Key Points
-
Infections by microbes cause major diseases in the nervous system but are relatively neglected in the neuroscience community.
-
Mechanisms have evolved by which microbes can bypass the barriers that protect the nervous system and target neuronal populations in various regions of the brain.
-
Immune responses in the nervous system are generally not robust. This allows microbes to hide and survive in this relatively protective environment, but can also lead to rapid, life-threatening infections.
-
Knowledge on the fundamental cellular mechanisms used by microbes to propagate to the nervous system is important for developing host-directed drugs as adjunctive treatments with antimicrobial drugs.
-
Infections with microbes can have late-onset effects on nervous system functions, leading to behaviour changes and epilepsy. Research on the pathogenic events during these long latency periods could aid the development of strategies to prevent the appearance of these signs of disease.
-
Studies on the interactions between neurons and microbes also provide powerful tools to decipher basic neuronal functions and molecular sorting mechanisms.
Abstract
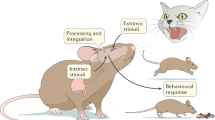
The nervous system is protected by barriers that restrict the invasion of pathogens. Nevertheless, mechanisms have evolved by which microbes can pass these barriers, enter and exit neurons and target various regions of the nervous system. In the brain, immune responses to pathogens are generally not robust, so microbes can hide and survive or, conversely, cause severe uncontrolled infections. Depending on their sites of entry and the regions that they target, microbes can cause diverse nervous system dysfunctions and even influence host behaviour to their own advantage. This Review discusses routes by which microbes can reach the nervous system and cause persistent or life-threatening infections.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Griffin, D. E. Emergence and re-emergence of viral diseases of the nervous system. Prog. Neurobiol. 91, 95–101 (2010).
Niederkorn, J. Y. See no evil, hear no evil, do no evil: the lessons of immune privilege. Nature Immunol. 7, 354–359 (2006).
Charles, P. C., Guida, J. D., Brosnan, C. F. & Horwitz, M. S. Mouse adenovirus type-1 replication is restricted to vascular endothelum in the CNS of susceptible strains of mice. Virology 245, 216–228 (1998).
Maisner, A. Neufeld, J. & Weingart, H. Organ- and endotheliotropism of Nipah virus infections in vivo and in vitro. Thromb. Haemost. 102, 1014–1023 (2009).
Ebrahimi, C. M. et al. Penetration of the blood–brain barrier by Bacillus anthracis requires the pXO1-encoded BslA protein. J. Bacteriol. 191, 7165–7173 (2009).
Warfel, J. M. & D'Agnillo, F. Anthrax lethal toxin enhances IκB kinase activation and differentially regulates pro-inflammatory genes in human endothelium. J. Biol. Chem. 284, 2571–2577 (2009).
Mankowski, J. L. et al. Neurovirulent simian immunodeficiency virus replicates productively in endothelial cells of the central nervous system in vivo and in vitro. J. Virol. 68, 8202–8208 (1994).
Bobardt, M. D. et al. Contribution of proteoglycans to human immunodeficiency virus type 1 brain invasion. J. Virol. 78, 6567–6584 (2004).
Alfonso, P. V. et al. Alteration of blood–brain barrier integrity by retroviral infection. PLoS Pathog. 4, e1000205 (2008).
Liou, M. L. & Hsu, C. Y. Japanese encephalitis virus is transported across the cerebral blood vessels by endocytosis in mouse brain. Cell Tissue Res. 293, 389–394 (1998).
Armulik, A. et al. Pericytes regulate the blood–brain barrier. Nature 468, 557–561 (2010).
Ludlow, M., Allen, I. & Schneider-Schaulis, J. Systemic spread of measles virus: overcoming the eipthelial and endothelial barriers. Thromb. Haemost. 102, 1050–1056 (2009).
Owens, T., Bechmann, I. & Engelhardt, B. Perivascular spaces and the two steps to neuroinflammation. J. Neuropathol. Exp. Neurol. 67, 1113–1121 (2008).
Sorokin, L. The impact of the extracellular matrix on inflammation. Nature Rev. Immunol. 10, 712–723 (2010). This study provides a detailed biochemical explanation of how various laminins in basement membranes can form networks with differences in resistance to cell penetration. It includes extensive references to the nervous system.
González-Scarano, F. & Martin-Garcia, J. The neuropathogenesis of AIDS. Nature Rev. Immunol. 5, 69–81 (2005).
Muratori, C., Mangino, G., Affabris, E. & Federico, M. Astrocytes contacting HIV-1-infected macrophages increase the release of CCL2 in response to the HIV-1-dependent enhancement of membrane-associated TNFα in macrophages. Glia 58, 1893–1904 (2010).
Clay, C. C. et al. Neuroinvasion of fluorescein-positive monocytes in acute simian immunodeficiency virus infection. J. Virol. 81, 12040–12048 (2007).
Drevets, D. A. & Bronze, M. S. Listeria monocytogenes: epidemiology, human disease, and mechanisms of brain invasion. FEMS Immunol. Med. Microbiol. 53, 151–165 (2008). This paper provides a good overview of mechanisms through which L. monocytogenes can spread to the nervous system of an infected individual.
Huang, S. H. & Jong, A. Y. Cellular mechanisms of microbial proteins contributing to invasion of the blood-brain barrier. Cell. Microbiol. 3, 277–287 (2001).
Lambert, H. & Barragan, A. Modelling parasite dissemination: host cell subversion and immune evasion by Toxoplasma gondii. Cell. Microbiol. 12, 292–300 (2010).
Kristensson, K., Nygård, M., Bertini, G. & Bentivoglio, M. African trypanosome infections of the nervous system: parasite entry and effects on neuronal functions. Prog. Neurobiol. 91, 152–171 (2010).
Amin, D. N. et al. Expression and role of CXCL10 during the encephalitic stage of experimental and clinical African trypanosomiasis. J. Infect. Dis. 200, 1556–1565 (2009).
Wang, T. et al. Toll-like receptor 3 mediates West Nile virus entry into the brain causing lethal encephalitis. Nature Med. 10, 1366–1373 (2004).
Wang, P. et al. Matrix metalloproteinase 9 facilitates West Nile virus entry into the brain. J. Virol. 82, 8978–8985 (2008).
Davis, L. E. et al. West Nile virus neuroinvasive disease. Ann. Neurol. 60, 286–300 (2006).
Combes, V., El-Assaad, F., Faille, D., Jambou, R., Hunt, N. H. & Grau, G. E. R. Microvesiculation and cell interactions at the brain–endothelial interface in cerebral malaria pathogenesis. Prog. Neurobiol. 91, 140–151 (2010). The original report of the release of microparticles in cerebral malaria; microparticles could potentially provide a new target for adjunctive therapy.
Vogt, A. M. et al. Release of sequestered malaria parasites upon injection of a glycosaminoglycan. PLoS Pathog. 2, 853–863 (2006).
Luuginbühl, A., Nikolic, M., Beck, H. P., Wahlgren, M. & Lutz, H. U. Complement factor D, albumin, and immunoglobulin G anti-band 3 protein antibodies mimic serum in promoting resetting of malaria-infected red blood cells. Infect. Immun. 75, 1771–1777 (2007).
Couper, K. N. et al. Parasite-derived plasma microparticles contribute significantly to malaria infection-induced inflammation through potent macrophage stimulation. PloS Pathog. 6, e1000744 (2010).
Mahnty, S. & Garcia, H. H. Cysticercosis and neurocysticercosis as pathogens affecting the nervous system. Prog. Neurobiol. 91, 172–184 (2010).
Wang, I.-C., Fan, P.-C., Lu, S. -C, Fan, C. K. & Su, K.-E. Suppresion of host Th1-type granulomatous inflammation by Taenia solium metacestodes is related to down-regulation of osteopontin gene expression. Int. J. Parasitol. 38, 239–248 (2008).
Alvarez, J. I. & Teale, J. M. Multiple expression of matrix metalloproteinases in murine neurocysticercosis: implications for leukocyte migration through multiple central nervous system barriers. Brain Res. 1214, 145–158 (2008).
Broadwell, R. D. & Sofroniew, M. V. Serum proteins bypass the blood–brain fluid barriers for extracellular entry to the central nervous system. Exp. Neurol. 120, 245–263 (1993).
Vu, K., Weksler, B., Romero, I., Couraud, P.-O. & Gelli. A. Immortalized human brain endothelial cell line HCMEC/D3 as a model of the blood–brain barrier facilitates in vitro studies of central nervous system infection by Cryptococcus neoformans. Eukaryotic Cell 8, 1803–1807 (2009).
Ring, A., Weiser, J. N. & Tuomanen, E. I. Pneumococcal trafficking across the blood–brain barrier molecular analysis of a novel bidirectional pathway. J. Clin. Invest. 102, 347–360 (1998).
Thornton, J. A., Durick-Eder, K. & Tuomanen, E. I. Pneumococcal pathogenesis: “innate invasion” yet organ-specific damage. J. Mol. Med. 88, 103–107 (2010).
Coureuil, M. et al. Meningococcus hijacks a β2-adrenoceptor/β-arrestin pathway to cross brain microvasculature endothelium. Cell 143, 1149–1160 (2010). A recent paper on the mechanisms used by meningococcus bacteria to cross the BBB.
van Ginkel, F. W. et al. Pneumococcal carriage results in ganglioside-mediated olfactory tissue infection. Proc. Natl Acad. Sci. USA 100, 14363–14367 (2003).
Tenenbaum, T. et al. Polar bacterial invasion and translocation of Streptococcus suis across the blood–cerebrospinal fluid barrier in vitro. Cell. Microbiol. 11, 323–336 (2009).
Domínguez-Punaro, M. C. et al. Streptococcus suis serotype 2, an important swine and human pathogen, induces strong systemic and cerebral inflammatory responses in a mouse model of infection. J. Immunol. 179, 1842–1854 (2007).
Rudd, P. A., Cattaneo, R. & von Messling, V. Canine distemper virus uses both the anterograde and the hematogenous pathway for neuroinvasion. J. Virol. 80, 9361–9370 (2006).
Christensen, J. E., de Lemos, C., Moos, T., Christensen, J. P. & Thomsen, A. R. CXCL10 is the key ligand for CXCR3 on CD8+ effector T cells involved in immune surveillance of the lymphocytic choriomeningitis virus-infected central nervous system. J. Immunol. 176, 4235–4243 (2006).
Thomsen, A. R. Lymphocytic choriomeningitis virus-induced central nervous system disease: a model for studying the role of chemokines in regulating the acute antiviral CD8+ T-cell response in an immune-privileged organ. J. Virol. 83, 20–28 (2009). A detailed review of the role of chemokines for the attraction or retention of T cells in the brain during a viral infection.
Kappes, D. J. et al. Protection of CD3 δ knockout mice from lymphocytic choriomeningitis virus-induced immunopathology: implications for viral neuroinvasion. Virology 269, 248–256 (2000).
Chen, H., Wood, C. & Petito, C. K. Comparisons of HIV-1 viral sequences in brain, choroid plexus and spleen: potential role of choroid plexus in the pathogenesis of HIV encephalitis. J. Neurovirol. 6, 498–506 (2000).
Kristensson, K. & Olsson, Y. Diffusion pathways and retrograde axonal transport of protein tracers in peripheral nerves. Prog. Neurobiol. 1, 87–109 (1973).
Mercer, J., Schelhaas, M. & Helenius, A. Virus entry by endocytosis. Annu. Rev. Biochem. 79, 803–820 (2011).
Radtke, K., Döhner, K. & Sodeik, B. Viral interactions with the cytoskeleton: a hitchhiker's guide to the cell. Cell. Microbiol. 8, 367–400 (2006).
Dollery, S. J., Delboy, M. G. & Nicola, A. V. Low pH-induced conformational change in herpes simplex virus glycoprotein B. J. Virol. 84, 3759–3766 (2010).
Salinas, S., Schiavo, G. & Kremer, E. J. A hitchhikers's guide to the nervous system: the complex journey of viruses and toxins. Nature Rev. Microbiol. 8, 645–655 (2010).
Lakadamyali, M., Rust, M. J. & Zhuang, X. Ligands for clathrin-mediated endocytosis are differentially sorted into distinct populations of early endosomes. Cell 124, 997–1009 (2006).
Klingen, Y., Conzelmann, K.-K. & Finke, S. Double-labeled rabies virus: live tracking of enveloped virus transport. J. Virol. 82, 237–245 (2008).
Lafon, M. Subversive neuroinvasive strategy of rabies virus. Arch. Virol. Suppl. 18, 149–159 (2004).
Salinas, S. et al. CAR-associated vesicular transport of an adenovirus in motor neuron axons. PloS Pathog. 5, e1000442 (2009).
Ohka, S. et al. Receptor-dependent and -independent axonal retrograde transport of poliovirus in motor neurons. J. Virol. 83, 4995–5004 (2009).
McGraw, H. M. & Friedman, H. M. Herpes simplex virus type 1 glycoprotein E mediates retrograde spread from epithelial cells to neurites. J. Virol. 83, 4791–4799 (2009).
Lee, J. I. et al. A herpesvirus encoded deubiquitinase is a novel neuroinvasive determinant. PloS Pathog. 5, e1000387 (2009).
Desai, P., DeLuca, N. A. & Person, S. Herpes simplex virus type 1 VP26 is not essential for replication in cell culture but influences production of infectious virus in the nervous system of infected mice. Virology 247, 115–124 (1998).
LaVail, J. H., Tauscher, A. N., Sucher, A., Harrabi, O. & Brandimarti, R. Viral regulation of the long distance axonal transport of herpes simplex virus nucleocapsid. Neuroscience 146, 974–985 (2007).
Miranda-Saksena, M. et al. Herpes simplex virus utilizes the large secretory vesicle pathway for anterograde transport of tegument and envelope proteins and for viral exocytosis from growth cones and human fetal axons. J. Virol. 83, 3187–3199 (2009).
Coller, K. E. & Smith G. A. Two viral kinases are required for sustained long distance axon transport of a neuroinvasive herpesvirus. Traffic 9, 1458–1470 (2008).
Curanovic´, D. & Enquist L. W. Directional transneuronal spread of α-herpesvirus infection. Future Virol. 4, 591–610 (2009). A comprehensive article on molecular mechanisms for the spread of various strains of herpesviruses in retrograde and anterograde directions in axons.
Dons, L., Jin, Y., Kristensson K. & Rottenberg, M. Axonal transport of Listeria monocytogenes and nerve-cell-induced bacterial killing. J. Neurosci. Rev. 85, 2529–2537 (2007).
Mohammed, A., Norrby, E. & Kristensson, K. Viruses and behavioural changes: a review of clinical and experimental findings. Rev. Neurosci. 4, 267–286 (1993).
Samuel, M. A., Wang, H., Siddharthan, V., Morrey, J. D. & Diamond, M. S. Axonal transport mediates West Nile virus entry into the central nervous system and induces acute flaccid paralysis. Proc. Natl Acad. Sci. USA 104, 17140–17145 (2007).
Morrey, J. D. et al. Increased blood brain barrier permeability is not a primary determinant for lethality of West Nile virus infection in rodents. J. Gen. Virol. 89, 467–473 (2008).
Yamada, M., Nakamura, K., Yoshii, M., Kaku, Y. & Narita, M. Brain lesions induced by experimental intranasal infection of Japanese encephalitis virus in piglets. J. Comp. Path. 141, 156–162 (2009).
Das, T. et al. Chikungunya fever: CNS infection and pathologies of a re-emerging arbovirus. Prog. Neurobiol. 91, 121–129 (2009).
Kiderlen, A. F. & Laube, U. Balamuthia mandrillaris, an opportunistic agent of granulomatous amebic encephalitis, infects the brain via the olfactory nerve pathway. Parasitol. Res. 94, 49–52 (2004).
Jung, S. Y. et al. Gene silencing of nfa1 affects the in vitro cytotoxicity of Naegleria fowleri in murine macrophages. Mol. Biochem. Parasitol. 165, 87–93 (2009).
Serrano-Luna, J., Cervantes-Sandoval, I., Tsutsumi, V. & Shibayama, M. A biochemical comparison of proteases from pathogenic Naegleria fowleri and non-pathogenic Naegleria gruberi. J. Eukaryot. Microbiol. 54, 411–417 (2007).
Backström, E., Ljunggren, H.-G. & Kristensson K. NK cell-mediated destruction of influenza A virus-infected peripheral but not central neurones. Scand. J. Immunol. 65, 353–361 (2007).
Decman, V., Kinchington, P. R., Harvey, S. A. K. & Hendricks, R. L. Gamma interferon can block herpes simplex virus type 1 reactivation from latency, even in the presence of late gene expression. J. Virol. 79, 10339–10347 (2005).
Neumann, H., Medana, I. M., Bauer, J. & Lassmann, H. Cytotoxic T lymphocytes in autoimmune and degenerative CNS diseases. Trends Neurosci. 25, 313–319 (2002).
Binder, G. K. & Griffin, D. E. Immune-mediated clearance of virus from the central nervous system. Microb. Infect. 5, 439–448 (2003).
Kristensson, K. & Norrby, E. Persistence of RNA viruses in the central nervous system. Ann. Rev. Microbiol. 40, 159–184 (1986).
Drögemüller, K. et al. Astrocyte gp130 expression is critical for the control of Toxoplasma encephalitis. J. Immunol. 181, 2683–2693 (2008).
Lafon, M. et al. Modulation of HLA-G expression in human neural cells after neurotropic viral infections. J. Virol. 79, 15226–15237 (2005).
Bock, M. & Stoye, J. P. Endogenous retroviruses and the human germline. Curr. Opin. Genet. Dev. 10, 651–655 (2000).
Mi, S. et al. Syncytin is a captive retroviral envelope protein ionvolved in human placental morphogenesis. Nature 403, 785–789 (2000).
Buckley, P. T. et al. Cytoplasmic intron sequence-retaining transcripts can be dendritically targeted via ID element retrotransposons. Neuron 69, 877–884 (2011). This paper may open up a new field of research on how retroviral elements could play a fundamental part in neuronal functions.
Prat, C. M. et al. Mutation of the protein kinase C site in Borna disease virus phosphoprotein abrogates viral interference with neuronal signaling and restores normal synaptic activity. PLoS Pathog. 5, 1–10 (2009).
Viviani, B., Gardoni, F. & Marinovich, M. Cytokines and neuronal ion channels in health and disease. Int. Rev. Neurobiol. 82, 247–263 (2007).
Lamberton, P. H., Donnelly, C. A. & Webster, J. P. Specificity of the Toxoplasma gondii-altered behaviour to definitive versus non-definitive host predation risk. Parasitology 135, 1143–1150 (2008).
Gulinello, M. et al. Acquired infection with Toxoplasma gondii in adult mice results in sensorimotor deficits but normal cognitive behavior despite widespread brain pathology. Microbes Infect. 12, 528–537 (2010).
Bingham, J. & van der Merwe, M. Distribution of rabies antigen in brain material: determining the reliability of different regions of the brain for the fluorescent antibody test. J. Virol. Meth. 101, 85–94 (2002).
Dellacasa-Lindberg, I., Hitziger, N. & Barragan, A. Localized recrudescence of Toxoplasma infections in the central nervous system of immunocompromised mice assessed by in vivo bioluminescence imaging. Microbes Infect. 9, 1291–1298 (2007).
Mansfield, K. L. et al. Tick-borne encephalitis virus — a review of an emerging zoonosis. J. Gen. Virol. 90, 1781–1794 (2009).
Murthy, J. M. K. & Prabhakar, S. Bacterial meningitis and epilepsy. Epilepsia 49, 8–12 (2008).
Misra, U. K., Tan, T. C. & Kalita, J. Viral encephalitis and epilepsy. Epilepsia 49, 13–18 (2008).
Idro, R., Ndiritu, M., Ogutu, B. & Mithwani, S. Burden, features, and outcome of neurological involvement in acute falciparum malaria in Kenyan children. JAMA 297, 2232–2240 (2007).
Palmer, B. S. Meta-analyses of three case controlled studies and an ecological study into the link between cryptogenic epilepsy and chronic toxoplasmosis infection. Seizure 16, 657–663 (2007).
Quet, F. et al. Meta-analysis of the association between cysticercosis and epilepsy in Africa. Epilepsia 51, 830–837 (2010).
Vezzani, A., French, J., Bartfai, T. & Baram, T. Z. The role of inflammation in epilepsy. Nature Rev. Neurol. 7, 31–40 (2011).
Stewart, K. A., Wilcox, K. S., Fujinami, R. S. & White, H. S. Theiler's virus infection chronically alters seizure susceptibility. Epilepsia 51, 1418–1428 (2010).
Vikman, K. S., Duggan, A. W. & Siddall, P. J. Interferon-γ induced disruption of GABAergic inhibition in the spinal dorsal horn in vivo. Pain 133, 18–28 (2007).
Pitkänen, A., Kharatishvili, I., Karhunen, H. & Lukasiuk, K. Epileptogenesis in experimental models. Epilepsia 48, 13–20 (2007).
Houweling, A. R., Bazhenov, M., Timofeev, I., Steriade, M. & Sejnowsski, T. J. Homeostatic synaptic plasticity can explain post-traumatic epileptogenesis in chronically isolated neocortex. Cereb. Cortex 15, 834–845 (2005).
Takeuchi, O. & Akira, S. Pattern recognition receptors and inflammation. Cell 140, 805–820 (2010).
Döring, A., Wild, M., Vestweber, D., Deutsch, U. & Engelhardt, B. E- and P-selectin are not required for the development of experimental autoimmune encephalomyelitis in C57BL/6 and SJL mice. J. Immunol. 179, 8470–8479 (2007).
Poteryaev, D., Datta, S., Ackema, K., Zerial, M. & Spang, A. Identification of the switch in early-to-late endosome transition. Cell 141, 497–508 (2010).
Deinhardt, K. et al. Rab5 and Rab7 control endocytic sorting along the axonal retrograde transport pathway. Neuron 52, 293–305 (2006).
Hirokawa, N., Niwa, S. & Tanaka, S. Molecular motors in neurons: transport mechanisms and roles in brain function, development, and disease. Neuron 68, 610–638 (2010). A comprehensive review on the molecular mechanisms for axonal transport. It also describes how disturbances to the transport machinery can cause distinct diseases.
Urbanska, E., Chambers, B. J., Ljunggren, H.-G., Norrby, E. & Kristensson. K. Spread of measles virus through axonal pathways into limbic structures in the brain of TAP1 -/- mice. J. Med. Virol. 52, 362–369 (1997).
Acknowledgements
The studies have been supported by grants from the Swedish Research Council (04480), European Commission (222887) and the US National Institutes of Health/Fogarty (5 R21 NS064888-02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing financial interests.
Related links
Glossary
- Neurovirulent
-
Refers to microbes that can replicate in the nervous system and cause functional disturbances.
- Blood–brain barrier
-
A structure that protects the brain from non-selective passage of molecules and toxins in the blood while still allowing essential metabolites to cross. It is composed of tightly linked endothelial cells surrounded by astrocyte cell projections that are termed astrocytic endfeet.
- Subarachnoid spaces
-
The space filled with cerebrospinal fluid between the arachnoid and the pia mater.
- Tight junctions
-
Structures apposed to the plasma membrane of adjacent endothelial cells. They consist of a network of sealing strands that prevent passage of extracellular fluids; ZO1 is a tight junction protein that is often used as a marker.
- Leptomeninges
-
The CNS is enclosed by three membranes — the outermost dura mater and the innermost pia mater with the arachnoid in between. The pia mater and the arachnoid are collectively called the leptomeninges.
- Monocytes
-
Mononuclear cells that are derived from the bone marrow and circulate in the bloodstream. They pass into the body tissues, where they can differentiate into various types of macrophages.
- Perivascular cuffs
-
Areas surrounding an inflamed blood vessel that contain inflammatory lymphocytes and are delimited by endothelial basement membrane on one side and parenchymal basement membrane on the other side.
- Neurovascular units
-
Microdomains in the brain formed by astrocytes that integrate neural circuitry with local blood flow. Astrocytic processes form a bridge between cerebral vessels and synapses, and both are covered by astrocytic membranes.
- Seizures
-
Transient abnormal, excessive or synchronous neuronal activity in the brain with clinical manifestations ranging from tonic spasm and clonic contractions of the muscles and convulsions to brief loss of awareness or psychic symptoms. Epilepsy signifies recurrent unprovoked seizures.
- Circumventricular organs
-
Except for area portrema in the fourth ventricle, these organs are all located along the wall of the third ventricle and include the subfornicular organ, the laminar terminalis, the subcommisural organ, the median eminence and the neurohypophysis. They have fenestrated, leaky vessels whereby, for instance, axons projecting from hypothalamic neurons can secrete products into the bloodstream, but they can also serve as chemoreceptors to regulate homeostatic functions.
- Perineurium
-
Layers of flattened cells that enclose fascicles of peripheral nerve fibres. The cells are joined by tight junctions, which prevent the diffusion of macromolecules into the enclosed nerve fibres.
- Endoneural vessels
-
Vessels within the endoneurium (all connective tissue elements and spaces enclosed by the perineurium) that have tight junctions between adjacent endothelial cells to prevent the diffusion of macromolecules from the blood into the endoneural spaces.
- Capsids
-
(From the Latin capsa, meaning box.) Protein shells that directly package viral DNA or RNA. The term nucleocapsid is sometimes used to describe the shell and its nucleic acid content.
- Peripheral ganglia
-
Ganglia of nerve cell bodies in the peripheral nervous system encompassing dorsal root ganglia and cranial ganglia of the somatic division as well as ganglia of the autonomic division.
Rights and permissions
About this article
Cite this article
Kristensson, K. Microbes' roadmap to neurons. Nat Rev Neurosci 12, 345–357 (2011). https://doi.org/10.1038/nrn3029
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrn3029
This article is cited by
-
Gram-negative bacteria and their lipopolysaccharides in Alzheimer’s disease: pathologic roles and therapeutic implications
Translational Neurodegeneration (2021)
-
An original infection model identifies host lipoprotein import as a route for blood-brain barrier crossing
Nature Communications (2020)
-
Macrophages at CNS interfaces: ontogeny and function in health and disease
Nature Reviews Neuroscience (2019)
-
Intranasal breast milk for premature infants with severe intraventricular hemorrhage—an observation
European Journal of Pediatrics (2019)
-
Unveiling Cerebral Leishmaniasis: parasites and brain inflammation in Leishmania donovani infected mice
Scientific Reports (2017)