
Emmanuel Kofi Quaye prepares genetic samples for sequencing at Yemaachi Biotech.Credit: Yemaachi Biotech
It took Eve Namisango four years to find funding for a project close to her heart: researching ways to deliver dignified and more personalized care to patients with complex non-communicable diseases, such as cancer, in settings where resources are scarce. Uganda, where Namisango is based as a clinical epidemiologist and palliative care expert, has just one specialized cancer-care centre. “We need evidence to shape our care,” says Namisango, yet finding grants to produce that evidence is extremely difficult.
With colleagues in Uganda, the United Kingdom and Zimbabwe, Namisango won a £180,000 (US$235,000) grant from the Medical Research Council, one of the United Kingdom’s national science funders, which enabled them to interview patients, caregivers and health-care professionals as part of a study into what patient-centred care might look like in Africa, and how it can be implemented. “We were grateful to get that grant,” says Namisango, who leads research at the African Palliative Care Association, a non-profit organization based in Kampala that supports the integration of palliative care into health systems across Africa.
Although cancer is a rapidly growing health concern in Africa, it is significantly under-studied. But as funders and scientists have become more aware of the need for equity and representation in medical research, African researchers are hopeful that change will come. “I wouldn’t say we are where we want to be, but people are becoming more aware of these things,” says Fidel Rubagumya, an oncologist at Rwanda Military Hospital in Kigali.
Africa’s cancer trajectory differs greatly from trends seen in high-income countries. The cancer death rate in the United States, for example, has fallen by one-third over the past three decades, according to a report published in January1, which cited advances in treatment and diagnosis and a decline in smoking as contributing factors. Sub-Saharan Africa, by comparison, expects to see cancer deaths double to reach 1 million per year by 20302.
Research has not kept up with Africa’s cancer crisis. A 2022 study3 led by Miriam Mutebi, a breast surgical oncologist at Aga Khan University in Nairobi, found that African countries produced five times more research on infectious diseases such as malaria, tuberculosis and HIV/AIDS between 2009 and 2020 than they did on cancer. The number of African cancer papers did increase rapidly over this time, by about 15% annually, but authorship was concentrated in the richest African countries: Egypt published nearly half (48%) of Africa’s cancer papers and South Africa and Nigeria produced 14% and 6%, respectively.
The study also found that Africans, on average, do not lead the research coming out of the continent. Among the more than 5,000 international cancer papers with at least one author from sub-Saharan Africa published during the study period, only 42% had African first authors, and 30% had African last authors.
Several factors contribute to this imbalance. Cancer research lacks domestic support across most of sub-Saharan Africa, says Violet Kayamba, a gastroenterologist who studies stomach cancers at the University of Zambia in Lusaka. This translates into a lack of funding and infrastructure for locally relevant priorities, as well as a lack of mentors for young Africans wanting to move into cancer research. “We need our local governments to take ownership and to take the lead in supporting African scientists,” says Kayamba.
Yaw Bediako, an immunologist and founder of Yemaachi Biotech, a company based in Accra, Ghana, believes government support is a small part of the solution. To tackle cancer, he says, Africa’s private sector must join the endeavour. At Yemaachi, Bediako is developing cancer diagnostics and treatments tailored to Africans, and he describes the limited official data on patients with cancer across Africa as a major challenge. “We don’t know how many people have cancer,” says Bediako. This prompted Yemaachi to build its own data set — something that similar companies in high-income settings with more robust cancer data do not have to do. “Because we have certain structural challenges on this end, it is difficult for us to move at the pace that scientists in the United Kingdom or United States can move,” says Bediako.
Breaking the cycle
One way of dealing with the uneven playing field is to design new collaborations between African researchers and colleagues in high-income countries. Maintaining equity is difficult, given the disparities in resources, says Rubagumya, who is lead author of a 2023 study4 that describes a “vicious cycle of challenges in the research ecosystem” that maintains an imbalance towards high-income nations.
There are two interventions that could help break this cycle, says Rubagumya. One is for research institutions to train more young researchers, in Africa and overseas, in ways to establish equitable partnerships. The second involves African researchers and governments drawing up policies that stop researchers and funders from high-income countries exploiting African researchers, communities and data.
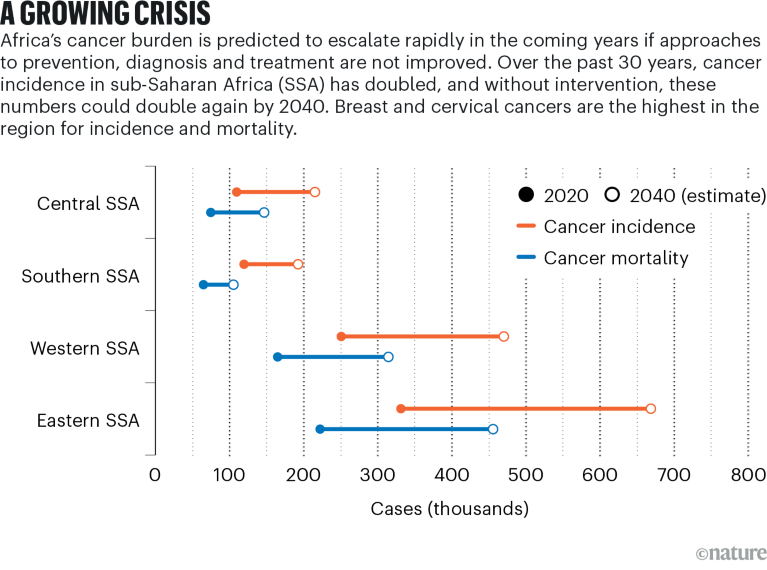
Source: International Agency for Research on Cancer
There are signs that Africa’s cancer-research capacity is expanding and diversifying. More young African researchers are showing an interest in the topic, says Solomon Rotimi, a cancer-genome scientist based at Covenant University in Ota, Nigeria. Rotimi leads the research committee of the African Organisation for Research and Training in Cancer (AORTIC), a non-profit organization that promotes intra-African collaboration in cancer research, education and care delivery. Before 2021, when AORTIC held its first dedicated international conference on cancer genomics, very few African countries had cancer-genomics experts presenting at the organization’s conferences, says Rotimi. A survey led by Rotimi of cancer-genomics papers published before 2019 found that roughly 40% of African countries had not published any research at all in the area5. When AORTIC held its second cancer-genomics conference, in Lagos, Nigeria, in May this year, several of the countries with no output in cancer genomics pre-2019, including Gabon, Zambia and Liberia, were represented for the first time.
That progress is embodied by young scientists such as Johnblack Kabukye, a postdoctoral health-informatics researcher at the Uganda Cancer Research Institute in Kampala, who sees opportunities in Africa’s cancer challenge. Before going into research, Kabukye tended to cancer patients as a junior medical officer and saw first-hand the gaps that existed in cancer care. “I took care of cancer patients who should have been handled by specialist oncologists,” he says.
Now, Kabukye develops tools to help African health-care personnel access specialist expertise. One such tool, developed by Kabukye with colleagues from Makerere University in Uganda and with funding from the Swedish Program for ICT in Developing Regions, a research centre at the Stockholm University Department of Computer and Systems Sciences, aims to improve the efficacy of cervical-cancer screening. In many African countries, cancer screening involves using visual inspection methods, such as examining the cervix with the naked eye using a focus lamp or torch light, rather than the lab-based PAP smears that are common in high-income countries. The smartphone-based telemedicine system connects a portable colposcope (a microscope with a strong light that is used to examine a patient’s cervix) with an app that connects non-specialists who carry out cervical-cancer screenings with gynaecologists to gain a second opinion. Users can also access artificial intelligence-powered analysis, which compares their observations with thousands of medical images. The device was deployed on a trial basis at the Uganda Cancer Institute and four satellite clinics across the country in 2019–21, and is described in a 2023 preprint6.
In Ghana, Bediako agrees that Africa has much to contribute to global cancer research, and not just in terms of patient data (although these are very valuable, he adds, with the need for research populations to become more diverse). Africa, with its tradition of valuing collective or community benefits, could lead the way in developing more ethical and patient-centred medical research, says Bediako. In many high-income countries, he says, data-rich medical research, especially using genomics, is growing increasingly fraught owing to concerns over privacy and exploitation. “We can bring our African culture and sensibility to cutting-edge science and lead this ethical discussion,” says Bediako. “I do think that is a contribution that Africa could and should make.”


 Can cancer research shift its focus?
Can cancer research shift its focus?
 Ukraine seeks to resume its role in cancer clinical trials
Ukraine seeks to resume its role in cancer clinical trials
 Four ways research aims to outwit cancer’s evasion tactics
Four ways research aims to outwit cancer’s evasion tactics
 Global leaders in science’s battle against cancer
Global leaders in science’s battle against cancer
 The gross imbalances of cancer research must be addressed
The gross imbalances of cancer research must be addressed






