Abstract
A survey was set up to gauge the opinions of neonatologists on the role of Ureaplasma in bronchopulmonary dysplasia (BPD) development, the use of azithromycin for BPD prevention and the factors influencing azithromycin use in European neonatal intensive care units (NICUs). 167 NICUs participated in the survey, representing 28 European countries. For respondents, the two major perceived risk factors for BPD were prematurity of <28 weeks and high oxygen requirements. Only 38% of NICUs had a protocol for BPD prevention and 47% routinely tested for Ureaplasma. In cases of infection, macrolides were the first choice. Most (78%) NICUs were interested in participating in a trial evaluating azithromycin safety and efficacy in reducing BPD rates. Opinions and clinical practice varied between European neonatal units and differences in Ureaplasma treatment and prevention of BPD highlight the need for further azithromycin evaluation and for improved therapeutic knowledge in preterms.
Similar content being viewed by others
Introduction
Bronchopulmonary dysplasia (BPD) is a chronic pulmonary disease affecting preterm and low birth weight babies (<32 weeks gestation and <1500 g). It is one of the major causes of mortality and morbidity in neonates, characterized by diffuse airway damage, smooth-muscle hypertrophy, neutrophilic inflammation and parenchymal fibrosis1 and is defined by the need for supplemental oxygen beyond 36 weeks postmenstrual age2.
Many factors contribute to BPD and, primarily, impair antenatal lung growth3, making the preterm infant's lungs more vulnerable to injuries associated with oxygen therapy or assisted ventilation4, intrauterine/postnatal infections5, patent ductus arteriosus6 and genetic predisposition7,8.
The role of Ureaplasma spp. colonization of the lungs in the development of BPD remains controversial9,10,11,12. Ureaplasma is an eubacteria sub-categorised into two different species (U.Urealyticum and U.Parvum). It is a common commensal of the maternal genital tract, as up to 80% of women have been reported to be colonized13. Mother to child transmission may occur in utero, during delivery, or even postnatally through nosocomial transmission14. Numerous studies and reviews have discussed the potential role of Ureaplasma in the development of BPD9,15.
As part of the FP7 TINN2 Project (Treat Infections in Neonates 2, www.tinn2-project.org) the present survey was undertaken to evaluate a) the practices and opinions of European neonatal intensive care units (NICUs) regarding Ureaplasma as a risk factor in the development of BPD; b) the use of azithromycin, which is currently used off-label throughout Europe for this indication, to prevent BPD; c) and the need for a randomized controlled trial to evaluate efficacy of azithromycin in reducing the rates of BPD. Practices were also compared taking into consideration size of the NICUs and the countries' BPD rates. A subsidiary goal was to underpin other clinical studies about prevention of BPD by summarizing clinical practice relevant to trial design in multiple European units.
Results
Overall, 276 units (35%) accessed the questionnaire online and 167 (21%) completed the survey adequately and their data were analyzed. The top four countries, in terms of number of replies, covered 44% of the data (UK, Italy, France and Spain), with a response rate ranging from 31% for the UK to 13% for France.
Section A: demographic information
The 167 questionnaires were from 28 European countries (88%): 80% of NICUs were level III and 20% level II, with a median of 16 and 6 intensive care beds, respectively. The majority of NICUs admit more than 200 neonates ≤ 28 days of life, with no statistical differences between the top four countries (UK, Italy, France and Spain) and the rest (χ2 = 1.9, P = 0.59). Concerning the number of annual admissions of neonates ≤ 32 or ≤28 weeks' gestation, there is no significant difference for either between responses by the four main countries and the rest (χ2 = 3.6, P = 0.30 and χ2 = 0.6, P = 0.89, respectively). Most NICUs responded with less than 20% of babies who die before 36 weeks' gestation, with no statistical differences between the main four and the rest (χ2 = 5.7, P = 0.13). Detailed demographic data are presented in Tables 1 and 2.
Section B and C: perceived risk factors for BPD
All responders stated that the two major perceived risk factors for BPD, from among those proposed in the questionnaire, were: prematurity ≤ 28 weeks and high oxygen requirements. More than 50% also included pulmonary interstitial emphysema, suspected or proven bacterial sepsis and positive pressure ventilation as perceived risk factors; and the risk of developing BPD was considered much lower in preterm infants of between 28 and 32 weeks' gestation. There were no considerable inter-country differences in the perceived risk factors proposed in the questionnaire. Details are given in Table 3.
Only 63 of 167 (38% [95% CI, 30.37–45.08]) of the NICUs had a standard written protocol for the prevention of BPD. When available, the protocol included fluid restriction (71% of cases), postnatal corticosteroids (62%) and inhaled corticosteroids (24%). Most respondents (90%) assessed oxygen dependency at 36 weeks corrected GA to diagnose BPD.
Section D: role of Ureaplasma in the development of BPD and position regarding the use of azithromycin
Less than half of NICUs (66, 40%) answered that, in their opinion, Ureaplasma was associated with an increased risk of bronchopulmonary dysplasia (Likert scale of 4 or 5) and 79 of 167 (47% [95% CI, 39.73–54.88]) tested for Ureaplasma colonization at birth, with a wide range of babies tested per year (median, 10 [95% CI, 7.50–15.00]). The most common samples used for testing were endotracheal or nasopharyngeal secretions, with cultures and/or PCR-based tests performed on the samples. Neonates with confirmed Ureaplasma presence range from 0 to 70 (median, 3 [95% CI, 2.00–4.00]) per year. Considering only the four main responding countries, UK, Italy, France and Spain, the median and 95% CIs were: (0.5 [95% CI, 0.00–6.00]), (3 [95% CI, 0.00–10.00]), (6 [95% CI, 0.00–40.00]) and (2 [95% CI, 0.00–10.00]), respectively.
The estimated rate of Ureaplasma colonization in infants <28 weeks gestation ranged from 25 to 50%, with no significant difference between the four main responders and the rest (χ2 = 2.1, P = 0.44). Treatment for Ureaplasma was administered in 79 NICUs (47%), and, for the NICUs belonging to the nine MOSAIC study countries, the decision to treat or not was not correlated with the countries' BPD rate. Most respondents stated that treatment should be started immediately after birth, even if confirmation of colonization took up to 72 hours.
In all, 79 NICUs tested for Ureaplasma and the choice to test was not correlated with the countries' BPD rate. In cases of proven Ureaplasma infection, treatment with macrolides was administered in 74 of 79 (94%, [95% CI, 88.30–99.04]) NICUs that test for Ureaplasma (5 did not specify which antibiotic class was preferably used). Several macrolides were used: azithromycin was used throughout Europe (27% NICUs in 12 countries), but was not the unique drug in any country. Azithromycin was usually administered at a starting dose of 10 mg/kg (60% of NICUs), followed by a daily maintenance dose of 5 mg/kg (43% of NICUs). It was given both intravenously and orally, but the oral route was preferred if the infant was older than 1 week and weighed more than 1500 grams. Erythromycin was the most widely used macrolide in 30 out of 79 NICUs (38% [95% CI, 27.27–48.68]), from a total of 13 countries and was used predominantly in UK (30%), Germany (13%) and Switzerland (10%). Clarithromycin, used in 19 of 79 NICUs (24% [95% CI, 14.63–33.48]), was most commonly used in Italy (42%) and Austria (11%). Josamycin was only used in France (5%, 4/79).
Azithromycin use as prophylaxis is limited: only 9 NICUs (from Croatia, Czech Republic, France, Germany, Greece, Italy, Poland, Turkey and UK) used azithromycin, with the most commonly reported daily dosage of 10 mg/kg for a duration of between 3 and 21 days. Azithromycin was prescribed for both its anti-infective and anti-inflammatory properties. Of the 147 NICUs that did not routinely use azithromycin for prophylaxis, 93 specified that they would use it for both its properties (63% [95% CI, 55.47–71.06]), while 31% preferred to use it for its anti-infective properties and the remaining 6% only for its anti-inflammatory properties.
The items that were considered most influential in the decision to use azithromycin in prophylaxis or not were the need to conduct additional studies on the use of azithromycin in the preterm population and the need to establish criteria to select high-risk patients in whom prophylaxis against development of BPD would be beneficial. Further details are given in Table 4. The size of the NICUs was not correlated with the choice to employ prophylaxis or not and neither was the country's BPD rate for the nine countries considered.
Section E: future research
Overall, 78% [95% CI, 72.21–84.68] of the NICUs were interested in participating in the TINN2 project in order to evaluate the safety and efficacy of azithromycin versus placebo in reducing the rates of BPD in preterm babies of less than 28 weeks' gestation, including those in which azithromycin was not normally used. In addition, most neonatologists suggested that newborns between 23 and 28 weeks gestational age would be the optimal population for inclusion in a clinical trial of this drug.
Discussion
The present European survey was conducted to evaluate the opinion of neonatologists regarding perceived risk factors for BPD, the role of Ureaplasma infection and the current use of azithromycin in preterm babies. In line with the findings from a similar, previous survey on the prevention and treatment of sepsis in European NICUs (www.tinn-project.org), opinions and practices were found to vary between countries and centers.
Responders were mostly from level III NICUs, although these were different in size and number of newborn infants admitted each year. In agreement with already published data, neonatologists identify numerous risk factors for bronchopulmonary dysplasia, including prematurity of ≤28 weeks gestational age (incidence of BPD being inversely related to gestational age), but also high oxygen requirements, pulmonary interstitial emphysema, suspected or proven bacterial sepsis and positive pressure ventilation. Regarding prematurity, it is clear for all responders that babies 29 weeks' gestation or older are at limited risk of the disease compared to more preterm neonates. However, the incidence rates of BPD reported among the European countries varied widely and may be attributable to different population characteristics, care practices, differences in bacterial or viral epidemiology and survival rates16. Systematic differences between practices that reflect the incidence of BPD could mean that clinicians have adapted their practice to local circumstances. In that scenario, standardization of practice in a trial protocol could lead to worse outcomes in some centres. When the testing and intervention practices found in the TINN2 survey were compared with the BPD rates, by country, no correlations were found. Accordingly, standardized practice is justifiable in TINN2 and other studies.
Bronchopulmonary dysplasia is a multifactorial disease and there are increasing inferences among the scientific community, as well as experimental evidence, of a central role of Ureaplasma infection in lung disease in preterm neonates.
Mother to baby transmission of Ureaplasma depends on many factors, such as birth weight for gestational age, route of delivery and preterm labour17,18. The rate of vertical transmission to the newborn is inversely correlated with maturity and birth weight18. As suggested by Viscardi and Hasday, Ureaplasma infection may induce a robust pro-inflammatory response when transmitted in utero or postnatally, affecting both interstitial tissue and bronchoalveolar epithelium and resulting in myofibroblast proliferation and excessive collagen and elastin deposition11.
More than half of the NICUs do not routinely test for Ureaplasma infection at birth. The results of previous studies, however, found high colonization rates19,20 and suggest that testing in NICUs should be improved, also in light of the declared reasons for not testing, such as excessive cost and delay in culture results20. On the other hand, many units routinely test for Ureaplasma. Testing for Ureaplasma is acceptable in research settings.
The samples used for Ureaplasma isolation and cultures vary widely from amniotic fluid, via antenatal amniocentesis, to gastric aspirate at delivery, to endotracheal, bronchoalveolar and nasopharyngeal aspirates, to blood. In the survey, endotracheal secretions were the most frequent sample reported, as in the UK survey20. Although the best clinical sample for Ureaplasma identification has not been defined, the choice of endotracheal aspirates is supported by the literature, since it is quite simple and performed frequently for medical care10,21,22. This data supports the use of endotracheal secretions in research protocols.
Whichever tests were used to identify Ureaplasma presence including culture, histochemical, or polymerase chain reaction (PCR), the results, depending on the sample, usually took 48 to 72 hours. This time delay was considered too long and most neonatologists stated that treatment should start immediately after birth in order to limit pulmonary inflammation, which is shown to be a strong predictor of subsequent development of bronchopulmonary dysplasia23.
Macrolide antibiotics are widely used as antibacterial drugs. Clinical and experimental data, however, indicate that they also have antiinflammatory and immunomodulatory properties and their therapeutic indications have been expanded. Although their use in preterm babies varies between countries and units, in the NICUs involved in the present survey three macrolides were prescribed for the prevention and treatment of BPD.
Clarithromycin use appeared limited. Its activity against Ureaplasma, described as greater than that of erythromycin, was shown to prevent BPD development in preterm infants born weighing less than 1250 g and colonized with Ureaplasma24. It has been suggested that the anti-inflammatory effects of clarithromycin contributed to the overall lower incidence of BPD in the treatment group also in the Ballard azithromycin study19. Both of these studies concluded that early treatment of Ureaplasma colonized/infected patients may be beneficial.
Erythromycin was most frequently used. However, compared to azithromycin, it is inactivated by gastric acid and given orally as a stable salt, extensively metabolized by the cytochrome P450 system, including CYP3A, subjected to drug interactions and is responsible for prolonged QTC intervals25,26,27.
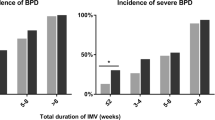
Azithromycin is the drug of choice in the treatment of Ureaplasma and prevention of BPD. It is hardly metabolized and has only a few adverse effects in adults and children. In this survey, azithromycin was used both for the treatment of confirmed infection and for prophylaxis of BPD in all preterm infants of less than 28 weeks gestation. Azithromycin has the advantage of having the lowest minimum inhibitory constants of less than 0.6 μg/L for both U. Urealyticum and U. Parvum. In addition, azithromycin was evaluated in a recent placebo-controlled study conducted in a population of 108 preterm neonates receiving oral azithromycin (10 mg/kg for 1 week then 5 mg/kg for 1 week), which found a lower BPD rate in treated patients (25% of BPD vs. 43% in the placebo group)28. To the best of the authors' knowledge, no trials exist comparing the efficacy of azithromycin to that of erythromycin in eradicating Ureaplasma in neonates. Results of an in-vitro susceptibility test showed that erythromycin is less active than azithromycin against Ureaplasma Urealyticum29. The efficacy of the drugs in prophylaxis or treatment in animal models was evaluated30 and the results showed that lung inflammation was significantly less in mice treated with azithromycin then in those treated with erythromycin, even if there was no statistically significant difference in survival. Initial clinical trials in preterm neonates used erythromycin to treat Ureaplasma infections, but its clinical efficacy has to be confirmed. In a study by Baier and colleagues27, erythromycin did not eliminate Ureaplasma from the airways of infants and did not reduce the incidence of BPD in VLBW. A Cochrane review by Mabanta et al31 confirmed the lack of efficacy of erythromycin in the treatment of Ureaplasma infections and showed no decrease in BPD incidence or severity.
The survey confirmed that azithromycin dosage was, in most cases, 10 mg/kg/day, but duration of treatment varied widely. The intravenous use of azithromycin as prophylaxis, or, in a few cases, the oral use, is still limited. Previous studies19,32,33,34 led to the currently most used dosage of 10 mg/kg/day, but the optimal dosage regime needs to be more well defined in additional studies and globally acknowledged recommendations need to be created. Azithromycin has recently been associated with cardiac arrhythmias in some vulnerable adult populations35. This association was not found in the clinical trials of azithromycin in neonates, published up to now, but need to be better studied19,28. Avoidance of bias is essential, so the risk/benefit ratio of the therapy must be based primarily on evidence from randomized controlled trials. Furthermore, the fact that no correlation seems to exist between a country's BPD rate and the practices of its NICUs and the fact that, in agreement with the previous UK survey20, neonatologists feel the need for additional data on the role of Ureaplasma in BPD, most likely reveal a lack of shared, acknowledged therapeutic strategies and underline uncertainty across the neonatal community in this area. In this context, the aim of the upcoming TINN2 study is to carry out an RCT to assess the safety and efficacy of azithromycin on the rate of survival without BPD and to lead to more well defined recommendations.
This survey has some limitations. Since a validated list of all EU NICUs does not exist, considerable effort was made to identify the majority of centres. A total of 793 NICUs in 32 European countries were contacted, but the response rate was low in some countries. It is possible that those who responded are more likely to culture for Ureaplasma or use azithromycin and this may have introduced some bias in the results. Furthermore, NICUs with few yearly admissions of preterm neonates were not excluded from the analyses in order to have a more representative description of the European context and this may have included NICUs with less experience in terms of caring for neonates at greater risk of developing BPD. Another limit is that the attempt to compare country BPD rates with NICU testing and intervention practices was limited to the list of nine countries from the MOSAIC study, so not all participating TINN2 countries were considered and the results of the comparison may not be generalisable. Finally, the BPD rates from the MOSAIC study referred to specific regions of the countries and were not necessarily representative of the entire countries. Another limit that should be mentioned is that the UK weighs more in terms of number of NICUs represented and this could have led to bias in the results. However, the dosage schedule, one of the most important variables investigated in the survey, varied independently of the country considered.
The survey permitted a precise description of the current strategies for BPD treatment in the different NICUs. These, as documented by others36,37, are based on postnatal surfactant, widespread use of antenatal corticosteroids, fluid restriction and mechanical ventilation to treat respiratory distress syndrome. This data can be used by other groups designing and assessing the feasibility of, pan-European trials of strategies to prevent BPD. Numerous centers declared that they would be interested in participating in the FP7 TINN2 project, stressing their desire for additional information on the safety and efficacy of azithromycin, which is currently used off-label in neonatal treatment and the need to improve therapeutic knowledge in this vulnerable population. This data will contribute to the development of a range of protocols concerning the prevention of BPD that are acceptable to study centres, for example by ensuring that inclusion criteria and sample collection strategies are relevant to clinical practice.
Methods
Questionnaire
The present survey was conducted through an online questionnaire similar to that used in a previous TINN group survey on the prophylactic use of fluconazole38 and piloted by members of the TINN2 consortium.
The survey consisted of 64 questions (15 of which compulsory) divided into five sections. Section A contained demographic information on the NICU: level of care and yearly admission of neonates and preterm babies less than 32 and 28 weeks' gestational age (GA). As the levels of care are not defined precisely in Europe, an acknowledged definition was provided as an annex39.
In sections B and D respondents were asked to state their unit's opinion on the perceived risk factors for BPD and the rationale for azithromycin prophylaxis. Responses were measured on a 5 point Likert scale (1: least important to 5: most important) and further dichotomized (≤3: less important and ≥4: important). Section C focused on BPD prevention and inquired about presence and content of BPD prevention protocols for babies < 28 weeks. Section D addressed Ureaplasma treatment used for BPD prophylaxis and collected data on drug use and dosage schedules. Section E inquired about general information on clinical research in neonates and about interest in participating in the FP7 TINN2 project.
Study participants
In order to be as representative as possible of European practices, the list of NICUs to contact was based on that created during the first TINN project (www.tinn-project.org). In addition, relevant neonatal networks, societies and individual physicians were emailed for additional contacts. Overall, 793 units in 32 countries (26 member states, plus Croatia, Republic of Macedonia, Norway, Serbia, Switzerland and Turkey) were invited to participate between April and July 2012. Each unit was contacted individually by email; the aims were described and a link to the survey provided. The invitation letter specified that the questionnaire was to be filled in by the unit head or delegated to a senior colleague and specified that all participants would receive the final report.
Additional reminders were emailed to encourage participation and to complete missing data. Up to three reminders were sent between May and June 2012. Data were checked for consistency and analyzed in a three month period.
Variation in clinical practice that reflects variation in outcomes may need to be respected in study protocols. In order to assess whether approaches for testing and interventions were associated with a country's rate of BPD, the rates for nine different countries, as recently found in the MOSAIC study16, were compared with the TINN2 data on the practices of NICUs in those countries. Specifically, the following variables were considered: whether the NICUs a) assessed oxygen dependency at 36 weeks corrected gestational age to assess bronchopulmonary dysplasia, b) tested for Ureaplasma, c) treated Ureaplasma and d) used azithromycin for prophylaxis. The Pearson's coefficient of correlation was used to calculate these correlations. The Chi-squared test was used to evaluate differences between demographic characteristics of the main four responding countries and the rest, with a P value of <0.05 considered to be statistically significant. The size of the NICUs, as measured in terms of yearly number of: a) admitted neonates, b) preterms < 28 weeks' gestational age, c) preterms < 32 weeks' gestational age and d) number of NICU beds, was also compared to their use or not of prophylaxis, using the Chi-squared test with Yates' correction.
References
Baraldi, E. & Filippone, M. Chronic lung disease after premature birth. N. Engl. J. Med. 357, 1946–1955 (2007).
Walsh, M. C. et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics. 114, 1305–1311(2004).
Lall, A., Prendergast, M. & Greenough, A. Risk factors for the development of bronchopulmonary dysplasia: the role of antenatal infection and inflammation. Expert Rev. Respir. Med. 1, 247–254 (2007).
Philip, A. G. Chronic lung disease of prematurity: a short history. Semin. Fetal Neonatal Med. 14, 333–338 (2009).
Lahra, M. M., Beeby, P. J. & Jeffery, H. E. Intrauterine inflammation, neonatal sepsis and chronic lung disease: a 13-year hospital cohort study. Pediatrics. 123, 1314–1319 (2009).
Redline, R. W., Wilson-Costello, D. & Hack, M. Placental and other perinatal risk factors for chronic lung disease in very low birth weight infants. Pediatr. Res. 52, 713–719 (2002).
Bhandari, V. & Gruen, J. R. The genetics of bronchopulmonary dysplasia. Semin. Perinatol. 30, 185–191 (2006).
Hadchouel, A. et al. Identification of SPOCK2 as a susceptibility gene for bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 184, 1164–1170 (2011).
Beeton, M. L. et al. Role of pulmonary infection in the development of chronic lung disease of prematurity. Eur. Respir. J. 37, 1424–1430 (2011).
Cassell, G. H. et al. Association of Ureaplasma urealyticum infection of the lower respiratory tract with chronic lung disease and death in very-low-birth-weight infants. Lancet. 2, 240–245 (1988).
Viscardi, R. M. & Hasday, J. D. Role of Ureaplasma species in neonatal chronic lung disease: epidemiologic and experimental evidence. Pediatr. Res. 65, 84R–90R (2009).
Waites, K. B., Katz, B. & Schelonka, R. L. Mycoplasmas and ureaplasmas as neonatal pathogens. Clin. Microbiol. Rev. 18, 757–789 (2005).
Abele-Horn, M., Wolff, C., Dressel, P., Pfaff, F. & Zimmermann, A. Association of Ureaplasma urealyticum biovars with clinical outcome for neonates, obstetric patients and gynecological patients with pelvic inflammatory disease. J. Clin. Microbiol. 35, 1199–1202 (1997).
Jobe, A. H. & Ikegami, M. Antenatal infection/inflammation and postnatal lung maturation and injury. Respir. Res. 2, 27–32 (2001).
Turner, M. A., Jacqz-Aigrain, E. & Kotecha, S. Azithromycin, Ureaplasma and chronic lung disease of prematurity: a case study for neonatal drug development. Arch. Dis. Child. 97, 573–577 (2012).
Gortner, L. et al. Rates of bronchopulmonary dysplasia in very preterm neonates in Europe: results from the MOSAIC cohort. Neonatology. 99, 112–117 (2011).
Cassell, G. H., Waites, K. B., Watson, H. L., Crouse, D. T. & Harasawa, R. Ureaplasma urealyticum intrauterine infection: role in prematurity and disease in newborns. Clin. Microbiol. Rev. 6, 69–87 (1993).
Sanchez, P. J. Perinatal transmission of Ureaplasma urealyticum: current concepts based on review of the literature. Clin. Infect. Dis. 17 Suppl 1 S107–S111 (1993).
Ballard, H. O. et al. Use of azithromycin for the prevention of bronchopulmonary dysplasia in preterm infants: a randomized, double-blind, placebo controlled trial. Pediatr. Pulmonol. 46, 111–118 (2011).
Maxwell, N. C., Nuttall, D. & Kotecha, S. Does Ureaplasma spp. cause chronic lung disease of prematurity: ask the audience? Early Hum. Dev. 85, 291–296 (2009).
Payne, M. S. et al. Molecular microbiological characterization of preterm neonates at risk of bronchopulmonary dysplasia. Pediatr. Res. 67, 412–418 (2010).
Miralles, R. et al. Relationship between antenatal inflammation and antenatal infection identified by detection of microbial genes by polymerase chain reaction. Pediatr. Res. 57, 570–577 (2005).
Kotecha, S., Chan, B., Azam, N., Silverman, M. & Shaw, R. J. Increase in interleukin-8 and soluble intercellular adhesion molecule-1 in bronchoalveolar lavage fluid from premature infants who develop chronic lung disease. Arch. Dis. Child. Fetal Neonatal Ed. 72, F90–F96 (1995).
Ozdemir, R. et al. Clarithromycin in preventing bronchopulmonary dysplasia in Ureaplasma urealyticum-positive preterm infants. Pediatrics. 128, e1496–e1501 (2011).
Lyon, A. J. et al. Randomised trial of erythromycin on the development of chronic lung disease in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 78, F10–F14 (1998).
Jonsson, B., Rylander, M. & Faxelius, G. Ureaplasma urealyticum, erythromycin and respiratory morbidity in high-risk preterm neonates. Acta Paediatr. 87, 1079–1084 (1998).
Baier, R. J., Loggins, J. & Kruger, T. E. Failure of erythromycin to eliminate airway colonization with ureaplasma urealyticum in very low birth weight infants. BMC Pediatr. 3, 10 (2003).
Gharehbaghi, M. M., Peirovifar, A., Ghojazadeh, M. & Mahallei, M. Efficacy of azithromycin for prevention of bronchopulmonary dysplasia (BPD). Turk J. Med. Sci. 42, 1070–1075 (2012).
Samra, Z., Rosenberg, S. & Dan, M. Susceptibility of Ureaplasma urealyticum to tetracycline, doxycycline, erythromycin, roxithromycin, clarithromycin, azithromycin, levofloxacin and moxifloxacin. J. Chemother. 23, 77–9 (2011).
Walls, S. A. et al. Antibiotic prophylaxis improves Ureaplasma-associated lung disease in suckling mice. Pediatr. Res. 66, 197–202 (2009).
Mabanta, C. G., Pryhuber, G. S., Weinberg, G. A. & Phelps, D. L. Erythromycin for the prevention of chronic lung disease in intubated preterm infants at risk for, or colonized or infected with Ureaplasma urealyticum. Cochrane Database Syst. Rev. CD003744 (2003).
Ballard, H. O., Anstead, M. I. & Shook, L. A. Azithromycin in the extremely low birth weight infant for the prevention of bronchopulmonary dysplasia: a pilot study. Respir. Res. 8, 41 (2007).
Hassan, H. E. et al. Pharmacokinetics, safety and biologic effects of azithromycin in extremely preterm infants at risk for ureaplasma colonization and bronchopulmonary dysplasia. J. Clin. Pharmacol. 51, 1264–75 (2011).
Viscardi, R. M. et al. Azithromycin to prevent bronchopulmonary dysplasia in ureaplasma-infected preterm infants: pharmacokinetics, safety, microbial response and clinical outcomes with a 20-milligram-per-kilogram single intravenous dose. Antimicrob. Agents Chemother. 57, 2127–33 (2013).
Ray, W. A., Murray, K. T., Hall, K., Arbogast, P. G. & Stein, C. M. Azithromycin and the risk of cardiovascular death. N. Engl. J. Med. 366, 1881–1890 (2012).
Bancalari, E. Changes in the pathogenesis and prevention of chronic lung disease of prematurity. Am. J. Perinatol. 18, 1–9 (2001).
Schelonka, R. L. & Waites, K. B. Ureaplasma infection and neonatal lung disease. Semin. Perinatol. 31, 2–9 (2007).
Kaguelidou, F. et al. European survey on the use of prophylactic fluconazole in neonatal intensive care units. Eur. J. Pediatr. 171, 439–445 (2012).
Stark, A. R. Levels of neonatal care. Pediatrics. 114, 1341–1347 (2004).
Acknowledgements
The authors would like to thank all the neonatologists who took the time to participate in the survey and Marco Sequi of the IRCCS-Mario Negri Institute for the statistical support and analyses. This work has been supported by the European Commission within the 7th Framework Programme under grant agreement no. FP7-HEALTH-2010-260908 (TINN2 Project).
Author information
Authors and Affiliations
Contributions
C. Pans managed the setting up and running of the survey and cleaned, managed and analysed data and wrote the main manuscript text. C. Pand assisted in setting up and running the survey and in cleaning and analysing data and revised the manuscript. V.E. assisted in analysing data and revised the manuscript text. M.T. contributed to setting up the survey and guiding the analyses and revised the manuscript. S.K. and E.J.A. designed the questionnaire, contributed to guiding the analyses and revised the manuscript. M.B. supervised the setting up and running of the survey and the data analyses and contributed to writing the manuscript. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Additional information
Funding: Supported by the European Commission (FP7-HEALTH-2010-260908, TINN2 Project)
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Pansieri, C., Pandolfini, C., Elie, V. et al. Ureaplasma, bronchopulmonary dysplasia and azithromycin in European neonatal intensive care units: a survey. Sci Rep 4, 4076 (2014). https://doi.org/10.1038/srep04076
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep04076
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.