Abstract
We previously demonstrated that the up-regulation of p53, Fas, and DNA damage are present in lung epithelial cells from patients with idiopathic interstitial pneumonias (IIP). Fas ligation induces apoptosis of lung epithelial cells predominantly through the direct activation of the caspase cascade via caspase-8 activation, whereas the up-regulation of p53 and other cellular stresses can induce mitochondria-mediated apoptosis. In this study, we investigated the incidence of mitochondria-mediated apoptosis of epithelial cells in IIP. We performed TUNEL staining to detect apoptotic cells and western blot analysis and immunohistochemistry to assess the expression and activation of caspases and the cytochrome c release from mitochondria in lung tissues from eight patients with usual interstitial pneumonia, five patients with nonspecific interstitial pneumonia, and eight patients with normal lung parenchyma. The expressions of pro- and cleaved caspase-8, 9, 3, and cytochrome c release from the mitochondria were all significantly increased in the lung tissues of IIP compared with normal lung parenchyma. The positive signals for caspases in epithelial cells were increased in IIP compared with normal lung parenchyma by immunohistochemistry. The results of TUNEL and electron microscopy suggested that apoptotic cells were predominantly epithelial cells. TUNEL-positive cells in % of epithelial cells were significantly increased in IIP compared with normal lung parenchyma, and significantly correlated with cytochrome c release from the mitochondria and with the expression of cleaved caspase-3 in epithelial cells. We conclude that mitochondria-mediated apoptosis may be involved in the pathophysiology of IIP.
Similar content being viewed by others
Introduction
Apoptosis has been implicated before as a homeostatic mechanism. Recently, evidence has been increasing that apoptosis may play a role in lung diseases in two different ways. First, disease may be caused by a malfunction of the apoptosis mechanism. Repair following acute lung injury requires the elimination of proliferating mesenchymal and inflammatory cells from the alveolar airspace or alveolar walls (Polnovsky et al, 1993). Failure to clear unwanted cells by apoptosis will prolong the inflammation because of the release of their toxic contents. Second, excessive apoptosis may itself cause disease. It has been demonstrated that intratracheal instillation of agonistic anti-Fas antibody or recombinant Fas ligand induces acute alveolar epithelial injury and lung inflammation (Matute-Bello et al, 2001a, 2001b), and that repeated inhalations of agonistic anti-Fas antibody induce epithelial cell apoptosis and lung inflammation, which subsequently lead to pulmonary fibrosis in mice (Hagimoto et al, 1997).
There are two principle-signaling pathways of apoptosis. One is a direct pathway from death receptor ligation to caspase cascade activation and cell death. Death receptor ligation triggers recruitment of the precursor form of caspase-8 to a death-inducing complex, through the adaptor protein FADD, which leads to caspase-8 activation. The other pathway triggered by stimuli such as drugs, radiation, infectious agents, and reactive oxygen species is initiated in mitochondria. After cytochrome c is released into the cytosol from the mitochondria, it binds to Apaf1 and ATP, which then activate caspase-9 (Kroemer and Reed, 2000). The activation of caspase-8 or caspase-9 leads to the activation of the caspase cascade and apoptosis.
The etiology of idiopathic interstitial pneumonias (IIP) is still uncertain. However, the initial lesion before the development of fibrosis is probably alveolitis, which subsequently leads to the loss of type I epithelial cells and type II pneumocyte hyperplasia. Although there are various initiating factors or causes, the terminal stages are characterized by proliferation and progressive accumulation of connective tissue replacing normal functional parenchyma. We previously demonstrated that the Fas-Fas ligand (FasL) pathway was up-regulated in IIP and may be associated with the damage and apoptosis of lung epithelial cells through FADD and caspase-8 activation (Kuwano et al, 1999; Maeyama et al, 2001). We also demonstrated that there was DNA damage or apoptosis accompanied by an up-regulation of p53 in lung epithelial cells from patients with IIP (Kuwano et al, 1996). Up-regulation of p53 expression and other cellular stresses could induce mitochondria-mediated apoptosis. Therefore, the purpose of this study is to investigate whether or not the mitochondria-mediated apoptotic pathway is involved in epithelial cell injury and apoptosis in the lung tissues from patients with IIP.
Results
Expression and Activation of Caspases
Immunohistochemistry
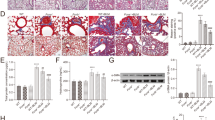
Positive signals for caspase-3 and -8 were predominantly detected in bronchiolar and alveolar epithelial cells in lung tissues from patients with usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP) as we previously demonstrated (Maeyama et al, 2001). Positive signals for caspase-9 were predominantly detected in bronchiolar and alveolar epithelial cells in UIP and NSIP (Fig. 1). The immunostaining grade for these caspases was significantly increased in lung epithelial cells from patients with UIP and NSIP, compared with the controls (Fig. 2). Positive signals for cleaved caspase-3 were mainly detected in the nuclei of epithelial cells of lung tissues from patients with UIP and NSIP, but not in epithelial cells of normal lung parenchyma (Fig. 3). The immunostaining grade for cleaved caspase-3 was significantly increased in lung epithelial cells from patients with UIP and NSIP, compared with the controls (Fig. 4A). The degree of positive staining for cleaved caspase-3 was increased accompanied by the progression of pulmonary fibrosis in UIP, but not in NSIP (Fig. 4B).
Semiquantitative analysis of immunostaining grade for caspase-8, -9, and -3 in bronchiolar and alveolar epithelial cells (*p < 0.01, **p < 0.05). These positive signals reflect pro- and cleaved form of caspases. Each circle represents one individual. The assessment of immunostaining grade is described in the Materials and Methods section.
Representative results of immunohistochemical analysis for cleaved caspase-3 in lung tissues from patients with IIP (b, c) and normal lung parenchyma (a) (original magnification, a, b; × 125, c; × 250). Positive signals were predominantly detected in the nucleus and cytoplasm of bronchiolar and alveolar epithelial cells (arrows).
A, Semiquantitative analysis of immunostaining grade for cleaved caspase-3 in lung epithelial cells (*p < 0.01, **p < 0.05). Each circle represents one individual. B, Association between immunostaining grade for cleaved caspase-3 in lung epithelial cells and the grade of pulmonary fibrosis in each field under light microscopy with × 125 magnification in UIP and NSIP (*p < 0.05).
Western Blot Analysis
The representative results of Western blot analysis show that the expression of both procaspases and cleaved caspases was up-regulated in UIP and NSIP, compared with the controls (Fig. 5A). Quantitative results show that the expression of procaspase-9 and -3 was significantly up-regulated in both UIP and NSIP, whereas the expression of procaspase-8 was significantly up-regulated only in NSIP, compared with the controls. The expression of cleaved caspase-8, -9, and -3 was significantly increased in both UIP and NSIP. There was a significant increase in the expression of cleaved caspase-3 in UIP, compared with NSIP (Fig. 5B).
Release of Cytochrome c from Mitochondria
To identify the activation of the mitochondria-mediated apoptosis pathway, we assessed the release of cytochrome c from the mitochondria. We extracted protein from the mitochondria-rich fraction and the cytoplasm separately, and performed western blot analysis for cytochrome c. The levels of cytochrome c in the cytoplasm were remarkably increased in both UIP and NSIP, compared with the controls (Fig. 6A). Quantitative results show that cytochrome c levels were significantly increased in both UIP and NSIP, compared with the controls, in both the cytoplasm and the mitochondria-rich fraction. The ratio of cytochrome c levels in the cytoplasm to those in the mitochondria-rich fraction was also significantly higher in both UIP and NSIP, compared with the controls (Fig. 6B). The immunoreactivity for cytochrome c was predominantly detected in the cytoplasm of epithelial cells (Fig. 7).
Representative results of immunohistochemical analysis for cytochrome c in lung tissues from patients with IIP (b, c) and normal lung parenchyma (a) (original magnification, a, b; × 125, c; × 250). Although positive signals were detected in cytoplasm of bronchiolar and alveolar epithelial cells in normal lung parenchyma, strong signals were detected in epithelial cells of IIP (arrows).
Electron Microscopy
Although the number of cases we could observe using electron microscopy (EM) was small, the type of apoptotic cells was predominantly type II epithelial cells except some apoptotic cells within alveolar macrophages. Figure 8a shows that the typical apoptotic type II epithelial cell, which included chromatin condensation to the nuclear membrane, numerous vacuoles, and vesicles in the cytoplasm, and the disappearance of microvilli on the cell surface, compared with the normal type II epithelial cell in the left side of the apoptotic cell. There are a few typical apoptotic cells and some dark cells, which are suggestive of apoptotic cells, in the lung tissues from patients with IIP. Some necrotic epithelial cells were also seen in the lung tissues from patients with IIP. The mitochondria in apoptotic type II epithelial cells (Fig. 8c) were condensed, compared with those in normal type II epithelial cells (Fig. 8b).
Representative results of apoptotic type II alveolar epithelium (arrow in a), normal type II alveolar epithelium (asterisk in a), normal mitochondria in normal type II alveolar epithelium (arrows in b), and condensed mitochondria in apoptotic alveolar epithelium (arrows in c) by electron microscopy (bar in A = 10 μm, bars in B and C = 1 μm).
TUNEL Assay
Positive signals for TUNEL were predominantly detected in the nuclei of bronchiolar and alveolar epithelial cells in the lung tissues from patients with IIP, whereas no positive signal was detected in the controls (Fig. 9). The TUNEL-positive cells for TUNEL in % of epithelial cells were significantly increased in both UIP and NSIP, compared with the controls. There was a significant increase of TUNEL-positive cells in UIP compared with NSIP (Fig. 10A). In both UIP and NSIP, positive signals were significantly increased in lesions showing a moderate grade of fibrosis (Fig. 10B). DNA repair and replication and RNA synthesis may be detected by the TUNEL method. To exclude these possibilities, we performed TUNEL staining and immunohistochemistry for PCNA, Ki67, and SC-35 using serial mirror sections. Positive cells for TUNEL were different cells from those for PCNA, Ki67, and SC-35 in serial mirror sections (Fig. 11).
A, Quantitative results of TUNEL staining in lung tissues from patients with IIP and normal lung parenchyma. Each circle represents one individual. The quantification of TUNEL-positive cells is described in the Materials and Methods section. B, Association between TUNEL-positive cells in % of epithelial cells and the grade of pulmonary fibrosis in each field under light microscopy with × 250 magnification in UIP and NSIP (*p < 0.05, **p < 0.01).
Correlation Between Apoptosis-Signaling Molecules in Lung Epithelial Cells
There was a significant correlation between TUNEL-positive cells in % of epithelial cells and the optical density of cytochrome c in the cytosol (p < 0.01, rs = 0.790; Fig. 12A). TUNEL-positive cells in % of epithelial cells were significantly correlated with the immunostaining grade for cleaved caspase-3 (p < 0.01, rs = 0.744; Fig. 12B), caspase-3 (p < 0.01, rs = 0.721), caspase-8 (p < 0.01, rs = 0.612), and caspase-9 (p < 0.001, rs = 0.862) in lung epithelial cells. TUNEL-positive cells in % of epithelial cells were significantly correlated with the optical density of procaspase-8 (p < 0.05, rs = 0.605), procaspase-9 (p < 0.01, rs = 0.734), procaspase-3 (p < 0.01, rs = 0.691), cleaved caspase-9 (p < 0.05, rs = 0.540), and cleaved caspase-3 (p < 0.01, rs = 0.887), but not with cleaved caspase-8 in Western blot analysis.
A, Correlation between TUNEL-positive cells in % of epithelial cells and the optical density of cytochrome c in cytosol in lung tissues from patients with IIP and normal lung parenchyma. rs = Spearman’s rank correlation coefficient. B, Correlation between TUNEL-positive cells in % of epithelial cells and the immunostaining grade for cleaved caspase-3 in lung epithelial cells from patients with IIP and normal lung parenchyma.
Discussion
We demonstrated here for the first time that mitochondria-mediated apoptotic pathways are activated in lung tissues from patients with IIP. The translocation of cytochrome c from the mitochondria to the cytoplasm was increased in lung tissues from patients with IIP, compared with normal lung parenchyma. The release of cytochrome c from the mitochondria leads to the activation of caspase-9. In fact, both the expression and activation of caspase-9 were remarkably up-regulated in IIP compared with normal lung parenchyma, and expression of caspase-9 was predominantly up-regulated in lung epithelial cells from patients with IIP. The expression and activation of the executioner caspase-3 were also up-regulated in lung epithelial cells of IIP. Positive signals for TUNEL were predominantly detected in lung epithelial cells and significantly increased in IIP compared with normal lung parenchyma. TUNEL-positive cells in % of epithelial cells were significantly correlated with cytochrome c release from the mitochondria and with the expression of cleaved caspase-3 in lung epithelial cells in IIP. Although the small number of subjects, combined with the inherent variability of the two major disease groups, represent a significant limitation in their data, these results indicate that mitochondria-mediated apoptotic pathways are up-regulated in lung epithelial cells in IIP.
Electron microscopic findings also demonstrate the incidence of apoptosis and the morphological changes to mitochondria in alveolar epithelial cells in the lung tissues from patients with IIP. Dinsdale et al (1999) demonstrated that the formation of ultracondensed mitochondria was observed in apoptotic monocytes with the release of cytochrome c, activation of caspases, and a reduction in inner mitochondrial potential. Condensed mitochondria in the apoptotic epithelium in this study also seemed to suggest the functional characteristics for apoptosis in mitochondria.
It is possible that TUNEL-positive cells are not necessarily dying cells. DNA repair and replication, and RNA synthesis, may be detected by the TUNEL method (Auten et al, 2002; Kanoh et al, 1999; Knox et al, 1998. To exclude these possibilities, we performed TUNEL staining and immunohistochemistry for proliferating cell nuclear antigen (PCNA), an indicator of DNA replication and repair (Shivji et al, 1992), Ki67, a replication-associated antigen (Sawhney and Hall, 1992), or splicing factor SC-35, an indicator of RNA synthesis (Kockx et al, 1998), using serial mirror sections. Positive cells for TUNEL were different from those for PCNA, Ki67, and SC-35 in serial mirror sections.
Since the distribution of positive signals for TUNEL is not uniform, substantial numbers of specimens should be examined to estimate the number of apoptotic cells by EM. Although it seems difficult to compare the number of apoptotic cells by EM and the number of positive signals for TUNEL in this study, we found several apoptotic cells and necrotic cells/mm2 in lung specimens from patients with IIP using EM. This prevalence seems compatible to the result of TUNEL. The results of immunohistochemistry using serial mirror sections and EM suggest that most of TUNEL-positive cells are dying cells.
Since the prognosis of patients with IIP is quite different between those with UIP and those with NSIP, we analyzed the data for UIP and NSIP separately to investigate whether there is any difference in the apoptotic pathway. There were some differences between these subgroups of IIP. Caspase-8 expression in epithelium of NSIP was significantly increased compared with that in UIP, whereas caspase-9 expression in epithelium of UIP was significantly increased compared with that in NSIP by immunohistochemistry. There was a significant increase in the expression of cleaved caspase-3 in UIP compared with NSIP in western blot analysis. There was a significant increase of TUNEL-positive cells in % of epithelial cells in UIP compared with NSIP. These results demonstrated the association between the degree of epithelial cell damage and apoptosis and the distinction of UIP and NSIP.
The fibroblastic foci, the signature of UIP, were found in all of eight cases with UIP. The fibroblastic foci appeared to be predominant in the intermediate stage of fibrosis, which seems to be compatible with the results that TUNEL-positive cells were also predominant in intermediate stage. Positive signals for TUNEL and caspases in epithelial cells were detected around the fibroblastic foci. However, these positive signals were also found in lesions without fibroblastic foci. Although the association of epithelial cell apoptosis and fibroblastic foci could not be verified in this study, this is an important issue to be clarified.
TUNEL staining disclosed evidence of apoptosis in all cases of IIP. The frequency of TUNEL-positive cells in epithelium was as low as 1 to 3% in IIP, compared with the observations in cell culture. Since apoptotic cells are quickly phagocytosed, they can be observed for only a few minutes under light microscopy, and apoptotic bodies can be found for only a few hours under electron microscopy (Gavrieli et al, 1992). Therefore, even the frequency of apoptotic cells is low, and the small number of TUNEL-positive cells visualized in tissue specimens may reflect a considerable magnitude of cell loss (Isner et al, 1995).
Although immunostaining grade for cleaved caspase-3 was significantly correlated with TUNEL-positive signals in % of epithelial cells, actual number of positive signals for cleaved caspase-3 was much higher than that of TUNEL-positive cells. Therefore, it is likely that the positive signals for cleaved caspase-3, especially in cytoplasm, are not always dying cells (Ishizaki et al, 1998; Weil et al, 1999). There was also a difference in the grade of fibrosis at the site where cleaved caspase-3 expression in lung epithelial cells is detected and the site where TUNEL-positive cells are predominantly detected. Concerning this difference, we assume that the lung epithelial cells are hyperplastic or regenerated epithelial cells in lesions showing severe fibrosis, and these cells may be resistant to apoptosis because of a survival mechanism acquired during the remodeling process.
Lung epithelial cells are always exposed to a variety of stresses such as oxygen stress. Reactive oxygen species (ROS) and their reactions with epithelial cells are involved in the pathophysiology of lung diseases. It has been reported that the spontaneous production of oxidants by lung inflammatory cells, and the myeloperoxidase concentration, are both increased in the alveolar epithelial lining fluid of patients with IIP (Cantin et al, 1987). ROS not only damage the cell membrane, which leads to necrosis, but also play important roles in apoptosis-signaling pathways induced by diverse stimuli. ROS were shown to up-regulate the Fas-FasL pathway and the release of cytochrome c (Stridh et al, 1998; Suhara et al, 1998), and also to activate p53 (Uberti et al, 1999). The activation of p53 leads to the up-regulation of Fas (Muller et al, 1998).
Cross talk between Fas-mediated and mitochondria-mediated pathway is provided by Bid. Activated caspase-8 directly activates caspase cascade and/or cleaves bid. Truncated bid transduces death signal to mitochondria, which results in cytochrome c release from mitochondria. The vulnerability to apoptosis induced by death receptors or other apoptosis stimulators is variable from cell type to cell type. In some cells, Fas-mediated apoptosis is associated with disruption of mitochondrial polarity and cytochrome c release with caspase-9 activation (Gewies et al, 2000). However, this cross talk is reported to be usually minimal, and Fas-mediated and mitochondria-mediated pathways operate largely independently of each other (Gross et al, 1999; Hengartner, 2000; Yin et al, 1999). Moreover, since caspase-8- and caspase-9-deficient mice develop almost normally (Wang and Lenardo, 2000), additional apoptosis-pathways, such as caspase-independent pathway, exist and may associate with the pathophysiology of diseases.
Considering our previous studies and the current study, it is possible that multiple proapoptotic molecules interrelate with each other and potentiate epithelial cell apoptosis through death-receptors and the mitochondrial-mediated pathway in IIP. Recently, King et al (2001) demonstrated that the critical pathway to end-stage fibrosis is not in fact “alveolitis” but rather the ongoing epithelial damage and repair process associated with persistent fibroblastic proliferation. Therefore, protecting epithelial cells from apoptosis and maintaining their function may be the primary and most effective strategy against IIP.
Materials and Methods
Materials
This study of IIP was performed on 13 lung samples obtained by thoracoscopic lung biopsy. The diagnosis of IIP was established by a combination of medical history, physical examination, laboratory tests, chest roentgenograms, pulmonary function tests, and the results of histological findings, according to previously described criteria (American Thoracic Society, 2000). The histologic findings of lung biopsy specimens were compatible with those of UIP in eight patients and NSIP in five patients. The UIP patients comprised eight men, whose ages ranged from 42 to 67 years (mean, 58.6 years). Seven were smokers and one was a nonsmoker. The NSIP patients comprised three men and two women, whose ages ranged from 50 to 68 years (mean, 58.2 years). Two were smokers and three were nonsmokers. The results from the IIP specimens were compared with those from eight normal lung parenchyma specimens obtained by lobectomy for lung cancer of a solitary pulmonary nodule. The lung cancer patients comprised five men and three women, whose ages ranged from 56 to 78 years (mean, 67 years), and all were smokers. After the lung tissue was obtained, it was immediately frozen in liquid nitrogen and stored at −80° C for Western blot analysis. Formalin-fixed, paraffin-embedded lung tissues were used for TUNEL staining and immunohistochemistry.
The specific antibodies used in this study were as follows: goat polyclonal anti-human caspase-3 antibody (K-19) (Santa Cruz Biotechnology, Santa Cruz, California), rabbit polyclonal anti-human caspase-8 antibody (R&D Systems Inc., Minneapolis, Minnesota), rabbit polyclonal anti-human caspase-9 antibody (R&D Systems Inc.), rabbit anti-human cleaved caspase-3 polyclonal antibody (Cell Signaling Technology, Beverly, Maine), rabbit anti-cleaved caspase-9 polyclonal antibody (Cell Signaling Technology), rabbit anti-human cytochrome c antibody (C-20) (Santa Cruz Biotechnology), mouse anti-splicing factor SC-35 monoclonal antibody (Clone SC-35) (Sigma, St. Louis, Missouri), rabbit anti-human Ki-67 antigen antibody (DAKO, Tokyo, Japan), and rabbit anti-PCNA polyclonal antibody (FL-261) (Santa Cruz Biotechnology). The antibodies used for Western blot analysis and those used for immunohistochemistry were the same.
Western Blot Analysis
Frozen lung tissues were homogenized in buffer A (25 mm Hepes pH 7.5, 5 mm MgCl2, 1 mm EGTA, 1 mm phenylmethyl sulfonyl fluoride (PMSF), 1 μg/ml leupeptin, and 1 μg/ml aprotinin) using a polytron homogenizer (Kinematica, Luzern, Switzerland). Extracted protein was used for Western blot analysis for caspases except for cleaved caspase-3.
To assess the release of cytochrome c from the mitochondria to the cytoplasm, subcellular fractions were separately extracted according to the methods of Marti et al (2001). Frozen lung tissues were homogenized on ice for 30 seconds (6–8 strokes) with a Potter-Elvehjem homogenizer (Tokyo Rikakikai, Tokyo, Japan) in buffer A (25 mm Hepes pH 7.5, 5 mm MgCl2, 1 mm EGTA, 1 mm phenylmethyl sulfonyl fluoride (PMSF), 1 μg/ml leupeptin, and 1 μg/ml aprotinin). After incubation on ice for 10 minutes, extracts were vortexed for 10 seconds and centrifuged at 800 × g for 2 minutes at 4° C to pellet nuclei. The supernatant was centrifuged at 15,000 × g for 30 minutes at 4° C. The cleared supernatant was taken as the cytoplasmic extract and the pellet as the mitochondria-enriched fraction. The mitochondria-enriched fraction was directly dissolved in SDS-sample buffer and boiled. Nuclear pellets were incubated in 50 μl buffer B (25 mm Hepes pH 7.5, 420 mm NaCl, 5 mm MgCl2, 1 mm EGTA, 1 mm PMSF, 1 μg/ml leupeptin, and 1 μg/ml aprotinin, and 25% glycerol) on ice for 30 minutes and then centrifuged at 15,000 × g for 30 minutes at 4° C. The supernatant was taken as the nuclear extract and was used for Western blot analysis for cleaved caspase-3.
Protein concentrations were determined using the Bio-Rad protein assay (Bio-Rad Laboratories, Hercules, California). Thirty micrograms of protein were loaded in each column. Proteins were separated by SDS-polyacrylamide gel electrophoresis (SDS-PAGE). After SDS-PAGE, the proteins were transferred to a polyvinylidene fluoride hydrophobic membrane (Millipore, Bedford, Massachusetts). Membranes were blocked by 5% nonfat dry milk in Tris buffer saline containing 0.05% Tween-20 (TBST) at 4° C for 2 hours. The membranes were rinsed with TBST and incubated with specific antibodies in blocking buffer at 4° C overnight. After being rinsed, the membranes were incubated with HRP-conjugated secondary antibodies (Santa Cruz) for 30 minutes at room temperature. The blots were developed using an ECL western blotting detection kit (Amersham Pharmacia Biotech, Buckinghamshire, United Kingdom). Pictures of the membranes were taken and scanned. The images were analyzed using NIH image Ver.1.61 (National Institutes of Health, Bethesda, Maryland).
Electron Microscopy
We performed electron microscopy to investigate the morphologic changes in mitochondria in apoptotic epithelial cells in IIP. Lung tissues used for electron microscopy were obtained from three patients with UIP and one patient with NSIP. Lung tissues were fixed with 2.5% glutaraldehyde in 0.1 M phosphate buffer, pH 7.4, for 18 hours. Lung tissues were postfixed for 1.5 hours in 1% OsO4, dissolved in 0.1 M phosphate buffer (pH 7.4), and dehydrated through a series of graded ethanol solutions and embedded in Epon. Ultrathin sections were cut, stained with uranyl acetate and lead nitrate, and examined under a JEM-1200 EX transmission electron microscope (JEOL Co., Tokyo, Japan).
Apoptosis Analysis in Lung Tissues
Apoptosis was detected by the TUNEL method using the DeadEnd Colorimetric Apoptosis Detection system (Promega, Madison, Wisconsin). After proteinase digestion and the removing of endogenous peroxidase, the sections were incubated in a mixture containing TdT and fluorescein isothiocyanate-labeled dUTP. The sections were then treated with the peroxidase labeled with anti-fluorescein isothiocyanate antibody. The reaction products were developed with 3,3[prime]-diaminobenzidine tetrahydrochloride and counterstained with methyl green. The number of positive cells for TUNEL was counted in randomly selected 20 fields per section under a microscope with × 250 magnification. The number of positive cells is presented as percent of epithelial cells positive. The fibrotic grade for each field was also analyzed at the same time. DNA repair and replication, and RNA synthesis may be detected by the TUNEL method. To exclude these possibilities, we performed TUNEL staining and immunohistochemistry for PCNA, Ki67, and SC-35 using serial mirror sections.
Immunohistochemistry
The tissue samples were fixed in 10% formalin overnight and embedded in paraffin. A 5-μm paraffin section was adhered to slides pretreated with poly-l-lysine. These sections were dewaxed by washing three times, for 5 minutes each in xylene, then dehydrated in 100%, 95%, and 80% ethanol, for 5 minutes each, before finally being rinsed with distilled water. We used hydrated autoclaving as a pretreatment to immunostaining for cleaved caspase-3, PCNA, Ki67, and SC-35, but not the others, as previously described (Shin et al, 1991). Following deparaffinization in xylene and rehydration in ethanol, the tissue sections were autoclaved at 121° C for 10 minutes in a glass pot filled with enough distilled water to completely immerse the sections, before being washed three times in 0.1M PBS.
Immunohistochemistry was performed using a modified streptavidin-biotinylated peroxidase technique using a Histofine SAB-PO kit from Nichirei Corporation (Tokyo, Japan). Nonspecific protein staining was blocked by rabbit or goat serum for 30 minutes at room temperature. The sections were incubated with a primary antibody or a control nonspecific antibody at 4° C overnight. The sections were rinsed with PBS and incubated with biotinylated secondary antibodies for 30 minutes, before being washed again with PBS and treated with 0.3% hydrogen peroxide in methanol for 30 minutes to inhibit the activity of any endogenous per-oxide. The slides were washed, incubated with streptavidin-biotin-peroxidase complex for 30 minutes, and developed according to the manufacturer’s directions. The sections were lightly counterstained with hematoxylin and mounted.
The degree of staining in lung epithelial cells was graded from 0 to 3 according to the percentage of immunoreactive cells per bronchiolar and alveolar epithelial cells (0, 0%; 1, <25%; 2, 25–50%; 3, >50%) in each field with × 125 magnification. The grade of fibrosis in each field was also assessed using the previously described criteria (Ashcroft et al, 1988) with slight modifications from grade 0 to 5 (0, normal lung; 1, minimal fibrous thickening of alveolar or bronchiolar walls; 2, moderate thickening of walls without obvious damage to lung architecture; 3, increased fibrosis with definite damage to lung structure and formation of fibrous bands or small fibrous masses; 4, severe distortion of structure and large fibrous areas, “honeycomb lung” is placed in this category; 5, total fibrous obliteration throughout the field). The immunoreactivity grade and fibrotic grade in each field were determined at the same time by two observers. The two observers agreed with each other regarding each of the grades. Twenty to 50 fields were assessed for each case.
Statistics
The optical density of Western blot analysis and TUNEL assay were analyzed by ANOVA followed by Scheffe’s F test. The difference in the immunostaining grade was analyzed by Kruskal-Wallis test followed by Mann-Whitney U test. The correlation was assessed by Spearman’s rank correlation. Statistics were analyzed by using Abacus Concepts Statview 5 package. A p value of less than 0.05 was considered statistically significant.
References
American Thoracic Society (2000). Idiopathic pulmonary fibrosis: Diagnosis and treatment. International Consensus Statement. Am J Respir Crit Care Med 161: 646–664.
Ashcroft T, Simpson JM, and Timbrell V (1988). Simple method of estimating severity of pulmonary fibrosis on a numerical scale. J Clin Pathol 41: 467–470.
Auten RL, Whorton MH, and Nicholas Mason S (2002). Blocking neutrophil influx reduces DNA damage in hyperoxia-exposed newborn rat lung. Am J Respir Cell Mol Biol 26: 391–397.
Cantin AM, North SL, Fells GA, Hubbard RC, and Crystal RG (1987). Oxidant-mediated epithelial cell injury in idiopathic pulmonary fibrosis. J Clin Invest 79: 1665–1673.
Dinsdale D, Zhuang J, and Cohen GM (1999). Redistribution of cytochrome c precedes the caspase-dependent formation of ultracondensed mitochondria, with a reduced inner membrane potential, in apoptotic monocytes. Am J Pathol 155: 607–618.
Gavrieli Y, Sherman Y, and Ben-Sasson SA (1992b). Identification of programmed cell death in situ via specific labeling of nuclear DNA fragmentation. 119: 493–501.
Gewies A, Rokhlin OW, and Cohen MB (2000). Cytochrome c is involved in Fas-mediated apoptosis of prostatic carcinoma cell lines. Cancer Res 60: 2163–2168.
Gross A, Yin XM, Wang K, Wei MC, Jockel J, Milliman C, Erdjument-Bromage H, Tempst P, and Korsmeyer SJ (1999). Caspase cleaved BID targets mitochondria and is required for cytochrome c release, while BCL-XL prevents this release but not tumor necrosis factor-R1/Fas death. J Biol Chem 274: 1156–1163.
Hagimoto N, Kuwano K, Miyazaki H, Kunitake R, Fujita M, Kawasaki M, Kaneko Y, Nomoto Y, and Hara N (1997). Induction of apoptosis and pulmonary fibrosis in mice in response to ligation of Fas antigen. Am J Respir Cell Mol Biol 17: 272–278.
Hengartner MO (2000). The biochemistry of apoptosis. Nature 407: 770–776.
Ishizaki Y, Jacobson MD, and Raff MC (1998). A role for caspases in lens fiber differentiation. J Cell Biol 140: 153–158.
Isner JM, Kearney M, Bortman S, and Passeri J (1995). Apoptosis in human atherosclerosis and restenosis. Circulation 91: 2703–2711.
Kanoh M, Takemura G, Misao J, Hayakawa Y, Aoyama T, Nishigaki K, Noda T, Fujiwara T, Fukuda K, Minatoguchi S, and Fujiwara H (1999). Significance of myocytes with positive DNA in situ nick end-labeling (TUNEL) in hearts with dilated cardiomyopathy: Not apoptosis but DNA repair. Circulation 99: 2757–2764.
King TE Jr, Schwarz MI, Brown K, Tooze JA, Colby TV, Waldron JA Jr, Flint A, Thurlbeck W, and Cherniack RM (2001). Idiopathic pulmonary fibrosis: Relationship between histopathologic features and mortality. Am J Respir Crit Care Med 164: 1025–1032.
Kockx MM, Muhring J, Knaapen MW, and de Meyer GR (1998). RNA synthesis and splicing interferes with DNA in situ end labeling techniques used to detect apoptosis. Am J Pathol 152: 885–888.
Kroemer G and Reed JC (2000). Mitochondrial control of cell death. Nature Med 6: 513–519.
Kuwano K, Kunitake R, Kawasaki M, Nomoto Y, Hagimoto N, Nakanishi Y, and Hara N (1996). P21Waf1/Cip1/Sdi1 and p53 expression in association with DNA strand breaks in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 154: 477–483.
Kuwano K, Miyazaki H, Hagimoto N, Kawasaki M, Fujita M, Kunitake R, Kaneko Y, and Hara N (1999). The involvement of Fas-Fas ligand pathway in fibrosing lung diseases. Am J Respir Cell Mol Biol 20: 53–60.
Maeyama T, Kuwano K, Kawasaki M, Kunitake R, Hagimoto N, Matsuba T, Yoshimi M, Inoshima I, Yoshida K, and Hara N (2001). Upregulation of Fas-signalling molecules in lung epithelial cells from patients with idiopathic pulmonary fibrosis. Eur Respir J 17: 180–189.
Marti A, Ritter PM, Jager R, Lazar H, Baltzer A, Schenkel J, Declercq W, Vandenabeele P, and Jaggi R (2001). Mouse mammary gland involution is associated with cytochrome c release and caspase activation. Mech Dev 104: 89–98.
Matute-Bello G, Liles WC, Frevert CW, Nakamura M, Ballman K, Vathanaprida C, Kiener PA, and Martin TR (2001a). Recombinant human Fas ligand induces alveolar epithelial cell apoptosis and lung injury in rabbits. Am J Physiol Lung Cell Mol Physiol 281: L328–335.
Matute-Bello G, Winn RK, Jonas M, Chi EY, Martin TR, and Liles WC (2001b). Fas (CD95) induces alveolar epithelial cell apoptosis in vivo: Implications for acute pulmonary inflammation. Am J Pathol 158: 153–161.
Muller M, Wilder S, Bannasch D, Israeli D, Lehlbach K, Li-Weber M, Friedman SL, Galle PR, Stremmel W, Oren M, and Krammer PH (1998). p53 activates the CD95 (APO-1/Fas) gene in response to DNA damage by anticancer drugs. J Exp Med 188: 2033–2045.
O’Reilly MA (2001). DNA damage and cell cycle checkpoints in hyperoxic lung injury: Braking to facilitate repair. Am J Physiol Lung Cell Mol Physiol 281: L291–305.
Polnovsky VA, Chen B, Henke C, Snover D, Wendt C, Ingbar DH, and Bitterman PB (1993). Role of mesenchymal cell death in lung remodeling after injury. J Clin Invest 92: 388–397.
Sawhney N and Hall PA (1992). Ki67–structure, function, and new antibodies. J Pathol 168: 161–162.
Shin RW, Iwaki T, Kitamoto T, and Tateishi J (1991). Methods in laboratory investigation. Hydrated autoclave pretreatment enhances TAU Immunoreactivity in formalin-fixed normal and Alzheimer’s disease brain tissues. Lab Invest 64: 693–702.
Shivji KK, Kenny MK, and Wood RD (1992). Proliferating cell nuclear antigen is required for DNA excision repair. Cell 69: 367–374.
Stridh H, Kimland M, Jones DP, Orrenius S, and Hampton MB (1998). Cytochrome c release and caspase activation in hydrogen peroxide- and tributyltin-induced apoptosis. FEBS Lett 429: 351–355.
Suhara T, Fukuo K, Sugimoto T, Morimoto S, Nakahashi T, Hata S, Shimizu M, and Ogihara T (1998). Hydrogen peroxide induces up-regulation of Fas in human endothelial cells. J Immunol 160: 4042–4047.
Uberti D, Yavin E, Gil S, Ayasola KR, Goldfinger N, and Rotter V (1999). Hydrogen peroxide induces nuclear translocation of p53 and apoptosis in cells of oligodendroglia origin. Brain Res Mol Brain Res 65: 167–175.
Wang J and Lenardo MJ (2000). Roles of caspases in apoptosis, development, and cytokine maturation revealed by homozygous gene deficiencies. J Cell Sci 113: 753–757.
Weil M, Raff MC, and Braga VM (1999). Caspase activation in the terminal differentiation of human epidermal keratinocytes. Curr Biol 9: 361–364.
Yin XM, Wang K, Gross A, Zhao Y, Zinkel S, Klocke B, Roth KA, and Korsmeyer SJ (1999). Bid-deficient mice are resistant to Fas-induced hepatocellular apoptosis. Nature 400: 886–891.
Acknowledgements
This work was supported by a Grant-in-Aid for Scientific Research (13670604) from the Ministry of Education, Science, and Culture of Japan.
The English used in this manuscript was revised by Miss K. Miller (Royal English Language Centre, Fukuoka, Japan).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuwano, K., Hagimoto, N., Maeyama, T. et al. Mitochondria-Mediated Apoptosis of Lung Epithelial Cells in Idiopathic Interstitial Pneumonias. Lab Invest 82, 1695–1706 (2002). https://doi.org/10.1097/01.LAB.0000045084.81853.76
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1097/01.LAB.0000045084.81853.76
This article is cited by
-
SLC15A3 plays a crucial role in pulmonary fibrosis by regulating macrophage oxidative stress
Cell Death & Differentiation (2024)
-
Deterioration of alveolar development in mice with both HIF-3α knockout and HIF-2α knockdown
BMC Research Notes (2018)
-
Increased ectodomain shedding of cell adhesion molecule 1 as a cause of type II alveolar epithelial cell apoptosis in patients with idiopathic interstitial pneumonia
Respiratory Research (2015)
-
Targeting NOX enzymes in pulmonary fibrosis
Cellular and Molecular Life Sciences (2012)
-
1-oxoeudesm-11(13)-ene-12,8α-lactone-induced apoptosis via ROS generation and mitochondria activation in MCF-7 cells
Archives of Pharmacal Research (2011)