increased more than twofold in both TS- and Snus-treated Elastase-IL-1β mice after 4 months of treatment (Figure 3a). Overexpression of COX-2 persisted in tobacco-treated Elastase-IL-1β mice after longer periods of treatment. By immunohistochemical staining (Figure 2d), the expression of COX-2 was found to be primarily localized to epithelial cells of pancreatic ducts. In control and tobacco-treated WT mice, RT–PCR and immunohistochemical analyses indicated that there was little to no COX-2 expression.
(a) Semi-quantitative RT–PCR of COX-2. Compared with control Elastase-IL-1β mice, COX-2 expression was more than twofold higher in TS-Elastase-IL-1β mice after 4 months of treatment. (b) Real-time PCR of TNF-α; groups include 1–3, SDS-, TS-, and Snus-treated WT of 4–6 months; 4–6, SDS-, TS-, and Snus-treated Elastase-IL-1β mice of 4–6 months; 7–9, SDS-, TS-, and Snus-treated WT mice of 7–9 months; 10–12, SDS-, TS-, and Snus-treated Elastase-IL-1β mice of 7–9 months; 13–15, SDS-, TS-, and Snus-treated WT mice of 13–15 months; 16–18, SDS-, TS-, and Snus-treated Elastase-IL-1β mice of 13–15 months. Three to five mice in each group were studied.
The expression of many chronic pancreatitis-associated genes, such as TNF-α, IL-6, TGF-β1, and SDF-1, was found to be up-regulated in control Elastase-IL-1β mice by real-time PCR assays (Figures 3b and 4). Overexpression of these genes was found to be time dependent. For instance, TNF-α was increased in Elastase-IL-1β mice at an early age of 5 weeks and persisted in older mice (eg 14–16 months of age) compared with age-matched WT mice (P<0.05). Overexpression of IL-6 in Elastase-IL-1β mice was found to occur at 5–7 months of age (P<0.05), but then diminish at 8–10 months old. By 14–16 months old, there was no difference in IL-6 expression between WT and Elastase-IL-1β mice (data not shown). TGF-β and SDF-1 were overexpressed in Elastase-IL-1β compared with WT mice at 5–7 months old and remained higher in older mice.
(a) Real-time PCR assay of mouse IL-6 on the pancreas mRNA at 4–6 months. Groups include SDS-, TS-, and Snus-treated WT and Elastase-IL-1β mice. Four mice in each group were studied. (b) Mouse IL-6 ELISA of the serum at 4–6 months. Groups include SDS-, TS-, and Snus-treated WT and Elastase-IL-1β mice. Four mice in each group were studied.
The expression of TNF-α mRNA in the pancreas was examined by real-time PCR assay. In WT mice, there were no differences among control-, TS-, and Snus-WT at all designated time points, including 4–6, 7–9, and 13–15 months of treatment. In TS-treated Elastase-IL-1β mice, from 4 to 9 months of treatment, the expression of TNF-α was increased more than twofold compared with that of age-matched control Elastase-IL-1β (P<0.05) (Figure 3b). In Snus-treated Elastase-IL-1β mice, compared with those of control Elastase-IL-1β mice, the expression of TNF-α was similar at 4–6 months of treatment and increased more than twofold at 7–9 months of treatment (P<0.05). However, at 13–15 months of treatment, there were no differences of TNF-α expression among control-, TS-, and Snus-Elastase-IL-1β mice.
Expression of IL-6 mRNA in the pancreas and levels of IL-6 in the serum were examined by real-time PCR assays and ELISA, respectively. In WT mice, by both real-time PCR assays and ELISA, there were no differences among control-, TS-, and Snus-WT at all designated time points, including 4–6, 7–9, and 13–15 months of treatment. In TS-Elastase-IL-1β mice, by real-time PCR, IL-6 was found to be overexpressed at 4–6 months of treatment (P<0.05) (Figure 4a), but not at 7–9 or 13–15 months of treatment (data not shown) compared with those of control Elastase-IL-1β mice. Similarly, by ELISA, the serum level of IL-6 in TS-Elastase-IL-1β mice at 4–6 months of treatment was significantly higher than that of untreated Elastase-IL-1β mice (P<0.05) (Figure 4b). At 7–9 or 13–15 months of treatment, the serum levels of IL-6 were similar between control- and TS-Elastase-IL-1β mice. In Snus-treated Elastase-IL-1β mice, the levels of IL-6 mRNA in the pancreas and serum levels of IL-6 were similar to those of control Elastase-IL-1β mice at all time points examined.
There were no differences in TGF-β and SDF-1 mRNA levels in the pancreas, by real-time PCR assays, among control-, TS-, and Snus-WT at all designated time points, including 4–6, 7–9, and 13–15 months of treatment. In contrast, levels of TGF-β and SDF-1 were increased in the pancreas of TS-Elastase-IL-1β mice, at 7–9 months (Figure 5a and b) and 13–15 months of treatment as well in comparison to those of their age-matched control Elastase-IL-1β mice (P<0.05). In Snus-treated Elastase-IL-1β mice, the mRNA levels of TGF-β and SDF-1 were similar to those of control Elastase-IL-1β mice at all time points examined.
(a) Real-time PCR assays of TGF-β mRNA in pancreas of Elastase-IL-1β mice at 9 months of treatment. Groups include SDS-, TS-, and Snus-treated Elastase-IL-1β mice. Three to five mice in each group were studied. (b) Real-time PCR assays of SDF-1 mRNA in the pancreas of Elastase-IL-1β mice at 8 months of treatment. Groups include SDS-, TS-, and Snus-treated Elastase-IL-1β mice. Three to five mice in each group were studied.
DISCUSSION
Cigarette smoking has been found to cause acute and chronic pancreatitis in both epidemiological and animal studies. To our knowledge, the potential carcinogenic effects of tobacco have not been evaluated in an animal model of chronic pancreatitis. In this study, we provide several lines of evidence suggesting important interactions between tobacco and chronic pancreatitis. First, although there were no morphological changes detected in the pancreas of tobacco-treated WT mice, prominent phenotypic changes occurred in the pancreas, including significant flattening of ductal epithelial cells and remarkably severe atrophy of acini, in tobacco-treated Elastase-IL-1β mice compared with untreated Elastase-IL-1β mice. Given similar levels of urine nicotine metabolites between corresponding groups of WT and Elastase-IL-1β mice, the background of chronic pancreatitis in Elastase-IL-1β mice stands out as the determinant of these phenotypic changes. Thus, these findings strongly suggest important interactions between tobacco and chronic pancreatitis. Second, the epithelial cells of the pancreatic ducts in control Elastase-IL-1β mice were shown to have a high proliferation index in the setting of chronic pancreatitis. With tobacco treatment, ductal epithelial cells displayed a much higher proliferation index compared with control Elastase-IL-1β mice. In contrast, there was no detectable level of proliferation of ductal epithelium in either control WT mice or tobacco-treated WT mice. Last, the expression of many signaling pathways that could contribute to these changes was examined.
It is interesting to note that COX-2 and TNF-α gene expression was up-regulated in both TS- and Snus-treated Elastase-IL-1β mice, whereas IL-6, TGF-β1, and SDF-1 gene expression was only increased in TS-treated Elastase-IL-1β mice, but not in WT mice. These findings not only support the notion of interactions between tobacco and chronic pancreatitis, but likely provide some clues as to the underlying mechanisms. For example, up-regulation of TNF-α, a major proinflammatory cytokine, was found to correlate with the onset of severe glandular atrophy in both TS- and Snus-Elastase-IL-1β mice. In TS-treated Elastase-IL-1β mice, overexpression of TNF-α and the onset of severe acinar atrophy were both first detected after 4 months of treatment. In Snus-treated Elastase-IL-1β mice, up-regulation of TNF-α occurred at 7–9 months of treatment, at a time when the onset of severe glandular atrophy was also first observed. These findings indicate that overexpression of TNF-α is likely to have a major function in acinar cell injury. Cigarette smoke and tobacco metabolites are known to contribute to chronic inflammation in the pancreas. TGF-β1, one of the major pathways in injury-induced remodeling, was found to be overexpressed in tobacco-induced chronic inflammation in rat pancreas.31 In our study, we showed that TGF-β1 was overexpressed in control Elastase-IL-1β mice compared with that of WT mice. With TS treatment, expression of TGF-β1 was further increased in Elastase-IL-1β mice. In view of the earlier evidence that tobacco use independently increases the risk of pancreatic cancer in the setting of chronic pancreatitis,32 further studies are required to elucidate the interactions between tobacco and chronic pancreatitis, and their functions in cancer development.
Cigarette smoke and Snus differ in the types of tobacco-derived chemicals delivered to their users as a result of marked differences in production, manufacturing, and mode of consumption. Although the two products share many common tobacco-derived metabolites such as nitrosamines, urinary levels of biomarkers for these ingredients often vary in human beings in all likelihood because of different concentrations and in vivo pharmacokinetics of these chemicals in commercial products.11, 12, 36, 37 In addition, cigarette smoke contains a variety of combustion-derived chemicals, not present in Snus, making cigarette smoke potentially more cytotoxic and carcinogenic.38 In this study, differences in constituents are believed to contribute to the disparities of phenotypic changes and expression profiles of signaling pathways examined between TS- and Snus-treated Elastase-IL-1β mice. For example, although glandular atrophy was worsened in both TS- and Snus-treated Elastase-IL-1β mice compared with untreated Elastase-IL-1β mice, these changes were found to be significantly more common in TS-treated mice (64%) compared with those of Snus-treated mice (35%). The onset of glandular atrophy was also earlier in TS-treated mice (4–6 months) in comparison with that of Snus-treated mice (after 8 months). In addition, expression profiles of many chronic pancreatitis-associated genes were quite different between TS- and Snus-treated Elastase-IL-1β mice. In Snus-treated mice, only TNF-α expression was found to be increased and expression of IL-6, TGF-β1, and SDF-1 remained similar to those of control Elastase-IL-1β mice. In TS-treated Elastase-IL-1β mice, compared with those of control Elastase-IL-1β mice, the expression of each of these genes was increased, whereas some of the effects were time dependent. Studies of individual constituents of cigarette smoke and Snus should lead to a better understanding of both their similarities and differences, and given our findings that these are present in TS and thus likely soluble, this would suggest a strategy for isolation and identification of specific components.
The etiology of flattening of ductal epithelium in tobacco-treated Elastase-IL-1β mice remains unclear. Given that this occurred in both TS- and Snus-treated Elastase-IL-1β mice, it is likely that common constituents shared by cigarette smoke and Snus are the cause. These chemicals could be tobacco-specific nitrosamines, as many of them are known to be cytotoxic.38 It is possible that these cytotoxic chemicals, either acting alone or in combination with others, induced direct injury to ductal epithelial cells, resulting in flattening of these epithelial cells. Maintenance of a single layer of the epithelial cells in these ducts, despite the increased cellular proliferation shown by Ki67 immunohistochemical staining, indicates a likely repair process in response to cell damage or injury. TUNEL assays excluded the possibility of apoptosis as the primary response to tobacco treatment here. The overall significance of flattening of ductal epithelium in tobacco-treated Elastase-IL-1β mice needs to be further characterized. In prostate carcinogenesis, atrophic-seeming epithelial cells in the setting of chronic inflammation are highly proliferative and considered to be signs of early preneoplasia.39, 40, 41 Apoptotic mechanisms in the flattened prostatic ductal cells are found to be inhibited by up-regulation of BCL-2 and AKT. These cells have been further characterized by the activation of cancer-initiating signaling pathways, such as COX-2, and genetic alterations including inactivation of p27 and PTEN.42 In our study, flattened epithelial cells of pancreatic ducts were found to be highly proliferative, minimally apoptotic and COX-2 positive, features seen in preneoplastic lesions. Although no more advanced lesions developed within 15 months of treatment, flattening of ductal epithelial cells may represent an early preneoplastic lesion.
Severe loss of acinar cells and resultant glandular atrophy is another prominent phenotypic change in tobacco-treated Elastase-IL-1β mice. In earlier studies using rats,29, 43 high concentrations (200 mg/l) of nicotine were found to induce morphological alterations in acinar cells, including cellular swelling/vacuolation and nuclear condensation. The proposed mechanisms underlying nicotine-induced acinar injury include intracellular calcium mobilization and activation of calmodulin-dependent protein kinases resulting in cytotoxicity and eventual cell death.44 However, in this study, we did not observe similar morphological changes in the acinar cells of tobacco-treated WT mice. In addition to the species differences, the nicotine intake by mice in our study was found to be much lower, <0.6 mg per day of Snus-treated mice and <0.1 mg per day of TS-treated WT, compared with an estimate of >15 mg per day in Chowdhury's study.29, 43 Unfortunately, we were not able to measure blood nicotine levels in our animals, which might have allowed a more direct comparison with the findings from these earlier studies. Furthermore, the findings of earlier onset and greater occurrence of severe glandular atrophy in TS-treated Elastase-IL-1β mice, in comparison with Snus mice, indicate that constituents in cigarette smoke not present in Snus may also contribute to tissue injury. However, cigarette smoke has been found to have weak and sporadic effects on acinar cells in Sprague–Dawley rats treated with smoke from combusting cigarettes.31 Acinar damage and atrophy occurred in <5% of pancreatic tissues and also required high-dose smoke exposure. Taken together, it seems likely that tobacco-derived chemicals have specific effects in the context of chronic pancreatitis induced by IL-1β. Many genes associated with chronic pancreatitis were up-regulated in both TS- and Snus-treated Elastase-IL-1β mice, and it seems likely that the further induction of these genes by tobacco-induced inflammation in the background of IL-1β-induced chronic pancreatitis could contribute to severe acinar atrophy. In any case, this is the first study to show that Snus can contribute to chronic inflammation in the pancreas.
As tobacco is an accepted risk factor for cancer, animal models of pancreatic cancer have been developed primarily through targeted exposure to tobacco-derived chemicals, such as implanting 7,12-dimethylbenzanthracene in the pancreas or feeding NNK- or NNAL-containing water.17, 18, 45, 46, 47 However, no animal model of pancreatic cancer has been established solely based on commercially available tobacco products, including cigarettes and Snus. This is likely due, in part, to the difficulty in delivering high concentrations of these tobacco products for extended periods of time. Our study is not the exception. In our study, during the 15-month observation period, we did not detect more advanced preneoplastic or neoplastic lesions in the pancreas of Elastase-IL-1β mice treated with tobacco. Although Snus intake in these mice was comparable with those of Snus users,19, 48, 49 the amount of tobacco intake in TS-treated mice may be lower than found in human cigarette smokers. Given the fact that most human pancreatic ductal adenocarcinoma occurs after the fifth decade of life, our study, similar to others, is potentially limited by the length of the observation period in mice, and a possible need for exposure to a higher concentration of tobacco carcinogens. Another limitation of our study is the relatively small number of mice carried out to 15 months. Future larger studies with more extended follow-up would be valuable to tease out the carcinogenic potential of tobacco components. In summary, our study shows for the first time the importance of interactions between tobacco and chronic pancreatitis in altering the biology of the pancreas. The findings support the notion that both cigarette smoke and Snus are potentially cytotoxic and carcinogenic to the pancreas.
References
Boyle P, Maisonneuve P, Bueno de Mesquita B, et al. Cigarette smoking and pancreas cancer: a case control study of the search programme of the IARC. Int J Cancer 1996;67:63–71.
Silverman DT . Risk factors for pancreatic cancer: a case-control study based on direct interviews. Teratog Carcinog Mutagen 2001;21:7–25.
Duell EJ, Holly EA, Bracci PM, et al. A population-based, case-control study of polymorphisms in carcinogen-metabolizing genes, smoking, and pancreatic adenocarcinoma risk. J Natl Cancer Inst 2002;94:297–306.
Michaud DS . Epidemiology of pancreatic cancer. Minerva Chir 2004;59:99–111.
Iodice S, Gandini S, Maisonneuve P, et al. Tobacco and the risk of pancreatic cancer: a review and meta-analysis. Langenbecks Arch Surg 2008;393:535–545.
Boffetta P, Aagnes B, Weiderpass E, et al. Smokeless tobacco use and risk of cancer of the pancreas and other organs. Int J Cancer 2005;114:992–995.
Luo J, Ye W, Zendehdel K, et al. Oral use of Swedish moist snuff (snus) and risk for cancer of the mouth, lung, and pancreas in male construction workers: a retrospective cohort study. Lancet 2007;369:2015–2020.
Alguacil J, Silverman DT . Smokeless and other noncigarette tobacco use and pancreatic cancer: a case-control study based on direct interviews. Cancer Epidemiol Biomarkers Prev 2004;13:55–58.
Hassan MM, Abbruzzese JL, Bondy ML, et al. Passive smoking and the use of noncigarette tobacco products in association with risk for pancreatic cancer: a case-control study. Cancer 2007;109:2547–2556.
Prokopczyk B, Hoffmann D, Bologna M, et al. Identification of tobacco-derived compounds in human pancreatic juice. Chem Res Toxicol 2002;15:677–685.
Benowitz NL, Jacob III P, Yu L . Daily use of smokeless tobacco: systemic effects. Ann Intern Med 1989;111:112–116.
Hecht SS, Carmella SG, Murphy SE, et al. Similar exposure to a tobacco-specific carcinogen in smokeless tobacco users and cigarette smokers. Cancer Epidemiol Biomarkers Prev 2007;16:1567–1572.
Belinsky SA, Devereux TR, Maronpot RR, et al. Relationship between the formation of promutagenic adducts and the activation of the K-ras protooncogene in lung tumors from A/J mice treated with nitrosamines. Cancer Res 1989;49:5305–5311.
Belinsky SA, Devereux TR, Anderson MW . Role of DNA methylation in the activation of proto-oncogenes and the induction of pulmonary neoplasia by nitrosamines. Mutat Res 1990;233:105–116.
Belinsky SA, Foley JF, White CM, et al. Dose-response relationship between O6-methylguanine formation in Clara cells and induction of pulmonary neoplasia in the rat by 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone. Cancer Res 1990;50:3772–3780.
Schuller HM . Mechanisms of smoking-related lung and pancreatic adenocarcinoma development. Nat Rev Cancer 2002;2:455–463.
Rivenson A, Hoffmann D, Prokopczyk B, et al. Induction of lung and exocrine pancreas tumors in F344 rats by tobacco-specific and Areca-derived N-nitrosamines. Cancer Res 1988;48:6912–6917.
Hoffmann D, Rivenson A, Abbi R, et al. A study of tobacco carcinogenesis: effect of the fat content of the diet on the carcinogenic activity of 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone in F344 rats. Cancer Res 1993;53:2758–2761.
Stenstrom B, Zhao CM, Rogers AB, et al. Swedish moist snuff accelerates gastric cancer development in Helicobacter pylori-infected wild-type and gastrin transgenic mice. Carcinogenesis 2007;28:2041–2046.
Yen S, Hsieh CC, MacMahon B . Consumption of alcohol and tobacco and other risk factors for pancreatitis. Am J Epidemiol 1982;116:407–414.
Lowenfels AB, Zwemer FL, Jhangiani S, et al. Pancreatitis in a native American Indian population. Pancreas 1987;2:694–697.
Bourliere M, Barthet M, Berthezene P, et al. Is tobacco a risk factor for chronic pancreatitis and alcoholic cirrhosis? Gut 1991;32:1392–1395.
Talamini G, Bassi C, Falconi M, et al. Cigarette smoking: an independent risk factor in alcoholic pancreatitis. Pancreas 1996;12:131–137.
Talamini G, Bassi C, Falconi M, et al. Alcohol and smoking as risk factors in chronic pancreatitis and pancreatic cancer. Dig Dis Sci 1999;44:1303–1311.
Lin Y, Tamakoshi A, Hayakawa T, et al. Cigarette smoking as a risk factor for chronic pancreatitis: a case-control study in Japan. Research Committee on Intractable Pancreatic Diseases. Pancreas 2000;21: 109–114.
Morton C, Klatsky AL, Udaltsova N . Smoking, coffee, and pancreatitis. Am J Gastroenterol 2004;99:731–738.
Lindkvist B, Appelros S, Manjer J, et al. A prospective cohort study of smoking in acute pancreatitis. Pancreatology 2008;8:63–70.
Tolstrup JS, Kristiansen L, Becker U, et al. Smoking and risk of acute and chronic pancreatitis among women and men: a population-based cohort study. Arch Intern Med 2009;169:603–609.
Chowdhury P, Rayford PL, Chang LW . Induction of pancreatic acinar pathology via inhalation of nicotine. Proc Soc Exp Biol Med 1992;201:159–164.
Chowdhury P, Doi R, Tangoku A, et al. Structural and functional changes of rat exocrine pancreas exposed to nicotine. Int J Pancreatol 1995;18:257–264.
Wittel UA, Pandey KK, Andrianifahanana M, et al. Chronic pancreatic inflammation induced by environmental tobacco smoke inhalation in rats. Am J Gastroenterol 2006;101:148–159.
Lowenfels AB, Maisonneuve P, Whitcomb DC, et al. Cigarette smoking as a risk factor for pancreatic cancer in patients with hereditary pancreatitis. JAMA 2001;286:169–170.
Marrache F, Tu SP, Bhagat G, et al. Overexpression of interleukin-1beta in the murine pancreas results in chronic pancreatitis. Gastroenterology 2008;135:1277–1287.
Bernert Jr JT, Turner WE, Pirkle JL, et al. Development and validation of sensitive method for determination of serum cotinine in smokers and nonsmokers by liquid chromatography/atmospheric pressure ionization tandem mass spectrometry. Clin Chem 1997;43:2281–2291.
Demols A, Van Laethem JL, Quertinmont E, et al. Endogenous interleukin-10 modulates fibrosis and regeneration in experimental chronic pancreatitis. Am J Physiol Gastrointest Liver Physiol 2002;282:G1105–G1112.
Hatsukami DK, Lemmonds C, Zhang Y, et al. Evaluation of carcinogen exposure in people who used ‘reduced exposure’ tobacco products. J Natl Cancer Inst 2004;96:844–852.
Boffetta P, Hecht S, Gray N, et al. Smokeless tobacco and cancer. Lancet Oncol 2008;9:667–675.
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Tobacco smoke and involuntary smoking. IARC Monogr Eval Carcinog Risks Hum 2004;83:1–1438.
Feneley MR, Young MP, Chinyama C, et al. Ki-67 expression in early prostate cancer and associated pathological lesions. J Clin Pathol 1996;49:741–748.
Ruska KM, Sauvageot J, Epstein JI . Histology and cellular kinetics of prostatic atrophy. Am J Surg Pathol 1998;22:1073–1077.
De Marzo AM, Marchi VL, Epstein JI, et al. Proliferative inflammatory atrophy of the prostate: implications for prostatic carcinogenesis. Am J Pathol 1999;155:1985–1992.
De Marzo AM, Platz EA, Sutcliffe S, et al. Inflammation in prostate carcinogenesis. Nat Rev Cancer 2007;7:256–269.
Chowdhury P, Hosotani R, Chang L, et al. Metabolic and pathologic effects of nicotine on gastrointestinal tract and pancreas of rats. Pancreas 1990;5:222–229.
Chowdhury P, MacLeod S, Udupa KB, et al. Pathophysiological effects of nicotine on the pancreas: an update. Exp Biol Med (Maywood) 2002;227:445–454.
Dissin J, Mills LR, Mains DL, et al. Experimental induction of pancreatic adenocarcinoma in rats. J Natl Cancer Inst 1975;55:857–864.
Osvaldt AB, Wendt LR, Bersch VP, et al. Pancreatic intraepithelial neoplasia and ductal adenocarcinoma induced by DMBA in mice. Surgery 2006;140:803–809.
Bersch VP, Osvaldt AB, Edelweiss MI, et al. Effect of nicotine and cigarette smoke on an experimental model of intraepithelial lesions and pancreatic adenocarcinoma induced by 7,12-dimethylbenzanthracene in mice. Pancreas 2009;38:65–70.
Rodu B, Jansson C . Smokeless tobacco and oral cancer: a review of the risks and determinants. Crit Rev Oral Biol Med 2004;15:252–263.
Nilsson R . De minimus non curat lex—virtual thresholds for cancer initiation by tobacco specific nitrosamines—prospects for harm reduction by smokeless tobacco. Int J Occup Med Environ Health 2006;19:6–35.
Acknowledgements
We are grateful to Shanisha Gordon and Anthony Mitchell for maintaining our mouse colonies and monitoring food and water intake, and to Genevieve Young, Jones Nauseef, and Ron Liebman for preparing TS solution. This study was supported by the Lustgarten Foundation Fund for Pancreatic Cancer Research (TC Wang). Michael Quante is supported by a grant from the Mildred-Scheel-Stiftung, Deutsche Krebshilfe, Germany. Dr Chen is supported by grants from St Olavs’ Hospital Foundation for Cancer Research and the Research Council of Norway.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE/CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supplementary Information accompanies the paper on the Laboratory Investigation website (http://www.laboratoryinvestigation.org)
Supplementary information
Rights and permissions
About this article
Cite this article
Song, Z., Bhagat, G., Quante, M. et al. Potential carcinogenic effects of cigarette smoke and Swedish moist snuff on pancreas: a study using a transgenic mouse model of chronic pancreatitis. Lab Invest 90, 426–435 (2010). https://doi.org/10.1038/labinvest.2009.145
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2009.145