Abstract
Diversity is the basis of fitness selection. Although the genome of an individual is considered to be largely stable, there is theoretical and experimental evidence — both in model organisms and in humans — that genetic mosaicism is the rule rather than the exception. The continuous generation of cell variants, their interactions and selective pressures lead to life-long tissue dynamics. Individuals may thus enjoy 'clonal health', defined as a clonal composition that supports healthy morphology and physiology, or suffer from clonal configurations that promote disease, such as cancer. The contribution of mosaicism to these processes starts during embryonic development. In this Opinion article, we argue that the road to cancer might begin during these early stages.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Youssoufian, H. & Pyeritz, R. E. Mechanisms and consequences of somatic mosaicism in humans. Nat. Rev. Genet. 3, 748–758 (2002).
Alexandrov, L. B. et al. Signatures of mutational processes in human cancer. Nature 500, 415–421 (2013).
Fearon, E. R. & Vogelstein, B. A genetic model for colorectal tumorigenesis. Cell 61, 759–767 (1990).
Nik-Zainal, S. et al. The life history of 21 breast cancers. Cell 149, 994–1007 (2012).
Behjati, S. et al. Genome sequencing of normal cells reveals developmental lineages and mutational processes. Nature 513, 422–425 (2014).
Nowell, P. C. The clonal evolution of tumor cell populations. Science 194, 23–28 (1976).
Dalerba, P., Cho, R. W. & Clarke, M. F. Cancer stem cells: models and concepts. Annu. Rev. Med. 58, 267–284 (2007).
Dick, J. E. Stem cell concepts renew cancer research. Blood 112, 4793–4807 (2008).
Frumkin, D., Wasserstrom, A., Kaplan, S., Feige, U. & Shapiro, E. Genomic variability within an organism exposes its cell lineage tree. PLoS Comput. Biol. 1, e50 (2005).
Lynch, M. Rate, molecular spectrum, and consequences of human mutation. Proc. Natl Acad. Sci. USA 107, 961–968 (2010).
McCulloch, S. D. & Kunkel, T. A. The fidelity of DNA synthesis by eukaryotic replicative and translesion synthesis polymerases. Cell Res. 18, 148–161 (2008).
Bianconi, E. et al. An estimation of the number of cells in the human body. Ann. Hum. Biol. 40, 463–471 (2013).
Poduri, A., Evrony, G. D., Cai, X. & Walsh, C. A. Somatic mutation, genomic variation, and neurological disease. Science 341, 1237758 (2013).
Doniger, S. W. et al. A catalog of neutral and deleterious polymorphism in yeast. PLoS Genet. 4, e1000183 (2008).
Leslie, R., O'Donnell, C. J. & Johnson, A. D. GRASP: analysis of genotype-phenotype results from 1390 genome-wide association studies and corresponding open access database. Bioinformatics 30, i185–i194 (2014).
Martin, D. I., Ward, R. & Suter, C. M. Germline epimutation: a basis for epigenetic disease in humans. Ann. NY Acad. Sci. 1054, 68–77 (2005).
Shlien, A. et al. Combined hereditary and somatic mutations of replication error repair genes result in rapid onset of ultra-hypermutated cancers. Nat. Genet. 47, 257–262 (2015).
Di Noia, J. M. & Neuberger, M. S. Molecular mechanisms of antibody somatic hypermutation. Annu. Rev. Biochem. 76, 1–22 (2007).
Baillie, J. K. et al. Somatic retrotransposition alters the genetic landscape of the human brain. Nature 479, 534–537 (2011).
Choate, K. A. et al. Mitotic recombination in patients with ichthyosis causes reversion of dominant mutations in KRT10. Science 330, 94–97 (2010).
Kiritsi, D. et al. Mechanisms of natural gene therapy in dystrophic epidermolysis bullosa. J. Invest. Dermatol. 134, 2097–2104 (2014).
Hirschhorn, R. et al. Spontaneous in vivo reversion to normal of an inherited mutation in a patient with adenosine deaminase deficiency. Nat. Genet. 13, 290–295 (1996).
McDermott, D. H. et al. Chromothriptic cure of WHIM syndrome. Cell 160, 686–699 (2015).
Lo Ten Foe, J. R. et al. Somatic mosaicism in Fanconi anemia: molecular basis and clinical significance. Eur. J. Hum. Genet. 5, 137–148 (1997).
Waisfisz, Q. et al. Spontaneous functional correction of homozygous Fanconi anaemia alleles reveals novel mechanistic basis for reverse mosaicism. Nat. Genet. 22, 379–383 (1999).
Lu, Q. L. et al. Massive idiosyncratic exon skipping corrects the nonsense mutation in dystrophic mouse muscle and produces functional revertant fibers by clonal expansion. J. Cell Biol. 148, 985–996 (2000).
Maley, C. C. et al. Genetic clonal diversity predicts progression to esophageal adenocarcinoma. Nat. Genet. 38, 468–473 (2006).
Park, S. Y., Gonen, M., Kim, H. J., Michor, F. & Polyak, K. Cellular and genetic diversity in the progression of in situ human breast carcinomas to an invasive phenotype. J. Clin. Invest. 120, 636–644 (2010).
Campbell, I. M., Shaw, C. A., Stankiewicz, P. & Lupski, J. R. Somatic mosaicism: implications for disease and transmission genetics. Trends Genet. 31, 382–392 (2015).
Chen, H., Lin, F., Xing, K. & He, X. The reverse evolution from multicellularity to unicellularity during carcinogenesis. Nat. Commun. 6, 6367 (2015).
Lodato, M. A. et al. Somatic mutation in single human neurons tracks developmental and transcriptional history. Science 350, 94–98 (2015).
Martincorena, I. et al. Tumor evolution. High burden and pervasive positive selection of somatic mutations in normal human skin. Science 348, 880–886 (2015).
Iannello, A. & Raulet, D. H. Immune surveillance of unhealthy cells by natural killer cells. Cold Spring Harb. Symp. Quant. Biol. 78, 249–257 (2013).
Pastor-Pareja, J. C. & Xu, T. Dissecting social cell biology and tumors using Drosophila genetics. Annu. Rev. Genet. 47, 51–74 (2013).
Reizel, Y. et al. Colon stem cell and crypt dynamics exposed by cell lineage reconstruction. PLoS Genet. 7, e1002192 (2011).
Snippert, H. J. et al. Intestinal crypt homeostasis results from neutral competition between symmetrically dividing Lgr5 stem cells. Cell 143, 134–144 (2010).
Alcolea, M. P. & Jones, P. H. Lineage analysis of epidermal stem cells. Cold Spring Harb. Perspect Med. 4, a015206 (2014).
Weissman, I. L., Warnke, R., Butcher, E. C., Rouse, R. & Levy, R. The lymphoid system. Its normal architecture and the potential for understanding the system through the study of lymphoproliferative diseases. Hum. Pathol. 9, 25–45 (1978).
Shapiro, E., Biezuner, T. & Linnarsson, S. Single-cell sequencing-based technologies will revolutionize whole-organism science. Nat. Rev. Genet. 14, 618–630 (2013).
Padron-Barthe, L. et al. Clonal analysis identifies hemogenic endothelium as the source of the blood-endothelial common lineage in the mouse embryo. Blood 124, 2523–2532 (2014).
Kinder, S. J. et al. The orderly allocation of mesodermal cells to the extraembryonic structures and the anteroposterior axis during gastrulation of the mouse embryo. Development 126, 4691–4701 (1999).
Burrell, R. A., McGranahan, N., Bartek, J. & Swanton, C. The causes and consequences of genetic heterogeneity in cancer evolution. Nature 501, 338–345 (2013).
Moreno, E. & Rhiner, C. Darwin's multicellularity: from neurotrophic theories and cell competition to fitness fingerprints. Curr. Opin. Cell Biol. 31, 16–22 (2014).
Fujita, Y. Interface between normal and transformed epithelial cells: a road to a novel type of cancer prevention and treatment. Cancer Sci. 102, 1749–1755 (2011).
Kwon, M. C. et al. Paracrine signaling between tumor subclones of mouse SCLC: a critical role of ETS transcription factor Pea3 in facilitating metastasis. Genes Dev. 29, 1587–1592 (2015).
Martins, V. C. et al. Cell competition is a tumour suppressor mechanism in the thymus. Nature 509, 465–470 (2014).
Goetz, J. G. et al. Biomechanical remodeling of the microenvironment by stromal caveolin-1 favors tumor invasion and metastasis. Cell 146, 148–163 (2011).
Biesecker, L. G. & Spinner, N. B. A genomic view of mosaicism and human disease. Nat. Rev. Genet. 14, 307–320 (2013).
Ford, A. M. et al. In utero rearrangements in the trithorax-related oncogene in infant leukaemias. Nature 363, 358–360 (1993).
Wiemels, J. L. et al. Prenatal origin of acute lymphoblastic leukaemia in children. Lancet 354, 1499–1503 (1999).
Teuffel, O. et al. Prenatal origin of separate evolution of leukemia in identical twins. Leukemia 18, 1624–1629 (2004).
Greaves, M. Darwin and evolutionary tales in leukemia. The Ham–Wasserman Lecture. Hematology Am. Soc. Hematol. Educ. Program 2009, 3–12 (2009).
McHale, C. M. et al. Prenatal origin of TEL–AML1-positive acute lymphoblastic leukemia in children born in California. Genes Chromosomes Cancer 37, 36–43 (2003).
Mori, H. et al. Chromosome translocations and covert leukemic clones are generated during normal fetal development. Proc. Natl Acad. Sci. USA 99, 8242–8247 (2002).
Romana, S. P. et al. The t(12;21) of acute lymphoblastic leukemia results in a tel-AML1 gene fusion. Blood 85, 3662–3670 (1995).
Shurtleff, S. A. et al. TEL/AML1 fusion resulting from a cryptic t(12;21) is the most common genetic lesion in pediatric ALL and defines a subgroup of patients with an excellent prognosis. Leukemia. 9, 1985–1989 (1995).
Borkhardt, A. et al. Incidence and clinical relevance of TEL/AML1 fusion genes in children with acute lymphoblastic leukemia enrolled in the German and Italian multicenter therapy trials. Blood 90, 571–577 (1997).
Hong, D. et al. Initiating and cancer-propagating cells in TEL-AML1-associated childhood leukemia. Science 319, 336–339 (2008).
Tsuzuki, S. & Seto, M. TEL (ETV6)-AML1 (RUNX1) initiates self-renewing fetal pro-B cells in association with a transcriptional program shared with embryonic stem cells in mice. Stem Cells 31, 236–247 (2013).
Eguchi-Ishimae, M. et al. Breakage and fusion of the TEL (ETV6) gene in immature B lymphocytes induced by apoptogenic signals. Blood 97, 737–743 (2001).
Marshall, G. M. et al. The prenatal origins of cancer. Nat. Rev. Cancer 14, 277–289 (2014).
Hotfilder, M. et al. Immature CD34+CD19– progenitor/stem cells in TEL/AML1-positive acute lymphoblastic leukemia are genetically and functionally normal. Blood 100, 640–646 (2002).
Greaves, M. F. & Wiemels, J. Origins of chromosome translocations in childhood leukaemia. Nat. Rev. Cancer 3, 639–649 (2003).
Gale, K. B. et al. Backtracking leukemia to birth: identification of clonotypic gene fusion sequences in neonatal blood spots. Proc. Natl Acad. Sci. USA 94, 13950–13954 (1997).
Cazzaniga, G. et al. Developmental origins and impact of BCR-ABL1 fusion and IKZF1 deletions in monozygotic twins with Ph+ acute lymphoblastic leukemia. Blood 118, 5559–5564 (2011).
Doisaki, S. et al. Somatic mosaicism for oncogenic NRAS mutations in juvenile myelomonocytic leukemia. Blood 120, 1485–1488 (2012).
Happle, R. & Rogers, M. Epidermal nevi. Adv. Dermatol. 18, 175–201 (2002).
Happle, R. Lethal genes surviving by mosaicism: a possible explanation for sporadic birth defects involving the skin. J. Am. Acad. Dermatol. 16, 899–906 (1987).
Hafner, C. et al. Mosaicism of activating FGFR3 mutations in human skin causes epidermal nevi. J. Clin. Invest. 116, 2201–2207 (2006).
Hafner, C. et al. Oncogenic PIK3CA mutations occur in epidermal nevi and seborrheic keratoses with a characteristic mutation pattern. Proc. Natl Acad. Sci. USA 104, 13450–13454 (2007).
Hafner, C. et al. Keratinocytic epidermal nevi are associated with mosaic RAS mutations. J. Med. Genet. 49, 249–253 (2012).
Bourdeaut, F. et al. Mosaicism for oncogenic G12D KRAS mutation associated with epidermal nevus, polycystic kidneys and rhabdomyosarcoma. J. Med. Genet. 47, 859–862 (2010).
Hafner, C., Toll, A. & Real, F. X. HRAS mutation mosaicism causing urothelial cancer and epidermal nevus. N. Engl. J. Med. 365, 1940–1942 (2011).
Toll, A. & Real, F. X. Somatic oncogenic mutations, benign skin lesions and cancer progression: where to look next? Cell Cycle 7, 2674–2681 (2008).
Groesser, L. et al. Postzygotic HRAS and KRAS mutations cause nevus sebaceous and Schimmelpenning syndrome. Nat. Genet. 44, 783–787 (2012).
Moody, M. N., Landau, J. M. & Goldberg, L. H. Nevus sebaceous revisited. Pediatr. Dermatol. 29, 15–23 (2012).
Groesser, L. et al. Phacomatosis pigmentokeratotica is caused by a postzygotic HRAS mutation in a multipotent progenitor cell. J. Invest. Dermatol. 133, 1998–2003 (2013).
Benjamin, L. T. Birthmarks of medical significance in the neonate. Semin. Perinatol. 37, 16–19 (2013).
Gerami, P. & Paller, A. S. Making a mountain out of a molehill: NRAS, mosaicism, and large congenital nevi. J. Invest. Dermatol. 133, 2127–2130 (2013).
Ichii-Nakato, N. et al. High frequency of BRAFV600E mutation in acquired nevi and small congenital nevi, but low frequency of mutation in medium-sized congenital nevi. J. Invest. Dermatol. 126, 2111–2118 (2006).
Kinsler, V. A. et al. Multiple congenital melanocytic nevi and neurocutaneous melanosis are caused by postzygotic mutations in codon 61 of NRAS. J. Invest. Dermatol. 133, 2229–2236 (2013).
Gripp, K. W., Stabley, D. L., Nicholson, L., Hoffman, J. D. & Sol-Church, K. Somatic mosaicism for an HRAS mutation causes Costello syndrome. Am. J. Med. Genet. A 140, 2163–2169 (2006).
Lindhurst, M. J. et al. A mosaic activating mutation in AKT1 associated with the Proteus syndrome. N. Engl. J. Med. 365, 611–619 (2011).
Kurek, K. C. et al. Somatic mosaic activating mutations in PIK3CA cause CLOVES syndrome. Am. J. Hum. Genet. 90, 1108–1115 (2012).
Shirley, M. D. et al. Sturge–Weber syndrome and port-wine stains caused by somatic mutation in GNAQ. N. Engl. J. Med. 368, 1971–1979 (2013).
Colman, S. D., Rasmussen, S. A., Ho, V. T., Abernathy, C. R. & Wallace, M. R. Somatic mosaicism in a patient with neurofibromatosis type 1. Am. J. Hum. Genet. 58, 484–490 (1996).
Messiaen, L. et al. Mosaic type-1 NF1 microdeletions as a cause of both generalized and segmental neurofibromatosis type-1 (NF1). Hum. Mutat. 32, 213–219 (2011).
Trofatter, J. A. et al. A novel moesin-, ezrin-, radixin-like gene is a candidate for the neurofibromatosis 2 tumor suppressor. Cell 72, 791–800 (1993).
Baser, M. E. et al. Genotype–phenotype correlations for nervous system tumors in neurofibromatosis 2: a population-based study. Am. J. Hum. Genet. 75, 231–239 (2004).
Goutagny, S. & Kalamarides, M. Meningiomas and neurofibromatosis. J. Neurooncol. 99, 341–347 (2010).
Amary, M. F. et al. Ollier disease and Maffucci syndrome are caused by somatic mosaic mutations of IDH1 and IDH2. Nat. Genet. 43, 1262–1265 (2011).
Pansuriya, T. C. et al. Somatic mosaic IDH1 and IDH2 mutations are associated with enchondroma and spindle cell hemangioma in Ollier disease and Maffucci syndrome. Nat. Genet. 43, 1256–1261 (2011).
Dommering, C. J. et al. RB1 mutation spectrum in a comprehensive nationwide cohort of retinoblastoma patients. J. Med. Genet. 51, 366–374 (2014).
Amitrano, S. et al. Next generation sequencing in sporadic retinoblastoma patients reveals somatic mosaicism. Eur. J. Hum. Genet. 23, 1523–1530 (2015).
Walsh, T. et al. Mutations in 12 genes for inherited ovarian, fallopian tube, and peritoneal carcinoma identified by massively parallel sequencing. Proc. Natl Acad. Sci. USA 108, 18032–18037 (2011).
Behjati, S. et al. A pathogenic mosaic TP53 mutation in two germ layers detected by next generation sequencing. PLoS ONE 9, e96531 (2014).
Hes, F. J. et al. Somatic APC mosaicism: an underestimated cause of polyposis coli. Gut 57, 71–76 (2008).
Macrae, F., du Sart, D. & Nasioulas, S. Familial adenomatous polyposis. Best Pract. Res. Clin. Gastroenterol. 23, 197–207 (2009).
Necker, J., Kovac, M., Attenhofer, M., Reichlin, B. & Heinimann, K. Detection of APC germ line mosaicism in patients with de novo familial adenomatous polyposis: a plea for the protein truncation test. J. Med. Genet. 48, 526–529 (2011).
Friedman, E. et al. Low-level constitutional mosaicism of a de novo BRCA1 gene mutation. Br. J. Cancer. 112, 765–768 (2015).
Ruark, E. et al. Mosaic PPM1D mutations are associated with predisposition to breast and ovarian cancer. Nature 493, 406–410 (2013).
Akbari, M. R. et al. PPM1D mutations in circulating white blood cells and the risk for ovarian cancer. J. Natl Cancer Inst. 106, djt323 (2014).
Buffet, A. et al. Mosaicism in HIF2A-related polycythemia-paraganglioma syndrome. J. Clin. Endocrinol. Metab. 99, E369–E373 (2014).
Rodriguez-Santiago, B. et al. Mosaic uniparental disomies and aneuploidies as large structural variants of the human genome. Am. J. Hum. Genet. 87, 129–138 (2010).
Tomasetti, C. & Vogelstein, B. Cancer etiology. Variation in cancer risk among tissues can be explained by the number of stem cell divisions. Science 347, 78–81 (2015).
Rozhok, A. I., Wahl, G. M. & DeGregori, J. A critical examination of the “bad luck” explanation of cancer risk. Cancer Prev. Res. (Phila.) 8, 762–764 (2015).
Weiss, L. M., Warnke, R. A., Sklar, J. & Cleary, M. L. Molecular analysis of the t(14;18) chromosomal translocation in malignant lymphomas. N. Engl. J. Med. 317, 1185–1189 (1987).
Zelenetz, A. D. et al. Enhanced detection of the t(14;18) translocation in malignant lymphoma using pulsed-field gel electrophoresis. Blood 78, 1552–1560 (1991).
McDonnell, T. J. et al. bcl-2-Immunoglobulin transgenic mice demonstrate extended B cell survival and follicular lymphoproliferation. Cell 57, 79–88 (1989).
Egle, A., Harris, A. W., Bath, M. L., O'Reilly, L. & Cory, S. VavP-Bcl2 transgenic mice develop follicular lymphoma preceded by germinal center hyperplasia. Blood 103, 2276–2283 (2004).
Roulland, S. et al. Long-term clonal persistence and evolution of t(14;18)-bearing B cells in healthy individuals. Leukemia 20, 158–162 (2006).
Roulland, S. et al. t(14;18) translocation: a predictive blood biomarker for follicular lymphoma. J. Clin. Oncol. 32, 1347–1355 (2014).
Kishimoto, W. & Nishikori, M. Molecular pathogenesis of follicular lymphoma. J. Clin. Exp. Hematop. 54, 23–30 (2014).
Forsberg, L. A. et al. Age-related somatic structural changes in the nuclear genome of human blood cells. Am. J. Hum. Genet. 90, 217–228 (2012).
Jacobs, K. B. et al. Detectable clonal mosaicism and its relationship to aging and cancer. Nat. Genet. 44, 651–658 (2012).
Laurie, C. C. et al. Detectable clonal mosaicism from birth to old age and its relationship to cancer. Nat. Genet. 44, 642–650 (2012).
Machiela, M. J. et al. Characterization of large structural genetic mosaicism in human autosomes. Am. J. Hum. Genet. 96, 487–497 (2015).
Dumanski, J. P. & Piotrowski, A. Structural genetic variation in the context of somatic mosaicism. Methods Mol. Biol. 838, 249–272 (2012).
Bonnefond, A. et al. Association between large detectable clonal mosaicism and type 2 diabetes with vascular complications. Nat. Genet. 45, 1040–1043 (2013).
McKerrell, T. et al. Leukemia-associated somatic mutations drive distinct patterns of age-related clonal hemopoiesis. Cell Rep. 10, 1239–1245 (2015).
Schick, U. M. et al. Confirmation of the reported association of clonal chromosomal mosaicism with an increased risk of incident hematologic cancer. PLoS ONE 8, e59823 (2013).
Genovese, G., Jaiswal, S., Ebert, B. L. & McCarroll, S. A. Clonal hematopoiesis and blood-cancer risk. N. Engl. J. Med. 372, 1071–1072 (2015).
Jaiswal, S. et al. Age-related clonal hematopoiesis associated with adverse outcomes. N. Engl. J. Med. 371, 2488–2498 (2014).
Ortmann, C. A. et al. Effect of mutation order on myeloproliferative neoplasms. N. Engl. J. Med. 372, 601–612 (2015).
McKerrell, T. & Vassiliou, G. S. Aging as a driver of leukemogenesis. Sci. Transl Med. 7, 306fs38 (2015).
Hanks, S. et al. Constitutional aneuploidy and cancer predisposition caused by biallelic mutations in BUB1B. Nat. Genet. 36, 1159–1161 (2004).
Snape, K. et al. Mutations in CEP57 cause mosaic variegated aneuploidy syndrome. Nat. Genet. 43, 527–529 (2011).
Forsberg, L. A. et al. Mosaic loss of chromosome Y in peripheral blood is associated with shorter survival and higher risk of cancer. Nat. Genet. 46, 624–628 (2014).
Dumanski, J. P. et al. Mutagenesis. Smoking is associated with mosaic loss of chromosome Y. Science 347, 81–83 (2015).
Hafner, C. et al. Multiple oncogenic mutations and clonal relationship in spatially distinct benign human epidermal tumors. Proc. Natl Acad. Sci. USA 107, 20780–20785 (2010).
Slaughter, D. P., Southwick, H. W. & Smejkal, W. Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer 6, 963–968 (1953).
Simple, M., Suresh, A., Das, D. & Kuriakose, M. A. Cancer stem cells and field cancerization of oral squamous cell carcinoma. Oral Oncol. 51, 643–651 (2015).
Mohan, M. & Jagannathan, N. Oral field cancerization: an update on current concepts. Oncol. Rev. 8, 244 (2014).
Torezan, L. A. & Festa-Neto, C. Cutaneous field cancerization: clinical, histopathological and therapeutic aspects. An. Bras. Dermatol. 88, 775–786 (2013).
Zeki, S. S., McDonald, S. A. & Graham, T. A. Field cancerization in Barrett's esophagus. Discov. Med. 12, 371–379 (2011).
Rivenbark, A. G. & Coleman, W. B. Field cancerization in mammary carcinogenesis — implications for prevention and treatment of breast cancer. Exp. Mol. Pathol. 93, 391–398 (2012).
Forsberg, L. A. et al. Signatures of post-zygotic structural genetic aberrations in the cells of histologically normal breast tissue that can predispose to sporadic breast cancer. Genome Res. 25, 1521–1535 (2015).
Galandiuk, S. et al. Field cancerization in the intestinal epithelium of patients with Crohn's ileocolitis. Gastroenterology 142, 855–864.e8 (2012).
Cheng, L. et al. The origins of urothelial carcinoma. Expert Rev. Anticancer Ther. 10, 865–880 (2010).
Weaver, J. M. et al. Ordering of mutations in preinvasive disease stages of esophageal carcinogenesis. Nat. Genet. 46, 837–843 (2014).
Nakazawa, H. et al. UV and skin cancer: specific p53 gene mutation in normal skin as a biologically relevant exposure measurement. Proc. Natl Acad. Sci. USA 91, 360–364 (1994).
Ziegler, A. et al. Sunburn and p53 in the onset of skin cancer. Nature 372, 773–776 (1994).
Goriely, A. et al. Activating mutations in FGFR3 and HRAS reveal a shared genetic origin for congenital disorders and testicular tumors. Nat. Genet. 41, 1247–1252 (2009).
Maher, G. J., Goriely, A. & Wilkie, A. O. Cellular evidence for selfish spermatogonial selection in aged human testes. Andrology 2, 304–314 (2014).
Hu, B. et al. Multifocal epithelial tumors and field cancerization from loss of mesenchymal CSL signaling. Cell 149, 1207–1220 (2012).
Yates, L. R. et al. Subclonal diversification of primary breast cancer revealed by multiregion sequencing. Nat. Med. 21, 751–759 (2015).
Lander, E. S. et al. Initial sequencing and analysis of the human genome. Nature 409, 860–921 (2001).
Brouha, B. et al. Hot L1s account for the bulk of retrotransposition in the human population. Proc. Natl Acad. Sci. USA 100, 5280–5285 (2003).
Kano, H. et al. L1 retrotransposition occurs mainly in embryogenesis and creates somatic mosaicism. Genes Dev. 23, 1303–1312 (2009).
Nagaoka, S. I., Hassold, T. J. & Hunt, P. A. Human aneuploidy: mechanisms and new insights into an age-old problem. Nat. Rev. Genet. 13, 493–504 (2012).
Ballif, B. C. et al. Detection of low-level mosaicism by array CGH in routine diagnostic specimens. Am. J. Med. Genet. A 140, 2757–2767 (2006).
Bruder, C. E. et al. Phenotypically concordant and discordant monozygotic twins display different DNA copy-number-variation profiles. Am. J. Hum. Genet. 82, 763–771 (2008).
Piotrowski, A. et al. Somatic mosaicism for copy number variation in differentiated human tissues. Hum. Mutat. 29, 1118–1124 (2008).
Colnaghi, R., Carpenter, G., Volker, M. & O'Driscoll, M. The consequences of structural genomic alterations in humans: genomic disorders, genomic instability and cancer. Semin. Cell Dev. Biol. 22, 875–885 (2011).
Liu, P., Carvalho, C. M., Hastings, P. J. & Lupski, J. R. Mechanisms for recurrent and complex human genomic rearrangements. Curr. Opin. Genet. Dev. 22, 211–220 (2012).
Lee, J. A., Carvalho, C. M. & Lupski, J. R. A DNA replication mechanism for generating nonrecurrent rearrangements associated with genomic disorders. Cell 131, 1235–1247 (2007).
Hastings, P. J., Ira, G. & Lupski, J. R. A microhomology-mediated break-induced replication model for the origin of human copy number variation. PLoS Genet. 5, e1000327 (2009).
Stephens, P. J. et al. Massive genomic rearrangement acquired in a single catastrophic event during cancer development. Cell 144, 27–40 (2011).
Maher, C. A. & Wilson, R. K. Chromothripsis and human disease: piecing together the shattering process. Cell 148, 29–32 (2012).
Tuna, M., Knuutila, S. & Mills, G. B. Uniparental disomy in cancer. Trends Mol. Med. 15, 120–128 (2009).
Cohen, A. S., Wilson, S. L., Trinh, J. & Ye, X. C. Detecting somatic mosaicism: considerations and clinical implications. Clin. Genet. 87, 554–562 (2015).
Jonkman, M. F. & Pasmooij, A. M. Realm of revertant mosaicism expanding. J. Invest. Dermatol. 132, 514–516 (2012).
Soriano, P. Generalized lacZ expression with the ROSA26 Cre reporter strain. Nat. Genet. 21, 70–71 (1999).
Lao, Z., Raju, G. P., Bai, C. B. & Joyner, A. L. MASTR: a technique for mosaic mutant analysis with spatial and temporal control of recombination using conditional floxed alleles in mice. Cell Rep. 2, 386–396 (2012).
Schonhuber, N. et al. A next-generation dual-recombinase system for time- and host-specific targeting of pancreatic cancer. Nat. Med. 20, 1340–1347 (2014).
Guerra, C. et al. Tumor induction by an endogenous K-ras oncogene is highly dependent on cellular context. Cancer Cell 4, 111–120 (2003).
Guerra, C. et al. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell 11, 291–302 (2007).
Shibata, H. et al. Rapid colorectal adenoma formation initiated by conditional targeting of the Apc gene. Science 278, 120–123 (1997).
Barker, N. et al. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature 457, 608–611 (2009).
Schepers, A. G. et al. Lineage tracing reveals Lgr5+ stem cell activity in mouse intestinal adenomas. Science 337, 730–735 (2012).
Claveria, C., Giovinazzo, G., Sierra, R. & Torres, M. Myc-driven endogenous cell competition in the early mammalian embryo. Nature 500, 39–44 (2013).
Villa del Campo, C., Claveria, C., Sierra, R. & Torres, M. Cell competition promotes phenotypically silent cardiomyocyte replacement in the mammalian heart. Cell Rep. 8, 1741–1751 (2014).
Morata, G. & Ripoll, P. Minutes: mutants of Drosophila autonomously affecting cell division rate. Dev. Biol. 42, 211–221 (1975).
Moreno, E., Basler, K. & Morata, G. Cells compete for decapentaplegic survival factor to prevent apoptosis in Drosophila wing development. Nature 416, 755–759 (2002).
Amoyel, M. & Bach, E. A. Cell competition: how to eliminate your neighbours. Development 141, 988–1000 (2014).
Amoyel, M. & Bach, E. A. Functions of the Drosophila JAK-STAT pathway: lessons from stem cells. JAKSTAT 1, 176–183 (2012).
Moreno, E. Is cell competition relevant to cancer? Nat. Rev. Cancer 8, 141–147 (2008).
Hogan, C. et al. Characterization of the interface between normal and transformed epithelial cells. Nat. Cell Biol. 11, 460–467 (2009).
Menendez, J., Perez-Garijo, A., Calleja, M. & Morata, G. A tumor-suppressing mechanism in Drosophila involving cell competition and the Hippo pathway. Proc. Natl Acad. Sci. USA 107, 14651–14656 (2010).
Ballesteros-Arias, L., Saavedra, V. & Morata, G. Cell competition may function either as tumour-suppressing or as tumour-stimulating factor in Drosophila. Oncogene 33, 4377–4384 (2013).
Wu, M., Pastor-Pareja, J. C. & Xu, T. Interaction between RasV12 and scribbled clones induces tumour growth and invasion. Nature 463, 545–548 (2010).
Fan, Y. & Bergmann, A. Distinct mechanisms of apoptosis-induced compensatory proliferation in proliferating and differentiating tissues in the Drosophila eye. Dev. Cell 14, 399–410 (2008).
Perez-Garijo, A., Martin, F. A., Struhl, G. & Morata, G. Dpp signaling and the induction of neoplastic tumors by caspase-inhibited apoptotic cells in Drosophila. Proc. Natl Acad. Sci. USA 102, 17664–17669 (2005).
Hariharan, I. K. & Bilder, D. Regulation of imaginal disc growth by tumor-suppressor genes in Drosophila. Annu. Rev. Genet. 40, 335–361 (2006).
Snuderl, M. et al. Mosaic amplification of multiple receptor tyrosine kinase genes in glioblastoma. Cancer Cell 20, 810–817 (2011).
Szerlip, N. J. et al. Intratumoral heterogeneity of receptor tyrosine kinases EGFR and PDGFRA amplification in glioblastoma defines subpopulations with distinct growth factor response. Proc. Natl Acad. Sci. USA 109, 3041–3046 (2012).
Luks, V. L. et al. Lymphatic and other vascular malformative/overgrowth disorders are caused by somatic mutations in PIK3CA. J. Pediatr. 166, 1048–1054 (2015).
Salo-Mullen, E. E. et al. Mosaic partial deletion of the PTEN gene in a patient with Cowden syndrome. Fam. Cancer 13, 459–467 (2014).
Altarescu, G. et al. PGD for germline mosaicism. Reprod. Biomed. Online 25, 390–395 (2012).
Tabareau-Delalande, F. et al. Diagnostic value of investigating GNAS mutations in fibro-osseous lesions: a retrospective study of 91 cases of fibrous dysplasia and 40 other fibro-osseous lesions. Mod. Pathol. 26, 911–921 (2013).
Neveling, K., Endt, D., Hoehn, H. & Schindler, D. Genotype–phenotype correlations in Fanconi anemia. Mutat. Res. 668, 73–91 (2009).
Acknowledgements
The authors thank G. Morata, Y. Fujita, F. Notta, L. Pérez-Jurado, A. Toll and E. Wagner for valuable comments on the manuscript. Work in the authors' laboratories was supported by grants BFU2012-31086 and ISCIII-RD12/0019/0005 (ISCIII) to M.T., SAF2011-29530, ISCIII-RD12-0036-0034 and ONCOBIO Consolíder to F.X.R., and the CEL-DD programme from the Comunidad Autónoma de Madrid (to M.T. and F.X.R.). The Centro Nacional de Investigaciones Cardiovasculares (CNIC) is supported by the Government of Spain through the Ministry of Economy and Competitiveness (MINECO) and the Pro-CNIC Foundation. L.C.F. was the recipient of a Marie Curie training grant (FP7-PEOPLE-2010-IEF, project 274946).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
PowerPoint slides
Glossary
- Age-related clonal haematopoiesis
-
(ARCH). Defined by comparing genetic findings in blood from patients with leukaemia and from healthy individuals. Mutations found in leukaemia could also be demonstrated at low frequency in DNA from leukocytes of individuals without leukaemia. The prevalence of these mutations increases with age and reflects the expansion of founder clones that only infrequently acquire additional genetic alterations to become leukaemic.
- Blaschko's lines
-
Lines that identify pathways of embryonic cell migration. Skin diseases caused by mosaicism are often characterized by a distribution along Blaschko's lines; these lines cannot be seen in the absence of such lesions.
- Cellular heterogeneity
-
Phenotypic cellular diversity that occurs widely in tissues. Genetic mosaicism is only one of the mechanisms contributing to cellular heterogeneity. Epigenetic and cell-specific transcriptional programmes confer cellular identity through different mechanisms. Many other processes (for example, protein glycosylation) can also contribute to cellular heterogeneity.
- Epigenetic mosaicism
-
A form of mosaicism in which a stable epigenetic modification is clonally transmitted. Epigenetic mosaicism can occur in differentiated cells and can contribute to field cancerization and tumour development. Females are naturally epigenetically mosaic: one X chromosome is active and the second is epigenetically silenced. Clonal selection may favour X inactivation disequilibrium in association with ageing.
- Field cancerization
-
The occurrence of genetic alterations in histologically normal or abnormal — but non-neoplastic — tissues that are shared with an adjacent primary tumour. It is also often used to describe seemingly unrelated patches of cells harbouring genetic changes when they are found in non-neoplastic tissue.
- Gonadal mosaicism
-
The occurrence of two or more genetically distinct cell populations present in the gonads; this phenomenon can give rise to de novo mutations in the human population as determined in blood or tissue DNA from the progeny. It comprises conditions that generally behave with an autosomal dominant pattern of inheritance, the parents being either unaffected or with a mild phenotype.
- Guthrie cards
-
Pre-printed cards used to collect blood spots from newborns to allow testing for phenylketonuria, among other metabolic conditions.
- Metazoans
-
Pluricellular animals composed of cells that have functional specialization.
- Neutral drift
-
A shift in the genetic composition of a cell group (or individual) that originates solely from random fluctuations in the clonal contribution of the progenitor pool. The smaller the founder population, the stronger the effects of neutral drifts.
- Selfish clonal expansion
-
Unequal preferential expansion of genetic clones in tissues or whole organisms at the expense of the surrounding cells.
- Somatic mosaicism
-
The occurrence of two or more genetically distinct cell populations exclusively in somatic cells. Mutations that occur after the first division of the zygote are called postzygotic. When it can be demonstrated that they have occurred during embryonic development, because they give rise to a congenital lesion or because they affect tissues from more than one germ layer (an event that is thought not to take place in vivo after gastrulation), they are considered embryonic. When mosaicism is detected only in cells from adult tissues, it is often impossible to determine when the genetic event leading to mosaicism occurred.
Rights and permissions
About this article
Cite this article
Fernández, L., Torres, M. & Real, F. Somatic mosaicism: on the road to cancer. Nat Rev Cancer 16, 43–55 (2016). https://doi.org/10.1038/nrc.2015.1
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrc.2015.1
This article is cited by
-
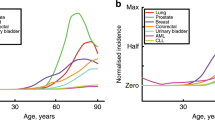
Age influences on the molecular presentation of tumours
Nature Communications (2022)
-
Clinical relevance of postzygotic mosaicism in Cornelia de Lange syndrome and purifying selection of NIPBL variants in blood
Scientific Reports (2021)
-
Effect of naive and cancer-educated fibroblasts on colon cancer cell circadian growth rhythm
Cell Death & Disease (2020)
-
The duality of human oncoproteins: drivers of cancer and congenital disorders
Nature Reviews Cancer (2020)
-
Chronic inflammatory changes and oxidative stress in the background of “pancreatic ductal adenocarcinoma concomitant with intraductal papillary mucinous neoplasm”
Virchows Archiv (2020)