Abstract
Diagnostic discrepancy, defined as different admission and discharge diagnoses, could be a potential source of diagnostic error. We evaluated whether acute kidney injury (AKI) in the elderly affected their risk for diagnostic discrepancy. Patients aged ≥60 years from the general medical wards were prospectively enrolled and divided according to AKI status upon admission, using the Kidney Disease Improving Global Outcomes (KDIGO) criteria. We compared their discharge and admission diagnoses and identified patients with a diagnostic discrepancy, using multiple logistic regression analysis to evaluate the relationship between initial AKI and the presence of a diagnostic discrepancy. A total of 188 participants (mean age, 77.9 years) were recruited. Regression analysis showed that initial AKI on admission was associated with a higher risk of diagnostic discrepancy upon discharge (odds ratio [OR] 3.3; p < 0.01). In contrast, higher AKI severity was also associated with an increased risk of diagnostic discrepancy (for KDIGO grade 1, 2, and 3; OR 2.92, 3.91, and 4.32; p = 0.04, 0.03, and 0.02, respectively), suggesting that initial AKI upon admission could be an important risk factor for diagnostic discrepancy. Consequently, reducing geriatric AKI might have the potential to reduce diagnostic discrepancy among these patients.
Similar content being viewed by others
Introduction
The number of elderly patients is increasing worldwide. Healthcare spending in this population is increasing, owing to multimorbidity, functional decline, a higher prevalence of frailty, and increased vulnerability to adverse environment1,2,3. Elderly patients who sustain acute illness, especially infection-related episodes, are more likely to be hospitalised than their younger counterparts; studies have identified a progressive increase in the incidence of hospitalization with older age, irrespective of pathogens4. Elderly patients undergo medical investigation and intervention frequently during their visit to the emergency department and during hospitalizations, leading to the increased utilization of healthcare resources5.
A prompt and accurate diagnosis upon admission is important for all patients, since a correct initial diagnosis facilitates the selection of the appropriate management strategy and thus influences subsequent treatment planning. A mismatch of diagnoses upon admission and discharge can have major clinical implications, as a diagnostic discrepancy might herald a higher incidence of diagnostic error and potentially increase the possibility of implementing unnecessary examinations or interventions6. Large practice-based registries have shown that diagnostic errors are responsible for 7 to 17% of in-hospital adverse events, contributing to increased hospital mortality7,8. Consequently, the identification of diagnostic discrepancy among hospitalised patients can pave the way toward uncovering diagnostic errors and improving the quality of inpatient care.
Currently, there are very few studies addressing factors influencing diagnostic discrepancy among the hospitalised elderly, despite available reports suggesting that increased age might be associated with a higher incidence9,10. We previously found that the elderly diagnosed with acute kidney injury (AKI) upon admission had a significantly higher risk of developing in-hospital complications and increased mortality11,12. As patients with renal disorders reportedly have a higher risk of a diagnostic discrepancy9, we hypothesised that the presence of an initial diagnosis of AKI upon admission in the elderly might also affect diagnostic discrepancy upon their discharge. We prospectively investigated the relationship between the presence of AKI and diagnostic discrepancy by utilizing a consecutively enrolled cohort of geriatric patients.
Methods
Recruitment of participants and study design
Patients aged 60 years and older who were hospitalised in the general medical wards of National Taiwan University Hospital (NTUH) between December 2013 and November 2014 were prospectively enrolled. NTUH, an affiliate of National Taiwan University, is a 2000-bed tertiary medical center located in the capital of Taiwan serving patients with acute and chronic care needs around the country13. There are six general medical wards in NTUH admitting patients with general medical diseases including urinary tract infection, pneumonia, ileus, and others, but are not limited to specific types of disease. Those with surgical diseases or those requiring surgical interventions are ineligible for admission to the general medical wards. The mean age of admitted patients is 66.4 years, with a mean Charlson comorbidity index of 3, and 53.4% are men13. Pneumonia is the most common admission diagnosis, followed by urinary tract infection; nearly 95% patients were admitted via the emergency department.
Upon admission of the patient, we recorded medical history, age, sex, a comprehensive list of comorbidities, and their vital signs (blood pressure [BP] and heart rate [HR])11,14. Comorbidities were ascertained based upon corresponding laboratory data, imaging findings, pathologic evidence, or by certified specialists as appropriate. Laboratory data including haemogram and serum biochemistry test results were also collected. Diagnoses at admission were independently made by the attending staff, and were categorised into cardiopulmonary disorders, nephrourological disorders, gastrointestino-hepatic disorders, haemato-oncologic disorders, fever of unknown origin (FUO), and acute cerebrovascular events15. Variables pertaining to treatment courses, including intensive care unit transfer and hospital mortality, were also recorded.
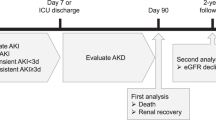
Presence of initial AKI was also ascertained upon admission, according to the serum creatinine (Scr) criteria of the KDIGO classification16. In brief, AKI was diagnosed if, upon admission, the participants had an Scr level increase ≥0.3 mg/dL within 48 hours or a 50% increase from their baseline Scr level within the 7 days before the current admission. In addition, grade 1, 2, and 3 AKI were diagnosed if the Scr level increased 50%, 100%, or 200% from the baseline level, respectively. We retrieved the baseline Scr level of all participants from three months before and up to the time of their admission. Chronic kidney disease (CKD) was defined as a baseline estimated glomerular filtration rate (eGFR) of less than 60 ml/min/1.73 m2 according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.
This study was approved by the ethical committee of NTUH (No. 201306089RINA) and all participants provided informed consent. This study adhered to the tenets of the Declaration of Helsinki.
Outcomes of interest
All elderly patients were prospectively followed up until discharge from the hospital or death. The same staff provided the admission and discharge diagnoses. After patient discharge, we documented discharge diagnoses using a similar classification method, and compared the discharge and admission diagnoses. A diagnostic discrepancy was noted if the main discharge and admission diagnoses differed.
Statistical analysis
SPSS 18.0 software (SPSS Inc., Chicago, IL, USA) was used in this study for statistical analysis. We described continuous variables as the mean ± standard deviation. Comparisons between each group were performed using an independent t-test or a Mann-Whitney U test, as appropriate. We described categorical variables as event numbers and percentages, and between-group comparisons were performed using a chi-square test.
Initially, we examined the overall clinical features including demographic profiles, comorbidities, admission diagnoses and vital parameters, as well as laboratory results. After these patients were discharged, we collected their discharge diagnoses to ascertain whether there was a diagnostic discrepancy. Those with diagnostic discrepancy after hospitalization are described in detail. We then compared clinical data between the participants with and without AKI to establish any significant differences. On univariate anlaysis, we made comparisons between those with and without diagnostic discrepancy. Those with significant differences were then selected and subsequently underwent multiple logistic regression analyses with the diagnostic discrepancy presence as the dependent variable. We utilised several pre-specified definitions for important variables in the multivariate analyses to affirm our findings, including binary division of the variable AKI (with vs. without) and severity-based grading of AKI (KDIGO grades). Sensitivity analyses based on different age strata and diagnostic subgroups were also conducted. Two-sided p-values less than 0.05 were considered statistically significant in all analyses.
Results
Clinical features of the participants
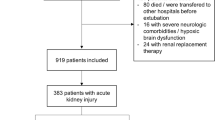
We enrolled 188 elderly patients during the study period (21.3% were aged between 60–70 years, 29.3% were between 70–80 years, and 49.5% were older than 80 years), with 84 (44.7%) presenting with AKI upon admission (Table 1). Among those with AKI, 61.9% of cases were related to sepsis, followed by hypotension (14; 16.7%), cardiorenal syndrome (11; 13.1%), dehydration (5; 6%), pancreatitis (1; 1.2%), and hepatorenal syndrome (1; 1.2%).
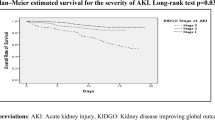
There was no significant difference between participants with or without initial AKI regarding demographic profiles (age and sex) and comorbidities. The participants with an initial AKI diagnosis had significantly lower systolic and diastolic BP compared to those without (initial AKI vs. without initial AKI: systolic BP, 125 vs. 145 mm Hg, p < 0.01; diastolic BP, 72 vs. 80 mm Hg, p < 0.01). Half of this cohort was admitted due to cardiopulmonary disorders (49%), followed by gastrointestinal and hepatic disorders (18%), and nephrourological disorders (12%). No significant differences were observed among laboratory data, diagnoses at admission, or receipt of intensive care between those with and without AKI. Among the participants, the overall hospital length of stay was 15.4 ± 15.6 days, and the mortality rate was 12%. Elderly with increasing severity of AKI had a significantly higher mortality (for non-AKI vs. KDIGO stage 1 vs. stage 2 vs. stage 3, 10% vs. 7% vs. 15% vs. 32%, p = 0.04) and a trend of longer hospital stay (for non-AKI vs. KDIGO stage 1 vs. stage 2 vs. stage 3, 14.4 ± 11 vs. 13.8 ± 12.5 vs. 19.1 ± 13.8 vs. 21 ± 34.5 days, p = 0.21). Upon discharge, the distribution of discharge diagnoses was similar to that of the admission diagnoses (Table 1).
Diagnostic discrepancy among elderly inpatients
After comparison between the admission and the discharge diagnoses, we found that 28 (14.9%) participants had a diagnostic discrepancy. A description of all the cases with a diagnostic discrepancy is provided in Table 2. One-fourth of the 28 patients were initially admitted for pulmonary/respiratory disorders and FUO, followed by nephrourological disorders (21%), and gastrointestino-hepatic disorders (14%).
Participants with initial AKI upon admission were significantly more likely to have a diagnostic discrepancy on discharge (with vs. without: 23% vs. 9%, p < 0.01). We further classified the diagnostic discrepancies into the following four types based on their reasoning: a switch from a general to a specific diagnosis (n = 10), confusion with presentations of different diseases (n = 4), emergence of in-hospital complications (n = 3), and an unrelated diagnosis not related to in-hospital complications (n = 11). We found that the participants with initial AKI were more likely to have a diagnostic discrepancy from an unrelated diagnosis compared to those without (with vs. without, 82% vs. 18%, p = 0.01; Fig. 1).
Comparisons between participants with and without diagnostic discrepancy
No significant difference in demographic profiles was observed between participants with and without a diagnostic discrepancy (Table 3). Those with a diagnostic discrepancy were significantly more likely to have heart failure (with vs. without: 32% vs. 16%, p = 0.04), but not other comorbidities. Nephrourological disorders and FUO were the most common admission diagnoses among the participants with a diagnostic discrepancy compared to those without (p = 0.03). Participants with a diagnostic discrepancy were more likely to have an initial AKI diagnosis on admission (p < 0.01), more likely to have received intensive care during hospitalization (p = 0.01), and had higher mortality (p < 0.01). Finally, oncologic disorders, fever of other infectious foci, and non–infection related fever were more common discharge diagnoses among the participants with a diagnostic discrepancy compared to those without (p < 0.01).
Regression analysis for factors influencing diagnostic discrepancies in the participants
We conducted multiple regression analysis to assess the relationship between an initial AKI diagnosis upon admission and diagnostic discrepancy among the participants of this cohort. After accounting for clinical parameters (demographic profiles, comorbidities, admission diagnoses, laboratory data) and treatment course variables, initial AKI diagnosis upon admission was associated with a significantly higher risk of a diagnostic discrepancy on discharge (OR 3.3, p < 0.01) (Table 4). An AKI of higher severity was also associated with a stepwise higher risk of a diagnostic discrepancy (for KDIGO grades 1, 2, and 3, OR 2.92, 3.91, and 4.32, p = 0.04, 0.03, and 0.02, respectively). These associations remained significant even after adjusting for other clinical parameters (Table 4). We also used different types of sensitivity analysis to affirm the validity of our findings. First, we focused on patients of different age strata for sub-analysis, with the results being essentially similar. Second, we excluded participants with stage 5 CKD (eGFR < 15 ml/min/1.73 m2) and repeated the analysis. AKI was still associated with a significantly higher risk of diagnostic discrepancy among the remaining participants (OR 5.38, p = 0.002). The participants with increasing AKI severity also exhibited a stepwise higher risk of having a diagnostic discrepancy (OR 4.61, 4.38, and 11.7 for stage 1, 2, and 3 AKI, p = 0.01, 0.04, and 0.002, respectively). Finally, we excluded those with FUO for reassurance. AKI was significantly associated with a higher risk of diagnostic discrepancy (OR 7.96, p = 0.001). Participants with increasing AKI severity exhibited a stepwise higher risk of diagnostic discrepancy (OR 6.74, 9.03, and 10.3 for stage 1, 2, and 3 AKI, p = 0.006, 0.023, and 0.004, respectively). It appears that removing those with advanced CKD or those with FUO further strengthens the identified associations, lending more credibility to our findings.
Discussion
We found that 14.9% of the participants had a diagnostic discrepancy upon discharge. Those with a diagnostic discrepancy were more likely to have been admitted for a nephrourological disorder or FUO, and no significant difference in comorbidity patterns was found regardless of discrepancy status. The presence of an initial AKI diagnosis on admission was significantly more common among the participants with a diagnostic discrepancy, with a correlation between severity of initial AKI and incrementally higher risk of a diagnostic discrepancy at discharge. Hence, it is likely that an initial AKI diagnosis among geriatric inpatients might interfere with the physicians’ ability to make appropriate diagnoses on admission, which could lead to diagnostic or treatment delay and potentially contribute to adverse patient prognosis.
The incidence of AKI has recently increased with increasing awareness among healthcare workers and patients, as well as the availability of novel biomarkers. AKI predominantly affects the elderly, who have both structural and functional renal alterations and less physiologic reserve to cope with nephrotoxic injuries17. Epidemiologic studies have suggested that the risk of AKI has increased by 5- to 10-fold in the elderly compared to that in the general population. The incidence of geriatric AKI varies widely between 5% and 50%, depending on the patients’ age, the clinical setting (medical, surgery, or mixed), and the requirement for intensive care12,18,19. In our cohort, the participants were predominantly of advanced age (mean, 77.9 years), and 44.7% of them had AKI on admission. This number is within the high-normal range of that reported in the literature, and underlines the need for assessing the impact of AKI in the geriatric population.
The issue of diagnostic discrepancy in hospitalised patients is rarely addressed in the literature, with no studies focusing on the elderly. The importance of evaluating diagnostic discrepancy might result from the concern over a close link between diagnostic discrepancies and medical errors6. Although the reasons for diagnostic discrepancy include true diagnostic errors, disagreement in interpretation, or inconsistencies in diagnostic criteria, the incidence of diagnostic discrepancies frequently parallels that of medical errors6,20. Consequently, improving diagnostic accuracy and mitigating factors that contribute to diagnostic discrepancies attenuate error rates and lower the risk of adverse events during hospitalization.
Notably, researchers started describing the prevalence of diagnostic discrepancies and their determinants 4 decades ago; they found that 26.8% of participants had diagnostic changes upon discharge21. A more recent study comparing the diagnoses made by emergency physicians to those made upon discharge discovered that 7% to 10% of admissions contained clinically important diagnostic discrepancies22. Similarly, Heuer et al. reported that nearly 10% of discharge diagnoses differed from the admission diagnoses in a multi-centre study23. Based on this, the rate of diagnostic discrepancy has decreased over time, presumably due to the advancement in medical diagnostics and the clinical experience of physicians24. In our study, we also observed that 14.9% of the participants had a diagnostic discrepancy after discharge (Table 3), which is slightly higher than that recently reported by other groups. This could result from our focus on geriatric patients only, as the incidence of diagnostic discrepancy is reportedly higher among the elderly and nursing home residents23.
The patient characteristics affecting the incidence of diagnostic discrepancy remain unclear. Advanced age, different admission diagnoses (medical diseases as opposed to surgical diseases), neurological disorders, and the presence of neurologic impairment have all been reported to increase the possibility of disagreement between admission and discharge diagnoses21,23. In addition, autopsy studies comparing postmortem diagnoses to antemortem diagnoses have suggested that patients with admission diagnoses of nephrourological or infectious diseases tend to have a diagnostic discrepancy9. Since nearly half of our participants with a diagnostic discrepancy were admitted for these disorders, our findings are similar to those of these autopsy studies (Table 3). We show that elderly participants with a diagnostic discrepancy are more likely to have AKI upon admission, independent of other clinical features, which has not been previously reported. In light of our finding, we propose that more attention is needed in the care of elderly patients with AKI upon admission to avoid potential medical errors during their hospitalization.
The reasons for diagnostic discrepancies include, but are not limited to, a switch from a general diagnosis to a more specific one in relevant fields, grossly incorrect initial impressions due to various reasons, an over- or under-estimation of disease severity, and others22,23,25. We discovered that most elderly patients with a diagnostic discrepancy were found to have unrelated diagnoses (39%), while a switch from general to specific diagnosis accounted for 36% of the cases (Fig. 1). Furthermore, the higher frequency of a diagnostic discrepancy among the elderly with AKI is likely due to a higher proportion of unrelated diagnoses made upon discharge. This is an interesting finding that might explain the association between AKI and diagnostic discrepancies. AKI adversely influences the outcomes of hospitalised patients, and early diagnosis and management of AKI has been strongly suggested by various researchers26. Considering the increasing awareness of AKI-related symptomatology, a possibility exists that the emphasis on AKI might overshadow the importance of other symptoms reported by patients, leading to an incomplete initial diagnosis list. Moreover, disease-related complaints of older patients are often more subtle and atypical compared to those of younger patients, further diverting the physician’s attention away from the main illnesses to AKI27. This increases the possibility of making an incorrect diagnosis during the initial visit28. It is also possible that the symptoms caused by AKI can mislead the physicians and prompt them to make an alternative diagnosis. In addition, the components of the examination for AKI, including serial blood and urine tests, radiologic examinations, or even renal biopsy, might supplant the necessary diagnostic tests for other accompanying illnesses. Moreover, adjunct diagnoses might be overlooked. A more holistic and comprehensive approach for managing geriatric patients is frequently needed, but when a major diagnosis, such as AKI, appears in the list of impressions, the effort to investigate other accompanying diagnoses might be less of a priority. This is an under-recognised influence on medical practice posed by AKI, especially in the elderly. Nonetheless, more investigations are needed to clarify other associations between initial AKI and diagnostic discrepancy in this population.
There are strengths and limitations to this study. Regarding strengths, we have identified an important risk factor; diagnostic discrepancies represent an important but under-recognised tool for assessing the care of the elderly. The dose-dependent relationship between AKI and diagnostic discrepancy further lends to the credibility of our findings. However, the single-centre nature and geriatric-only patient cohort in medical wards limit the applicability of these results. In addition, the size of our cohort is modest; studies enrolling more elderly patients might validate this phenomenon further. Additionally, the characteristics of patients admitted to the general medical wards of this institute might be different from those admitted to others, and extrapolation of our findings might not be feasible. More studies focusing on this issue are required to extend our findings.
Conclusion
The elderly population is gaining importance in healthcare, given the constant rise in the proportion of the older-aged. Diagnostic discrepancies can assist in the evaluation of diagnostic errors during clinical practice. We found that the incidence of a diagnostic discrepancy was 2- to 3-fold higher among elderly patients with an initial AKI diagnosis on admission, a finding that has not been previously reported. Therefore, reducing the risk of geriatric AKI might lower the incidence of diagnostic discrepancies among this patient population.
Additional Information
How to cite this article: Chao, C.-T. et al. Acute kidney injury as a risk factor for diagnostic discrepancy among geriatric patients: a pilot study. Sci. Rep. 6, 38549; doi: 10.1038/srep38549 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Goodman, R. A. et al. Multimorbidity Patterns in the United States: Implications for Research and Clinical Practice. J. Gerontol. A. Biol. Sci. Med. Sci 71, 215–220 (2016).
Buurman, B. M. et al. Trajectories of Disability Among Older Persons Before and After a Hospitalization Leading to a Skilled Nursing Facility Admission. J. Am. Med. Dir. Assoc. 17, 225–231 (2016).
Theou, O. et al. Exploring the relationship between national economic indicators and relative fitness and frailty in middle-aged and older Europeans. Age. Ageing. 42, 614–619 (2013).
Jain, S. et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N. Engl. J. Med. 373, 415–427 (2015).
Dwyer, R. et al. A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age. Ageing. 43, 759–766 (2014).
Berner, E. S. & Graber, M. L. Overconfidence as a Cause of Diagnostic Error in Medicine. Am. J. Med. 121, S2–S23 (2008).
Leape, L. L. et al. The Nature of Adverse Events in Hospitalized Patients. N. Engl. J. Med. 324, 377–384 (1991).
Baker, G. R. et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. Can. Med. Assoc. J. 170, 1678–1686 (2004).
Wittschieber, D. et al. Who Is at Risk for Diagnostic Discrepancies? Comparison of Pre- and Postmortal Diagnoses in 1800 Patients of 3 Medical Decades in East and West Berlin. PLoS. One 7, e37460 (2012).
Saad, R. et al. Comparison between clinical and autopsy diagnoses in a cardiology hospital. Heart. 93, 1414–1419 (2007).
Chao, C. T. et al.The severity of initial acute kidney injury at admission of geriatric patients significantly correlates with subsequent in-hospital complications. Sci. Rep. 5, 13925 (2015).
Chao, C. T. et al. Advanced age affects the outcome-predictive power of RIFLE classification in geriatric patients with acute kidney injury. Kidney. Int. 82, 920–927 (2012).
Hsu, N. C. et al. Why do general medical patients have a lengthy wait in the emergency department before admission? J. Formos. Med. Assoc. 113, 557–561 (2014).
Chao, C. T. et al. Cumulative Cardiovascular Polypharmacy Is Associated With the Risk of Acute Kidney Injury in Elderly Patients. Medicine. 94, e1251 (2015).
Chao C. T. et al. In Nonagenarians, Acute Kidney Injury Predicts In-Hospital Mortality, while Heart Failure Predicts Hospital Length of Stay. PLoS. One 8, e77929 (2013).
Section 2: AKI Definition. Kidney Int Suppl 2, 19–36 (2012).
Coca, S. G. Acute Kidney Injury in Elderly Persons. Am. J. Kidney. Dis. 56, 122–131 (2011).
Chronopoulos, A., Rosner, M. H., Cruz, D. N. & Ronco, C. Acute kidney injury in the elderly: a review. Contrib. Nephrol. 165, 315–321 (2010).
Chronopoulos, A., Cruz, D. N. & Ronco, C. Hospital-acquired acute kidney injury in the elderly. Nat. Rev. Nephrol. 6, 141–149 (2010).
Berner, E. S., Miller, R. A. & Graber, M. L. Missed and delayed diagnoses in the ambulatory setting. Ann. Intern. Med. 146, 470 (2007).
Leske, M. C., Sorensen, A. A. & Zimmer, J. G. Discrepancies between admission and discharge diagnoses in a university hospital. Med. Care. 16, 740–748 (1978).
Arntz, H. R., Klatt, S., Stern, R., Willich, S. N. & Beneker, J. Are emergency physicians’ diagnoses accurate? Anaesthesist 45, 163–170 (1996).
Heuer, J. F., Gruschka, D., Crozier, T. A., Bleckmann, A., Plock, E., Moerer, O., Quintel, M. & Roessler, M. Accuracy of prehospital diagnoses by emergency physicians: comparison with discharge diagnosis. Eur J Emerg Med 19, 292–296 (2012).
Sonderegger-lseli, K., Burger, S., Muntwyler, J. & Salomon, F. Diagnostic errors in three medical eras: a necropsy study. The. Lancet. 355, 2027–2031 (2000).
Liisanantti, J. H. & Ala-Kokko, T. I. The impact of antemortem computed tomographic scanning on postmortem examination rate and frequency of missed diagnosis. J. Crit. Care. 30, 1420.e1–e4 (2015).
Brady, P. et al. “SHOUT” to improve the quality of care delivered to patients with acute kidney injury at Great Western Hospital. BMJ. Qual. Improv. Rep. 4, pii: u207938.w3198, doi: 10.1136/bmjquality.u207938.w3198 (2015).
Morgan, R., Pendleton, N., Claque, J. E. & Horan, M. A. Older people’s perceptions about symptoms. Br. J. Gen. Pract. 47, 427–430 (1997).
Montgomery, J. & Mitty, E. Resident Condition Change: Should I Call 911? Geriatr. Nurs. 29, 15–26 (2008).
Acknowledgements
We are grateful to the assistance of the entire staff in the Second Core Laboratory of National Taiwan University Hospital (NTUH). This study is financially supported by NTUH grant (NO. 105-N3206) and Ministry of Science and Technology, Taiwan (MOST 105-2314-B-002-176-).
Author information
Authors and Affiliations
Consortia
Contributions
Study design – C.T.C., J.W.H., C.K.C.; Data analysis – C.T.C., H.B.T., J.W.H., C.K.C., COGENT study group (COhort of GEriatric Nephrology in NTUH study group); Drafting article – C.T.C., H.B.T., J.W.H., C.K.C., K.Y.H., COGENT study group (COhort of GEriatric Nephrology in NTUH study group); Approval of article – all authors.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chao, CT., Tsai, HB., Chiang, CK. et al. Acute kidney injury as a risk factor for diagnostic discrepancy among geriatric patients: a pilot study. Sci Rep 6, 38549 (2016). https://doi.org/10.1038/srep38549
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep38549
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.