Global cancer-research ecosystems invest billions of dollars in the development of oncological medicines and technologies, such as robotics and radiotherapy, yet comparatively little into programmes that aim to advance affordable, equitable and high-quality care and outcomes. The extraordinary growth in public and private expenditure on cancer discovery science and technologies, fuelled by the huge profits of cancer biopharmaceutical companies, has failed to create more opportunities for research in neglected areas. Instead, funding opportunities are narrowing. By 2026, an estimated US$307 billion will be spent on cancer-drug research and development worldwide, with 55% of this in just four areas: breast, lung, prostate and multiple myeloma (blood cancer).
The impact of such investment has been extremely variable. Significant improvements have been made in some adult blood-cancer outcomes, for example, but changes in survival for stage 4 solid adult cancers, including breast, lung and prostate cancer, have been modest and uneven. The rate of improvements in outcomes for cancers of the pancreas and upper gastrointestinal tract has been glacial.
A plethora of cancer medicines approved for market every year do not deliver clinically meaningful benefit. Of the 161 approvals for solid adult cancer therapies by the US Food and Drug Administration since 2017, only 35% were graded as delivering substantial clinically meaningful benefit on the European Society for Medical Oncology Scale, a standardized tool for assessing new anticancer therapies.
Beyond biopharmaceuticals, we are witnessing enormous technical expansions in both surgery and radiotherapy, as well as imaging and artificial intelligence. Surgical oncology has been dramatically changed, not just by the introduction of more advanced minimally invasive surgery, but also robotics. Like cancer medicines, these new technologies come with premium pricing and with a whole host of real-world implementation issues. Although minimally invasive surgery has been a significant advance for some cancer types in low- and middle-income countries (LMICs), the extended learning curves, prolonged operative times, lack of interoperability between systems and overall costs continue to be a major issue. There is also good evidence that in surgical oncology, robotics have created market forces that favour affluent patients at the expense of more equitable service delivery. The state of global radiotherapy research reflects similar inequalities, with most of the research focused on high-income settings and technical innovation, and less than 2% of global R&D focused on implementation.
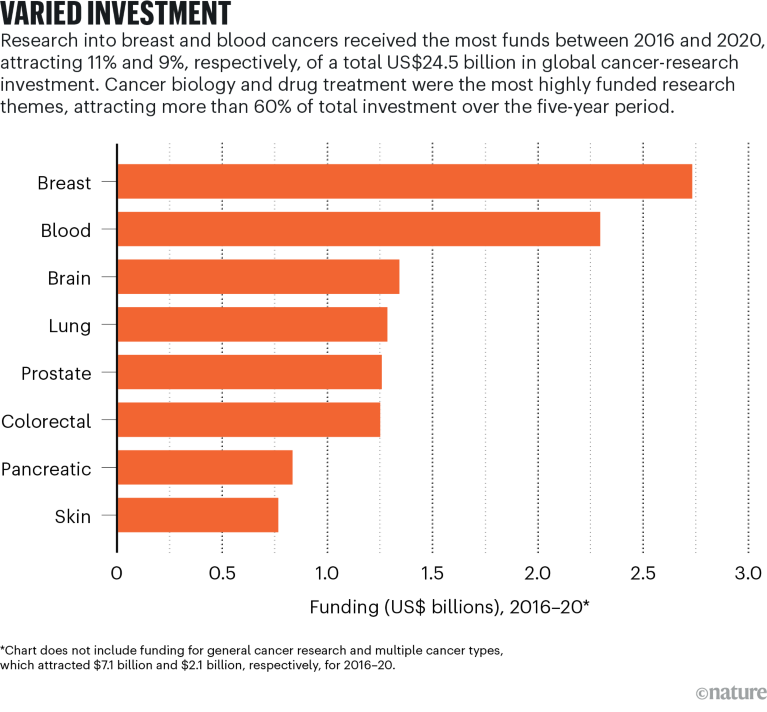
Source: McIntosh, S. A. et al. Lancet Oncol. 24, 636–645 (2023).
Surveying the global cancer-research ecosystem is to bear witness to gross imbalances. Ten years after the first Lancet Oncology commission into delivering affordable cancer care, there is an abundance of evidence to show that cancer research has become ever more focused on discovery science and biopharmaceutical R&D, with little evidence of better translation of research insights into meaningful changes in clinical practice and patient outcomes. New medicines and technologies face an increasingly low evidential bar for market entry and there is a dearth of real-world evidence studies, which seek to understand how technologies actually work on the ground. This further reflects systems that are entirely focused on production, rather than actual clinical and societal benefit.
More broadly, analysis of research outputs over the past two decades shows that all other major domains (prevention and public health, palliative care, even surgery and radiotherapy) are being squeezed out by the dominance of cancer discovery science and biopharmaceuticals. Such a monoculture is foundationally unhealthy.
Less than 4% of all cancer research published by the United States and United Kingdom is with, or germane to, LMICs. There is also little concordance between the research needs in these settings and the pattern of funding provided by high-income institutions. There is an intrinsic and long-standing weakness in cancer-research cultures and infrastructure in many countries that also needs to be addressed by building research careers and methodological capability into national systems, for example, as well as creating domestic and regional research-funding mechanisms.
This is not an anti-innovation agenda. Rather, it is a need for research funders to recognize that delivering affordable and equitable outcomes requires redistributive investment in the broad church of cancer research — especially in areas associated with prevention and implementation — and in deepening capacity-building and research in LMICs.



 Can cancer research shift its focus?
Can cancer research shift its focus?
 Ukraine seeks to resume its role in cancer clinical trials
Ukraine seeks to resume its role in cancer clinical trials
 Four ways research aims to outwit cancer’s evasion tactics
Four ways research aims to outwit cancer’s evasion tactics
 Global leaders in science’s battle against cancer
Global leaders in science’s battle against cancer
 African scientists call for research equity as a cancer crisis looms
African scientists call for research equity as a cancer crisis looms







