Abstract
Statins are widely used in the evidence-based lowering of cardiovascular disease (CVD) risk. The use of these drugs for secondary prevention of CVD is well founded, but their expanding use in primary prevention—in individuals without documented CVD—has raised some concerns. Firstly, evidence suggests that, in primary prevention, statins substantially decrease CVD morbidity, but only moderately reduce CVD mortality. Secondly, long-term statin use might cause adverse effects, such as incident diabetes mellitus. Thirdly, the cost-effectiveness of such a strategy is unclear, and has to be balanced against the risk of 'overmedicating' the general population. Data clearly support the use of statins for primary prevention in high-risk individuals, in whom the strategy is cost-effective and the benefits exceed the risks. Whether primary prevention is beneficial in individuals at low or moderate risk is not certain. Therefore, the prescription of statins for primary prevention should be individualized on the basis of clinical judgment, particularly for low-risk individuals. In appropriately selected individuals, statins should also be used for primary prevention of ischaemic stroke and transient ischaemic attack.
Key Points
-
Large clinical trials and meta-analyses suggest that lowering the LDL-cholesterol level with statins in primary prevention modestly reduces all-cause mortality and substantially decreases the rate of cardiovascular events
-
Statins are recommended for primary prevention in nearly all high-risk individuals, whereas an individualized approach is recommended in those at moderate or low risk
-
Statins should be used for primary prevention of cardiovascular disease in women in the same manner as in men
-
Statins reduce cardiovascular risk when used for primary prevention in elderly individuals, but their use, particularly in high doses, requires clinical judgment and an individualized approach
-
Statins should be used for primary prevention of ischaemic stroke and transient ischaemic attack, at least in appropriately selected individuals
-
Low-cost, generic forms of statins are particularly cost-effective for primary prevention, especially in high-risk individuals
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Merkler, M. & Reiner, Ž. The burden of hyperlipidaemia and diabetes in cardiovascular diseases. Fundam. Clin. Pharmacol. 21 (Suppl. 2), 1–3 (2007).
Graham, I., Cooney, M. T., Bradley, D., Dudina, A. & Reiner, Ž. Dyslipidemias in the prevention of cardiovascular disease: risks and causality. Curr. Cardiol. Rep. 14, 709–720 (2012).
Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 344, 1383–1389 (1994).
The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N. Engl. J. Med. 339, 1349–1357 (1998).
Sacks, F. M. et al. Relationship between plasma LDL concentrations during treatment with pravastatin and recurrent coronary events in the Cholesterol and Recurrent Events trial. Circulation 97, 1446–1452 (1998).
Gould, A. L., Davies, G. M., Alemao, E., Yin, D. D. & Cook, J. R. Cholesterol reduction yields clinical benefits: meta-analysis including recent trials. Clin. Ther. 29, 778–794 (2007).
Baigent, C. et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366, 1267–1278 (2005).
Kotseva, K. et al. EUROASPIRE III. Management of cardiovascular risk factors in asymptomatic high-risk patients in general practice: cross-sectional survey in 12 European countries. Eur. J. Cardiovasc. Prev. Rehabil. 17, 530–540 (2010).
Eaton, C. B. et al. Family physician's knowledge, beliefs, and self-reported practice patterns regarding hyperlipidemia: a National Research Network (NRN) survey. J. Am. Board Fam. Med. 19, 46–53 (2006).
Reiner, Ž., Sonicki, Z. & Tedeschi-Reiner, E. Physicians' perception, knowledge and awareness of cardiovascular risk factors and adherence to prevention guidelines: The PERCRO-DOC survey. Atherosclerosis 213, 598–603 (2010).
Reiner, Ž., Sonicki, Z. & Tedeschi-Reiner, E. Public perceptions of cardiovascular risk factors in Croatia: the PERCRO survey. Prev. Med. 51, 494–496 (2010).
Dallongeville, J. et al. Survey of physicians' practices in the control of cardiovascular risk factors: the EURIKA study. Eur. J. Prev. Cardiol. 19, 541–550 (2012).
Young, F., Capewell, S., Ford, E. S. & Critchley, J. A. Coronary mortality declines in the U. S. between 1980 and 2000 quantifying the contributions from primary and secondary prevention. Am. J. Prev. Med. 39, 228–234 (2010).
Grundy, S. M. et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 110, 227–239 (2004).
Reiner, Ž. et al. ESC/EAS guidelines for the management of dyslipidaemias: the Task Force for the Management of Dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur. Heart J. 32, 1769–1818 (2011).
Perk, J. et al. European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur. Heart J. 33, 1635–1701 (2012).
Graham, I. et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur. Heart J. 28, 2375–2414 (2007).
Reiner, Ž. New ESC/EAS guidelines for the management of dyslipidaemias—any controversies behind the consensus? Eur. J. Cardiovasc. Prev. Rehabil. 18, 724–727 (2011).
Martin, S. S. et al. Friedewald estimated versus directly measured low-density lipoprotein cholesterol and treatment implications. J. Am. Coll. Cardiol. http://dx.doi.org/10.1016/j.jacc.2013.01.079.
Reiner, Ž. Guidelines, position papers and critical reviews: differences and similarities. Eur. J. Prev. Cardiol. 20, 3–5 (2013).
De Backer, G. et al. Guidelines on CVD prevention: confusing or complementary? Atherosclerosis 226, 299–300 (2012).
Zannad, F. et al. Prevention of cardiovascular disease guided by total risk estimations—challenges and opportunities for practical implementation: highlights of a CardioVascular Clinical Trialists (CVCT) Workshop of the ESC Working Group on CardioVascular Pharmacology and Drug Therapy. Eur. J. Prev. Cardiol. 19, 1454–1464 (2012).
Zannad, F. et al. Risk stratification in cardiovascular disease primary prevention—scoring systems, novel markers, and imaging techniques. Fundam. Clin. Pharmacol. 26, 163–174 (2012).
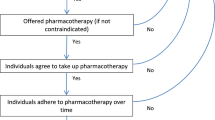
Perreault, S. et al. Persistence and determinants of statin therapy among middle-aged patients free of cardiovascular disease. Eur. J. Clin. Pharmacol. 61, 667–674 (2005).
Perreault, S. et al. Persistence and determinants of statin therapy among middle-aged patients for primary and secondary prevention. Br. J. Clin. Pharmacol. 59, 564–573 (2005).
Haffner, S. M., Lehto, S., Rönnemaa, T., Pyörälä, K. & Laakso, M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N. Engl. J. Med. 339, 229–324 (1998).
Palmer, S. C. et al. Benefits and harms of statin therapy for persons with chronic kidney disease: a systematic review and meta-analysis. Ann. Intern. Med. 157, 263–275 (2012).
Page, R. L. 2nd, Miller, G. G. & Lindenfeld, J. Drug therapy in the heart transplant recipient: part IV: drug–drug interactions. Circulation 111, 230–239 (2005).
Navaneethan, S. D. et al. HMG CoA reductase inhibitors (statins) for kidney transplant recipients. Cochrane Database of Systematic Reviews Issue 2. Art. No.: CD005019. http://dx.doi.org/10.1002/14651858.CD005019.pub3.
Lundgren, J. D. et al. European AIDS Clinical Society (EACS) guidelines on the prevention and management of metabolic diseases in HIV. HIV Med. 9, 72–81 (2008).
Rasmussen, L. D. et al. Statin therapy and mortality in HIV-infected individuals: a Danish nationwide population-based cohort study. PLoS ONE 8, e52828 (2013).
Shepherd, J. et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N. Engl. J. Med. 333, 1301–1307 (1995).
Ford, I. et al. Long-term follow-up of the West of Scotland Coronary Prevention Study. N. Engl. J. Med. 357, 1477–1486 (2007).
Clearfield, M. et al. Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS): efficacy and tolerability of long-term hypercholesterolemia and early atherosclerosis treatment with lovastatin in women. J. Women's Health Gender-Based Med. 10, 971–981 (2001).
Downs, J. R. et al. Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS): additional perspectives on tolerability of long-term treatment with lovastatin. Am. J. Cardiol. 87, 1074–1079 (2001).
Management of Elevated Cholesterol in the Primary Prevention Group of Adult Japanese (MEGA) Study Group. Design and baseline characteristics of a study of primary prevention of coronary events with pravastatin among Japanese with mildly elevated cholesterol levels. Circ. J. 68, 860–867 (2004).
Nakamura, H. et al. Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA study): a prospective randomised controlled trial. Lancet 368, 1155–1163 (2006).
Teramoto, T. et al. Association between lowering low-density lipoprotein cholesterol with pravastatin and primary prevention of cardiovascular disease in mild to moderate hypercholesterolemic Japanese. J. Atheroscler. Thromb. 17, 879–887 (2010).
Sever, P. S. et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial—Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet 361, 1149–1158 (2003).
Ridker, P. M. et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N. Engl. J. Med. 359, 2195–2207 (2008).
Morrissey, R. P., Diamond, G. A. & Kaul, S. The JUPITER trial: myth or reality? Curr. Atheroscler. Rep. 13, 413–421 (2011).
Yusuf, S., Lonn, E. & Bosch, J. Lipid lowering for primary prevention. Lancet 373, 1152–1155 (2009).
Thavendiranathan, P., Bagai, A., Brookhart, M. A. & Choudhry, N. K. Primary prevention of cardiovascular diseases with statin therapy: a meta-analysis of randomized controlled trials. Arch. Intern. Med. 166, 2307–2313 (2006).
Mills, E. J. et al. Primary prevention of cardiovascular mortality and events with statin treatments: a network meta-analysis involving more than 65,000 patients. J. Am. Coll. Cardiol. 52, 1769–1781 (2008).
Brugts, J. J. et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trials. BMJ 338, b2376 (2009).
Taylor, F. et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database of Systematic Reviews Issue 1. Art. No.: CD004816. http://dx.doi.org/10.1002/14651858.CD004816.pub4.
Ray, K. K. et al. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch. Intern. Med. 170, 1024–1031 (2010).
Mihaylova, B. et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 380, 581–590 (2012).
Ferket, B. et al. Personalized prediction of lifetime benefits with statin therapy for asymptomatic individuals: a modeling study. PLoS Med. 9, e1001361 (2012).
Kashani, A. et al. Risks associated with statin therapy: a systematic overview of randomized clinical trials. Circulation 114, 2788–2797 (2006).
Hoffman, K. B., Kraus, C., Dimbil, M. & Golomb, B. A. A survey of the FDA's AERS database regarding muscle and tendon adverse events linked to the statin drug class. PLoS ONE 7, e42866 (2012).
Alberton, M., Wu, P., Druyts, E., Briel, M. & Mills, E. J. Adverse events associated with individual statin treatments for cardiovascular disease: an indirect comparison meta-analysis. QJM 105, 145–157 (2012).
Athyros, V. G. et al. Safety and eficacy of long-term statin treatment for cardiovascular events in patients with coronary heart disease and abnormal liver tests in the Greek Atorvastatin and Coronary Heart Disease Evaluation (GREACE) study: a post-hoc analysis. Lancet 376, 1916–1922 (2010).
Preiss, D. et al. Lipid-modifying therapies and risk of pancreatitis: a meta-analysis. JAMA 308, 804–811 (2012).
Muldoon, M. F. et al. Effects of lovastatin on cognitive function and psychological well-being. Am. J. Med. 108, 538–546 (2000).
Dale, K. M., Coleman, C. I., Henyan, N. N., Kluger, J. & White, C. M. Statins and cancer risk: a meta-analysis. JAMA 295, 74–80 (2006).
Taylor, M. L., Wells, B. J. & Smolak, M. J. Statins and cancer: a meta-analysis of case–control studies. Eur. J. Cancer Prev. 17, 259–268 (2008).
Jakovljević, M., Reiner, Ž. & Milicˇic´, D. Mental disorders, treatment response, mortality and serum cholesterol: a new holistic look at old data. Psychiatr. Danub. 19, 270–281 (2007).
Baigent, C. et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 376, 1670–1681 (2010).
Ahern, T. P. et al. Statin prescriptions and breast cancer recurrence risk: a Danish nationwide prospective cohort study. J. Natl Cancer Inst. 103, 1461–1468 (2011).
Chiu, H. F., Ho, S. C., Chang, C. C., Wu, T. N. & Yang, C. Y. Statins are associated with a reduced risk of gastric cancer: a population-based case–control study. Am. J. Gastroenterol. 106, 2098–2103 (2011).
Leung, H. W., Chan, A. L., Lo, D., Leung, J. H. & Chen, H. L. Common cancer risk and statins: a population-based case–control study in a Chinese population. Expert Opin. Drug Saf. 12, 19–27 (2013).
Singh, S., Singh, P. P., Singh, A. G., Murad, M. H. & Sanchez, W. Statins are associated with a reduced risk of hepatocellular cancer: a systematic review and meta-analysis. Gastroenterology 144, 223–232 (2013).
Alsheikh-Ali, A. A., Trikalinos, T. A., Kent, D. M. & Karas, R. H. Statins, low-density lipoprotein cholesterol, and risk of cancer. J. Am. Coll. Cardiol. 52, 1141–1147 (2008).
Emberson, J. R. et al. Lack of effect of lowering LDL cholesterol on cancer: meta-analysis of individual data from 175,000 people in 27 randomised trials of statin therapy. PLoS ONE 7, e29849 (2012).
Park, H. S. et al. Statins and prostate cancer recurrence following radical prostatectomy or radiotherapy: a systematic review and meta-analysis. Ann. Oncol. 24, 1427–1434 (2013).
Zhang, X. L. et al. Statin use and risk of bladder cancer: a meta-analysis. Cancer Causes Control 24, 769–776 (2013).
Tan, M. et al. Statins and the risk of lung cancer: a meta-analysis. PLoS ONE 8, e57349 (2013).
Chan, T. F., Chiu, H. F., Wu, C. H., Lin, C. L. & Yang, C. Y. Statin use and the risk of esophageal cancer: a population-based case–control study. Expert Opin. Drug Saf. 12, 293–298 (2013).
Singh, S., Singh, A. G., Singh, P. P., Murad, M. H. & Iyer, P. G. Statins are associated with reduced risk of esophageal cancer, particularly in patients with Barrett's esophagus: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 11, 620–629 (2013).
Nielsen, S. F., Nordestgaard, B. G. & Bojesen, S. E. Statin use and reduced cancer-related mortality. N. Engl. J. Med. 367, 1792–1802 (2012).
Rajpathak, S. N. et al. Statin therapy and risk of developing type 2 diabetes: a meta-analysis. Diabetes Care 32, 1924–1929 (2009).
Sattar, N. et al. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 375, 735–742 (2010).
Culver, A. L. et al. Statin use and risk of diabetes mellitus in postmenopausal women in the Women's Health Initiative. Arch. Intern. Med. 172, 144–152 (2012).
Preiss, D. et al. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA 305, 2556–2564 (2011).
Freeman, D. J. et al. Pravastatin and the development of diabetes mellitus: evidence for a protective treatment effect in the West of Scotland Coronary Prevention Study. Circulation 103, 357–362 (2001).
Ridker, P. M., Pradhan, A., MacFadyen, J. G., Libby, P. & Glynn, R. J. Cardiovascular benefits and diabetes risks of statin therapy in primary prevention: an analysis from the JUPITER trial. Lancet 380, 565–571 (2012).
Barham, A. H. et al. Appropriateness of cholesterol management in primary care by sex and level of cardiovascular risk. Prev. Cardiol. 12, 95–101 (2009).
Vulic, D., Lee, B. T., Dede, J., Lopez, V. A. & Wong, N. D. Extent of control of cardiovascular risk factors and adherence to recommended therapies in US multiethnic adults with coronary heart disease: from a 2005–2006 national survey. Am. J. Cardiovasc. Drugs 10, 109–114 (2010).
Driscoll, A. et al. Suboptimal management of cardiovascular risk factors in coronary heart disease patients in primary care occurs particularly in women. Intern. Med. J. 41, 730–736 (2011).
Sheppard, J. P., Singh, S., Fletcher, K., McManus, R. J. & Mant, J. Impact of age and sex on primary preventive treatment for cardiovascular disease in the West Midlands, UK: cross sectional study. BMJ 345, e4535 (2012).
Petretta, M., Costanzo, P., Perrone-Filardi, P. & Chiariello, M. Impact of gender in primary prevention of coronary heart disease with statin therapy: a meta-analysis. Int. J. Cardiol. 138, 25–31 (2010).
Bukkapatnam, R. N., Gabler, N. B. & Lewis, W. R. Statins for primary prevention of cardiovascular mortality in women: a systematic review and meta-analysis. Prev. Cardiol. 13, 84–90 (2010).
Kostis, W. J., Cheng, J. Q., Dobrzynski, J. M., Cabrera, J. & Kostis, J. B. Meta-analysis of statin effects in women versus men. J. Am. Coll. Cardiol. 59, 572–582 (2012).
Mora, S. et al. Statins for the primary prevention of cardiovascular events in women with elevated high-sensitivity C-reactive protein or dyslipidemia: results from the Justification for the Use of Statins in Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER) and meta-analysis of women from primary prevention trials. Circulation 121, 1069–1077 (2010).
Lemaitre, R. N. et al. Time trends in the use of cholesterol-lowering agents in older adults: the Cardiovascular Health Study. Arch. Intern. Med. 158, 1761–1718 (1998).
Whincup, P. H. et al. Low prevalence of lipid lowering drug use in older men with established coronary heart disease. Heart 88, 25–29 (2002).
Ko, D. T., Mamdani, M. & Alter, D. A. Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA 291, 1864–1870 (2004).
Gnavi, R. et al. Statins prescribing for the secondary prevention of ischaemic heart disease in Torino, Italy: a case of ageism and social inequalities. Eur. J. Public Health 17, 492–496 (2007).
Niska, R. & Han, B. Statins for secondary cardiovascular disease prevention for older primary care patients. J. Natl Med. Assoc. 101, 705–710 (2009).
Robinson, J. G. & Booth, B. Statin use and lipid levels in older adults: National Health and Nutrition Examination Survey, 2001 to 2006. J. Clin. Lipidol. 4, 483–490 (2010).
Downs, J. R. et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA 279, 1615–1622 (1998).
Nakaya, N. et al. Low-dose pravastatin and age-related differences in risk factors for cardiovascular disease in hypercholesterolaemic Japanese: analysis of the management of elevated cholesterol in the primary prevention group of adult Japanese (MEGA study). Drugs Aging 28, 681–692 (2011).
Shepherd, J. et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet 360, 1623–1630 (2002).
Glynn, R. J., Koenig, W., Nordestgaard, B. G., Shepherd, J. & Ridker, P. M. Rosuvastatin for primary prevention in older persons with elevated C-reactive protein and low to average low-density lipoprotein cholesterol levels: exploratory analysis of a randomized trial. Ann. Intern. Med. 152, 488–496 (2010).
Zieman, S. J. & Ouyang, P. Statins for primary prevention in older adults: who is high risk, who is old, and what denotes primary prevention? Ann. Intern. Med. 152, 528–530 (2010).
Setoguchi, S., Glynn, R. J., Avorn, J., Mogun, H. & Schneeweiss, S. Statins and the risk of lung, breast, and colorectal cancer in the elderly. Circulation 115, 27–33 (2007).
Hunt, D. et al. Benefits of pravastatin on cardiovascular events and mortality in older patients with coronary heart disease are equal to or exceed those seen in younger patients: results from the LIPID trial. Ann. Intern. Med. 134, 931–940 (2001).
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 128 (Suppl. 5), S213–S256 (2011).
de Jongh, S. et al. Early statin therapy restores endothelial function in children with familial hypercholesterolemia. J. Am. Coll. Cardiol. 40, 2117–2121 (2002).
Wiegman, A. et al. Efficacy and safety of statin therapy in children with familial hypercholesterolemia: a randomized controlled trial. JAMA 292, 331–337 (2004).
Rodenburg, J. et al. Statin treatment in children with familial hypercholesterolemia: the younger, the better. Circulation 116, 664–668 (2007).
Berenson, G. S. et al. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults: the Bogalusa Heart Study. N. Engl. J. Med. 338, 1650–1656 (1998).
Kurth, T. et al. Lipid levels and the risk of ischemic stroke in women. Neurology 68, 556–562 (2007).
Amarenco, P. & Labreuche, J. Lipid management in the prevention of stroke: review and updated meta-analysis of statins for stroke prevention. Lancet Neurol. 8, 453–463 (2009).
O'Regan, C., Wu, P., Arora, P., Perri, D. & Mills, E. J. Statin therapy in stroke prevention: a meta-analysis involving 121,000 patients. Am. J. Med. 121, 24–33 (2008).
Amarenco, P. et al. High-dose atorvastatin after stroke or transient ischemic attack. N. Engl. J. Med. 355, 549–559 (2006).
Hackam, D. G. et al. Statins and intracerebral hemorrhage: a retrospective cohort study. Arch. Neurol. 69, 39–45 (2012).
McKinney, J. S. & Kostis, W. J. Statin therapy and the risk of intracerebral hemorrhage: a meta-analysis of 31 randomized controlled trials. Stroke 43, 2149–2156 (2012).
Wagner, M. et al. Cost-effectiveness of intensive lipid lowering therapy with 80 mg of atorvastatin, versus 10 mg of atorvastatin, for secondary prevention of cardiovascular disease in Canada. Can. J. Clin. Pharmacol. 16, e331–e345 (2009).
Taylor, D. C. et al. Cost-effectiveness of atorvastatin therapy in secondary cardiovascular prevention in the United Kingdom, Spain, and Germany, based on the Treating to New Targets Study. Eur. J. Health Econ. 10, 255–265 (2009).
De Smedt, D. et al. Cost-effectiveness of optimizing prevention in patients with coronary heart disease: the EUROASPIRE III Health Economics Project. Eur. Heart. J. 33, 2865–2872 (2012).
Mitchell, A. P. & Simpson, R. J. Statin cost effectiveness in primary prevention: a systematic review of the recent cost-effectiveness literature in the United States. BMC Res. Notes 5, 373 (2012).
Brugts, J. J. & Deckers, J. W. Statin prescription in men and women at cardiovascular risk: to whom and when? Curr. Opin. Cardiol. 25, 484–489 (2010).
Calonge, N. et al. Aspirin for the prevention of cardiovascular disease: U. S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 150, 396–404 (2009).
Wright, J. M. & Musini, V. M. First-line drugs for hypertension. Cochrane Database of Systematic Reviews Issue 3. Art. No.: CD001841. http://dx.doi.org/10.1002/14651858.CD001841.pub2.
Pletcher, M. J. et al. Comparing impact and cost-effectiveness of primary prevention strategies for lipid-lowering. Ann. Intern. Med. 150, 243–254 (2009).
Ito, M. K. et al. Statins for cardiovascular prevention according to different strategies: a cost analysis. Am. J. Cardiovasc. Drugs 11, 33–44 (2011).
MacDonald, G. P. Cost-effectiveness of rosuvastatin for primary prevention of cardiovascular events according to Framingham Risk Score in patients with elevated C-reactive protein. J. Am. Osteopath. Assoc. 110, 427–436 (2010).
Lazar, L. D., Pletcher, M. J., Coxson, P. G., Bibbins-Domingo, K. & Goldman, L. Cost-effectiveness of statin therapy for primary prevention in a low-cost statin era. Circulation 124, 146–153 (2011).
Schwartz, J. S. Primary prevention of coronary heart disease with statins: it's not about the money. Circulation 124, 130–132 (2011).
Greving, J. P., Visseren, F. L., de Wit, G. A. & Algra, A. Statin treatment for primary prevention of vascular disease: whom to treat? Cost-effectiveness analysis. BMJ 342, d1672 (2011).
Erickson, K. F. et al. Cost-effectiveness of statins for primary cardiovascular prevention in chronic kidney disease. Am. Coll. Cardiol. 61, 1250–1258 (2013).
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author declares that he has received honoraria from the following companies: Abbot, AstraZeneca, Bayer, and Sanofi.
Rights and permissions
About this article
Cite this article
Reiner, Ž. Statins in the primary prevention of cardiovascular disease. Nat Rev Cardiol 10, 453–464 (2013). https://doi.org/10.1038/nrcardio.2013.80
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2013.80
This article is cited by
-
Prevalence and trend of multiple coronary artery disease risk factors and their 5-year incidence rate among adult population of Kerman: results from KERCADR study
BMC Public Health (2024)
-
Target-Based Virtual and Biochemical Screening Against HMG-CoA Reductase Reveals Allium sativum-Derived Organosulfur Compound N-Acetyl Cysteine as a Cardioprotective Agent
Revista Brasileira de Farmacognosia (2022)
-
Healthcare resource utilization in patients on lipid-lowering therapies outside Western Europe and North America: findings of the cross-sectional observational International ChoLesterol management Practice Study (ICLPS)
Lipids in Health and Disease (2020)
-
Low-density lipoprotein cholesterol lowering treatment: the current approach
Lipids in Health and Disease (2020)
-
The therapeutic potential of BRD4 in cardiovascular disease
Hypertension Research (2020)