Abstract
To examine whether the predictive performance of prostate-specific antigen (PSA) and PSA-related markers for prostate cancer (PCa) is modified by body mass index (BMI). Patients with a PSA 2–10 ng/mL who underwent multicore prostate biopsies were recruited from three tertiary centers. Serum markers measured included total PSA (tPSA), free-to-total PSA (f/tPSA), p2PSA, percentage of p2PSA (%p2PSA) and prostate health index (PHI). The association between serum markers and PCa risk was assessed by logistic regression. Predictive performance for each marker was quantified using the area under the receiver operator curves (AUC). Among 516 men, 18.2% had PCa at biopsy. For all tested markers, their predictive value on PCa risk was lower in obese patients compared to normal weight patients. We found statistically significant interactions between BMI and tPSA (P = 0.0026) and p2PSA (P = 0.038). PHI achieved an AUC of 0.872 in normal weight patients and 0.745 in obese patients, which outperformed the other predictors regardless of BMI category. In conclusion, PHI achieved the best predictive performance for detecting PCa and was not influenced by BMI.
Similar content being viewed by others
Introduction
Over the last decade, a steady increase in prostate cancer (PCa) incidence has been observed in the People’s Republic of China1. In developed areas such as Shanghai, an annual increase of 8% was reported and PCa was ranked as the fifth most common male malignancy in this region after 20101. The emerging incidence of PCa may be partly explained by the widespread use of prostate-specific antigen (PSA) testing in urban areas. We previously examined patient characteristics in patients undergoing radical prostatectomy between 2012 and 2014 and found that 64.3% of those patients had increased PSA levels but no PCa symptoms, suggesting wide-spread PSA screening2. In contrast, in 2005 the percentage of patients undergoing radical prostatectomy with T1c disease (elevated PSA only) was as low as 10%, as reported by a multicenter study from the People’s Republic of China3.
Over the past 15 years, not only has PCa incidence increased, but similar trends have been noted in increased body mass index rates4. Hou et al. compared two cross-sectional surveys (1998–2001 vs. 2007–2008) that investigated the prevalence of obesity among Chinese adults in urban Shanghai5 and found that among men during that period, the prevalence of obese (body mass index [BMI] ≥ 25) increased from 31.5% to 39.1% while metabolically active obesity (i.e. central obesity) increased from 19.5% to 27.3%.5
The difficulty of detecting PCa in obese men is well recognized6. One of the main reasons cancers can be harded to find in obese men is that obese subjects have lower serum PSA values due to hemodilution7. However, detection biases of serum markers could be minimized or even reversed by the higher probability of PCa in obese individuals8. Recently, Abrate et al. assessed the effect of obesity on the predictive value of PSA-related markers in European patients9. Their findings indicated that PSA and all PSA-based markers (p2PSA, %p2PSA and PHI) except free PSA and percent free PSA performed better in obese men. However, in general there were no differences between normal weight and obese subjects arguing against a dose-response effect. As such, there is no clear logical explanation for those findings. Indeed, multiple other studies suggest that obesity does not modify the ability of PSA in predicting PCa10,11. To what degree those results can be generalized to Chinese men is unclear because there is a pronounced difference in PCa incidence between Chinese and Caucasian populations. For men with PSA 4–10 ng/mL, the detection rate of PCa may in Caucasian men may be up to 40%9,11, but only approximately 20% in Chinese men12. Also, how BMI affects other serum based markers beyond PSA has not been tested to date with the exception of the study by Abrate et al.
Herein, we examined the associations between PSA-related markers and PCa risk according to BMI categories among men undergoing prostate biopsy. Specifically, we tested for interactions between BMI and serum makers to assess whether BMI affected the ability of these PSA-based markers to predict PCa diagnosis. Furthermore, we used head-to-head comparisons to find predictors with superior discriminative ability in different BMI subgroups. We hypothesized that the predictive value of PSA serum markers to detect PCa at biopsy would not be influenced by BMI.
Results
Baseline study characteristics
Of 516 men included in this study, PCa was diagnosed in 94 (18.2%) subjects, including 64 (12.4%) with Gleason score ≥7. Using a BMI cutoff of 25 kg/m2 13, 188 (36.4%) men were defined as being obese (BMI ≥ 25 kg/m2) at the time of biopsy. There was no significant difference in demographic or clinical characteristics between normal weight and obese men (all p ≥ 0.068) ( Table 1 ). Similarly, normal weight and obese men had similar rates of PCa detection including similar risks of high-grade disease (all ≥ 0.594).
Effect of serum based markers on PCa risk stratified by BMI
As shown in Table 2 , logistic regression analysis models revealed the effect size (odds ratios, OR) of serum predictors on PCa risk in the entire sample and stratified by BMI. Although tPSA was significantly associated with PCa risk in the normal weight subgroup (OR = 1.369, p < 0.0001), the association was lost in the obese subgroup (OR = 0.962, p = 0.661) (p-interaction = 0.0026). A similar trend was also observed for p2PSA and its effect size was halved in obese men (OR = 1.063, p = 0.038) compared with their normal weight counterparts (OR = 1.132, p < 0.001) (p-interaction = 0.038). While a similar trend was noticed for PHI (i.e. stronger in normal weight men compared to obese men), it was a strong predictor in both groups (both p < 0.001) and the interaction was not statistically significant (p-interaction = 0.085).
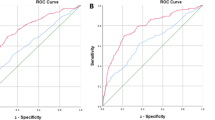
We further evaluated which serum marker had the best discriminative ability among normal weight and obese subgroups, respectively. The AUC of all predictors was lower in the obese samples ( Table 3 ). Among normal weight men, PHI had the highest discriminative ability among the five predictors examined with an AUC of 0.872 and a specificity of 60.9% when sensitivity was set to 90%. Indeed, its accuracy was significantly greater than all markers (all p ≤ 0.001). In the obese group, PHI still achieved the highest AUC of 0.745 and remained significantly better than all other markers (all p≤0.01) except %p2PSA, which had similar accuracy (AUC 0.731).
Effect of serum based markers on high-grade PCa risk stratified by BMI
Finally, we evaluated the influence of BMI on serum markers’ effect size (Supplementary Table 1) and discriminative ability (Supplementary Table 2) for detecting high-grade disease. Importantly, all markers except tPSA (p-interaction = 0.014) showed equal ability to detect high-grade disease in normal weight and obese men (all p-interaction ≥ 0.59). Similar to predicting all cancers, PHI had the best discriminative accuracy in normal weight men (AUC 0.885) and obese men (AUC 0.839). Also, PHI outperformed all other markers in normal weight men (all p ≤ 0.001) and all other markers in obese men (all p ≤ 0.025) except %p2PSA (p = 0.806).
Discussion
In this multicenter study of men who underwent extended biopsy, we tested whether the predictive performance of serum PSA-related tumor markers for PCa was influenced by obesity. Our findings showed a weaker association with PCa in obese men for all tested markers. The interaction between obesity and serum predictors was statistically significant for tPSA and p2PSA, but not for PHI. PHI achieved better discriminative ability for PCa than PSA and its derivatives in both normal weight and obese men.
There are several possible ways by which obesity may influence the predictive performance of serum markers6. First, the hemodilution effect of PSA is well recognized in obese men7. The implication is that circulating PSA levels released from PCa tissue are diluted in obese men due to greater blood volume leading to lower PSA levels. However, in our study, we did not see lower tPSA levels in obese men. In fact, obese men had slightly higher tPSA levels, though this was not statistically significant. The hemodilution theory, as PSA is simply diluted and the association with PCa is not fundamentally changed, it is anticipated that this would have no effect on BMI modifying the ability of serum markers to detect PCa.
An alternative way that obesity may affect the performance of serum markers is that obese men have larger prostate volumes. This poses a problem from two aspects. First, this increases the probability of false-negative biopsies (i.e. difficulty finding the cancer). Second, larger prostates result in larger PSA values, independent of PCa, thereby decreasing the accuracy of PSA. Indeed, treatment for enlarged prostate with a 5-alpha reductase inhibitor, which shrinks the prostate, results in improved accuracy of PSA for predicting total and high-grade prostate cancer14. However, while prostate volumes in our cohort were larger in the obese men, the differences compared to normal weight men were small and not significant. Nonetheless, larger prostates and hence greater degree of benign prostatic hyperplasia in obese men would be expected to worsen serum markers ability to detect PCa in obese men.
A third way that obesity may influence serum-markers is that obesity may be related to different subtypes of PCa15 differently. Specifically, in PSA-screened men, obesity appears to be associated with low risk of low-grade PCa and higher risk of high-grade PCa6. As most serum markers perform better for high-grade disease, this would be expected to result in serum markers performing better in obese men.
In summary, depending on the potential mechanism, serum markers could be postulated to work similarly, worse, or better in obese men. Given this controversy, it is of note that multiple prior studies have addressed the performance of serum markers for detecting PCa as a function of elevated BMI (Supplementary Table 3)9,11,16,17,18,19. Among these seven studies (including the current study), three reported notable alterations in PSA performance by BMI categories whereas four, including two from Korea, showed no differences. Among the three studies that found obesity altered PSA’s performance, Abrate et al. found an increased performance of PSA among obese European men9. Conversely, our group and Chiu et al.16 showed the reverse relationship in Chinese men. The reasons for these discrepancies are not clear. However, we do note that the cancer detection rate in the two Chinese studies (16–18%) is much lower than the other studies (22–43%). Also, the two Chinese studies had the lowest percentage of men with “elevated” BMI (defined as >25 kg/m2 in the current study). Thus, it remains plausible that geographic differences and underlying PCa biological differences across ethnic groups could contribute to our findings. However, our findings are consistent with the only prior study from China, lending some credibility to our findings. Future research is needed to better outstand how geographic and ethnic differences in PCa may alter the ability to detect PCa as a function of obesity and current serum based markers.
Given the high rate of negative biopsies (>80% in the current study), despite an elevated PSA of 2–10 ng/ml, new and better serum markers are needed. Within our cohort, PHI was the strongest predictor of overall and high-grade PCa and importantly its performance was not influenced by BMI. Other studies have also shown that PHI is an accurate predictor of PCa including in Chinese patients20,21. As such, future studies should further explore PHI as a strong predictor of PCa, including high-grade disease.
The strength of our study is its multicenter design, head-to-head comparisons of multiple serum markers and that we enrolled a contemporary cohort of prostate biopsies in an under-reported population. However, the current study has several limitations. First, patients were recruited consecutively from three tertiary centers in Shanghai and Hong Kong. Thus, our results should be interpreted with caution for possible selection bias and may not be applicable to community-based series. Second, although all centers were experienced in multicore prostate biopsies and pathological examination, the possibility of underdiagnoses should be acknowledged. Third, all men were selected for biopsy due to an elevated PSA and those with very high PSA values (>10 ng/ml) were excluded. This creates a narrow and truncated range for PSA and thus inhibits its ability to predict PCa. Moreover, it results in us being unable to assess the performance of the other markers in a broad secreening population. Finally, the drawbacks of BMI for characterizing adiposity have been recognized22. Therefore, our study should be considered as one step toward optimizing tumor marker use in the context of an obesity epidemic. We are prospectively collecting more data, such as waist circumference and waist-to-hip ratio, for further analyses.
In conclusion, in our cohort of men undergoing prostate biopsy in China with a cancer detection rate of 18%, all serum markers, except PHI, performed better in normal weight men relative to obese men. Overall, PHI had the best performance characteristics for detecting overall and high-grade PCa and was not influenced by BMI. PHI appears to be a promising biomarker for predicting overall and high-grade PCa among men in the PSA gray zone of 2-10 ng/ml.
Material and Methods
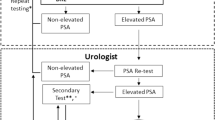
Study population
Patients were recruited from three tertiary centers, two from Shanghai (Fudan University Shanghai Cancer Center and Fudan University Huashan Hospital) and one from Hong Kong (Chinese University of Hong Kong). The period for recruitment was between April 2012 and August 2014 for Shanghai and between April 2008 and April 2013 for Hong Kong. Biopsy indication was PSA >4 ng/mL or abnormal digital rectal examination (DRE). Patients underwent transrectal ultrasound-guided prostate biopsies according to a standardized extended scheme with at least 10 cores. Specific genitourinary pathologists evaluated the biopsy tissue. Serum taken prior to biopsy was assayed for [-2]proPSA (p2PSA, pg/ml), total PSA (tPSA, ng/ml) and free PSA (fPSA, ng/ml) using Beckman Coulter’s DxI 800 Immunoassay system in a central laboratory. f/tPSA and %p2PSA were calculated as  and
and  , respectively. Prostate health index (PHI) was calculated according to the following formula:
, respectively. Prostate health index (PHI) was calculated according to the following formula:  . BMI was categorized as normal weight (<25 kg/m2) vs. obese (≥25 kg/m2) according to World Health Organization and National Institute of Health classifications23. Few patients had a BMI ≥ 30 kg/m2 (n = 12).
. BMI was categorized as normal weight (<25 kg/m2) vs. obese (≥25 kg/m2) according to World Health Organization and National Institute of Health classifications23. Few patients had a BMI ≥ 30 kg/m2 (n = 12).
For the current analyses, the inclusion criteria were an initial prostate biopsy and PSA of 2–10 ng/mL. We excluded patients with acute prostate infection (National Institute of Health Classification, Category I24), history of 5-α reductase inhibitor use within 6 months prior to biopsy and a serum sample archived for more than 3 years. This study was carried out in accordance with the ethical standards of Helsinki Declaration II and approved by the Institution Review Boards of Fudan University Shanghai Cancer Center, Fudan University Huashan Hospital and Chinese University of Hong Kong. Written informed consent was obtained from each patient before any study-specific investigation was performed.
Statistical Analysis
Our primary outcome was PCa diagnosis at biopsy by BMI category and our exposures were serum total PSA, free PSA and [–2] proPSA (p2PSA). Free-to-tPSA ratio (%fPSA), p2PSA-to-tPSA ratio, PSA density (PSAD) and PHI, were calculated, using standard formulas. Continuous variables are presented as median and interquartile ranges and categorical variables are presented as nominal numbers (or numerical values) and percentages. For comparisons, the Chi-square and rank sum tests were used for categorical variables and continuous variables, respectively. Logistic regression models were used to test the associations between serum markers and PCa risk at biopsy stratified by BMI category. As markers were collinear, separate models were run for each marker. Interaction terms between serum markers and BMI categories for predicting PCa were then assessed by using a cross-product term in the respective model. Discriminative ability was quantified as area under the receiver operating characteristic curve (AUC). The DeLong method was used to compare AUCs. All statistical analyses were performed using R and publicly available packages. Significance was set at P < 0.05.
Additional Information
How to cite this article: Zhu, Y. et al. Effect of Body mass index on the performance characteristics of PSA-related markers to detect prostate cancer. Sci. Rep. 6, 19034; doi: 10.1038/srep19034 (2016).
References
Zhu, Y., Wang, H. K., Qu, Y. Y. & Ye, D. W. Prostate cancer in East Asia: evolving trend over the last decade. Asian journal of andrology 17, 48–57, 10.4103/1008-682X.132780 (2015).
Zhu, Y. et al. Pathological Features of Localized Prostate Cancer in China: A Contemporary Analysis of Radical Prostatectomy Specimens. PloS one 10, e0121076, 10.1371/journal.pone.0121076 (2015).
Peyromaure, M. et al. Management of prostate cancer in China: a multicenter report of 6 institutions. J Urol 174, 1794–1797, 10.1097/01.ju.0000176817.46279.93 (2005).
Gordon-Larsen, P., Wang, H. & Popkin, B. M. Overweight dynamics in Chinese children and adults. Obesity reviews : an official journal of the International Association for the Study of Obesity 15 Suppl 1, 37–48, 10.1111/obr.12121 (2014).
Hou, X. et al. Ten-year changes in the prevalence of overweight, obesity and central obesity among the Chinese adults in urban Shanghai, 1998–2007 - comparison of two cross-sectional surveys. BMC public health 13, 1064, 10.1186/1471-2458-13-1064 (2013).
Allott, E. H., Masko, E. M. & Freedland, S. J. Obesity and prostate cancer: weighing the evidence. European urology 63, 800–809, 10.1016/j.eururo.2012.11.013 (2013).
Banez, L. L. et al. Obesity-related plasma hemodilution and PSA concentration among men with prostate cancer. Jama 298, 2275–2280, 10.1001/jama.298.19.2275 (2007).
Renehan, A. G., Tyson, M., Egger, M., Heller, R. F. & Zwahlen, M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371, 569–578, 10.1016/S0140-6736(08)60269-X (2008).
Abrate, A. et al. Clinical performance of Prostate Health Index (PHI) for prediction of prostate cancer in obese men: data from a multicenter European prospective study, PROMEtheuS project. BJU Int, 10.1111/bju.12907 (2014).
Vidal, A. C. et al. Does obesity modify the ability of pre-biopsy PSA to detect prostate cancer on repeat biopsy? Results from the REDUCE study. J Urol, 10.1016/j.juro.2015.01.111 (2015).
Banez, L. L., Albisinni, S., Freedland, S. J., Tubaro, A. & De Nunzio, C. The impact of obesity on the predictive accuracy of PSA in men undergoing prostate biopsy. World J Urol 32, 323–328, 10.1007/s00345-012-0919-9 (2014).
Ren, S. et al. Plateau effect of prostate cancer risk-associated SNPs in discriminating prostate biopsy outcomes. The Prostate, 10.1002/pros.22721 (2013).
Kanazawa, M. et al. Criteria and classification of obesity in Japan and Asia-Oceania. World review of nutrition and dietetics 94, 1–12, 10.1159/000088200 (2005).
Thompson, I. M. et al. Effect of finasteride on the sensitivity of PSA for detecting prostate cancer. Journal of the National Cancer Institute 98, 1128–1133, 10.1093/jnci/djj307 (2006).
Liu, J. et al. High-calorie diet exacerbates prostate neoplasia in mice with haploinsufficiency of Pten tumor suppressor gene. Molecular metabolism 4, 186–198, 10.1016/j.molmet.2014.12.011 (2015).
Chiu, P. K. et al. Role of PSA density in diagnosis of prostate cancer in obese men. Int Urol Nephrol 46, 2251–2254, 10.1007/s11255-014-0826-7 (2014).
Oh, J. J. et al. Does obesity affect the accuracy of prostate-specific antigen (PSA) for predicting prostate cancer among men undergoing prostate biopsy. BJU Int 112, E265–271, 10.1111/j.1464-410X.2012.11766.x (2013).
Kim, J. H. et al. Impact of obesity on the predictive accuracy of prostate-specific antigen density and prostate-specific antigen in native Korean men undergoing prostate biopsy. International journal of urology: official journal of the Japanese Urological Association 21, 987–990, 10.1111/iju.12486 (2014).
Vidal, A. C. et al. Does Obesity Modify the Ability of Prebiopsy Prostate Specific Antigen to Detect Prostate Cancer on Repeat Biopsy? Results from the REDUCE Study. J Urol, 10.1016/j.juro.2015.01.111 (2015).
Huang, Y. Q., Sun, T., Zhong, W. D. & Wu, C. L. Clinical performance of serum [−2] proPSA derivatives, %p2PSA and PHI, in the detection and management of prostate cancer. American journal of clinical and experimental urology 2, 343–350 (2014).
Na, R. et al. Performance of serum prostate-specific antigen isoform [−2] proPSA (p2PSA) and the prostate health index (PHI) in a Chinese hospital-based biopsy population. The Prostate 74, 1569–1575, 10.1002/pros.22876 (2014).
Okorodudu, D. O. et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. International journal of obesity 34, 791–799, 10.1038/ijo.2010.5 (2010).
Aronne, L. J. Classification of obesity and assessment of obesity-related health risks. Obesity research 10 Suppl 2, 105S–115S, 10.1038/oby.2002.203 (2002).
Krieger, J. N., Nyberg, L., Jr. & Nickel, J. C. NIH consensus definition and classification of prostatitis. Jama 282, 236–237 (1999).
Acknowledgements
This study was supported by National Natural Science Foundation of China (Grant No. 81472377) and Shanghai municipal hospital emerging advanced technology joint research project (Grant No. SHDC12013122).
Author information
Authors and Affiliations
Contributions
Y.Z. and T.C.H. acquired the data and drafted the manuscript, Y.Z. and G.M.Z. analyzed the data, F.L. and Q.D. interpreted the data, J.F.X., A.C.V. and S.T.F. edited all tables, W.D.Y. and A.C.N. designed the study. All authors reviewed and approved the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhu, Y., Han, CT., Zhang, GM. et al. Effect of Body mass index on the performance characteristics of PSA-related markers to detect prostate cancer. Sci Rep 6, 19034 (2016). https://doi.org/10.1038/srep19034
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep19034
This article is cited by
-
Using clinical parameters to predict prostate cancer and reduce the unnecessary biopsy among patients with PSA in the gray zone
Scientific Reports (2020)
-
A predictive model for prostate cancer incorporating PSA molecular forms and age
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.