Abstract
Background:
We retrospectively analyzed sunitinib outcome as a function of age in metastatic renal cell carcinoma (mRCC) patients.
Methods:
Data were pooled from 1059 patients in six trials. Kaplan–Meier estimates of progression-free survival (PFS) and overall survival (OS) were compared by log-rank test between patients aged <70 (n=857; 81%) and ⩾70 (n=202; 19%) years.
Results:
In first-line patients, median PFS was comparable in younger and older patients, 9.9 vs 11.0 months, respectively (HR, 0.89; 95% CI: 0.73–1.09; P=0.2629), as was median OS, 23.6 vs 25.6 months (HR, 0.93; 95% CI: 0.74–1.18; P=0.5442). Similarly, in cytokine-refractory patients, median PFS was 8.1 vs 8.4 months (HR, 0.79; 95% CI: 0.49–1.28; P=0.3350), while median OS was 20.2 vs 15.8 months (HR, 1.14; 95% CI: 0.73–1.79; P=0.5657). Some treatment-emergent adverse events were significantly less common in younger vs older patients, including fatigue (60% vs 69%), cough (20% vs 29%), peripheral edema (17% vs 27%), anemia (18% vs 25%), decreased appetite (13% vs 29%), and thrombocytopenia (16% vs 25%; all P<0.05). Hand–foot syndrome was more common in younger patients (32% vs 24%).
Conclusions:
Advanced age should not be a deterrent to sunitinib therapy and elderly patients may achieve additional clinical benefit.
Similar content being viewed by others
Main
The incidence of renal cell carcinoma (RCC) peaks between ages 60 and 70 years (Ljungberg et al, 2010). Patients with RCC ⩾65 years account for ∼50% of those diagnosed in the United States of America and almost 70% of those dying from this tumor (Altekruse et al, 2010). Several studies have suggested that increasing age is an adverse prognostic factor in RCC, with older age associated with higher tumor stage and grade (Denzinger et al, 2007; Verhoest et al, 2007; Karakiewicz et al, 2008; Jung et al, 2009), although others have found that age has little impact on presentation or survival (Doherty et al, 1999; Thompson et al, 2008; Scoll et al, 2009). In general, survival tends to be poorer in older cancer patients (Bouchardy et al, 2003; Petignat et al, 2004; Quaglia et al, 2009; Janssen-Heijnen et al, 2010), reflecting a complex picture of less frequent referral to cancer specialists (Tyldesley et al, 2000; Delva et al, 2011); inadequate treatment (Mor et al, 1985; Earle et al, 2002; Easson et al, 2002; Bouchardy et al, 2003; Houterman et al, 2006; Vulto et al, 2006); and impact of comorbidities (Extermann, 2007), since older patients are at significant risk for multiple comorbidities (e.g., 35% of patients age 65 years or older who are eligible for both US Medicare and Medicaid have ⩾4 comorbidities (Fox and Reichard, 2013)). In addition, aging trends will only exacerbate this issue. In the United States, for example, people age 65 years or older represented 13% of the population in 2007; however, by 2030, this age group is projected to represent 19% of the population (US Department of Health and Human Services, 2009).
Therefore, it is imperative that the elderly are thoroughly assessed for suitability for treatment (National Comprehensive Cancer Network (NCCN), 2011) and that new treatments are adequately evaluated in this major segment of the cancer population. To date, however, elderly patients have been substantially underrepresented in oncology clinical trials (Lewis et al, 2003; Yee et al, 2003; Talarico et al, 2004; Yonemori et al, 2010). Potential reasons include greater frequency of comorbidities (and associated polypharmacy), some degree of baseline end-organ dysfunction, which may lead to failure to meet eligibility criteria or higher potential for renal and hepatic impairment, and concerns about toxicity and poor compliance (Kornblith et al, 2002; Yee et al, 2003; Aapro et al, 2005; Townsley et al, 2005).
Several new treatments have been approved for advanced RCC, and characterizing the safety and efficacy of these treatments in elderly patients is an important goal. One such treatment is sunitinib malate (SUTENT; Pfizer, New York, NY, USA), an orally administered, multitargeted inhibitor of receptors for vascular endothelial growth factor, platelet-derived growth factor, and other tyrosine kinases. Efficacy and safety of sunitinib in the first-line and cytokine-refractory settings have been demonstrated in six key clinical trials, using two different schedules: the approved schedule of 50 mg per day for 4 weeks on treatment followed by 2 weeks off treatment (Schedule 4/2), and a continuous daily dosing (CDD) schedule of 37.5 mg per day (Motzer et al, 2006a, 2006b, 2007, 2009, 2012; Escudier et al, 2009; Barrios et al, 2012). Here, we report findings of a retrospective analysis using a pooled database of patients from these six trials in which we compared the efficacy and safety of sunitinib in patients aged <70 or ⩾70 years.
Materials and methods
Patients
Eligibility criteria included age ⩾18 years, histologically confirmed metastatic RCC, presence of measurable disease by Response Evaluation Criteria in Solid Tumors (RECIST) version 1.0 (Therasse et al, 2000), no known brain metastases, Eastern Cooperative Oncology Group (ECOG) performance status 0 or 1 (or Karnofsky performance status of ⩾70% in one trial (Motzer et al, 2012)), and adequate organ function.
Study design
This retrospective analysis investigated the efficacy and safety of sunitinib as a function of age using pooled data from 1059 patients who received sunitinib in either the first-line or cytokine-refractory metastatic RCC setting in six prospective multinational Pfizer-sponsored clinical trials (Motzer et al, 2006a, 2006b, 2007, 2009, 2012; Escudier et al, 2009; Barrios et al, 2012). Data from 360 patients treated with interferon alpha (IFN-α) in the first-line setting in one of the trials, a randomized phase III study, were also analyzed (Motzer et al, 2007, 2009). Sunitinib was administered orally at a starting dose of 50 mg per day on Schedule 4/2 in repeated 6-week cycles (n=690; 65%), or 37.5 mg per day on the CDD schedule (n=369; 35%). IFN-α was administered by subcutaneous injection thrice weekly on nonconsecutive days at 3 MU per dose in the first week, 6 MU the second week, and 9 MU thereafter. Treatment continued until disease progression, lack of clinical benefit, unacceptable toxicity, or consent withdrawal.
Efficacy endpoints included progression-free survival (PFS) and overall survival (OS). Tumor response and progression were assessed by investigators using RECIST version 1.0 (Therasse et al, 2000), and schedules specified in each trial protocol (initially every 4–6 weeks, increasing to every 8–12 weeks after ∼6 months). Adverse events (AEs) were recorded regularly and graded according to the National Cancer Institute Common Terminology Criteria for AEs (CTCAE), version 3.0 (version 2.0 in one trial (Motzer et al, 2006a)).
Studies were run in accordance with the International Conference on Harmonization Good Clinical Practice guidelines (or Declaration of Helsinki) and applicable local regulatory requirements and laws, and approved by the institutional review boards/independent ethics committees of each participating center (ClinicalTrials.gov: NCT00267748, NCT00137423, NCT00083889, NCT00077974, NCT00054886, NCT00338884).
Statistical methods
Median PFS and OS for direct comparison of sunitinib-treated patients aged <70 and ⩾70 years (including by treatment setting) were estimated by Kaplan–Meier method and compared using log-rank test. This age cutoff was chosen to address the increasing age expectancy in the general population, thus defining a population more representative of the elderly, and was the same one used in a previously reported analysis of elderly sorafenib-treated patients with advanced RCC (Eisen et al, 2008). A comparison of treatment-naïve patients on sunitinib vs IFN-α was performed using log-rank test. All hazard ratios (HRs) were calculated by Cox proportional hazards model. Pearson χ2 test was used to assess differences in AE incidence rates between age groups. Differences in incidence rates of common treatment-emergent AEs (incidence ⩾10%) were also assessed separately for patients in first-line trials only, and for patients who received sunitinib by the two different treatment schedules; P-values were calculated by two-sided Fisher’s exact test.
Results
Baseline characteristics
Of 1059 sunitinib-treated patients, 857 (81%) were <70 years and 202 (19%) were ⩾70 years (Table 1). The median age in the <70 and ⩾70 years age groups was 57 years (range: 24–69) and 73 years (range: 70–87), respectively. Baseline characteristics of the two sunitinib age groups were generally similar, although more patients aged <70 years than ⩾70 years were male (73% vs 59%) and had had a prior nephrectomy (81% vs 71%).
Baseline characteristics were also similar in the two age groups treated with IFN-α (Table 1). Of 360 patients, 299 (83%) were aged <70 with a median of 57 years (range: 38–69) and 61 (17%) were aged ⩾70 years with a median of 74 years (range: 70–85).
Disposition and exposure in sunitinib-treated patients
Sunitinib treatment was administered to 783 first-line patients (74%) and 276 cytokine-refractory patients (26%). Across all trials, the overall proportion of patients remaining on treatment in the younger and older age groups was 12.3% and 8.9%, respectively. The most common reasons for discontinuing treatment included, in patients aged <70 vs ⩾70 years, respectively, disease progression (20% vs 21%), death (1% vs 2%), AE (16% vs 27%), and consent withdrawal (2% vs 5%).
Exposure to sunitinib was comparable in younger and elderly age groups. Patients aged <70 and ⩾70 years were treated for a median of 196 days (range: 2–1037) and 168 days (range: 3–840), respectively, and the median relative (percentage of actual/intended) dose intensity of sunitinib was 97.12% (range: 4.76–130.15%) and 89.72% (range: 7.14–270.24%), respectively. In patients aged <70 vs ⩾70 years, 59% vs 68% had ⩾1 dose interruption and 42% vs 57% had dose reductions.
Efficacy
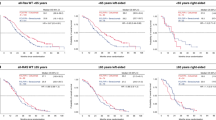
Across the entire pooled sunitinib-treated population, PFS and OS were similar in younger and elderly sunitinib-treated patients. In the first-line treatment setting, for patients aged <70 and ⩾70 years, respectively, median PFS was 9.9 vs 11.0 months with an HR of 0.89 (95% confidence interval (CI): 0.73–1.09; P=0.2629), while median OS was 23.6 vs 25.6 months, with an HR of 0.93 (95% CI: 0.74–1.18; P=0.5442). In the cytokine-refractory treatment setting, for patients aged <70 and ⩾70 years, respectively, median PFS was 8.1 vs 8.4 months with an HR of 0.79 (95% CI: 0.49–1.28; P=0.3350), while median OS was 20.2 vs 15.8 months, with an HR of 1.14 (95% CI: 0.73–1.79; P=0.5657). Sunitinib efficacy was maintained in elderly patients, regardless of treatment setting (Table 2; Figure 1).
Kaplan–Meier estimates of survival in sunitinib-treated patients by age (<70 vs ⩾70 years). (A) Progression-free survival in the first-line setting; (B) overall survival in the first-line setting; (C) progression-free survival in the cytokine-refractory setting; (D) overall survival in the cytokine-refractory setting.
Within the first-line treatment setting, median PFS was significantly greater with sunitinib than with IFN-α in the groups of patients aged <70 and ⩾70 years (P⩽0.0197), and median OS was also improved in each age group, although this difference did not reach significance (Table 3).
Safety in sunitinib-treated patients by age
The incidences of most treatment-emergent AEs were similar in both age groups (Table 4). Some events, however, were significantly more common (P<0.05) in patients aged ⩾70 years compared with those aged <70 years (Table 4), including fatigue, cough, anemia, peripheral edema, thrombocytopenia, decreased weight, decreased appetite, dizziness, hypothyroidism, dehydration, and urinary tract infection. Hand–foot syndrome, hair color changes, and chest pain were all more common in younger patients. A similar profile of age-associated differences in the incidence of common treatment-emergent AEs (i.e., events reported in ⩾10%) was observed when the analysis was limited to patients in first-line treatment trials only (data not shown).
Patients who received sunitinib by the two different treatment schedules (Schedule 4/2 and CDD) were analyzed separately (data not shown). Although, overall, the incidence profile of common treatment-emergent AEs was broadly similar to that observed in the total patient population, there were a few differences. In patients who received sunitinib on Schedule 4/2, the incidences of fatigue, dizziness, dehydration, and hand–foot syndrome were not significantly different between the two age groups; constipation, asthenia, anorexia, and erythema were significantly more common in older patients, and pyrexia and flatulence were significantly more common in younger patients. Among patients who received sunitinib on CDD, the incidences of anemia and hand–foot syndrome were not significantly different between the two age groups, and nausea, hyponatremia, arthralgia, and pruritus were significantly more common in older patients.
Overall, treatment-emergent AEs by highest grade/severity were compared for the two age groups. The profiles were significantly different for patients aged <70 years and ⩾70 years, irrespective of whether data for all trials were considered together or if data from first-line and cytokine-refractory trials were considered separately (P<0.001, P=0.023, and P=0.035, respectively). Overall, treatment-emergent AEs by highest grade in each age group, for all trials (first-line and cytokine-refractory combined) are summarized in Table 5. These data show that a greater proportion of the younger patients had highest severity of grade 1 or 2 and the older patients were more likely to have a highest severity of grade 3. There was no difference in the occurrence of highest grade AEs of grade 4 or 5 between the two age groups, with the majority of grade 5 AEs occurring in treatment-naïve patients regardless of age (aged <70: n=51; aged ⩾70: n=13).
Discussion
This retrospective, pooled analysis found that sunitinib efficacy was comparable in elderly (⩾70 years) and younger (<70 years) patients with metastatic RCC, regardless of treatment setting. Elderly patients treated with IFN-α in a randomized phase III study vs sunitinib in the first-line setting (Motzer et al, 2007, 2009) also derived similar benefit as younger patients randomized to IFN-α; however, the survival benefits of sunitinib over IFN-α in this trial were maintained in both age groups. Our analysis is limited by its exploratory nature, and the fact that the study was not designed to test for statistically significant differences in efficacy or safety between patients aged <70 and ⩾70 years. Although baseline characteristics of older and younger sunitinib-treated patients appeared balanced (apart from gender), risk factor data were missing for 17%; any imbalance in these data may have influenced results. In addition, because these patients were treated in clinical trials, they may represent a more selective patient population that is not adequately reflective of a real-world setting in which elderly patients warrant special consideration given the risk of AEs with targeted therapy. Nonetheless, our findings support observations from an expanded access trial of sunitinib with less restrictive eligibility criteria, in which PFS and OS for elderly patients (1418 patients; 32% of the population), although defined differently (⩾65 years), were comparable with those of the overall population, median age 59 years (range: 19–89; Gore et al, 2009). Correspondingly, although the definition of ‘elderly’ can be arbitrary, our analyses suggest that, regardless of the age cutoff used, there is no apparent difference in outcome with sunitinib.
Although there was no significant difference in PFS or OS between age groups, there was a trend toward improved PFS in older sunitinib-treated patients in the overall population (i.e., both treatment settings combined) with median PFS of 10.9 months compared with 9.0 months in younger patients (HR, 0.85; 95% CI: 0.70–1.02; P=0.0830). A similar trend was reported for elderly patients (⩾70 years) receiving sorafenib (Eisen et al, 2008), raising the possibility that elderly patients with RCC may be more responsive to anti-angiogenic therapy; although, in our analysis, IFN-α-treated elderly patients also seemed to benefit more than younger ones from treatment (median PFS 7.9 vs 5.0 months). These studies, however, contradict a recently reported retrospective analysis of the Surveillance, Epidemiology, and End Results (SEER) registry in which disease-specific survival was inferior in older adults (⩾75 years) with metastatic RCC (Nelson et al, 2013); also, in contrast to younger patients, older patients in the SEER analysis did not experience an improvement in survival in the ‘targeted therapy era’ (2005–2009) relative to the ‘cytokine era’ (1992–2004). Of note, however, this analysis did not report comorbidity data that may have confounded the results; only patients with de novo metastatic disease and thus inherently intermediate- or poor-risk disease were included. In addition, the registry lacked data pertaining to the systemic therapies received; thus, actual practice patterns could not be confirmed. Preclinical studies have shown that there are age-dependent differences in tumor growth, but these patterns are not consistent across tumor types (Pili et al, 1994; Anisimov, 2006; Reed et al, 2007). Also, a recent RCC tumor biopsy study revealed age-related differences in tumor vasculature, in which clear cell RCC tumors from patients aged ⩾65 years had significantly higher microvascular density than those from patients aged <65 years, and markers of angiogenic activity also differed (Meehan et al, 2011). Further work is needed on a larger number of tumor samples, but it is conceivable that the higher microvascular density in older patients results in greater sensitivity to anti-angiogenic treatment or that higher vessel density is inversely associated with tumor aggressiveness (Yildiz et al, 2008).
Our analysis showed that the AE profile was broadly similar in older and younger patients for the total patient population, in first-line patients, and regardless of treatment schedule. Some AEs, such as fatigue, were significantly more common in older patients, and the profile of the highest grade AEs was overall significantly more severe in older patients (younger patients were more likely to have a highest grade AE of grade 1 or 2, and older patients more likely to have a highest grade AE of grade 3), possibly due to more comorbidities in this population. Similar observations were made in a recently reported retrospective analysis of elderly patients with metastatic RCC in which patients ⩾75 years received fewer lines of systemic therapy as compared with other age-based subsets and more frequently discontinued therapies due to toxicity (Pal et al, 2013). However, importantly, the increased incidences of certain AEs in our analysis did not impact on overall efficacy in the elderly population, despite observed trends for increased dosing interruptions, reductions, and treatment discontinuations. Of note, hand–foot syndrome was more common in younger patients, possibly due to relatively higher activity levels, resulting in increased pressure on the hands and feet. While it is difficult to generalize across therapeutic agents, our study adds to a growing number of publications suggesting that older patients can tolerate molecularly targeted agents as well as younger patients (Pal et al, 2011). However, further post-marketing data for the elderly population are needed, in addition to results from clinical trials in which patients may not represent the general population, in order to fully assess response and tolerability in the presence of comorbidities. In addition, there may be potential pharmacokinetic differences in this population, which might explain our findings.
The results reported here demonstrate that the efficacy profile of sunitinib appears comparable in older and younger patients with advanced RCC, with some limited differences in the safety profiles. Therefore, advanced age alone should not be a deterrent to treating with sunitinib in this population, nor should less effective or non recommended treatment options be chosen (National Comprehensive Cancer Network (NCCN), 2011) due to concerns regarding age-related tolerability; and, in fact, elderly patients may achieve additional clinical benefit with sunitinib.
Change history
04 March 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aapro MS, Köhne CH, Cohen HJ, Extermann M (2005) Never too old? Age should not be a barrier to enrollment in cancer clinical trials. Oncologist 10: 198–204.
Altekruse SF, Kosary CL, Krapcho M, Neyman N, Aminou R, Waldron W, Ruhl J, Howlader N, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Cronin K, Chen HS, Feuer EJ, Stinchcomb DG, Edwards BK (eds). (2010) SEER Cancer Statistics Review, 1975-2007. National Cancer Institute: Bethesda, MD http://seer.cancer.gov/csr/1975_2007/ based on November 2009 SEER data submission, posted to the SEER website 2010.
Anisimov VN (2006) Effect of host age on tumor growth rate in rodents. Front Biosci 11: 412–422.
Barrios CH, Hernandez-Barajas D, Brown MP, Lee SH, Fein L, Liu JH, Hariharan S, Martell BA, Yuan J, Bello A, Wang Z, Mundayat R, Rha SY (2012) Phase II trial of continuous once-daily dosing of sunitinib as first-line treatment in patients with metastatic renal cell carcinoma. Cancer 118: 1252–1259.
Bouchardy C, Rapiti E, Fioretta G, Laissue P, Neyroud-Caspar I, Schäfer P, Kurtz J, Sappino AP, Vlastos G (2003) Undertreatment strongly decreases prognosis of breast cancer in elderly women. J Clin Oncol 21: 3580–3587.
Delva F, Marien E, Fonck M, Rainfray M, Demeaux JL, Moreaud P, Soubeyran P, Sasco AJ, Mathoulin-Pélissier S (2011) Factors influencing general practitioners in the referral of elderly cancer patients. BMC Cancer 11: 5.
Denzinger S, Otto W, Burger M, Hammerschmied C, Junker K, Hartmann A, Wieland WF, Walter B (2007) Sporadic renal cell carcinoma in young and elderly patients: are there different clinicopathological features and disease specific survival rates? World J Surg Oncol 5: 16.
Doherty JG, Rüfer A, Bartholomew P, Beaumont DM (1999) The presentation, treatment and outcome of renal cell carcinoma in old age. Age Ageing 28: 359–362.
Earle CC, Neumann PJ, Gelber RD, Weinstein MC, Weeks JC (2002) Impact of referral patterns on the use of chemotherapy for lung cancer. J Clin Oncol 20: 1786–1792.
Easson AM, Cotterchio M, Crosby JA, Sutherland H, Dale D, Aronson M, Holowaty E, Gallinger S (2002) A population-based study of the extent of surgical resection of potentially curable colon cancer. Ann Surg Oncol 9: 380–387.
Eisen T, Oudard S, Szczylik C, Gravis G, Heinzer H, Middleton R, Cihon F, Anderson S, Shah S, Bukowski R, Escudier B on behalf of the TARGET Study Group (2008) Sorafenib for older patients with renal cell carcinoma: subset analysis from a randomized trial. J Natl Cancer Inst 100: 1454–1463.
Escudier B, Roigas J, Gillessen S, Harmenberg U, Srinivas S, Mulder SF, Fountzilas G, Peschel C, Flodgren P, Maneval EC, Chen I, Vogelzang NJ (2009) Phase II study of sunitinib administered in a continuous once-daily dosing regimen in patients with cytokine-refractory metastatic renal cell carcinoma. J Clin Oncol 27: 4068–4075.
Extermann M (2007) Interaction between comorbidity and cancer. Cancer Control 14: 13–22.
Fox MH, Reichard A (2013) Disability, health, and multiple chronic conditions among people eligible for both Medicare and Medicaid, 2005-2010. Prev Chronic Dis 10: E157.
Gore ME, Szczylik C, Porta C, Bracarda S, Bjarnason GA, Oudard S, Hariharan S, Lee SH, Haanen J, Castellano D, Vrdoljak E, Schöffski P, Mainwaring P, Nieto A, Yuan J, Bukowski R (2009) Safety and efficacy of sunitinib for metastatic renal-cell carcinoma: an expanded-access trial. Lancet Oncol 10: 757–763.
Houterman S, Janssen-Heijnen ML, Hendrikx AJ, van den Berg HA, Coebergh JW (2006) Impact of comorbidity on treatment and prognosis of prostate cancer patients: a population-based study. Crit Rev Oncol Hematol 58: 60–67.
Janssen-Heijnen ML, Gondos A, Bray F, Hakulinen T, Brewster DH, Brenner H, Coebergh JW (2010) Clinical relevance of conditional survival of cancer patients in Europe: age-specific analyses of 13 cancers. J Clin Oncol 28: 2520–2528.
Jung EJ, Lee HJ, Kwak C, Ku JH, Moon KC (2009) Young age is independent prognostic factor for cancer-specific survival of low-stage clear cell renal cell carcinoma. Urology 73: 137–141.
Karakiewicz PI, Jeldres C, Suardi N, Hutterer GC, Perrotte P, Capitanio U, Ficarra V, Cindolo L, de La Taille A, Tostain J, Mulders PF, Salomon L, Zigeuner R, Schips L, Chautard D, Valeri A, Lechevallier E, Descots JL, Lang H, Mejean A, Verhoest G, Patard JJ (2008) Age at diagnosis is a determinant factor of renal cell carcinoma-specific survival in patients treated with nephrectomy. Can Urol Assoc J 2: 610–617.
Kornblith AB, Kemeny M, Peterson BL, Wheeler J, Crawford J, Bartlett N, Fleming G, Graziano S, Muss H, Cohen HJ on behalf of the Cancer and Leukemia Group B (2002) Survey of oncologists’ perceptions of barriers to accrual of older patients with breast carcinoma to clinical trials. Cancer 95: 989–996.
Lewis JH, Kilgore ML, Goldman DP, Trimble EL, Kaplan R, Montello MJ, Housman MG, Escarce JJ (2003) Participation of patients 65 years of age or older in cancer clinical trials. J Clin Oncol 21: 1383–1389.
Ljungberg B, Cowan NC, Hanbury DC, Hora M, Kuczyk MA, Merseburger AS, Patard JJ, Mulders PF, Sinescu IC on behalf of the European Association of Urology Guideline Group (2010) EAU guidelines on renal cell carcinoma: the 2010 update. Eur Urol 58: 398–406.
Meehan B, Appu S, St Croix B, Rak-Poznanska K, Klotz L, Rak J (2011) Age-related properties of the tumour vasculature in renal cell carcinoma. BJU Int 107: 416–424.
Mor V, Masterson-Allen S, Goldberg RJ, Cummings FJ, Glicksman AS, Fretwell MD (1985) Relationship between age at diagnosis and treatments received by cancer patients. J Am Geriatr Soc 33: 585–589.
Motzer RJ, Bacik J, Murphy BA, Russo P, Mazumdar M (2002) Interferon-alfa as a comparative treatment for clinical trials of new therapies against advanced renal cell carcinoma. J Clin Oncol 20: 289–296.
Motzer RJ, Hutson TE, Olsen MR, Hudes GR, Burke JM, Edenfield WJ, Wilding G, Agarwal N, Thompson JA, Cella D, Bello A, Korytowsky B, Yuan J, Valota O, Martell B, Hariharan S, Figlin RA (2012) Randomized phase II trial of sunitinib on an intermittent versus continuous dosing schedule as first-line therapy for advanced renal cell carcinoma. J Clin Oncol 30: 1371–1377.
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Oudard S, Negrier S, Szczylik C, Pili R, Bjarnason GA, Garcia-del-Muro X, Sosman JA, Solska E, Wilding G, Thompson JA, Kim ST, Chen I, Huang X, Figlin RA (2009) Overall survival and updated results for sunitinib compared with interferon alfa in patients with metastatic renal cell carcinoma. J Clin Oncol 27: 3584–3590.
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, Oudard S, Negrier S, Szczylik C, Kim ST, Chen I, Bycott PW, Baum CM, Figlin RA (2007) Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med 356: 115–124.
Motzer RJ, Michaelson MD, Redman BG, Hudes GR, Wilding G, Figlin RA, Ginsberg MS, Kim ST, Baum CM, DePrimo SE, Li JZ, Bello CL, Theuer CP, George DJ, Rini BI (2006a) Activity of SU11248, a multitargeted inhibitor of vascular endothelial growth factor receptor and platelet-derived growth factor receptor, in patients with metastatic renal cell carcinoma. J Clin Oncol 24: 16–24.
Motzer RJ, Rini BI, Bukowski RM, Curti BD, George DJ, Hudes GR, Redman BG, Margolin KA, Merchan JR, Wilding G, Ginsberg MS, Bacik J, Kim ST, Baum CM, Michaelson MD (2006b) Sunitinib in patients with metastatic renal cell carcinoma. JAMA 295: 2516–2524.
National Comprehensive Cancer Network (NCCN) (2011) Clinical Practice Guidelines in Oncology: Senior Adult Oncology, Version 2.2011. Available at http://www.nccn.org/professionals/physician_gls/f_guidelines.asp accessed July 11, 2011.
Nelson RA, Vogelzang N, Pal SK (2013) A gap in disease-specific survival between younger and older adults with de novo metastatic renal cell carcinoma: results of a SEER database analysis. Clin Genitourin Cancer 11: 303–310.
Pal SK, Vanderwalde A, Hurria A, Figlin RA (2011) Systemic therapies for metastatic renal cell carcinoma in older adults. Drugs Aging 28: 635–649.
Pal SK, Hsu J, Hsu S, Hu J, Bergerot P, Carmichael C, Saikia J, Liu X, Lau C, Twardowski P, Figlin RA, Yuh BE (2013) Impact of age on treatment trends and clinical outcome in patients with metastatic renal cell carcinoma. J Geriatr Oncol 4: 128–133.
Petignat P, Fioretta G, Verkooijen HM, Vlastos AT, Rapiti E, Bouchardy C, Vlastos G (2004) Poorer survival of elderly patients with ovarian cancer: a population-based study. Surg Oncol 13: 181–186.
Pili R, Guo Y, Chang J, Nakanishi H, Martin GR, Passaniti A (1994) Altered angiogenesis underlying age-dependent changes in tumor growth. J Natl Cancer Inst 86: 1303–1314.
Quaglia A, Tavilla A, Shack L, Brenner H, Janssen-Heijnen M, Allemani C, Colonna M, Grande E, Grosclaude P, Vercelli M on behalf of the EUROCARE Working Group (2009) The cancer survival gap between elderly and middle-aged patients in Europe is widening. Eur J Cancer 45: 1006–1016.
Reed MJ, Karres N, Eyman D, Cruz A, Brekken RA, Plymate S (2007) The effects of aging on tumor growth and angiogenesis are tumor-cell dependent. Int J Cancer 120: 753–760.
Scoll BJ, Wong YN, Egleston BL, Kunkle DA, Saad IR, Uzzo RG (2009) Age, tumor size and relative survival of patients with localized renal cell carcinoma: a surveillance, epidemiology and end results analysis. J Urol 181: 506–511.
Talarico L, Chen G, Pazdur R (2004) Enrollment of elderly patients in clinical trials for cancer drug registration: a 7-year experience by the US Food and Drug Administration. J Clin Oncol 22: 4626–4631.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst 92: 205–216.
Thompson RH, Ordonez MA, Iasonos A, Secin FP, Guillonneau B, Russo P, Touijer K (2008) Renal cell carcinoma in young and old patients: is there a difference? J Urol 180: 1262–1266.
Townsley CA, Selby R, Siu LL (2005) Systematic review of barriers to the recruitment of older patients with cancer onto clinical trials. J Clin Oncol 23: 3112–3124.
Tyldesley S, Zhang-Salomons J, Groome PA, Zhou S, Schulze K, Paszat LF, Mackillop WJ (2000) Association between age and the utilization of radiotherapy in Ontario. Int J Radiat Oncol Biol Phys 47: 469–480.
US Department of Health and Human Services (2009) Administration on Aging. A Profile of Older Americans. Available at http://www.aoa.gov/aoaroot/aging_statistics/profile/2009/ accessed November 21, 2013.
Verhoest G, Veillard D, Guillé F, De La Taille A, Salomon L, Abbou CC, Valéri A, Lechevallier E, Descotes JL, Lang H, Jacqmin D, Tostain J, Cindolo L, Ficarra V, Artibani W, Schips L, Zigeuner R, Mulders PF, Mejean A, Patard JJ (2007) Relationship between age at diagnosis and clinicopathologic features of renal cell carcinoma. Eur Urol 51: 1298–1304.
Vulto AJ, Lemmens VE, Louwman MW, Janssen-Heijnen ML, Poortmans PH, Lybeert ML, Coebergh JW (2006) The influence of age and comorbidity on receiving radiotherapy as part of primary treatment for cancer in South Netherlands, 1995 to 2002. Cancer 106: 2734–2742.
Yee KW, Pater JL, Pho L, Zee B, Siu LL (2003) Enrollment of older patients in cancer treatment trials in Canada: why is age a barrier? J Clin Oncol 21: 1618–1623.
Yildiz E, Ayan S, Goze F, Gokce G, Gultekin EY (2008) Relation of microvessel density with microvascular invasion, metastasis and prognosis in renal cell carcinoma. BJU Int 101: 758–764.
Yonemori K, Hirakawa A, Komiyama N, Kouno T, Ando M, Fujiwara Y, Urano T, Akagawa H, Maruyama H, Toyoshima S (2010) Participation of elderly patients in registration trials for oncology drug applications in Japan. Ann Oncol 21: 2112–2118.
Acknowledgements
We thank participating patients and their families, and the investigators, research nurses, study coordinators, and operations staff. The study was sponsored by Pfizer. Medical writing support was provided by Andy Gannon and Jean Scott at ACUMED (New York, NY, USA) with funding from Pfizer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
RMB received honoraria and consultant fees from Pfizer, Novartis, Genentech, GlaxoSmithKline, and Bristol-Myers Squibb, and consultant fees from Argos and Exelixis. BIR received research funding and consultant fees from Pfizer. MEG received advisory board and speaker bureau fees from Pfizer, Bayer, Roche, Novartis, GlaxoSmithKline, and Aveo/Astellas, and acknowledges NHS funding to the NIHR Biomedical Research Centre. JML received research funding, honoraria, and consultant fees from Pfizer, Novartis, Bristol-Myers Squibb, and GlaxoSmithKline, and acknowledges NHS funding to the NIHR Biomedical Research Centre. BE received advisory fees from Pfizer, GlaxoSmithKline, Novartis, Bayer, and Aveo. XL, KF, and EM are compensated employees of Pfizer and own Pfizer stock. BM is a former employee of Pfizer. RJM received research funding from Pfizer, GlaxoSmithKline, Novartis, and Bristol-Myers Squibb, and consultant fees from Pfizer and Genentech. The remaining authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Hutson, T., Bukowski, R., Rini, B. et al. Efficacy and safety of sunitinib in elderly patients with metastatic renal cell carcinoma. Br J Cancer 110, 1125–1132 (2014). https://doi.org/10.1038/bjc.2013.832
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.832
Keywords
This article is cited by
-
Pharmacotherapeutic Management of Well-Differentiated Neuroendocrine Tumors in Older Patients: Current Status and Potential Therapies
Drugs & Aging (2022)
-
Pazopanib has equivalent anti-tumor effectiveness and lower Total costs than Sunitinib for treating metastatic or advanced renal cell carcinoma: a meta-analysis
BMC Cancer (2019)
-
Evaluation of efficacy and safety of sorafenib in kidney cancer patients aged 75 years and older: a propensity score-matched analysis
British Journal of Cancer (2018)
-
Toxicity of Cancer Therapies in Older Patients
Current Oncology Reports (2018)
-
Nierenzellkarzinom des alten und geriatrischen Patienten
Der Urologe (2017)