Abstract
Sutures are an increasing focus of research in knee arthroplasty (KA). Whether knotless barbed sutures (KBS) are safe and efficient in KA remains controversial. The objective of our study is to compare the clinical outcomes of KA according to wound closure method: KBS versus knotted traditional sutures (KTS). To clarify this, we conducted a systematic review and meta-analysis. Nine articles involving 10 studies were included in this study. The dataset consisted of 1729 patients with 1754 KA. Among these, 814 patients’ wounds were closed with KBS and 915 with KTS. Our analysis indicates that KBS is preferable for KA wound closure given its shorter wound closure time and lower total cost; postoperative Knee Society scores and complication rates were similar to those of surgeries using KTS. The subgroup analysis revealed that closure of arthrotomy with KBS appears to be associated with a lower risk of complications. This meta-analysis indicates that use of KBS in KA reduces operative time and cost. KBS is the preferred option for wound closures, including arthrotomy and reattachment of subcutaneous and subcuticular tissues. Given the possible biases, adequately powered and better-designed studies with longer follow-up are required to reach a firmer conclusion.
Similar content being viewed by others
Introduction
As the population ages and medical technology improves, the rate of knee arthroplasties (KA) has increased considerably over the past two decades. According to a recent survey, the rate of KA increased by 59.4% from 1991 to 2010: that is, from 3.2 to 5.1 per 10,000 people1. This rapid growth in the number of surgeries has also coincided with innovation in surgical procedures, minimizing complications and improving postoperative function. Moreover, improper soft tissue handling remains a risk factor for complications after KA. Thus, sutures are an increasing focus of research in this field, as their quality is crucial to minimize wound complications and withstand forces across the incision during early postoperative knee motion2.
The knotless barbed suture (KBS) was first described by R.A. Mckenzie in 19673 and has since been adopted in several surgical fields4. KBS has been demonstrated to provide shorter closure time and better soft-tissue repair than knotted traditional suture (KTS) in plastic surgery, urology and obstetrics5,6,7. However, whether KBS is safe and efficient in KA remains controversial. Several studies have found that KBS provides several advantages, including elimination of the need for knot tying and handling of multiple sutures, shorter closure time, use of less suture material and improved tissue distribution8,9,10. Moreover, postoperative clinical outcomes are similar to those of surgeries using KTS2,4,11,12,13,14. In contrast, Campbell et al. found that KBS use is associated with a higher rate of infections requiring antibiotics than wound closure with KTS15. Furthermore, work by Smith et al. suggests that KBS is associated with greater frequency and severity of wound-related complications16.
Therefore, this quantitative meta-analysis was undertaken to inform clinical practice regarding which of the two suture methods (KBS or KTS) leads to better outcomes and lower rates of complications in KA.
Materials and Methods
This meta-analysis was performed strictly according to the guidelines for ‘preferred reporting items for systematic reviews and meta-analyses’ (the ‘PRISMA’ statement)17.
Data retrieval
Two independent researchers searched PubMed, Embase and the Cochrane Library. Data were last updated on March 4, 2015. The following keywords or corresponding Medical Subject Headings (MeSH) were used: “barbed” or “knotless” and “knee arthroplasty” or “knee replacement” or “joint replacement” or “joint arthroplasty”. Reference lists of the relevant articles were also reviewed for additional relevant studies. The search was not limited by language.
Inclusion criteria
Studies were identified according to the following inclusion criteria: 1) participants: human with relevant diseases requiring surgical intervention, 2) intervention: primary KA, 3) comparison: wound closure with the use of KBS (closing at least subcutaneous and subcuticular tissue) versus KTS (closing subcutaneous and subcuticular tissue as well as the arthrotomy), 4) Outcomes: at least one of the following: wound closure time, complications, cost, postoperative function, 5) Methodological criterion: a prospective study, a case-control study or a cohort study.
The following exclusion criteria were used: 1) insufficient data to estimate an odds ratio (OR) or weighted mean difference (WMD), 2) non-human or cadaver subjects, 3) redundant publications, 4) non-primary research (editorials, commentaries, etc.).
Data extraction
Two authors extracted relevant data independently, including the first author’s name, study design, publication year, number of patients in each group, average patient age, gender ratio, details on the suture method and technique, total complications and major complications, total cost of wound closure and postoperative Knee Society scores (KSS). Major complications were defined as those requiring further surgical interventions. Total cost of wound closure included both suture material and operating room time. The cost of operating room time estimates are based upon the average cost for professional staff and resources required for these cases. Intention-to-treat (ITT) data were used when available. Data in other forms, such as medians, interquartile ranges and means ± 95% confidence interval (CI), were converted to means ± SD following the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions 5.0.2.
Quality assessment
Using a 12-item scale18, the methodological quality of each included study was assessed by two independent researchers. The 12-item scale consisted of the following: adequate randomization, concealment of allocation, patient blinding, care provider blinding, outcome assessor blinding, dropout rate, ITT analysis, avoidance of selective reporting, similarity of baseline characteristics, similarity or absence of cofactors, patient compliance and similarity of timing. Disagreements were evaluated by kappa test and consensus was achieved by discussion with the corresponding author.
Statistical analysis
Statistical analyses were performed using Stata software (ver. 12.0; StataCorp LP, College Station, TX, USA). Weighted mean differences (WMD) with 95% confidence interval (95% CI) were calculated for continuous data and odds ratios (OR) with 95% CIs were calculated for dichotomous data. Statistical heterogeneity was assessed by Q-test and I2. I2 values of 25%, 50% and 75% were considered to indicate low, moderate and high heterogeneity, respectively19. If P > 0.1 and I2 < 50%, a fixed-effects model was used; otherwise, a random-effects model was used. For substantial heterogeneity (I2 > 50%), a sensitivity analysis (backward elimination step-wise regression analysis) was conducted by omitting one study sequentially to examine the influence of each.
The stratified subgroup analysis compared outcomes according to suture type (within the KBS group, whether the arthrotomy was closed with KBS; in the KTS group, whether subcuticular tissue was closed with a running or an interrupted suture) or study design (randomized controlled trials (RCTs) versus non-RCTs).
Publication bias was assessed by Egger’s test and Begg’s test. For all statistical analyses, with the exception of heterogeneity, a value of P < 0.05 was considered to indicate statistical significance and all tests were two-sided.
Results
Study selection
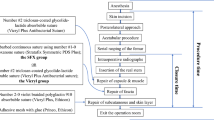
The article selection process is shown in Fig. 1. The search yielded 88 potentially relevant articles: 46 from PubMed, 32 from Embase and 10 from the Cochrane library. Of these, 32 duplicates were removed using Endnote software. Upon review of titles and abstracts of the 56 remaining articles, the full text of 11 articles was retrieved. Because sufficient data were not available in two articles, they were excluded20,21, leaving a total of nine articles included in this study2,4,11,12,13,14,15,16.
Study characteristics
The characteristics of the nine articles are presented in Table 1. These 9 articles, published between 2010 and 2015, actually include 10 studies; that by Smith et al.16 included a RCT and a retrospective study. Of these, four were RCTs, one was a prospective cohort study and five were retrospective studies. The dataset consisted of 1729 patients, including 1754 KA. Among these, 814 patients’ wounds were closed with KBS and 915 with KTS. Each study included between 18 and 416 patients. The average age, gender ratio and surgical site were also noted. In each study, the demographic characteristics of the two groups were similar.
For KA, details on the exact type of suture used and the method of placement are in Table 2. For surgeries involving both of KBS and KTS, placement and type of stitches varied. Among surgeries using the KBS method, the arthrotomy was closed with an interrupted knotted suture in two studies15,22, while others used a running KBS. In the KTS group, subcuticular tissue was closed with a running suture in three studies, while others used the interrupted suture technique.
Study quality
Table 3 shows the quality of the included studies. Of these, only one study was high quality; the others were of moderate quality. There was excellent inter-rater agreement between the investigators regarding eligibility (κ = 0.78).
Meta-analysis results
Wound closure time
In KA using the KBS method, wound closure times were on average 3.56 minutes shorter than in those using KTS (n = 971, WMD = −3.56, 95% CI = −5.05 to −2.08, P < 0.01, I2 = 94%, P < 0.01). We could not eliminate heterogeneity through a sensitivity analysis and thus a random-effects model was used.
Risk of total complications
No significant difference was detected in total complication rate between the two groups (n = 1729, OR = 0.98, 95% CI = 0.51 to 1.87, P = 0.95, I2 = 56%, P = 0.02). Heterogeneity was moderate in the pooled result (I2 = 56%); a sensitivity analysis was thus performed. Exclusion of data from the Campbell et al. study12 decreased heterogeneity significantly from 56% to 6%. However, there was still no difference in total risk of complications between the two groups (n = 1313, OR = 0.73, 95% CI = 0.46 to 1.15, P = 0.17, I2 = 6%, P = 0.38).
Major complications and other complications
Patients in both groups experienced similar rates of major complications (n = 1634, OR = 1.17, 95% CI = 0.67 to 2.18, P = 0.62, I2 = 17%, P = 0.30).
Full details of complications are summarized in Table 4. There were no differences between the two groups in rates of superficial infection, deep infection, wound dehiscence, arthrofibrosis, hematoma, or suture abscess.
Postoperative KSS
Three studies examined postoperative function in terms of KSS at 6 weeks after surgery. KA patients receiving KBS had a postoperative KSS value 0.98 points greater than those receiving KTS (n = 677, WMD = 0.98, 95% CI = 0.69 to 1.26, P < 0.01, I2 = 31%, P = 0.24).
Cost
The cost differences in terms of material between the two groups were summarized in Table 5. Upon analysis of the pooled cost data, KBS was associated with 290.72 USD lower costs than KTS (n = 871, WMD = −290.72, 95% CI = −474.00 to −107.45, P = 0.002, I2 = 99.1%, P < 0.01, Fig. 2).
Result of the subgroup analysis
Table 6 shows the results of the subgroup analysis. No significant difference was observed in risk of complications according to different types of study design (Supplement materials 1–3). Using KBS to close arthrotomies appears to lead to a lower total risk of complications relative to KTS. However, among surgeries employing KBS, rates of all complications, major complications (deep infection and others complications which required further surgical interventions, including polyethylene exchange, irrigation and debridement) and superficial infection were greater if KBS was not used for arthrotomy closure. Other factors did not differ significantly between the two groups.
Publication bias
Begg’s test (P = 0.89, continuity corrected) and Egger’s test (P = 0.108) indicated that publication bias did not affect our results.
Discussion
Our study found that in KA, KBS was associated with shorter wound closure times and lower costs than KTS. Meanwhile, closure of arthrotomies with KBS led to similar postoperative function and lower risk of all complications within the KBS group.
KBS was associated with a shorter time to wound closure in our study, confirming results of previous studies20,21,23,24. Stephens et al. found that KBS saved approximately 4 minutes in KA compared with KTS21. Moreover, in a study by Mansour et al. of spinal fusions, KBS resulted in a 40% reduction in wound closure time23. KBS is self-anchoring, requiring no knots, thus allowing faster closure13. However, we observed substantial heterogeneity in wound closure time, likely resulting from variation in KBS and KTS technique (Table 2). Among included studies, surgical approaches employing KBS varied with regard to suture method for arthrotomy and superficial skin closure, making significant heterogeneity in wound closure time unavoidable.
We observed no difference in complication rate between surgeries employing KBS versus KTS, consistent with previous studies20,21. Theoretically, knots may place uneven pressure on soft tissue, resulting in ischemia, while adsorption of bulky knots may cause local tissue inflammation and scarring and serve as a potential nidus for infection. Moreover, KBS provides more uniform tissue tension to reduce local ischemia, thereby decreasing risk of wound complications12. However, KBS is a running suture, which can strangulate the vascular supply and inhibit soft tissue healing16. Additionally, Shermak et al. found that KBS increases risk of wound healing complications in the arm25, which they speculated results from increased surface area caused by barbs and continuous suturing, promoting spread of inflammation along the length of the closure25.
Moreover, we also found that closure of arthrotomy, subcutaneous and subcuticular tissues with KBS appeared to decrease the total complication rate in KA. Conversely, arthrotomy closure by other methods in KBS group appeared to lead to a higher complication rate. A cadaver study simulating tense hemarthrosis found 74% lower leakage from a barbed suture arthrotomy closure than from KTS9. Arthrotomy leakage was minimal when distal arthrotomy closure was tight. Moreover, a biomechanical study found that KBS arthrotomy closure provides similar performance to interrupted KTS upon cyclical loading. Furthermore, KBS performed better than interrupted sutures when the repair was intentionally damaged8. Thus, using KBS to close arthrotomy is very important. Whereby achieving a more watertight wound closure may limit the risk of complications9.
At early stages (<6 weeks), patients receiving KBS had 0.98 higher postoperative KSS than those receiving KTSs in our study; this difference was not clinically significant. Likewise, Sah et al. found that range of knee motion is similar for both suture methods for up to one year2. An adequately powered RCT with long-term follow-up is necessary to determine the effect of suture method on recovery of function.
Our analysis found that KBS to significant cost savings. Similarly, Mansour et al. found that KBS closure of spinal fusion incisions resulted in hospital charges for operation time that were 884.60 USD lower than those of surgeries using KTS23. The cost of operating room time estimates are based upon the average cost for professional staff and resources required for these cases. The average cost of operating room was USD 62 per minute (range, USD 22–133/minute) in 100 United States hospitals26. In our study, KBS were associated with a mean savings of 3.56 minutes, which is in the range of 2.08 to 5.05 minutes with use of this suture device. Of note, the material cost with KTS could be saved USD 91.93, at most, in these included studies. Though barbed closure materials are more expensive than those for KTS, shorter surgery time leads to a reduced total cost.
To our knowledge, this is the first meta-analysis comparing the risk of complications and postoperative function between KBS and KTS for KA that includes all available comparative evidence and comprehensively investigates differences in the clinical outcomes. However, it has the following limitations. Most importantly, surgeries classified as KBS and KTS included multiple methods for closing superficial skin (Table 2), making significant heterogeneity in wound closure time and total cost unavoidable. Moreover, there is a lack of uniform technique of KTS. Second, as few RCTs in this area have been performed (perhaps because KBS remains relatively new in KA), our study included several non-RCTs, which inevitably involved recall and interviewer bias, which likely weakened our analysis. Nonetheless, excluding non-RCTs would have underpowered the analysis, increase the risk of false-negative errors and influence the accuracy of our findings. Demographic characteristics were similar between the two groups in all included studies, suggesting that selection bias was limited. Third, follow-up duration was relatively short, preventing examination of long-term outcomes, especially postoperative function. Furthermore, the bias might also be produced by the variations of stitches, such as V-Loc stitch and Quill stitch in KBS.
Conclusions
Based on available evidence, use of KBS in KA leads to shorter operation times and lower total costs. Closure of arthrotomy and subcutaneous and subcuticular tissues by KBS yields similar postoperative function and lower total complication risk when compared with KTS. We thus conclude that KBS is an optimal approach for closure of arthrotomies and subcutaneous and subcuticular tissues in KA. Given the relevant possible biases in our study, adequately powered and better-designed studies with long-term follow-up are required to reach a firmer conclusion.
Additional Information
How to cite this article: Zhang, W. et al. Barbed versus traditional sutures for wound closure in knee arthroplasty: a systematic review and meta-analysis. Sci. Rep. 6, 19764; doi: 10.1038/srep19764 (2016).
References
Oleske, D. M., Bonafede, M. M., Jick, S., Ji, M. & Hall, J. A. Electronic health databases for epidemiological research on joint replacements: considerations when making cross-national comparisons. Ann Epidemiol. 24, 660–5 (2014).
Sah, A. P. Is There an Advantage to Knotless Barbed Suture in TKA Wound Closure? A Randomized Trial in Simultaneous Bilateral TKAs. Clin Orthop Relat Res. 473 2019–27 (2015).
McKenzie, A. R. An experimental multiple barbed suture for the long flexor tendons of the palm and fingers. Preliminary report. J Bone Joint Surg Br. 49 440–7 (1967).
Maheshwari, A. V. et al. Barbed sutures in total knee arthroplasty: are these safe, efficacious and cost-effective? J Knee Surg. 28 151–6 (2015).
Villa, M. T., White, L. E., Alam, M., Yoo, S. S. & Walton, R. L. Barbed sutures: a review of the literature. Plast Reconstr Surg. 121 102e–08e (2008).
Wright, R. C. et al. Extensor mechanism repair failure with use of bidirectional barbed suture in total knee arthroplasty. J Arthroplasty. 27 1413 e1–4 (2012).
Paul, M. D. Barbed sutures in aesthetic plastic surgery: evolution of thought and process. Aesthet Surg J. 33 17S–31S (2013).
Vakil, J. J. et al. Knee arthrotomy repair with a continuous barbed suture: a biomechanical study. J Arthroplasty. 26 710–3 (2011).
Nett, M., Avelar, R., Sheehan, M. & Cushner, F. Water-tight knee arthrotomy closure: comparison of a novel single bidirectional barbed self-retaining running suture versus conventional interrupted sutures. J Knee Surg. 24 55–9 (2011).
Zaruby, J., Gingras, K., Taylor, J. & Maul, D. An in vivo comparison of barbed suture devices and conventional monofilament sutures for cosmetic skin closure: biomechanical wound strength and histology. Aesthet Surg J. 31 232–40 (2011).
Eickmann, T. & Quane, E. Total knee arthroplasty closure with barbed sutures. J Knee Surg. 23 163–7 (2010).
Gililland, J. M. et al. Barbed versus standard sutures for closure in total knee arthroplasty: a multicenter prospective randomized trial. J Arthroplasty. 29 135–8 (2014).
Gililland, J. M., Anderson, L. A., Sun, G., Erickson, J. A. & Peters, C. L. Perioperative Closure-related Complication Rates and Cost Analysis of Barbed Suture for Closure in TKA. Clin Orthop Relat R. 470 125–29 (2012).
Ting, N. T., Moric, M. M., Della Valle, C. J. & Levine, B. R. Use of knotless suture for closure of total hip and knee arthroplasties: a prospective, randomized clinical trial. J Arthroplasty. 27 1783–8 (2012).
Campbell, A. L., Patrick, D. A., Jr., Liabaud, B. & Geller, J. A. Superficial wound closure complications with barbed sutures following knee arthroplasty. J Arthroplasty. 29 966–9 (2014).
Smith, E. L., DiSegna, S. T., Shukla, P. Y. & Matzkin, E. G. Barbed versus traditional sutures: closure time, cost and wound related outcomes in total joint arthroplasty. J Arthroplasty. 29 283–7 (2014).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 151 264–9, W64 (2009).
Furlan, A. D., Pennick, V., Bombardier, C., van Tulder, M. & Editorial Board C. B. R. G. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 34 1929–41 (2009).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ. 327 557–60 (2003).
Levine, B. R., Ting, N. & Della Valle, C. J. Use of a barbed suture in the closure of hip and knee arthroplasty wounds. Orthopedics. 34 e473–5 (2011).
Stephens, S., Politi, J. & Taylor, B. C. Evaluation of Primary Total Knee Arthroplasty Incision Closure with the Use of Continuous Bidirectional Barbed Suture. Surg Technol Int. 21 199–203 (2011).
Patel, R. M., Cayo, M., Patel, A., Albarillo, M. & Puri, L. Wound complications in joint arthroplasty: comparing traditional and modern methods of skin closure. Orthopedics. 35 e641–6 (2012).
Mansour, A., Ballard, R., Garg, S., Baulesh, D. & Erickson, M. The Use of Barbed Sutures During Scoliosis Fusion Wound Closure: A Quality Improvement Analysis. J Pediatr Orthoped. 33 786–90 (2013).
Rosenberg, A. G. The use of a barbed suture in hip and knee replacement wound closure. Seminars in Arthroplasty. 24 132–34 (2013).
Shermak, M. A., Mallalieu, J. & Chang, D. Barbed suture impact on wound closure in body contouring surgery. Plast Reconstr Surg. 126 1735–41 (2010).
Macario, A. What does one minute of operating room time cost? J Clin Anesth. 22 233–6 (2010).
Acknowledgements
This work was supported by a grant from the National Natural Science Foundation of China (No. 81271973 and No. 81201397), the Zhejiang Provincial Natural Science Foundation of China (No. LY15H060001; No. LY15H060002 and No. LY13H060002) and Zhejiang medical and health science and technology plan project (No. 2015116473).
Author information
Authors and Affiliations
Contributions
W.Z. and D.X. carried out the entire procedure including the literature search, data extraction, performed the statistical analysis, drafted the manuscript, revised submitted the manuscript. Z.P. conceived of the study, coordinated and participated in the entire process of drafting and revised the manuscript. H.Y., H.X., H.M. and E.C. contributed to statistical analysis and revision the manuscript. D.H. contributed to the literature search, data extraction and the statistical analysis. D.H. and H.X. contributed to the revisions of the manuscript. All authors have contributed significantly. All authors read and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Competing interests
All authors have contributed significantly and are in agreement with the content of the manuscript. All authors have no relevant financial relationships to disclose.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhang, W., Xue, D., Yin, H. et al. Barbed versus traditional sutures for wound closure in knee arthroplasty: a systematic review and meta-analysis. Sci Rep 6, 19764 (2016). https://doi.org/10.1038/srep19764
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep19764
This article is cited by
-
The Examination of the Benefits of the Usage of Barbed, Knotless Suture in Capsule Repair During Total Knee Arthroplasty: A Prospective, Double-Blind, Randomized Controlled Study
Indian Journal of Orthopaedics (2023)
-
Chirurgisches Nahtmaterial – Grundlagen
Operative Orthopädie und Traumatologie (2023)
-
The use of novel knotless barbed sutures in posterior long-segment lumbar surgery: a randomized controlled trial
Journal of Orthopaedic Surgery and Research (2022)
-
Barbed Sutures for Total Hip and Knee Arthroplasty Have Shorter Wound Closure Time and are Cost-Effective in Comparison to Traditional Sutures: A Systematic Review and Meta-analysis of 16 Randomized Controlled Trials
Indian Journal of Orthopaedics (2022)
-
Barbed sutures reduce arthrotomy closure duration compared to interrupted conventional sutures for total knee arthroplasty: a randomized controlled trial
MUSCULOSKELETAL SURGERY (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.