Abstract
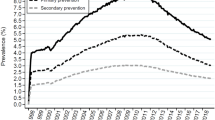
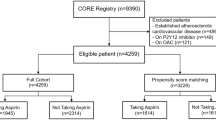
The benefits of aspirin therapy for the secondary prevention of cardiovascular disease clearly outweigh the risks of bleeding, and low-dose aspirin is uniformly recommended in this setting. However, no clear consensus exists about whether, and if so in whom, aspirin therapy is appropriate for the primary prevention of cardiovascular disease. Three trials of low-dose aspirin versus placebo in three populations at increased risk of myocardial infarction or ischaemic stroke in the absence of established cardiovascular disease were reported in 2018. The ASPREE trial in elderly people was terminated early for futility because aspirin had no effect on disability-free survival but significantly increased the risk of major haemorrhage and, unexpectedly, all-cause mortality. In the ASCEND trial in patients with diabetes mellitus and no evidence of vascular disease, aspirin significantly reduced serious vascular events but increased major bleeding. In the ARRIVE trial in people with multiple risk factors for cardiovascular disease, aspirin had no effect on major cardiovascular events but increased gastrointestinal bleeding. The aim of this Review is to place these new results in the context of previous evidence on aspirin for the primary prevention of cardiovascular disease and to appraise whether the new evidence is likely to enable the more targeted use of aspirin in particular individuals for whom the net benefit is both clinically worthwhile and statistically definite.
Key points
-
The benefits of aspirin therapy for the secondary prevention of cardiovascular disease (CVD) clearly outweigh the risks of bleeding, but whether to recommend low-dose aspirin for primary prevention of CVD is controversial.
-
Use of risk scores for vascular events and major extracranial bleeds to classify individual participant data from a meta-analysis shows that individuals at the highest risk of vascular events are also at the highest risk of bleeding.
-
In 2018, results from three trials of low-dose aspirin in three populations at increased risk of myocardial infarction or ischaemic stroke in the absence of established CVD added to the evidence base.
-
Overall, other than for myocardial infarction, the effects of aspirin on the other major efficacy and safety outcomes seem similar in all the primary prevention trials, including the three (ASPREE, ASCEND and ARRIVE) completed in 2018.
-
The main challenge when assessing the net benefit of aspirin is that benefits and risks are strongly correlated; therefore, identifying large numbers of people at high risk of vascular ischaemia but low risk of bleeding is difficult.
-
New approaches are required to overcome this challenge, perhaps combining coronary imaging to identify apparently healthy people at substantially increased risk of vascular events with gastroprotectant therapy to reduce the risk of bleeding.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Patrono, C., García Rodríguez, L. A., Landolfi, R. & Baigent, C. Low-dose aspirin for the prevention of atherothrombosis. N. Engl. J. Med. 353, 2373–2383 (2005).
Patrono, C. Low-dose aspirin in primary prevention: cardioprotection, chemoprevention, both or neither? Eur. Heart J. 34, 2403–2411 (2013).
Cleland, J. G. Is aspirin useful in primary prevention? Eur. Heart J. 34, 3412–3418 (2013).
Peto, R. et al. Randomised trial of prophylactic daily aspirin in British male doctors. BMJ 296, 313–316 (1988).
Steering Committee of the Physicians’ Health Study Research Group. Final report on the aspirin component of the ongoing Physicians’ Health Study. N. Engl. J. Med. 321, 129–135 (1989).
Vandvik, P. O. et al. Primary and secondary prevention of cardiovascular disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141 (Suppl. 2), e637S–e668S (2012).
Rydén, L. et al. ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, prediabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur. Heart J. 34, 3035–3087 (2013).
American Diabetes Association. 10. Cardiovascular disease and risk management: Standards of medical care in diabetes. Diabetes Care 42 (Suppl. 1), S103–S123 (2019).
Piepoli, M. F. et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention and Rehabilitation (EACPR). Eur. Heart J. 37, 2315–2381 (2016).
Bibbins-Domingo, K. & U.S. Preventive Services Task Force. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 164, 836–845 (2016).
Arnett, D. K. et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease. J. Am. Coll. Cardiol. https://doi.org/10.1016/j.jacc.2019.03.010 (2019).
McNeil, J. J. et al. Effect of aspirin on disability-free survival in the healthy elderly. N. Engl. J. Med. 379, 1499–1508 (2018).
McNeil, J. J. et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N. Engl. J. Med. 379, 1509–1518 (2018).
McNeil, J. J. et al. Effect of aspirin on all-cause mortality in the healthy elderly. N. Engl. J. Med. 379, 1519–1528 (2018).
The ASCEND Study Collaborative Group. Effects of aspirin for primary prevention in persons with diabetes mellitus. N. Engl. J. Med. 379, 1529–1539 (2018).
Gaziano, J. M. et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet 392, 1036–1046 (2018).
Patrignani, P. & Patrono, C. Aspirin and cancer. J. Am. Coll. Cardiol. 68, 967–976 (2016).
Patrono, C. The multifaceted clinical read-outs of platelet inhibition by low-dose aspirin. J. Am. Coll. Cardiol. 66, 74–85 (2015).
Loll, P. J., Picot, D. & Garavito, R. M. The structural basis of aspirin activity inferred from the crystal structure of inactivated prostaglandin H2 synthase. Nat. Struct. Biol. 2, 637–643 (1995).
Patrignani, P. et al. Reappraisal of the clinical pharmacology of low-dose aspirin by comparing novel direct and traditional indirect biomarkers of drug action. J. Thromb. Haemost. 12, 1320–1330 (2014).
Patrignani, P., Filabozzi, P. & Patrono, C. Selective cumulative inhibition of platelet thromboxane production by low-dose aspirin in healthy subjects. J. Clin. Invest. 69, 1366–1372 (1982).
Pedersen, A. K. & FitzGerald, G. A. Dose-related kinetics of aspirin: presystemic acetylation of platelet cyclooxygenase. N. Engl. J. Med. 311, 1206–1211 (1984).
Patrono, C., Baigent, C., Hirsh, J. & Roth, G. Antiplatelet drugs: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest 133, 199S–233S (2008).
Rocca, B. et al. Antithrombotic therapy and body mass: an expert position paper of the ESC Working Group on Thrombosis. Eur. Heart J. 39, 1672–1686f (2018).
Giaretta, A., Rocca, B., Di Camillo, B., Toffolo, G. M. & Patrono, C. In silico modeling of the antiplatelet pharmacodynamics of low-dose aspirin in health and disease. Clin. Pharmacol. Ther. 102, 823–831 (2017).
Pascale, S. et al. Aspirin-insensitive thromboxane biosynthesis in essential thrombocythemia is explained by accelerated renewal of the drug target. Blood 119, 3595–3603 (2012).
Rocca, B. et al. The recovery of platelet cyclooxygenase activity explains interindividual variability in responsiveness to low-dose aspirin in patients with and without diabetes. J. Thromb. Haemost. 10, 1220–1230 (2012).
Tefferi, A., Vannucchi, A. M. & Barbui, T. Essential thrombocythemia treatment algorithm 2018. Blood Cancer J. 8, 2 (2018).
Murata, T. et al. Altered pain perception and inflammatory response in mice lacking prostacyclin receptor. Nature 388, 678–682 (1997).
Coxib and traditional NSAID Trialists’ (CNT) Collaboration. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet 382, 769–779 (2013).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT02697916 (2019).
Ridker, P. M. et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N. Engl. J. Med. 352, 1293–1304 (2005).
Hansson, L. et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet 351, 1755–1762 (1998).
Kassoff, A. et al. Aspirin effects on mortality and morbidity in patients with diabetes mellitus. Early treatment diabetic retinopathy study report 14. JAMA 268, 1292–1300 (1992).
Belch, J. et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ 337, a1840 (2008).
Ogawa, H. et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA 300, 2134–2141 (2008).
Fowkes, F. G. et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA 303, 841–848 (2010).
de Gaetano, G. et al. Low-dose aspirin and vitamin E in people at cardiovascular risk: a randomised trial in general practice. Lancet 357, 89–95 (2001).
The Medical Research Council’s General Practice Research Framework. Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet 351, 233–241 (1998).
Ikeda, Y. et al. Low-dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: a randomized clinical trial. JAMA 312, 2510–2520 (2014).
Antithrombotic Trialists’ (ATT) Collaboration. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 373, 1849–1860 (2009).
Guirguis-Blake, J. M., Evans, C. V., Senger, C. A., O’Connor, E. A. & Whitlock, E. P. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 164, 804–813 (2016).
Whitlock, E. P., Burda, B. U., Williams, S. B., Guirguis-Blake, J. M. & Evans, C. V. Bleeding risks with aspirin use for primary prevention in adults: a systematic review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 164, 826–835 (2016).
Baigent, C. Aspirin for disease prevention: public policy or personal choice? Ann. Intern. Med. 164, 846–847 (2016).
Davì, G. et al. Thromboxane biosynthesis and platelet function in type-II diabetes mellitus. N. Engl. J. Med. 322, 1769–1774 (1990).
Zheng, S. L. & Roddick, A. J. Association of aspirin use for primary prevention with cardiovascular events and bleeding events. A systematic review and meta-analysis. JAMA 321, 277–287 (2019).
García Rodríguez, L. A., Hernández-Díaz, S. & de Abajo, F. J. Association between aspirin and upper gastrointestinal complications: systematic review of epidemiologic studies. Br. J. Clin. Pharmacol. 52, 563–571 (2001).
Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high-risk patients. BMJ 324, 71–86 (2002).
Lanas, A. & Chan, F. K. L. Peptic ulcer disease. Lancet 390, 613–624 (2017).
Moayyedi, P. et al. Pantoprazole to prevents gastroduodenal events in patients receiving rivaroxaban and/or aspirin in a randomized, double-blind, placebocontrolled trial.Gastroenterology https://doi.org/10.1053/j.gastro.2019.04.041 (2019).
Scally, B. et al. Effects of gastroprotectant drugs for the prevention and treatment of peptic ulcer disease and its complications: a meta-analysis of randomised trials. Lancet Gastroenterol. Hepatol. 3, 231–241 (2018).
Focks, J. J. et al. Concomitant use of clopidogrel and proton pump inhibitors: impact on platelet function and clinical outcome- a systematic review. Heart 99, 520–527 (2013).
Yu, E. W., Bauer, S. R., Bain, P. A. & Bauer, D. C. Proton pump inhibitors and risk of fractures: a meta analysis of 11 international studies. Am. J. Med. 124, 519–526 (2011).
Janarthanan, S., Ditah, I., Adler, D. G. & Ehrinpreis, M. N. Clostridium difficile-associated diarrhea and proton pump inhibitor therapy: a meta-analysis. Am. J. Gastroenterol. 107, 1001–1010 (2012).
Greenland, P., Blaha, M. J., Budoff, M. J., Erbel, R. & Watson, K. E. Coronary calcium score and cardiovascular risk. J. Am. Coll. Cardiol. 72, 434–447 (2018).
Dehmer, S. P., Maciosek, M. V., Flottemesch, T. J., LaFrance, A. B. & Whitlock, E. P. Aspirin for the primary prevention of cardiovascular disease and colorectal cancer: a decision analysis for the US Preventive Services Task Force. Ann. Intern. Med. 164, 777–786 (2016).
Dorresteijn, J. A. N. et al. Aspirin for primary prevention of vascular events in women: individualized prediction of treatment effects. Eur. Heart J. 32, 2962–2969 (2011).
van Kruijsdijk, R. C. M. et al. Individualized prediction of alternate-day aspirin treatment on the combined risk of cancer, cardiovascular disease and gastro-intestinal bleeding in healthy women. Heart 101, 369–376 (2015).
Bonaca, M. P. et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N. Engl. J. Med. 372, 1791–1800 (2015).
Eikelboom, J. W. et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N. Engl. J. Med. 377, 1319–1330 (2017).
Lin, J. S. et al. Nontraditional risk factors in cardiovascular disease risk assessment: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 320, 281–297 (2018).
Gachet, C. Antiplatelet drugs: which targets for which treatments? J. Thromb. Haemost. 13 (Suppl. 1), S313–S322 (2015).
De Stefano, V. et al. The Aspirin Regimens in Essential Thrombocythemia (ARES) phase II randomized trial design: implementation of the serum thromboxane B2 assay as an evaluation tool of different dosing regimens in the clinical setting. Blood. Cancer J. 8, 49 (2018).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT02520921 (2009).
Rocca, B. & Patrono, C. Determinants of the interindividual variability in response to antiplatelet drugs. J. Thromb. Haemost. 8, 1597–1602 (2005).
Author information
Authors and Affiliations
Contributions
Both authors researched data for the article, discussed its content, wrote the manuscript and reviewed and edited it before submission.
Corresponding author
Ethics declarations
Competing interests
C.P. reports consulting and lecture fees from Acticor Biotech, Amgen, Bayer, GlaxoSmithKline and Zambon and institutional research grants from Bayer, Cancer Research UK (Catalyst Award — Aspirin for Cancer Prevention Collaboration), the European Commission and the Italian Drug Agency (AIFA); he serves as chairperson of the Scientific Advisory Board of the International Aspirin Foundation. C.B. reports grants from Boehringer Ingelheim, the British Heart Foundation, the Medical Research Council and the UK National Institute for Health Research.
Additional information
Peer review information
Nature Reviews Cardiology thanks P. Gurbel, and the other anonymous reviewer(s), for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ADAPTABLE trial: https://theaspirinstudy.org
Rights and permissions
About this article
Cite this article
Patrono, C., Baigent, C. Role of aspirin in primary prevention of cardiovascular disease. Nat Rev Cardiol 16, 675–686 (2019). https://doi.org/10.1038/s41569-019-0225-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-019-0225-y
This article is cited by
-
Lipoprotein(a), platelet function and cardiovascular disease
Nature Reviews Cardiology (2024)
-
Bio-prospective of Acidophile Microorganisms in Biodegradation of NSAIDs
Current Pollution Reports (2024)
-
The role of non-steroidal anti-inflammatory drugs as adjuncts to periodontal treatment and in periodontal regeneration
Journal of Translational Medicine (2023)
-
Meloxicam inhibits STING phosphorylation and alleviates intracellular DNA-mediated autoimmune responses
Cell & Bioscience (2023)
-
The impact of long-term aspirin use on the patients undergoing shoulder arthroplasty
Journal of Orthopaedic Surgery and Research (2023)